Abstract
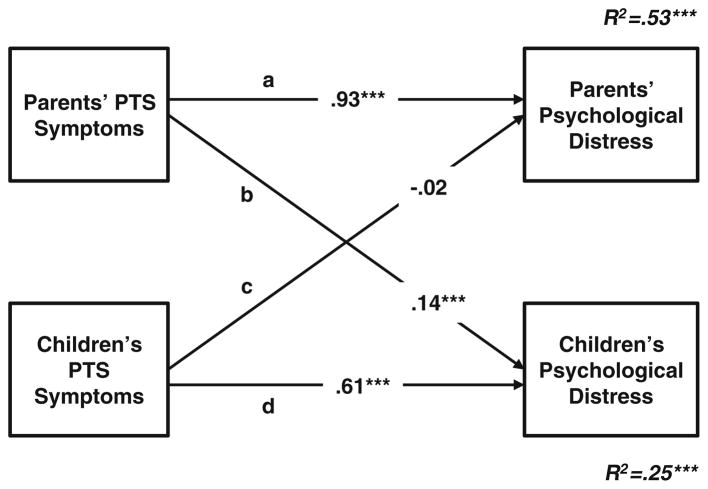
The interdependent adjustment of children and their parents following disasters has been well documented. We used the Actor-Partner Interdependence Model (APIM) to provide an appropriate analytical framework for examining how family members may contribute to each other’s post-disaster mental health. Independent self-reports were collected from parent–child dyads (n=397) residing in a rural community in Indonesia that was devastated by a major earthquake. Elementary school children (M=10 years; 51 % female) and one of their parents (M=41 years; 73 % female) each reported on their disaster exposure, posttraumatic stress (PTS) symptoms, and general distress. The APIM was used to examine mental health within dyads and moderation by gender across dyads. Children reported lower disaster exposure and fewer PTS symptoms, but similar general distress levels, as their parents. Children’s and parents’ disaster-specific PTS symptoms were the strongest predictor of their own general distress. Parents’ PTS symptoms were associated with children’s general distress (b=0.14, p<0.001), but children’s PTS symptoms were not associated with parents’ general distress (b=−0.02, p>0.05). Findings were not moderated by parents’ or children’s gender. Although children and parents may respond differently to natural disasters, they may be best understood as a dyad. APIM analyses provide new evidence suggesting a unidirectional path of influence from parents’ disaster-related symptomatology to children’s general mental health. Dyadic approaches to understanding mental health and treating symptoms of distress among disaster survivors and their families following trauma are encouraged.
Keywords: Parent–child dyads, Posttraumatic stress, Distress, Trauma exposure, Natural disaster
When a natural disaster devastates an entire community, its survivors are often left with psychological remnants of the event, including general distress and posttraumatic stress (PTS) symptoms such as emotional numbing and avoidance (Norris et al. 2002). Yet, as proposed by social ecological and family systems theory (Bronfenbrenner 1979; Weems and Overstreet 2008), individuals may be best understood in light of their contextual and interpersonal surroundings. A large body of empirical studies shows that disaster survivors do not experience their symptoms in isolation as these events also affect others around them (e.g., Kelley et al. 2010; Lambert et al. 2014; Salmon and Bryant 2002; Spell et al. 2008). This is especially relevant for parents and young children who typically go through the post-disaster adjustment period together as an interdependent unit, or dyad, because physical proximity is required for the child to receive and the parent to provide care. In addition, Attachment Theory (Bowlby 1988) suggests that children and parents desire emotional proximity as it ensures survival and provides a sense of security for the child and fulfills parents’ inherent needs to care for their offspring. As such, parent–child dyads have a highly interwoven relationship marked with frequent and prolonged interactions (Cox and Paley 2003); this presents an example of how a shared disaster experience may set the stage for interdependent mental health, such that one person’s psychological disequilibrium is likely tied to the other’s (Birmes et al. 2009; Charuvastra and Cloitre 2008; Gil-Rivas et al. 2010; Hafstad et al. 2010; Li et al. 2010; Polusny et al. 2011; Scheeringa and Zeanah 2008; Wickrama and Kaspar 2007).
In light of the inherent dynamics in parent–child relationships, there are several ways through which post-disaster PTS symptoms may spill over to general distress within parent–child dyads. For example, child-rearing presents normative demands on a parent (Deater-Deckard 2004), but providing care for a child who exhibits PTS symptoms may be distressing (Costa et al. 2006). This may be especially true when parents themselves are simultaneously coping with the disaster and its aftermath. Furthermore, parents’ natural tendency to provide for and protect their children may make it particularly difficult for them to see their son or daughter exhibit PTS symptoms, leading the parent to feel helpless (Appleyard and Osofsky 2003) and even more distressed. In addition, whereas children’s needs for attention are likely to increase after a disaster, their parents’ ability to provide that attention could diminish (Schwerdtfeger and Geoff 2007), especially as parents may be trying to re-establish lost resources (e.g., shelter, financial security) as well as manage their own adjustment. In fact, parents may experience their own PTS symptoms, subjecting children to inadequate parental support (e.g., emotional unresponsiveness) and poor parenting behaviors (e.g., rejection, avoidance, distancing; Hafstad et al. 2010; Kelley et al. 2010). This, in turn, may make it difficult for children to emotionally and cognitively process and adjust to the traumatic event (Salmon and Bryant 2002), resulting in heightened distress.
Indeed, parents and children’s intertwined relationship (La Greca et al. 2010; Laor et al. 1997; Silverman and La Greca 2002), as well as the links between their mental health following disasters (Bonanno et al. 2010; Masten and Narayan 2012; Morris et al. 2012), have been researched extensively. However, two primary shortcomings remain within the literature. First, evidence consistently shows that parents’ mental health spills over, or contributes, to their children’s adjustment (Furr et al. 2010; Leen-Feldner et al. 2013; Levine et al. 2005), but findings demonstrating the relevance of children’s mental health in their parents’ adjustment are less frequent. In part, this may be due to the challenges associated with obtaining self-reports from children about their disaster-related experiences; however, adults may be equally susceptible to their children’s mental health following a disaster and this warrants further attention. Second, many research studies fail to recruit both individuals, either due to logistical challenges or a lack of recognition of the need to include both members of a dyad in order to adequately assess how one person may influence the other. Some prior work controls for parents’ and children’s mental health in assessing each dyad member’s adjustment (e.g., Gil-Rivas et al. 2004), but neither this nor running separate analytic models to examine psychological outcomes in a dyad is adequate. For example, when investigating the role of children’s and parents’ PTS symptoms in each other’s general psychological distress, both their PTS symptoms and their general distress may be correlated. Ideally, this should be examined with an analytic technique that closely matches the conceptual understanding of the interdependent relationship between parents and children (Kenny 1996).
The Actor-Partner Interdependence Model (APIM; Kenny et al. 2006) is ideal for examining a relational phenomenon between two interdependent individuals because it treats the dyad (instead of the individual parent or child) as the unit of analysis. The APIM is specifically designed to test associations between correlated constructs from two members of a dyad, for instance, how parents’ and children’s PTS symptoms may contribute to each other’s general distress, while accounting for the interdependent nature of their relationship. It has been used by prior studies examining similar dyadic phenomena during and following traumatic experiences (e.g., Juth et al. 2015; Smith et al. 2001). Moreover, it can be used to compare the relative importance of disaster-related PTS symptoms for general distress within a dyad member (e.g., are children’s own PTS symptoms or parents’ PTS symptoms a stronger predictor of children’s general distress?), between dyad members (e.g., are spillover effects from PTS symptoms to general distress stronger in parents vs. children?), or between dyads (e.g., are spillover effects stronger in mother–child dyads vs. father–child dyads?). This has the potential to expand the theoretical understanding of dyadic interactions within family systems following disaster. It also has important implications for clinical treatments and interventions as interpreting psychological outcomes without considering the role of proximal social contacts could lead to false conclusions about the contributing source(s) of disaster-related adjustment.
The current study examines the interdependent mental health of parents and children in a developing country prone to repeated natural disasters. It was conducted in a rural community near Yogyakarta, Indonesia, whose inhabitants experienced a 6.3 magnitude earthquake in May 2006, resulting in approximately 6000 deaths, almost 40,000 injuries, and over 500,000 damaged or destroyed homes that were unrepaired for several years (U.S. Department of the Interior 2010). We applied the APIM to 794 independent self-reports of earthquake exposure and mental health from parents and children to investigate a potential spillover effect from parents’ and children’s PTS symptoms to each other’s general psychological distress after the 2006 earthquake. We hypothesized that parents’ and children’s PTS symptoms would spill over to each other’s general distress.
In addition, we considered gender as a potential moderator of the mental health spillover effects as it is possible that parents’ and children’s gender is related to their interdependence. An important shortcoming of the literature is that most studies examining post-disaster psychological responses in parent–child dyads only include mothers (Scheeringa and Zeanah 2008). While children generally have more frequent interactions and closer relationships with their mothers compared to their fathers (Collins and Russell 1991; Montemayor and Brownlee 1987), fathers also play an important role in children’s psychological and emotional well-being (Kilic et al. 2003; Weitzman et al. 2011). It may be that spillover effects of mental health may differ between mother–child dyads vs. father–child dyads. Furthermore, the child’s gender may moderate the spillover effects as young boys typically follow a different developmental trajectory than young girls (Brody 1985). For instance, girls are generally more engaged with their mothers than fathers, whereas the opposite is true for boys (Hosley and Montemayor 1997). As there is neither consistent nor ample evidence for how parents’ and children’s genders differentially impact their interdependent well-being following natural disasters (Scheeringa and Zeanah 2008), this remains an important avenue for investigation. Therefore, we also explored the possibility that parents’ and children’s gender would moderate the observed spillover effects such that spillover effects would differ in magnitude between father–child vs. mother–child dyads and between parent-son versus parent-daughter dyads.
Methods
This study was a collaborative effort with the Universitas Sanata Dharma in Indonesia and Psychology Beyond Borders as part of larger project designed to investigate Indonesian families exposed to the 2006 earthquake and other natural disasters. Families were recruited in 2009 from six schools (two from each of the three main school systems: State-sponsored, Catholic, Islamic) in the highly exposed educational subdistricts of Bambanglipuro and Pundong in Bantul, Special District of Yogyakarta, after an initial needs assessment was conducted in the community (Widyatmoko et al. 2011). Although the larger project included an intervention assessment, only baseline data were utilized for the present report of parent–child dyads.
Sample and Procedures
Each school distributed a letter to families of children in the fourth and fifth grades explaining the goals of the research and inviting one parent from each family to attend an information session. At this session, informed consent was explained and verbally requested from the parents; those who agreed to participate were provided with a survey to complete at that time. Over the next several days, children were assented and completed similar surveys during after-school sessions with trained research assistants available to answer questions.
Out of 538 families, 80 % of parents (n=428; Female = 311, Male = 101, no gender information = 16) came to the session and completed a survey. Those parents who were illiterate or could not comprehend the questions were read the items by a trained research assistant. All parents who completed a survey consented to their children’s participation; all children provided assent. When more than one child from a family participated, one child was randomly selected for inclusion in analyses (results did not change when the other child was included instead). Parents were excluded from the analyses if their children were absent on the day the survey was administered in their school (n=31), resulting in 397 parent–child dyads (providing adequate power for our analyses; Kenny et al. 2006). All procedures for this study were approved by the Institutional Review Board of the University of California, Irvine.
Children were 51 % female and had a mean age of 10 years (SD=1.00; range=8–17). Parents (or in a few cases, other guardians) were primarily female (73 %), had a mean age of 41 years (SD=9.39), with a median education level of high school, and median monthly household income of 500,000–750,000 rupiah (approximately USD $50–$75).
Measures
In order to develop culturally-sensitive measures for conducting research with an ethnic population for whom no pre-existing measures have been validated, a brief ethnography model (Bolton and Tang 2004) was used. We assessed whether existing constructs for PTS symptoms and general distress were feasible for this population through open-ended qualitative interviews with people in the community, as well as interviews with people identified as being knowledgeable about local distress (i.e., teachers, village heads).
All measures were translated using a dual-forward with review translation process (Maxwell 1996). This was done to ensure that each measure accurately assessed the construct of interest in adults and children. Two individuals independently translated the measures from English to Indonesian (Bahasa Indonesia). The translations were then compared by a team including monolingual English and Indonesian speakers, as well as bilingual English-Indonesian speakers. The translated wording was used if the two translations matched and were confirmed by the team. If there were discrepancies in translation or questions about content, the team reviewed the documents and came to consensus on the most accurate version. Some survey items and instructions were modified using the local Javanese (Basa Jawa) wording as pilot testing indicated that this dialect was more appropriate.
Earthquake Exposure
Parents’ and children’s objective disaster exposure was assessed with items from the UCLA-PTSD Reaction Index for Children (PTSD-RI; Steinberg et al. 2004). Participants reported yes or no to whether they were hurt badly, someone else was hurt badly, someone died, they saw a dead body, and they or their family suffered any material loss due to the earthquake. The number of exposures was summed and averaged for each member of the dyad.
General Distress
The Brief Symptom Inventory-18 (BSI-18; Derogatis 2001) assessed parents’ and children’s distress (also used in similar post-disaster studies; e.g., Gil-Rivas et al. 2004). One item, “feeling blue”, was removed because an Indonesian translation of this phrase was not interpretable. Participants were asked to report how much they experienced symptoms of anxiety, depression, and somatization during the past 7 days on a 0 (not at all) to 4 (extremely) scale. An average score was calculated to represent global distress (Cronbach’s αparents=0.96, Cronbach’s αchildren=0.89).
Posttraumatic Stress Symptoms
Two measures were used to assess PTS symptoms because trauma-specific distress manifests differently in adults and children (Hamblen and Barnett 2009). The UCLA-PTSD Reaction Index for Children (PTSD-RI; Steinberg et al. 2004) assessed the frequency with which children experienced PTS symptoms. Children reported how often they experienced each item during the past month on a 0 (none of the time) to 4 (most of the time) scale. The brief ethnography methodology also identified four additional symptoms that were not captured in the existing assessment tool: (1) not wanting to talk, (2) “ndomblong” (a local term with no direct English translation that can be described as “zoning out,” “blank stare,” or “excessive daydreaming”), (3) wanting to be accompanied by an adult at all times, and (4) being lazy specifically in reference to studying for school (“malas mengerjakan”). Single items assessing each of these symptoms were added to the PTSD-RI. An average score of responses to the 24 items was calculated to represent PTS severity (Cronbach’s α with and without added items=0.88).
The PTSD Checklist (PCL-C; Weathers et al. 1991) assessed 17 trauma-related symptoms specific to the earthquake among parents, including re-experiencing the trauma, emotional numbing/avoidance, and hyperarousal. Parents reported how often they experienced each item during the past month on a 0 (none of the time) to 4 (most of the time) scale. The brief ethnography methodology identified three additional symptoms that were not captured in the existing assessment tool: (1) unable to control anger (a less severe form of the culture-bound disorder amok associated with Malaysia; Westermeyer 1973), (2) thinking excessively or having too many thoughts in general (not related to the earthquake or another specific event), and (3) “ndomblong” (see description above). An average score of responses to the 20 items was calculated to represent PTS severity (Cronbach’s α without added items=0.94, Cronbach’s α with added items=0.95).
Overview of Analyses
Child and adult survey data were assessed for missingness and nonresponse. Overall rates of per-item missing data ranged from 0.39–3.59 % in children and 0–5.9 % in adults. Multiple imputation (MI) was used to replace missing item values in the PTS symptoms and general distress measures from the distribution of complete observed and missing values using SPSS expectation maximization MI procedures (Little and Rubin 1987). Demographic and earthquake exposure items were not imputed. Conducting analyses without imputations yielded the same pattern of results and significant associations; all results reported are based on imputed data. One child was several years older than the others (i.e., 17 years old); when analyses were conducted with versus without this participant, the pattern of results remained the same.
Descriptive statistics were conducted for parents’ and children’s mental health measures. Next, the APIM was tested in a Structural Equation Modeling (SEM) framework using Mplus 7.0 (Muthén & Muthén, 1998–2011) to examine the interrelated mental health of parent–child dyads. The APIM fits regression coefficients to the associations between the examined constructs. These associations are typically described in terms of actor effects (e.g., the association between children’s PTS symptoms and their own general distress) and partner effects (e.g., the association between parents’ PTS symptoms and children’s general distress). The advantage of this analytic model is threefold: (1) it accounts for the shared variances and correlated error variance between the dyad members’ parameters (i.e., parents’ and children’s PTS and general distress) to control for nonindependence of the constructs and residual errors; (2) it can be run in a SEM framework in which actor and partner effects are examined simultaneously within a single model that controls for all other effects (i.e., parents’ and children’s PTS are regressed on their own and each other’s general distress, controlling for all other regressions in the model); (3) a SEM APIM enables effect size comparisons between regression coefficients within a dyad member (e.g., are children’s own PTS symptoms or parents’ PTS symptoms a stronger predictor of children’s general distress?), between dyad members (e.g., are spillover effects from PTS symptoms to general distress stronger in parents vs. children?), or between dyads (e.g., are spillover effects stronger in mother–child dyads vs. father–child dyads?).
Results
Descriptive Statistics
Participants had been exposed to repeated natural disasters, including a tsunami, floods, and volcanic eruption, in the 5 years preceding this study. Nevertheless, a majority of participants (84 % of adults; 87 % of children) reported the 2006 earthquake as being the worst recent disaster they had experienced. Table 1 provides a summary and comparison of parents’ and children’s reported earthquake exposure. Approximately two-thirds of the parents and children saw a dead body as a result of the earthquake, more than two-thirds of the families suffered material loss in the earthquake, approximately 10 % of the adults and 16 % of the children were hurt badly in the disaster, and over 75 % of the adults and children reported someone else being hurt badly.
Table 1.
Children’s and parents’ disaster exposure and mental health
| Parents
|
Children
|
Paired t-test
|
|||||
|---|---|---|---|---|---|---|---|
| Item | n (%) | M (SD) | n (%) | M (SD) | t (df) | 95 % Confidence Interval | Cohen’s d |
| Disaster exposurea (0–5) | 2.49 (0.90) | 2.36 (0.95) | 2.230 (373)* | 0.015, 0.236 | 0.12 | ||
| I was hurt badly | 39 (10) | 60 (15) | |||||
| Someone else was hurt badly | 302 (76) | 307 (77) | |||||
| Someone died | 311 (78) | 302 (76) | |||||
| I saw a dead body in my town as a result of the earthquake | 262 (66) | 255 (64) | |||||
| My family or I suffered material loss in the earthquake | 342 (86) | 267 (67) | |||||
| Posttraumatic stress symptomsb (0–4) | 2.13 (0.81) | 1.31 (0.58) | 16.474 (396)*** | 0.726, 0.922 | 0.83 | ||
| General distressc (0–4) | 1.28 (1.04) | 1.38 (0.75) | −1.592 (396) | −0.211, 0.022 | 0.08 | ||
Differences in sample size due to missing data
p<0.05.
p<0.001
n=374 dyads.
n=359 dyads.
n=397 dyads
Two-tailed paired t-test comparisons indicate that parents reported greater exposure and higher numbers of PTS symptoms than their children. Parents and children reported similar levels of general distress; paired sample t-tests revealed no significant differences in psychological distress within dyads (Table 1). One-way ANOVA and Tukey post-hoc tests indicated that there were no significant differences in PTS symptoms or general distress among families recruited from State-sponsored (n=163; 41 %), Muslim (n=136; 34 %), and Catholic (n=98; 25 %) schools (ps>0.05).
Post-Disaster Dyadic Mental Health
First, the base version of the APIM was fitted to obtain actor and partner effects of PTS symptoms on general distress for parents and children among all dyads. When all model paths (all actor and partner effects) were specified to be estimated freely, the model was just-identified (i.e., the observed and model-implied covariance matrices are equal; df=0); as such, conventional model fit statistics (R2) are reported. As hypothesized, the base version of the model (Fig. 1) provides evidence that PTS symptoms are correlated with general distress in parents and children. It also provides evidence for a partner effect from parents’ PTS symptoms to children’s distress, but not vice versa. That is, there is a spillover effect from parents’ post-disaster symptomatology to children’s general distress, even when controlling for children’s own PTS symptoms. Repeating these analyses controlling for type of school and for parents’ and children’s degree of earthquake exposure revealed the same pattern of results and significance; therefore, these variables are excluded to fit a more parsimonious model to the data.
Fig. 1.
Standardized beta coefficients of APIM analyses regressing parents’ and children’s PTS symptoms on general distress (n=397 dyads). Actor effects are represented by Paths a and d. Partner effects are represented by Paths b and c. R2s represent the variance in parents’ and children’s general distress explained by the model. 95 % Confidence Intervals: Path a (0.85, 1.02), Path b (0.06, 0.22), Path c (−0.14, 0.10), Path d (0.50, 0.72). Standard Errors of beta coefficients: Path a (0.04), Path b (0.04), Path c (0.06), Path d (0.05). ***p<0.001
Next, the APIM was re-run with constrained model paths to examine differences in the magnitude of actor and partner effects within and between dyad members. Constraining model paths specifies their standardized estimates to be equal. If the χ2 test statistic of the model with constrained paths is significant, then the constrained model paths may not be equal. If the χ2 test statistic is not significant, then the results provide no evidence that the constrained model paths are significantly different from one another. To examine the magnitude of actor effects and partner effects within parents and children, these effects were constrained to be equivalent within each dyad member. For both parents and children, actor effects were stronger than partner effects; that is, parents’ and children’s own PTS symptoms were a stronger predictor of their general distress levels compared to each other’s PTS symptoms. To test whether actor effects and partner effects were similar in magnitude between parents and children, these effects were constrained to be equivalent between dyad members. Constrained paths showed that parents’ actor effects and children’s partner effects were significantly stronger than children’s actor effects and parents’ partner effects, respectively. Thus, the association between PTS symptoms and general distress is stronger in parents than in children, and parents’ PTS symptoms have a stronger association with children’s general distress than vice versa.
Finally, separate multigroup APIM analyses with cross-group equality constraints were conducted to test the significant spillover effects for moderation by parent and child gender. As with the baseline APIM, constraining model paths across two groups specifies the standardized estimates of those model paths to be equal in both groups. The χ2 test statistic then provides information as to whether the two paths are significantly different from one another. First, parent–child dyads were split into father–child and mother–child dyad groups to determine whether parents’ gender moderated any of the significant spillover effects. Because only the spillover effect from parents’ PTS symptoms to children’s general distress was significant, this effect was tested for moderation by parents’ gender in two separate models with constrained partner paths. When all parameters were free to vary across the two groups, the model was fully saturated (df=0). Comparing the different dyad groups with constrained paths, the models provided no evidence that mothers’ versus fathers’ PTS symptoms differentially predicted children’s general distress (bmothers =0.139; bfathers = 0.147; χ2(1)=0.006, p=0.940). Next, parent–child dyads were split into parent–daughter and parent–son dyad groups and the same steps were repeated. This model, too, was fully saturated (df=0) when all parameters were free to vary across the two groups and presented no evidence that parents’ PTS symptoms differentially predicted daughters’ vs. sons’ general distress (bdaughters =0.117; bsons =0.174; χ2(1)=0.515, p=0.473). Thus, there is no evidence that parents’ or children’s genders moderate the spillover effect from parents’ PTS symptoms to children’s general distress.
Possible Alternative Spillover Model
We examined whether there may be an alternative spillover effect within parent–child dyads such that general distress spills over to PTS symptoms. According to the model χ2 statistics (df=0), this model was just-identified and therefore fit indices cannot be compared to those of the baseline APIM. However, the alternative model did not yield spillover effects for parents or children (ps>0.05) and compared to the baseline APIM, it explained slightly less of the variance in mental health for children (R2=24 %) and the same amount of variance in mental health for parents (R2=53 %). On this basis, we did not have reason to utilize this alternative model over the initial baseline APIM.
Discussion
The current study examined the interdependent mental health in 397 parent–child dyads 3 years after a major earthquake that devastated their community. Our data show that, controlling for their individual disaster exposure, parents’ earthquake-related PTS symptoms are significantly associated with their children’s general psychological distress, whereas children’s PTS symptoms are not associated with their parents’ general psychological distress. This provides a stringent test of the relevance and importance of parents’ post-disaster psychological responses for their children’s psychological adjustment. Our findings also suggest that mothers and fathers may have similar spillover effects on their children and that spillover effects from parents are comparable for daughters and sons.
Our study design and analytic approach make important and novel contributions to the existing literature. First, using independent participant self-reports enabled us to overcome biases from parent proxy reports that are often used in studies examining traumatic events involving children. Second, we believe this is the first paper to address the mental health of parents and children as a dyadic phenomenon using the APIM in an SEM framework. This approach allowed us to examine the associations between parents’ and children’s PTS symptoms and each other’s general distress simultaneously in a single statistical model, and it allowed us to compare the effect sizes of these associations. Findings from these statistical strategies support the inclusion of children’s family members in intervention efforts (e.g., cognitive behavioral therapy; Cohen and Mannarino 1996) for treating symptoms of distress following trauma, especially in dyads similar to those in this study in which parents’ mental health is repeatedly challenged from exposure to recurrent stressors (i.e., repeated natural disasters). Third, it is noteworthy that the spillover effects remained, even when controlling for parents’ and children’s degree of exposure to the earthquake, suggesting that dyadic approaches are pertinent to understanding post-disaster psychological adjustment among disaster survivors with a range of exposures. Finally, an ethnically and demographically homogenous sample is advantageous for the internal reliability of our findings, and a study of parent–child dyads from Indonesia adds to the paucity of research in underdeveloped countries. We encourage increased efforts to explore psychological health in such populations, especially as they are noted to experience (on average) more severe consequences as a result of natural disasters (Norris et al. 2002).
Although the current study’s data cannot identify the mechanisms for the observed spillover effects from parents to children, preliminary evidence from other research can provide some insight. For instance, parents’ PTS-related psychological and behavioral symptoms may reduce positive interactions within parent–child dyads (Foster et al. 2007), which may exacerbate children’s general distress. Also, PTS symptoms in parents may hinder their ability to provide adequate care to their children (Masten et al. 1990) during a time when they most need it (Salmon and Bryant 2002). Attachment Theory (Bowlby 1988) also suggests that parents’ PTS symptoms may prevent their children from feeling emotionally connected to them, leaving children to feel unsafe, insecure, and distressed. Of course, children may vary in their susceptibility to parents’ mental health and care-giving quality depending on their age, as older children may be more independent. Future studies should explore these and other plausible pathways (i.e., parenting qualities, specific aspects of parent–child attachment) for the observed spillover effects in children at different stages of development.
As observed in previous research (Levine et al. 2005), we did not see a mental health spillover effect from children to their parents. Perhaps post-disaster obligations (e.g., rebuilding the community and home environment, re-establishing the family’s resources; Kaniasty 2011; Sattler et al. 2002) limit parents’ exposure or attentiveness to their children’s adjustment difficulties. It is also possible that the lack of spillover effect from children to parents is a consequence of the restricted variance in children’s PTS scores; future research should seek to replicate these findings. Nevertheless, despite the lack of spillover from children to parents, our statistical model explains a large amount of variance in parents’ general distress. In fact, we were able to account for almost twice as much of the variance in parents’ mental health as in their children’s. This may be due to the significantly higher levels of PTS symptoms in parents versus children, as well as a significantly stronger association between PTS and general distress in parents than in children. Overall, our findings corroborate a large corpus of literature highlighting parental mental functioning as a key contributor to overall familial function during and after disasters (Kaniasty 2011; Rowe et al. 2010).
A few limitations warrant discussion. First, families were not surveyed until 3 years after the disaster and we do not have information about their early responses to the earthquake and its aftermath. Nevertheless, the results demonstrate persistent psychological remnants of natural disasters among children as well as adults, especially when their physical environment continues to show vivid reminders of an earthquake’s devastation. The significant associations between PTS and general distress are consistent with data collected on teachers within the same region (Seyle et al. 2013) and support prior research showing psychological impairment among disaster survivors past the immediate post-disaster period (Bonanno et al. 2010; Felix et al. 2011; Weems et al. 2010); these findings suggest that post-disaster recovery services should extend beyond the initial disaster recovery period (Kilmer and Gil-Rivas 2010a). Second, our sample included relatively few fathers. Therefore, we were unable to examine whether gender (mis)match (e.g., male child/female caregiver vs. female child/male caregiver) played a role in spillover effects. Prior research suggests that there may be a gender matching effect within parent–child dyads that might moderate their interdependent mental health (Russell and Saebel 1997), which should be tested with larger samples. Third, as our data were correlational, causal inferences are not possible. It is possible that children’s general distress may add to parents’ PTS symptoms; however, our supplemental analyses provided little evidence for a spillover effect in this direction (i.e., from general distress to PTS symptoms). The proposed directionality in our APIM is also supported by evidence that PTS fosters or exacerbates additional psychological distress (Copeland et al. 2007; Goenjian et al. 2001; Laor et al. 1997). Of note, there may be a shared genetic vulnerability to stressful or traumatic events that may partially account for the observed spillover effects (see Leen-Feldner et al. 2013); this is an important topic for future research. Finally, as participants in this study consisted of families from a rural region in Indonesia, the generalizability of our findings may be limited as parent–child relationships and interactions can vary across cultures (French et al. 2001). Nonetheless, child-rearing can be just as variable within cultures (Stevenson-Hinde 1998) and other factors such as socioeconomic status (Zevalkink and Riksen-Walraven 2001) may be more important than culture.
Clinical Implications
Findings from the present study support research highlighting the family unit as a promising social milieu in which to focus intervention efforts for adults and children (Birmes et al. 2009; Rowe et al. 2010; Weems and Overstreet 2008). The spillover effects from parents’ PTS symptoms to children’s general distress suggest that clinical treatments may be enhanced by utilizing broader family-based approaches as strengthened connections in proximal social contexts may facilitate children’s adaptation following natural disasters (La Greca et al. 2009). Notably, children’s post-disaster mental health may be influenced or exacerbated by other familial factors such as maltreatment and violence (Becker-Blease et al. 2010; Curtis et al. 2000; Mohammad et al. 2015). As relief efforts reach out to families following disasters, this may provide opportunities to identify children in need of help managing their psychological symptoms, as well as protection from unsafe homes. In families that are unable to provide a safe environment for children, other means of intervention should be considered (cf., Cutter and Finch 2008).
Moreover, our findings suggest that fathers and mothers may be equally important targets of intervention for the mental health of young female and male disaster survivors. Nonetheless, given that mothers typically serve as children’s primary caregiver (Collins and Russell 1991), they may be particularly important for ensuring children’s adjustment following trauma. These findings also support prior work showing that a positive relationship with a competent adult (Masten et al. 1990) and positive coping advice from caregivers (Kilmer and Gil-Rivas 2010b) help children adjust to disasters. However, our effect size comparisons indicated that parents’ trauma-related responses are not as strongly associated with children’s general distress as children’s own trauma-related responses. As such, children may still benefit from treatments and interventions tailored to their unique disaster experiences and psychological distress (Dorsey et al. 2011). Lastly, the link between PTS symptoms and general distress within parents and children suggests that post-disaster psychological screening should include more than PTS symptomatology as comorbidity with other psychological problems (e.g., depression, anxiety, or somatization) is probable.
Conclusion
Overall, this study supports prior theoretical and empirical work emphasizing the importance of social systems in understanding post-disaster adjustment. It builds on the current literature by demonstrating the unique yet interrelated experiences of children and parents following a shared trauma, and presents evidence that parents and children may be considered as a social unit in the context of both research and clinical work. A dyadic approach to understanding post-disaster mental health in families can help researchers identify—and mental health care providers treat—the most influential sources of distress that might hinder parents’ and children’s adjustment following a major disaster.
Acknowledgments
This project was designed, developed and funded by Psychology Beyond Borders, Austin, Texas. Vanessa Juth was supported by a T32 award [UL1 RR031985] from the Institute of Clinical and Translational Science at the University of California, Irvine, which was made possible through a grant [UL1 TR000153] from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
We thank Toula Skiadas from Psychology Beyond Borders for her invaluable assistance throughout this project and the research team from Universitas Sanata Dharma who assisted with data collection, including Elisabeth Haksi Mayawati, Santa Evelin Sitepu, Krisna Novian Prabandaru, Sasmito Adi Singowidjojo, Agung Sudarmanto, Nines Resiska Sukmawati, Ignatius Krisna Susantyo, and Oktavia Zamharin.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
- Appleyard K, Osofsky JD. Parenting after trauma: supporting parents and caregivers in the treatment of children impacted by violence. Infant Mental Health Journal. 2003;24:111–125. doi: 10.1002/imhj.10050. [DOI] [Google Scholar]
- Becker-Blease KA, Turner HA, Finkelhor D. Disasters, victimization, and children’s mental health. Child Development. 2010;81:1040–1052. doi: 10.1111/j.1467-8624.2010.01453.x. [DOI] [PubMed] [Google Scholar]
- Birmes P, Raynaud JP, Daubisse L, Brunet A, Arbus C, Klein R, Allenou C, Hazane F, Grandjean H, Schmitt L. Children’s enduring PTSD symptoms are related to their family’s adaptability and cohesion. Community Mental Health Journal. 2009;45:290–299. doi: 10.1007/s10597-008-9166-3. [DOI] [PubMed] [Google Scholar]
- Bolton P, Tang AM. Using ethnographic methods in the selection of post-disaster mental-health interventions. Prehospital and Disaster Medicine. 2004;19:97–101. doi: 10.1017/S1049023X00001540. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Brewin CR, Kaniasty K, La Greca AM. Weighing the costs of disaster: consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest. 2010;11:1–49. doi: 10.1177/1529100610387086. [DOI] [PubMed] [Google Scholar]
- Bowlby J. A secure base: Parent–child attachment and healthy human development. New York: Basic Books; 1988. [Google Scholar]
- Brody LR. Gender differences in emotional development: a review of theories and research. Journal of Personality. 1985;53:102–149. doi: 10.1111/j.1467-6494.1985.tb00361.x. [DOI] [Google Scholar]
- Bronfenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Charuvastra A, Cloitre M. Social bonds and posttraumatic stress disorder. Annual Review of Psychology. 2008;59:301–328. doi: 10.1146/annurev.psych.58.110405.085650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. A treatment outcome study for sexually abused preschool children: initial findings. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:42–50. doi: 10.1097/00004583-199601000-00011. [DOI] [PubMed] [Google Scholar]
- Collins W, Russell G. Mother-child and father-child relationships in middle adolescence: a developmental analysis. Developmental Review. 1991;11:99–136. doi: 10.1016/0273-2297(91)90004-8. [DOI] [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Costa NM, Weems CF, Pellerin K, Dalton R. Parenting stress and childhood psychopathology: an examination of specificity to internalizing and externalizing symptoms. Journal of Psychopathology and Behavioral Assessment. 2006;28:113–122. doi: 10.1007/s10862-006-7489-3. [DOI] [Google Scholar]
- Cox MJ, Paley B. Understanding families as systems. Current Directions in Psychological Science. 2003;12:193–196. doi: 10.1111/1467-8721.01259. [DOI] [Google Scholar]
- Curtis T, Miller BC, Berry EH. Changes in reports and incidence of child abuse following natural disasters. Child Abuse & Neglect. 2000;24:1151–1162. doi: 10.1016/S0145-2134(00)00176-9. [DOI] [PubMed] [Google Scholar]
- Cutter SL, Finch C. Temporal and spatial changes in social vulnerability to natural hazards. Proceedings of the National Academy of Sciences of the United States of America. 2008;105:2301–2306. doi: 10.1073/pnas.0710375105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deater-Deckard K. Parenting stress. New Haven, CT: Yale University Press; 2004. [Google Scholar]
- Derogatis LR. Brief Symptom Inventory-18. Administration, scoring, and procedures manual. Minneapolis, MN: NCS Assessments; 2001. [Google Scholar]
- Dorsey S, Briggs EC, Woods BA. Cognitive behavioral treatment for posttraumatic stress disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America. 2011;20:255–269. doi: 10.1016/j.chc.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felix E, Hernández LA, Bravo M, Ramirez R, Cabiya J, Canino G. Natural disaster and risk of psychiatric disorders in Puerto Rican children. Journal of Abnormal Child Psychology. 2011;39:589–600. doi: 10.1007/s10802-010-9483-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster CJE, Garber J, Durlak JA. Current and past maternal depression, maternal interaction behaviors, and children’s externalizing and internalizing symptoms. Journal of Abnormal Child Psychology. 2007;35:1021–1033. doi: 10.1007/s10802-007-9197-1. [DOI] [PubMed] [Google Scholar]
- French DC, Rianasari M, Pidada S, Nelwan P, Buhrmester D. Social support of Indonesian and U.S. children and adolescents by family members and friends. Merrill-Palmer Quarterly. 2001;47:377–394. doi: 10.1353/mpq.2001.0015. [DOI] [Google Scholar]
- Furr JM, Comer JS, Edmunds JM, Kendall PC. Disasters and youth: a meta-analytic examination of posttraumatic stress. Journal of Consulting and Clinical Psychology. 2010;78:765–780. doi: 10.1037/a0021482. [DOI] [PubMed] [Google Scholar]
- Gil-Rivas V, Holman EA, Silver RC. Adolescent vulnerability following the September 11th terrorist attacks: a study of parents and their children. Applied Developmental Science. 2004;8:130–142. doi: 10.1207/s1532480xads0803_3. [DOI] [Google Scholar]
- Gil-Rivas V, Kilmer RP, Hypes AW, Roof KA. The caregiver-child relationship and children’s adjustment post-Hurricane Katrina. In: Kilmer RP, Gil-Rivas V, Tedeschi RG, Calhoun LG, editors. Helping families and communities recover from disaster: Lessons learned from Hurricane Katrina and its aftermath. Washington, DC: American Psychological Association; 2010. pp. 55–76. [Google Scholar]
- Goenjian AK, Molina L, Steinberg AM, Fairbanks LA, Alvarez ML, Goenjian HA, Pynoos RS. Posttraumatic stress and depressive reactions among Nicaraguan adolescents after Hurricane Mitch. American Journal of Psychiatry. 2001;158:788–794. doi: 10.1176/appi.ajp.158.5.788. [DOI] [PubMed] [Google Scholar]
- Hafstad GS, Gil-Rivas V, Kilmer RP, Raeder S. Parental adjustment, family functioning, and posttraumatic growth among Norwegian children and adolescents following a natural disaster. American Journal of Orthopsychiatry. 2010;80:248–257. doi: 10.1111/j.1939-0025.2010.01028.x. [DOI] [PubMed] [Google Scholar]
- Hamblen J, Barnett E. PTSD in children and adolescents: A National Center for PTSD fact sheet. 2009 RetrievedNovember 5 2012, from http://www.ncptsd.va.gov/ncmain/ncdocs/fact_shts/fs_children.html.
- Hosley CA, Montemayor R. Fathers and adolescents. In: Lamb ME, editor. The role of the father in child development. 3. Hoboken, NJ: Wiley; 1997. pp. 162–178. [Google Scholar]
- Juth V, Silver RC, Sender L. The shared experience of adolescent and young adult cancer patients and their caregivers. Psycho-Oncology. 2015 doi: 10.1002/pon.3785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaniasty K. Parental crucibles: Families coping with disaster. In: Buchwald P, Moore K, Ringeisen T, editors. Stress and anxiety: Application to education and health. Berlin, Germany: Logos Verlag; 2011. pp. 83–93. [Google Scholar]
- Kelley ML, Self-Brown S, Le B, Bosson JV, Hernandez BC, Gordon AT. Predicting posttraumatic stress symptoms in children following Hurricane Katrina: a prospective analysis of the effect of parental distress and parenting practices. Journal of Traumatic Stress. 2010;23:582–590. doi: 10.1002/jts.20573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA. Models of nonindependence in dyadic research. Journal of Social and Personal Relationships. 1996;13:279–294. doi: 10.1177/0265407596132007. [DOI] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York, NY: Guilford Press; 2006. [Google Scholar]
- Kilic EZ, Özgüven HD, Sayil I. The psychological effects of parental mental health on children experiencing disaster: the experience of Bolu earthquake in Turkey. Family Process. 2003;42:485–495. doi: 10.1111/j.1545-5300.2003.00485.x. [DOI] [PubMed] [Google Scholar]
- Kilmer RP, Gil-Rivas V. Responding to the needs of children and families after a disaster: linkages between unmet needs and caregiver functioning. American Journal of Orthopsychiatry. 2010a;80:135–142. doi: 10.1111/j.1939-0025.2010.01016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer RP, Gil-Rivas V. Exploring posttraumatic growth in children impacted by Hurricane Katrina: correlates of the phenomenon and developmental considerations. Child Development. 2010b;81:1211–1227. doi: 10.1111/j.1467-8624.2010.01463.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Lai B, Jaccard J. Hurricane-related exposure experiences and stressors, other life events, and social support: concurrent and prospective impact on children’s persistent posttraumatic stress symptoms. Journal of Consulting and Clinical Psychology. 2010;78:794–805. doi: 10.1037/a0020775. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Lochman JE. Moving beyond efficacy and effectiveness in child and adolescent intervention research. Journal of Consulting and Clinical Psychology. 2009;77:373–382. doi: 10.1037/a0015954. [DOI] [PubMed] [Google Scholar]
- Lambert JE, Holzer J, Hasbun A. Association between parents’ PTSD severity and children’s psychological distress: a meta-analysis. Journal of Traumatic Stress. 2014;27:9–17. doi: 10.1002/jts.21891. [DOI] [PubMed] [Google Scholar]
- Laor N, Wolmer L, Mayes LC, Gerson A, Weizman R, Cohen DJ. Israeli preschoolers under Scuds: a thirty-month follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:349–356. doi: 10.1097/00004583-199703000-00013. [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Feldner MT, Knapp A, Bunaciu L, Blumenthal H, Amstadter AB. Offspring psychological and biological correlates of parental posttraumatic stress: review of the literature and research agenda. Clinical Psychology Review. 2013;33:1106–113. doi: 10.1016/j.cpr.2013.09.001. [DOI] [PubMed] [Google Scholar]
- Levine LJ, Whalen CK, Henker B, Jamner JD. Looking back on September 11, 2001: appraised impact and memory for emotions in adolescents and adults. Journal of Adolescent Research. 2005;20:497–523. doi: 10.1177/0743558405274893. [DOI] [Google Scholar]
- Li X, Huang X, Tan H, Liu A, Zhou J, Yang T. A study on the relationship between posttraumatic stress disorder in flood victim parents and children in Hunan, China. Australian and New Zealand Journal of Psychiatry. 2010;44:543–550. doi: 10.3109/00048671003601400. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York, NY: Wiley; 1987. [Google Scholar]
- Masten AS, Best KM, Garmezy N. Resilience and development: contributions from the study of children who overcome adversity. Development and Psychopathology. 1990;2:425–444. doi: 10.1017/S0954579400005812. [DOI] [Google Scholar]
- Masten AS, Narayan AJ. Child development in the context of disaster, war and terrorism: pathways of risk and resilience. Annual Review of Psychology. 2012;63:227–257. doi: 10.1146/annurev-psych-120710-100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell B. Translation and cultural adaptation of the survey instruments. In: Martin MO, Kelly DL, editors. Third International Mathematics and Science Study (TIMSS) technical report, Volume I: Design and development. Chestnut Hill, MA: Boston College; 1996. [Google Scholar]
- Mohammad WT, Shapiro ER, Wainwright LD, Carter AS. Impacts of family and community violence exposure on child coping and mental health. Journal of Abnormal Child Psychology. 2015;43:203–215. doi: 10.1007/s10802-014-9889-2. [DOI] [PubMed] [Google Scholar]
- Montemayor R, Brownlee JR. Fathers, mothers, and adolescents: gender-based differences in parental roles during adolescence. Journal of Youth and Adolescence. 1987;16:281–291. doi: 10.1007/BF02139095. [DOI] [PubMed] [Google Scholar]
- Morris A, Gabert-Quillen C, Delahanty D. The association between parent PTSD/depression symptoms and child PTSD symptoms: a meta-analysis. Journal of Pediatric Psychology. 2012;37:1076–1088. doi: 10.1093/jpepsy/jss091. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2011. [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: part I. an empirical review of the empirical literature, 1981–2001. Psychiatry: Interpersonal and Biological Processes. 2002;65:207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- Polusny MA, Ries BJ, Meis LA, DeGarmo D, McCormick-Deaton CM, Thuras P, Erbes CR. Effects of parents’ experiential avoidance and PTSD on adolescent disaster-related posttraumatic stress symptomatology. Journal of Family Psychology. 2011;25:220–229. doi: 10.1037/a0022945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe CL, La Greca AM, Alexandersson A. Family and individual factors associated with substance involvement and PTS symptoms among adolescents in greater New Orleans after Hurricane Katrina. Journal of Consulting and Clinical Psychology. 2010;78:806–817. doi: 10.1037/a0020808. [DOI] [PubMed] [Google Scholar]
- Russell A, Saebel J. Mother-son, mother-daughter, father-son, and father-daughter: are they distinct relationships? Developmental Review. 1997;17:111–147. doi: 10.1006/drev.1996.0431. [DOI] [Google Scholar]
- Salmon K, Bryant RA. Posttraumatic stress disorder in children: the influence of developmental factors. Clinical Psychology Review. 2002;22:163–188. doi: 10.1016/S0272-7358(01)00086-1. [DOI] [PubMed] [Google Scholar]
- Sattler DN, Preston AJ, Kaiser CF, Olivera VE, Valdez J, Schlueter S. Hurricane Georges: a cross-national study examining preparedness, resource loss, and psychological distress in the U.S. Virgin Islands, Puerto Rico, Dominican Republic, and the United States. Journal of Traumatic Stress. 2002;15:339–350. doi: 10.1023/A:1020138022300. [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH. Reconsideration of harm’s way: onsets and comorbidity patterns of disorders in preschool children and their caregivers following Hurricane Katrina. Journal of Clinical Child and Adolescent Psychology. 2008;37:508–518. doi: 10.1080/15374410802148178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwerdtfeger KL, Geoff BN. Intergenerational transmission of trauma: exploring mother-infant prenatal attachment. Journal of Traumatic Stress. 2007;20:39–51. doi: 10.1002/jts.20179. [DOI] [PubMed] [Google Scholar]
- Seyle DC, Widyatmoko CS, Silver RC. Coping with natural disasters in Yogyakarta, Indonesia: a study of elementary school teachers. School Psychology International. 2013;34:387–404. doi: 10.1177/0143034312446889. [DOI] [Google Scholar]
- Silverman WK, La Greca AM. Children experiencing disasters: Definitions, reactions, and predictors of outcomes. In: La Greca AM, Silverman WK, Vernberg WM, Roberts MC, editors. Helping children cope with disasters and terrorism. Washington, DC: American Psychological Association; 2002. pp. 11–33. [DOI] [Google Scholar]
- Smith P, Perrin S, Yule W, Rabe-Hasketh S. War exposure and maternal reactions in the psychological adjustment of children from Bosnia-Hercegovina. Journal of Child Psychology and Psychiatry. 2001;42:395–404. doi: 10.1017/S0021963001007065. [DOI] [PubMed] [Google Scholar]
- Spell AW, Kelley ML, Wang J, Self-Brown S, Davidson KL, Pellegrin A, Palcic JL, Meyer K, Paasch V, Baumeister A. The moderating effects of maternal psychopathology on children’s adjustment post-Hurricane Katrina. Journal of Clinical Child and Adolescent Psychology. 2008;37:553–563. doi: 10.1080/15374410802148210. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles Post-traumatic stress disorder reaction index. Current Psychiatry Reports. 2004;6:96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Stevenson-Hinde J. Parenting in different cultures: time to focus. Developmental Psychology. 1998;34:698–700. doi: 10.1037/0012-1649.34.4.698. [DOI] [PubMed] [Google Scholar]
- U.S. Department of the Interior. US Geological Survey: Earthquake Hazards Maps and Data: Magnitude 6.3 - Java, Indonesia, 2006 May 26, 22:53:58. UTC; 2010. Retrieved from http://earthquake.usgs.gov/earthquakes/recenteqsww/Quakes/usneb6.php#summary. [Google Scholar]
- Weathers FW, Huska JA, Keane TM. PCL-C for DSM-IV. Boston, MA: National Center for PTSD-Behavioral Science Division; 1991. [Google Scholar]
- Weems CF, Overstreet S. Child and adolescent mental health research in the context of Hurricane Katrina: an ecological-needs-based perspective and introduction to the Special Section. Journal of Clinical Child and Adolescent Psychology. 2008;37:487–494. doi: 10.1080/15374410802148251. [DOI] [PubMed] [Google Scholar]
- Weems CF, Taylor LK, Cannon MF, Marino RC, Romano DM, Scott BG, Perry AM, Triplett V. Post traumatic stress, context, and the lingering effects of the Hurricane Katrina disaster among ethnic minority youth. Journal of Abnormal Child Psychology. 2010;38:49–56. doi: 10.1007/s10802-009-9352-y. [DOI] [PubMed] [Google Scholar]
- Weitzman M, Rosenthal DG, Liu YH. Paternal depressive symptoms and child behavioral or emotional problems in the United States. Pediatrics. 2011;128:1126–1134. doi: 10.1542/peds.2010-3034. [DOI] [PubMed] [Google Scholar]
- Westermeyer J. On the epidemicity of amok violence. Archives of General Psychiatry. 1973;28:873–876. doi: 10.1001/archpsyc.1973.01750360085012. [DOI] [PubMed] [Google Scholar]
- Wickrama K, Kaspar V. Family context of mental health risk in tsunami-exposed adolescents: findings from a pilot study in Sri Lanka. Social Science & Medicine. 2007;64:713–723. doi: 10.1016/j.socscimed.2006.09.031. [DOI] [PubMed] [Google Scholar]
- Widyatmoko CS, Tan ET, Seyle DC, Mayawati EH, Silver RC. Coping with natural disasters in Yogyakarta, Indonesia: the psychological state of elementary school children as assessed by their teachers. School Psychology International. 2011;32:484–497. doi: 10.1177/0143034311402919. [DOI] [Google Scholar]
- Zevalkink J, Riksen-Walraven JM. Parenting in Indonesia: inter- and intracultural differences in mothers’ interactions with their young children. International Journal of Behavioral Development. 2001;25:167–175. doi: 10.1080/01650250042000113. [DOI] [Google Scholar]