Abstract
IMPORTANCE
Abusive head trauma (AHT) is a serious condition, with an incidence of approximately 30 cases per 100 000 person-years in the first year of life.
OBJECTIVE
To assess the effectiveness of a statewide universal AHT prevention program.
DESIGN, SETTING, AND PARTICIPANTS
In total, 88.29% of parents of newborns (n = 405 060) in North Carolina received the intervention (June 1, 2009, to September 30, 2012). A comparison of preintervention and postintervention was performed using nurse advice line telephone calls regarding infant crying (January 1, 2005, to December 31, 2010). A difference-in-difference analysis compared AHT rates in the prevention program state with those of other states before and after the implementation of the program (January 1, 2000, to December 31, 2011).
INTERVENTION
The Period of PURPLE Crying intervention, developed by the National Center on Shaken Baby Syndrome, was delivered by nurse-provided education, a DVD, and a booklet, with reinforcement by primary care practices and a media campaign.
MAIN OUTCOMES AND MEASURES
Changes in proportions of telephone calls for crying concerns to a nurse advice line and in AHT rates per 100 000 infants after the intervention (June 1, 2009, to September 30, 2011) in the first year of life using hospital discharge data for January 1, 2000, to December 31, 2011.
RESULTS
In the 2 years after implementation of the intervention, parental telephone calls to the nurse advice line for crying declined by 20%for children younger than 3 months (rate ratio, 0.80; 95%CI, 0.73–0.87; P < .001) and by 12%for children 3 to 12 months old (rate ratio, 0.88; 95%CI, 0.78–0.99; P = .03). No reduction in state-level AHT rates was observed, with mean rates of 34.01 person-years before the intervention and 36.04 person-years after the intervention. A difference-in-difference analysis from January 1, 2000, to December 31, 2011, controlling for economic indicators, indicated that the intervention did not have a statistically significant effect on AHT rates (β coefficient, −1.42; 95%CI, −13.31 to 10.45).
CONCLUSIONS AND RELEVANCE
The Period of PURPLE Crying intervention was associated with a reduction in telephone calls to a nurse advice line. The study found no reduction in AHT rates over time in North Carolina relative to other states. Consequently, while this observational study was feasible and supported the program effectiveness in part, further programmatic efforts and evaluation are needed to demonstrate an effect on AHT rates.
Abusive head trauma (AHT), also known as shaken baby syndrome, is a rare but severe form of child maltreatment. Incidence studies1–3 in the United States and abroad have reported AHT rates ranging from24.0to29.7 cases per 100 000 person-years in the first year of life. Shaken baby syndrome was characterized in 1972 as a pattern of injuries marked by subdural hematomas, long-bone fractures, and retinal hemorrhages, with few signs of external injury.4 The consequences of AHT are severe. One-fourth of maltreated children die, and long-term neurological, developmental, and cognitive sequelae are the norm.1,5–8 Financial costs are enormous. Medical costs alone attributable to AHT in the 4 years after diagnosis average approximately $48 000 per affected child.9
In previous studies, AHT prevention education has been shown to increase awareness and understanding by parents. Specifically, AHT education increases parental knowledge of infant crying, the most significant trigger for AHT.10 In a survey of 7051 women who had received AHT education, 96% recommended continuing the program, and 98% reported that it was helpful in a posttest analysis.11 In addition, parents can be taught to share information about AHT prevention with other caregivers.12,13 However, to our knowledge, research on the effect of universal AHT prevention programs on AHT rates has been limited. Two previous studies14,15 of AHT using preintervention and postintervention designs reported significant effects of an intervention. Using a case-control design, a third study16 reported that a reduction in AHT was associated with a control exposure (routine newborn education) rather than AHT prevention education.
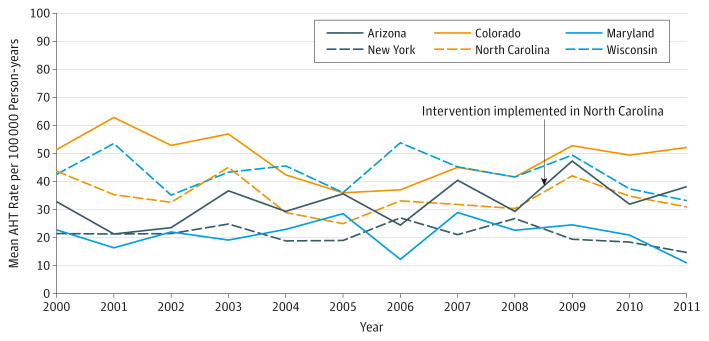
This article describes a universal AHT prevention program delivered to 405 060 parents of newborns in North Carolina. The intervention, the Period of PURPLE Crying, teaches parents about normal infant crying and the dangers of shaking. The educational materials for this program had been previously evaluated in Vancouver, British Columbia, Canada (delivered by visiting home nurses) and in Seattle, Washington (delivered at prenatal classes, maternity wards, and pediatric office practice visits to compare the 3 settings for delivery).12,13 No differences in discernible knowledge level were observed as a result of the use of the educational materials among the 3 settings in Seattle.13 The Period of PURPLE Crying has the following 2 goals: (1) to support caregivers in their understanding of early increased crying in infancy and (2) to reduce the incidence of AHT. To assess caregiver support behaviorally, we examined changes in the number of telephone calls to an after-hours nurse advice line for infant crying before and after implementation of the intervention. To assess whether there was a reduction in AHT cases, we performed a difference-in-difference analysis of AHT rates over time in North Carolina and 5 comparison states (New York, Arizona, Colorado, Wisconsin, and Maryland). Based on a previous study,15 we hypothesized that the Period of PURPLE Crying intervention would reduce AHT by 50% from a previously determined baseline and that no such decrease would be seen in the comparison states.
At a Glance.
The objective was to study the effectiveness of a statewide abusive head trauma prevention program (the Period of PURPLE Crying, developed by the National Center on Shaken Baby Syndrome).
Parental telephone calls to a nurse advice line for crying in children younger than 3 months declined by 20%(P < .001).
No reduction in North Carolina’s state-level abusive head trauma rate was observed. A difference-in-difference analysis from January 1, 2000, to December 31, 2011, controlling for economic indicators, indicated that the intervention did not have a statistically significant effect on abusive head trauma rates (β coefficient, −1.42; 95%CI, −13.31 to 10.45).
Methods
Intervention
The Period of PURPLE Crying is a proprietary, research-based intervention developed by the National Center on Shaken Baby Syndrome. The program materials include a DVD and a booklet that are given to new parents before hospital discharge. The program focuses on healthy infant crying, the dangers of shaking, and the importance of sharing information with other caretakers. It is based on more than 50 years of research on the characteristics of crying in healthy infants and describes the typical crying peak during the second month of life, the presence of unsoothable crying, and the danger of crying as a stimulus for caregiver frustration and shaking.10
The program was conceived as a 3-dose delivery of the intervention. Dose 1 was a North Carolina statewide universal intervention that included all parents of newborns receiving 3 minutes of education by a nurse, reading the booklet, and watching the video before hospital discharge. Parents received copies of the materials for later review and sharing with other caretakers. The implementation process required recruiting hospitals, signing of a memorandum of understanding, training at least80%of staff, and going live with an event. Each hospital had a volunteer program coordinator, nurses, or other staff who delivered the intervention after receiving standardized training (in-person or online). Dose 2 was a reinforcing message delivered in most primary care medical offices during visits in the first month of life. Dose 2 was not universal because of the large number of primary care practices and the project budget limitations. Dose 3 was a media campaign that included paid radio commercials in 3 of 6 large media markets in the state. Details of the intervention, hospital training, evaluation, and media campaign have been reported elsewhere.17–20 In 2007, two North Carolina hospitals served as pilot sites to test the processes of enrollment and implementation. Statewide implementation occurred over 18 months. Hospital recruitment began January 2, 2008, with 80% of North Carolina hospitals implementing the intervention by January 1, 2009, and 100% by June 1, 2009. In total, 88.29% of parents of newborns (n = 405 060) born June 1, 2009, to September 30, 2012, received the Period of PURPLE Crying intervention. Dose 2 was implemented in January 2, 2010, with ongoing message reinforcement efforts in primary care settings throughout the project period. Dose 3 was implemented January 1 to September 30, 2009, but a sustained media campaign effort was possible for only 9 months because of budget limitations. All study procedures were approved by the University of North Carolina Committee on Human Subjects Research.
Nurse Advice Line Telephone Calls
Data from an after-hours nurse advice line provided by University of North Carolina hospitals that triages telephone calls from physicians’ offices statewide (68 practices) were analyzed to assess changes in telephone call rates for advice about crying. These data were not collected for study purposes but rather were for a secondary analysis of reasons for calling for after-hours nurse or medical advice. This assessment was for telephone calls about crying not likely to be associated with illness. The nurse advice line is a proprietary service, and participating practices pay for the service. The practices are distributed across North Carolina but are not assumed to be representative of the state. The practices changed little over the study period although the total volume of telephone calls grew modestly. Therefore, a preintervention and postintervention comparison is valid even if the results are not generalizable to parents or practices outside of the sample. The number of children served by the practices is not known by the agency providing the service. All telephone calls to nurses were logged by the advising nurse and coded by subject matter, child age, and physician office. We obtained data for yearly total telephone calls from January 1, 2006, to December 31, 2010. We calculated the proportion of crying-related telephone calls in children younger than 3 months and in children between 3 months and 12 months old. Telephone calls were coded conservatively as calls regarding “crying” if no other symptoms were mentioned, consistent with our interest in parental behavior related to the response to a crying infant when no other symptoms of disease were present. We compared the proportions of these telephone calls about crying for the 3 years before vs the 2 years after implementation of the intervention by calculating a rate ratio.
Difference-in-Difference Model
A difference-in-difference analysis was performed to evaluate the effects of the intervention on AHT rates and to control for possible effects of an economic recession on AHT rates.21 An interrupted time series of AHT rates in North Carolina was compared with a time series in states without the intervention using ordinary least squares regression analysis.
State inpatient databases were purchased from the Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality, for North Carolina and 5 other states. The comparison states (New York, Arizona, Colorado, Wisconsin, and Maryland) were chosen after consultation with the National Center on Shaken Baby Syndrome to identify states with little or no use of the Period of PURPLE Crying among local prevention efforts. These states were chosen from 14 states with complete hospital discharge data available at lowcost. We identified states (among the 14with available data) having the fewest hospitals ordering the Period of PURPLE Crying materials for hospital-based programs. These 5 states had 3 to 8 hospitals implementing the intervention. In the difference-indifference analysis, the relevant measure is the state-level AHT rate. Child maltreatment prevention programs implemented before the intervention herein should not affect the results. For example, before and during the study period, New York State had a widespread universal AHT prevention program, with some characteristics similar to those of our program. However, that program was implemented well before the present study period and should not have contributed to a change in AHT rates during the study period. To assess the appropriateness of the comparison states, we examined their AHT rates before and after the study period. There is no obvious benefit in choosing states demographically similar to North Carolina in this type of analysis because the relevant issue is the preintervention trend in AHT rates over time.
A previously established International Classification of Diseases, Ninth Revision, coding algorithm was used to calculate yearly state-level AHT rates in children younger than 1 year.2,22 Given that the intervention herein was implemented during the most significant economic recession (December 2007 to June 2009) since the GreatDepression,23 we used midyear unemployment rates (http://www.bls.gov/lau/#tables) and mortgage foreclosure data (http://www.corelogic.com) as economic control data in the event that the recession may have differentially affected AHT rates in some states. The mortgage foreclosure rate is the number of mortgages in foreclosure divided by the total number of mortgages in a year. We also included controls for year and state indicators.
Results
Nurse Advice Line Telephone Calls
From January 1, 2006, to December 31, 2010, an average of 19 013 (range, 13 868–21 200) yearly after-hours calls were received by the nurse advice line about children younger than 1 year. For the 3 years before implementation of the intervention, 4% of telephone calls regarding children 3 to 12 months old and 7%of telephone calls regarding children younger than 3monthswere for crying. In the 2 years after implementation of the intervention, parental telephone calls to the nurse advice line for crying declined by20%for children younger than 3months (rate ratio, 0.80; 95%CI, 0.73–0.87; P < .001) and by 12% for children 3 to 12 months old (rate ratio, 0.88; 95% CI, 0.78–0.99; P = .03). After the intervention, a smaller proportion of telephone calls to the nurse advice line were for crying, without other reported symptoms.
Difference-in-Difference Analysis
Abusive head trauma rates in North Carolina calculated from hospital discharge data ranged from25.0 to 44.9 per 100 000 person-years between January 1,2000, and December 31, 2011. The year-to-year variation in annual AHT rates in North Carolina and the comparison states is shown in the Figure. Inspection of the data indicates that state AHT rates varied widely from year to year because AHT is rare. Overall, there was no obvious trend in AHT rates among the comparison states. North Carolina had mean AHT rates of 34.01 per 100 000 person-years before the intervention and 36.04 per 100 000 person-years after the intervention for children younger than 1 year. The comparison states had mean AHT rates of 33.22 per 100 000 person-years before the intervention and 33.41 per 100 000 person-years after the intervention for children younger than 1 year. The adjusted difference-in-difference analysis indicated that the intervention did not have a statistically significant effect on AHT rates (P = .81). In the Table, the β coefficient of interest is the difference-in-difference coefficient in the adjusted model.
Figure.
State-Level Abusive Head Trauma (AHT) Rates for Children Younger Than 1 Year in North Carolina and 5 Comparison States
Based on hospital discharge data, January 1, 2000, to December 31, 2011.
Table.
Difference-in-Difference Analysis of the Effect of the Period of PURPLE Crying Intervention (Developed by the National Center on Shaken Baby Syndrome) on AHT Rates in North Carolina Compared With Those of Other States, January 1, 2000, to December 31, 2011, Based on 72 Observationsa
| Variable | Difference in Difference (95% CI) | |
|---|---|---|
| Unadjusted | Adjusted | |
| Difference in difference | 1.84 (−16.05 to 19.73) | −1.42 (−13.31 to 10.45) |
| Mortgage foreclosure rate | NA | −0.94 (−5.54 to 3.66) |
| Unemployment rate | NA | 1.98 (−1.94 to 5.91) |
Abbreviations: AHT, abusive head trauma; NA, not applicable.
β coefficient and 95%CIs are reported. Adjusted model controls for state and year indicators, 90-day foreclosure rates, and unemployment rates.
Discussion
After implementation of the Period of PURPLE Crying intervention, the number of telephone calls to a nurse advice line, especially those regarding infants younger than 3months, significantly declined. However, no reduction in state-level AHT rates was identified using a difference-in-difference analysis to compare AHT rates in North Carolina with AHT rates in 5 selected comparison states over time, controlling for 2 economic indicators.
This study has several strengths and limitations. Strengths include that a large-scale AHT prevention project was successfully delivered with a high degree of fidelity to parents of approximately 88% of the newborns in North Carolina over a 4-year period.20 The setting was a large state, resulting in many cases with which to estimate reliable AHT rates. The use of an econometric difference-in-difference analysis to better estimate the effects compared with nonintervention control states is an important method to consider for the field of child maltreatment prevention research.
Limitations include that the study was a preintervention and postintervention design and not a randomized clinical trial. Randomized clinical trials may not be feasible when evaluating statewide or universal interventions, especially for rare illnesses. Although the distribution of the intervention program was high, with approximately88%of parents of newborns in North Carolina receiving the AHT prevention education, it is unknown whether those not exposed to the intervention were at highest risk for AHT. Furthermore, we were not able to examine whether perpetrators of AHT were exposed to the program. Although 27%of parents reported showing the DVD and 32% reported showing the booklet to someone else after hospital discharge,20 we cannot know with certainty that the program reached caregivers who were not present at the hospital. The comparison states were chosen based on expert opinion and knowledge of the use of this program in potential states, as well as the low cost of data sets. Regional or local prevention efforts may have been implemented and not known to us. The primary outcome, AHT rates, is based on administrative claims data. Claims may be subject to regional and temporal variation because they are intended primarily to support billing and not for research or surveillance. However, the use of claims data for AHT research has been empirically validated with death certificate data and shown to have high sensitivity and specificity compared with data abstracted from medical records.24–26
Although this study, to our knowledge, represents the largest intervention investigation of an AHT prevention program with a comprehensive evaluation to date, the sample size was limited in 2ways. First, the study was powered to showa50% reduction in AHT cases from January 1, 2001, to December 31, 2002, baseline period based on a previous trial of a different prevention program that reported a 47%reduction in the AHT rate.15 That degree reduction may have been ambitious. Second, the difference-in-difference analysis used each state’s yearly AHT rate as an observation. Therefore, the full model included only 72 observations, which limited the analytic power. Furthermore, only 3 years of data were available after implementation of the intervention in North Carolina, representing an important power limitation. These trends should be reexamined when more years of data become available.
In contrast to the results of 2 previous studies14,15 regarding a different universal AHT prevention program, our primary outcome failed to support the hypothesized decrease in AHT rates for children younger than 1 year. Findings are often not replicated from intervention trials, especially when using nonrandomized designs.27 In the present study, the intervention and AHT data collection occurred during an economic recession, which has previously been associated with increases in AHT.28–31 We used a difference-in-difference analysis to assess the effect of the intervention over time, controlling for the economic indicators of state-level unemployment and mortgage foreclosure rates. The latter variable was associated with a change in AHT rates in one of 2 analyses in which it was assessed.30,31 However, it is uncertain whether these or other economic indicators that we did not include in our model are most appropriate. The variables we used represented state level economic conditions in a given year, which may have masked considerable heterogeneity in the effect of the economic recession within the states.
The Period of PURPLE Crying intervention program may have other important benefits. It has been shown to increase parents’ knowledge about infant crying and their sharing of this information with other caregivers.12,13 In addition, most hospitals in this study reported their likelihood to continue using the program once the materials were no longer provided through the research study because of its simplicity, quality, and ease of use and implementation.20 In another jurisdiction, the program was associated with a 29.5% reduction in emergency department visits for crying not associated with physical disease.32 Other positive outcomes of the program, such as reduced parental stress or frustration, are as yet unreported and may hold promise.
Given the high economic, societal, and familial costs of AHT, efforts should continue to develop and rigorously test preventive interventions. The use of targeted populations or more intensive prevention efforts may be more effective. For example, AHT education might be included in visiting home nurse programs directed to those at highest risk with or without universal education. Child abuse preventionists should consider policy options that create a context more supportive of parenting, such as those that support income stability and high-quality early care and education.33
Conclusions
This study is an important contribution to the growing body of literature on AHT and child abuse prevention programs. Our analyses found an association of the Period of PURPLE Crying intervention with a reduction in telephone calls to a nurse advice line. However, the study failed to demonstrate a decrease in state-level AHT rates. It may be that the intervention was ineffective, the study was underpowered, the follow-up was too brief, or a decrease in cases may have been obscured by unmeasured confounding. Future research should use the most robust methods available to establish a causal relationship between prevention programs and AHT.
Acknowledgments
Funding/Support: This study was supported by cooperative agreement 5U49CE001275-04 from the National Center for Injury Prevention and Control of the Centers for Disease Control and Prevention, by grant 153970 from The Duke Endowment, and by grant 2007039 from the Doris Duke Charitable Foundation.
Footnotes
Conflict of Interest Disclosures: The National Center on Shaken Baby Syndrome (NCSBS) and Dr R. G. Barr jointly registered the trademark for the Period of PURPLE Crying. Graham Consulting Ltd consults and provides grants for child abuse prevention and child development programs. It owns the royalties that are aminor share of the net profits from the sale of the Period of PURPLE Crying program. Dr R. G. Barr and Ms M. Barr sit as 2 members of the uncompensated board of directors. Ms M. Barr was the former executive director of the NCSBS, a 501(c)(3) nonprofit organization. Both are uncompensated members of the international advisory board of the NCSBS. No other disclosures were reported.
Additional Contributions: We thank CoreLogic (http://www.corelogic.com) for the generous use of its data in this project. We express our gratitude for the advice from this project’s statewide leadership team and for the assistance of the hospital study coordinators and volunteer implementation project coordinators.
Author Contributions: Drs Zolotor and Runyan had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Zolotor, Runyan, Shanahan, Durrance, Sullivan, Klevens, Murphy, M. Barr, R. G. Barr.
Acquisition, analysis, or interpretation of data: Zolotor, Runyan, Shanahan, Durrance, Nocera, M. Barr, R. G. Barr.
Drafting of the manuscript: Zolotor, Runyan, Durrance, Sullivan, M. Barr, R. G. Barr.
Critical revision of the manuscript for important intellectual content: Zolotor, Shanahan, Durrance, Nocera, Klevens, Murphy, M. Barr, R. G. Barr.
Statistical analysis: Zolotor, Shanahan, Durrance.
Obtained funding: Zolotor, Runyan, Sullivan, Klevens, Murphy, M. Barr, R. G. Barr.
Administrative, technical, or material support: Zolotor, Runyan, Shanahan, Nocera, Murphy, M. Barr, R. G. Barr.
Study supervision: Zolotor, Runyan, Klevens, M. Barr, R. G. Barr.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. This study was approved by the agency of Dr Klevens, a scientific officer at the Centers for Disease Control and Prevention, but they made no substantive recommendations or requested any changes.
References
- 1.Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH. A population-based study of inflicted traumatic brain injury in young children. JAMA. 2003;290(5):621–626. doi: 10.1001/jama.290.5.621. [DOI] [PubMed] [Google Scholar]
- 2.Shanahan ME, Zolotor AJ, Parrish JW, Barr RG, Runyan DK. National, regional, and state abusive head trauma: application of the CDC algorithm. Pediatrics. 2013;132(6):e1546–e1553. doi: 10.1542/peds.2013-2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barlow KM, Minns RA. Annual incidence of shaken impact syndrome in young children. Lancet. 2000;356(9241):1571–1572. doi: 10.1016/S0140-6736(00)03130-5. [DOI] [PubMed] [Google Scholar]
- 4.Caffey J. On the theory and practice of shaking infants: its potential residual effects of permanent brain damage and mental retardation. Am J Dis Child. 1972;124(2):161–169. doi: 10.1001/archpedi.1972.02110140011001. [DOI] [PubMed] [Google Scholar]
- 5.Duhaime AC, Christian C, Moss E, Seidl T. Long-term outcome in infants with the shaking-impact syndrome. Pediatr Neurosurg. 1996;24(6):292–298. doi: 10.1159/000121058. [DOI] [PubMed] [Google Scholar]
- 6.Gessner RR, Runyan DK. The shaken infant: amilitary connection? Arch Pediatr Adolesc Med. 1995;149(4):467–469. doi: 10.1001/archpedi.1995.02170160121024. [DOI] [PubMed] [Google Scholar]
- 7.Keenan HT, Hooper SR, Wetherington CE, Nocera M, Runyan DK. Neurodevelopmental consequences of early traumatic brain injury in 3-year-old children. Pediatrics. 2007;119(3):e616–e623. doi: 10.1542/peds.2006-2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.King WJ, MacKay M, Sirnick A Canadian Shaken Baby Study Group. Shaken baby syndrome in Canada: clinical characteristics and outcomes of hospital cases. CMAJ. 2003;168(2):155–159. [PMC free article] [PubMed] [Google Scholar]
- 9.Peterson C, Xu L, Florence C, et al. The medical cost of abusive head trauma in the United States. Pediatrics. 2014;134(1):91–99. doi: 10.1542/peds.2014-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barr RG. Preventing abusive head trauma resulting from a failure of normal interaction between infants and their caregivers. Proc Natl Acad Sci U S A. 2012;109(suppl 2):17294–17301. doi: 10.1073/pnas.1121267109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deyo G, Skybo T, Carroll A. Secondary analysis of the “Love Me...Never ShakeMe” SBS education program. Child Abuse Negl. 2008;32(11):1017–1025. doi: 10.1016/j.chiabu.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Barr RG, Barr M, Fujiwara T, Conway J, Catherine N, Brant R. Do educational materials change knowledge and behaviour about crying and shaken baby syndrome? a randomized controlled trial. CMAJ. 2009;180(7):727–733. doi: 10.1503/cmaj.081419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barr RG, Rivara FP, Barr M, et al. Effectiveness of educational materials designed to change knowledge and behaviors regarding crying and shaken-baby syndrome in mothers of newborns: a randomized, controlled trial. Pediatrics. 2009;123(3):972–980. doi: 10.1542/peds.2008-0908. [DOI] [PubMed] [Google Scholar]
- 14.Altman RL, Canter J, Patrick PA, Daley N, Butt NK, Brand DA. Parent education by maternity nurses and prevention of abusive head trauma. Pediatrics. 2011;128(5):e1164–e1172. doi: 10.1542/peds.2010-3260. [DOI] [PubMed] [Google Scholar]
- 15.Dias MS, Smith K, DeGuehery K, Mazur P, Li V, Shaffer ML. Preventing abusive head trauma among infants and young children: a hospital-based, parent education program. Pediatrics. 2005;115(4):e470–e477. doi: 10.1542/peds.2004-1896. [DOI] [PubMed] [Google Scholar]
- 16.Keenan HT, Leventhal JM. A case-control study to evaluate Utah’s shaken baby prevention program. Acad Pediatr. 2010;10(6):389–394. doi: 10.1016/j.acap.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 17.Hennink-Kaminski HJ, Dougall EK. Tailoring hospital education materials for the Period of PURPLE Crying: Keeping Babies Safe in North Carolina media campaign. Soc Marketing Q. 2009;15(4):49–64. [Google Scholar]
- 18.Runyan D, Zolotor A. The Period of PURPLE Crying: Keeping Babies Safe in North Carolina. In: Dodge KA, Coleman DL, editors. Preventing Child Maltreatment. New York, NY: Guilford Press; 2009. [Google Scholar]
- 19.Runyan DK, Hennink-Kaminski HJ, Zolotor AJ, et al. Designing and testing a shaken baby syndrome prevention program: the Period of PURPLE Crying: Keeping Babies Safe in North Carolina. Soc Marketing Q. 2009;15(4):2–24. [Google Scholar]
- 20.Shanahan M, Fleming P, Nocera M, Sullivan K, Murphy R, Zolotor A. Process evaluation of a statewide abusive head trauma prevention program. Eval Program Plann. 2014;47:18–25. doi: 10.1016/j.evalprogplan.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 21.Cameron AC, Trivedi PK. Microeconomics. Cambridge, England: Cambridge University Press; 2005. pp. 55–57.pp. 768–770. [Google Scholar]
- 22.Parks SE, Annest JL, Hill HA, Karch DL. Pediatric Abusive Head Trauma: Recommended Definitions for Public Health Surveillance and Research. Atlanta, GA: Division of Violence Prevention, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 23.US Bureau of Labor Statistics. [Accessed March 28, 2015];The recession of 2007–2009. http://www.census.gov/history/pdf/greatrecession-bls.pdf. Published February 2012.
- 24.Berger RP, Parks S, Fromkin J, Rubin P, Pecora PJ. Assessing the accuracy of the International Classification of Diseases codes to identify abusive head trauma: a feasibility study. Inj Prev. 2015;21(e1):e133–e137. doi: 10.1136/injuryprev-2013-040924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hooft AM, Asnes AG, Livingston N, et al. The accuracy of ICD codes: identifying physical abuse in 4 children’s hospitals. Acad Pediatr. 2015;15(4):444–450. doi: 10.1016/j.acap.2015.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parks SE, Kegler SR, Annest JL, Mercy JA. Characteristics of fatal abusive head trauma among children in the USA: 2003–2007: an application of the CDC operational case definition to national vital statistics data. Inj Prev. 2012;18(3):193–199. doi: 10.1136/injuryprev-2011-040128. [DOI] [PubMed] [Google Scholar]
- 27.Ioannidis JP. Contradicted and initially stronger effects in highly cited clinical research. JAMA. 2005;294(2):218–228. doi: 10.1001/jama.294.2.218. [DOI] [PubMed] [Google Scholar]
- 28.Berger RP, Fromkin JB, Stutz H, et al. Abusive head trauma during a time of increased unemployment: a multicenter analysis. Pediatrics. 2011;128(4):637–643. doi: 10.1542/peds.2010-2185. [DOI] [PubMed] [Google Scholar]
- 29.Huang MI, O’Riordan MA, Fitzenrider E, McDavid L, Cohen AR, Robinson S. Increased incidence of nonaccidental head trauma in infants associated with the economic recession. J Neurosurg Pediatr. 2011;8(2):171–176. doi: 10.3171/2011.5.PEDS1139. [DOI] [PubMed] [Google Scholar]
- 30.Wood JN, Medina SP, Feudtner C, et al. Local macroeconomic trends and hospital admissions for child abuse, 2000–2009. Pediatrics. 2012;130(2):e358–e364. doi: 10.1542/peds.2011-3755. [DOI] [PubMed] [Google Scholar]
- 31.Wood JN, French B, Fromkin J, et al. Association of pediatric abusive head trauma rates with macroeconomic indicators [published online July 13, 2015] Acad Pediatr. doi: 10.1016/j.acap.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 32.Barr RG, Rajabali F, Aragon M, Colbourne M, Brant R. Education about crying in normal infants is associated with a reduction in pediatric emergency room visits for crying complaints. J Dev Behav Pediatr. 2015;36(4):252–257. doi: 10.1097/DBP.0000000000000156. [DOI] [PubMed] [Google Scholar]
- 33.Klevens J, Barnett SB, Florence C, Moore D. Exploring policies for the reduction of child physical abuse and neglect. Child Abuse Negl. 2015;40:1–11. doi: 10.1016/j.chiabu.2014.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]