Abstract
Matrix Metalloproteinase-2 (Mmp2) is a collagenase known to be important in the development of renal fibrosis. In unilateral ureteral obstruction (UUO) the obstructed kidney (OK) develops fibrosis, while the contralateral (CL) does not. In this study we investigated the effect of UUO on gene expression, fibrosis and pelvic remodeling in the kidneys of Mmp2 deficient mice (Mmp2-/-), heterozygous animals (Mmp2+/-) and wild-type mice (Mmp2+/+). Sham operated animals served as controls (Cntrl). UUO was prepared under isoflurane anaesthesia, and the animals were sacrificed after one week. UUO caused hydronephrosis, dilation of renal tubules, loss of parenchymal thickness, and fibrosis. Damage was most severe in Mmp2+/+ mice, while both Mmp2-/- and Mmp2+/- groups showed considerably milder hydronephrosis, no tubular necrosis, and less tubular dilation. Picrosirius red quantification of fibrous collagen showed 1.63±0.25% positivity in OK and 0.29±0.11% in CL (p<0.05) of Mmp2+/+, Mmp2-/- OK and Mmp2-/- CL exhibited only 0.49±0.09% and 0.23±0.04% (p<0.05) positivity, respectively. Mmp2+/- OK and Mmp2+/- CL showed 0.43±0.09% and 0.22±0.06% (p<0.05) positivity, respectively. Transcriptomic analysis showed that 26 genes (out of 48 examined) were differentially expressed by ANOVA (p<0.05). 25 genes were upregulated in Mmp2+/+ OK compared to Mmp2+/+ CL: Adamts1, -2, Col1a1, -2, -3a1, -4a1, -5a1, -5a2, Dcn, Fbln1, -5, Fmod, Fn1, Itga2, Loxl1, Mgp, Mmp2, -3, Nid1, Pdgfb, Spp1, Tgfb1, Timp2, Trf, Vim. In Mmp2-/- and Mmp2+/- 18 and 12 genes were expressed differentially between OK and CL, respectively. Only Mmp2 was differentially regulated when comparing Mmp2-/- OK and Mmp2+/- OK. Under stress, it appears that Mmp2+/- OK responds with less Mmp2 upregulation than Mmp2+/+ OK, suggesting that there is a threshold level of Mmp2 necessary for damage and fibrosis to occur. In conclusion, reduced Mmp2 expression during UUO protects mice against hydronephrosis and renal fibrosis.
Introduction
Obstructive nephropathy is a common cause of kidney damage and renal insufficiency, both in congenital obstructive nephropathy in children [1], and acquired obstruction caused by kidney stones, malignancies and benign prostate hyperplasia [2]. In rodents unilateral ureteral obstruction (UUO) is a well-studied model that leads to hydronephrosis with tubular dilation, cortical atrophy and fibrosis. UUO is interesting both as a model of ureteral obstruction, and for studying the fibrotic process as such [3]. The development and degree of fibrosis is considered to be one of the most reliable prognostic markers for loss of kidney function and progression towards end stage renal disease (ESRD) [4].
Matrix Metalloproteinase-2 (Mmp2), also known as gelatinase-A, is a 72 kDa collagenase that is important in extracellular matrix metabolism. Mmp2 cleaves type IV collagen, and degrades already denatured collagens [5]. In the kidney, Mmp2 is upregulated in several pathological states [6–9]. Inhibition of Mmp2 activity results in disparate outcomes depending on the phase of kidney disease studied and on the underlying cause [10,11]. For example, it has been shown that Mmp2 facilitates fibrosis by participating in epithelial to mesenchymal transition [12]. Mmp2 has also been found to be involved in tubular repair after acute kidney injury (AKI) [13], and Mmp2 deficiency protects against ischemia-reperfusion AKI [14].
Mmp2 knockout mice (Mmp2-/-) do not show major anatomical abnormalities, but are born smaller and grow more slowly than the wild type (Mmp2+/+), suggesting that Mmp2 is important for fetal development and growth [15]. Knockout of the Mmp2 gene occurs in exon 1, resulting in no Mmp2 expression neither at the RNA nor the protein level [15]. The Mmp2-/- mice show reduced angiogenic response in oxygen-induced retinopathy [16], and are more susceptible to diabetic nephropathy [17]. However, they are protected against haemorrhagic transformation during the early stages of cerebral ischemia and reperfusion [18].
Since UUO damage is closely connected to the remodeling of the renal pelvis and the deformation of the kidney parenchyma, we hypothesized that Mmp2-deficiency would protect the obstructed kidney (OK). However, a recent study of pharmacological inhibition in the UUO model showed increased fibrosis, while cellular infiltration was decreased [19]. The aim of the present study was to investigate the effect of homozygous and heterozygous genetic inactivation of Mmp2 on gene expression, fibrosis and pelvic remodeling in the kidneys of mice after one week of UUO.
The fibrotic process was investigated in knockout animals (Mmp2-/-), heterozygotes (Mmp2+/-) and wild-type C57Black6J (Mmp2+/+) mice. In addition, sham operated individuals from each group served as controls (Cntrl-/-, Cntrl+/-, Cntrl+/+). The genes selected for investigation in this study were chosen due to their involvement in fibrosis and renal damage.
Materials and Methods
Animals
Mmp2 deficient C57BL/6J mice were generously provided by Dr. Werb [15] at Inserm UMR 702, Université Pierre et Marie Curie, Paris, and later transferred to Bergen for use in the present project. The animals were kept and bred at the animal facility at the Department of Biomedicine in Bergen. The study consisted of 6 groups; Mmp2+/+ Control (Cntrl+/+) (n = 10) and UUO (n = 10), Mmp2+/- Control (Cntrl+/-) (n = 10) and UUO (n = 11), and Mmp2-/- Control (Cntrl-/-) (n = 10) and UUO (n = 9) (Table 1). The control groups were sham operated.
Table 1. Bodyweight and age of the mice at the start of the experiment.
| Mmp2+/+ | Mmp2+/- | Mmp2-/- | ||||
|---|---|---|---|---|---|---|
| Control | UUO | Control | UUO | Control | UUO | |
| n = | 10 | 10 | 10 | 11 | 10 | 9 |
| Bodyweight (g) | 31±0.4 | 23±0.3 | 35±1 | 38±2 | 29±2 | 29±2 |
| Age (weeks) | 14±0 | 9±0 | 19±1 | 37±2 | 20±2 | 41±6 |
Ethics Statement
The experiments were conducted in accordance with the guidelines of, and with approval obtained from the Norwegian State Board for Biological Experiments with Living Animals (Approval No: 2009–1899). All surgery was carried out under isoflurane anaesthesia.
Ureteral obstruction
UUO was prepared under isoflurane anaesthesia. The left ureter was identified through a subcostal incision, and obstructed using a silk ligature at the level of the lower pole of the kidney. The animals were sacrificed under isoflurane anaesthesia one week after obstruction. The abdominal aorta was dissected and cannulated in order to perfuse the animal with ice-cold PBS before the kidneys were removed. The kidneys were cut in transverse slices that were either stabilised in RNA-later, or fixed in 4% formaldehyde, processed and embedded in paraffin.
Histology
Morphological damage was investigated by light microscopy using 3 μm sections, stained with Periodic Acid-Schiff (PAS). In order to monitor the amount of collagen in the different experimental groups, 7 μm sections were stained with Picrosirius Red and examined according to our previously published protocol [9]. Briefly, digital images were captured randomly under constant polarized light in a Leica DMLB microscope connected to a CCD ColorView IIIu camera. Image acquisition and analysis was performed using CellD version 2.4. Intensity was separated as a gray-scale image from the HSI colour-space. The detection threshold was the same for all images. Collagen content was expressed as percent positive pixels of total pixels.
Quantitative RTPCR
RNA was extracted from the kidneys using an RNeasy mini kit (Qiagen, West Sussex, UK) as described in the protocol provided by the manufacturer, and cDNA was synthesised from RNA using Reverse Transcriptase Core Kit obtained from Eurogentec (Seraing, Belgium). A custom-made Low Density Array (LDA) from Applied Biosystems was used to determine the mRNA expression levels of a selection of genes. The method is based on the well-established quantitative RT-PCR (QRT-PCR) technique, however, LDA has the benefit of enabling quantification of several genes simultaneously and at the same time maintaining the sensitivity of QRT-PCR [20]. 18s ribosomal RNA was used as a standard. In addition Gapdh, Tbp, Pgk1 and Ppia were used as housekeeping genes.
Statistical analysis
Data is presented as means ± standard error of the mean (SEM), except for comparison of the expression of individual genes where the fold-change is used. The probability of chance difference was tested using ANOVA, with Fisher’s test and à priori contrasts to test individual comparisons. Comparisons between CL and OK were paired. The Bonferroni correction was used for gene-expression data, separately across samples and across genes for each comparison made. P < 0.05 was accepted as statistically significant.
Results
Kidney damage in UUO
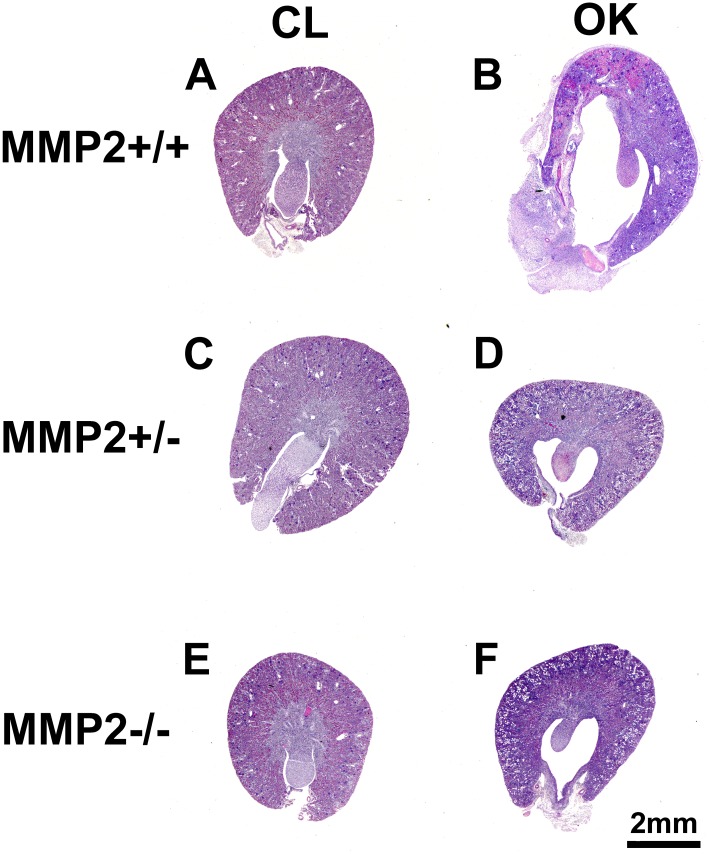
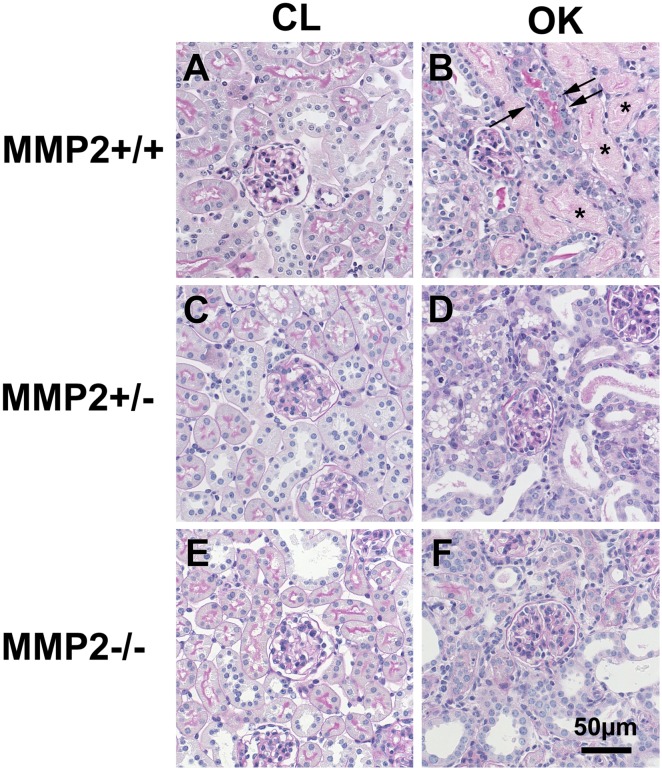
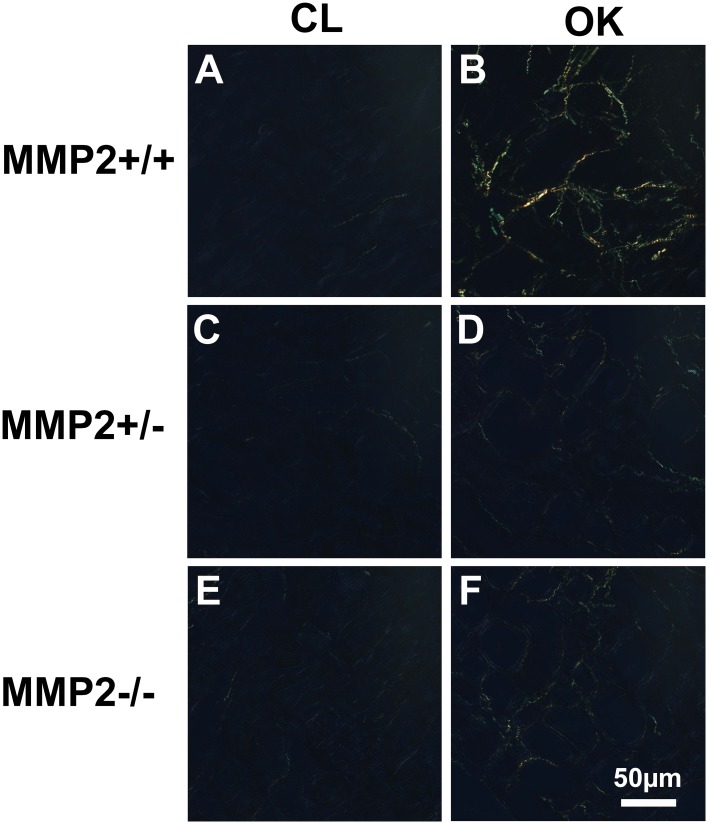
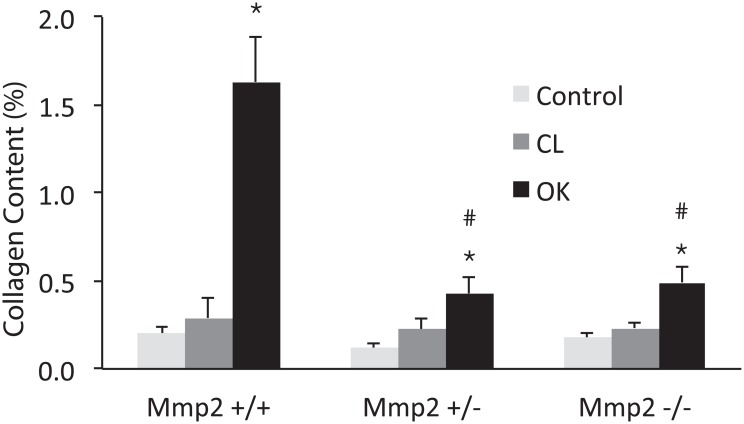
A total of 60 mice were used in the UUO experiment (Table 1). UUO caused severe hydronephrosis in Mmp2+/+, which was accompanied by tubular dilation, necrosis and atrophy, while Mmp2-/- and Mmp2+/- showed considerably milder hydronephrosis, no tubular necrosis, and less tubular dilation (Figs 1 and 2). Automatic image analysis of collagen content in Picrosirius Red stained sections showed 1.63±0.25% positivity in OK and 0.29±0.11% in CL (p<<0.05) of Mmp2+/+, whereas Mmp2-/- OK and Mmp2-/- CL only showed 0.49±0.09% and 0.23±0.04% (p<0.05) positivity, respectively, and Mmp2+/- OK and Mmp2+/- CL exhibited 0.43±0.09% and 0.22±0.06% (p<0.05) positivity, respectively (Figs 3 and 4). There were no significant discrepancies between the levels of fibrosis in the control kidneys and the CL kidneys in any of the groups.
Fig 1. Representative images of Period Acid-Schiff (PAS) stained transversal sections showing increased morphological damage in the Mmp2+/+ obstructed kidney (OK, 1B) compared to the other groups (1 D, F).
The Mmp2+/+ OK (1B) shows severe hydronephrosis and inflammation of the renal pelvis, while the Mmp2-/- OK (1F) and Mmp2+/- OK (1D) only display slight dilatation and minimal inflammation. The contralateral kidneys (CL, 1 A, C, E) do not differ from each other and show normal morphology.
Fig 2. Morphological damage in the obstructed kidney (OK, 2B, D, F) compared to the contralateral kidney (CL, 2 A, C, E).
All OK kidneys show tubular dilatation, flattened tubular epithelium with loss of brush border and reactive nuclear enlargement. Only Mmp2+/+ OK (2B) shows necrotic tubules (asterix) and many apoptotic cells (arrows). The morphology of the CL kidney is normal. (PAS stain).
Fig 3. Representative images of Picrosirius Red stained sections under polarised light from the obstructed kidney (OK, 3 B, D, F) compared to the contralateral kidney (CL, 3 A, C, E).
There is a higher level of collagen in Mmp2+/+ OK (3 B) compared to OK in both Mmp2+/- and Mmp2-/- (3 D, F). Only minimal levels of collagen are detected in CL kidneys across all groups (3 A, C, E).
Fig 4. Image analysis of collagen in Picrosirius Red stained sections under polarised light.
Collagen content is expressed as the percent of positive pixels to all pixels. * denotes P<0.05 compared to the contralateral kidney (CL). # denotes P<0.05 compared to OK in Mmp2+/+.
Gene expression
Using RTPCR, 26 out of 48 genes examined showed differential expression when ANOVA was applied across groups (Table 2). None of the housekeeping genes showed significant changes, and the results were comparable when using the different genes for normalisation. Data are presented using 18S as standard. There was no difference in gene expression between CL and control kidneys in any of the groups.
Table 2. Differential gene expression between strains (Mmp2 +/+, +/-, and -/-), and as paired comparisons between the obstructed (OK) and contralateral kidneys (CL) of the same animal.
| Gene | Average | OK-/- | OK-/- | OK+/- | OK-/- | CL-/- | OK+/- | CL+/- | OK+/+ | CL+/+ | Cntrl-/- | Cntrl-/- | Cntrl+/- |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CT-value | vs | vs | vs | vs | vs | vs | vs | vs | vs | vs | vs | vs | |
| ± SEM | OK+/+ | OK+/- | OK+/+ | CL-/- | Cntrl-/- | CL+/- | Cntrl+/- | CL+/+ | Cntrl+/+ | Cntrl+/+ | Cntrl+/- | Cntrl+/+ | |
| Mmp2 † | 33.05 ± 0.28 | -7.060 * | -5.774 * | -1.287 * | -0.907 | 0.704 | 3.973 * | -0.345 | 4.079 * | 0.455 | -2.323 * | -1.942 * | -0.381 |
| Adamts2 † | 31.06 ± 0.22 | -0.666 | 0.479 | -1.146 * | 2.748 * | 0.532 | 3.122 * | 0.247 | 3.867 * | 0.033 | -0.046 | 0.569 | -0.615 |
| Dcn † | 28.22 ± 0.18 | -0.533 | 0.534 | -1.067 * | 1.774 * | 0.914 | 1.269 | 0.801 | 3.078 * | -0.567 | -0.710 | -0.084 | -0.626 |
| Mgp † | 24.65 ± 0.32 | 0.829 | 0.421 | 0.408 | 2.853 * | 1.599 | 3.673 * | 0.420 | 3.555 * | -0.152 | -0.219 | 0.062 | -0.280 |
| Adamts1 † | 29.84 ± 0.24 | 0.726 | 0.435 | 0.291 | 3.840 * | -0.241 | 3.591 * | -0.626 | 2.463 * | -0.012 | -0.423 | -0.199 | -0.224 |
| Spp1 † | 23.72 ± 0.28 | 0.870 | 0.483 | 0.387 | 3.409 * | 1.432 | 4.996 * | -0.538 | 3.337 * | 0.887 | 0.255 | 0.100 | 0.154 |
| Col4a1 † | 25.82 ± 0.16 | -0.187 | 0.340 | -0.527 | 2.463 * | 0.071 | 0.977 | 1.208 | 2.160 * | 0.349 | -0.212 | -0.009 | -0.203 |
| Fn1 † | 29.61 ± 0.25 | -0.782 | 0.149 | -0.930 | 1.713 | 1.742 | 4.074 * | -0.643 | 4.371 * | 0.295 | 0.429 | 0.125 | 0.304 |
| Col1a2 † | 26.48 ± 0.23 | -0.845 | 0.475 | -1.320 | 3.921 * | -0.011 | 3.598 * | -0.133 | 4.415 * | 0.123 | -0.217 | 0.029 | -0.246 |
| Vim † | 27.38 ± 0.17 | -0.369 | 0.403 | -0.772 | 2.109 * | 0.633 | 1.032 | 1.342 | 3.098 * | 0.065 | 0.051 | 0.034 | 0.016 |
| Nid1 † | 29.28 ± 0.15 | -0.358 | 0.132 | -0.490 | 1.578 * | 0.620 | 1.296 * | 0.774 | 1.898 * | 0.764 | 0.106 | 0.004 | 0.103 |
| Mmp3 † | 32.99 ± 0.29 | 0.052 | 0.600 | -0.548 | 4.706 * | 0.870 | 4.741 * | -0.138 | 4.228 * | 0.029 | -1.267 | -0.374 | -0.893 |
| Trf † | 30.29 ± 0.23 | 0.461 | 0.530 | -0.069 | 1.550 * | 0.221 | 1.201 | 0.656 | 2.591 * | 0.025 | 1.305 | 0.616 | 0.689 |
| Col3a1 † | 28.04 ± 0.31 | -0.610 | 0.958 | -1.568 | 5.332 * | 0.239 | 4.743 * | -0.003 | 5.177 * | 0.561 | -0.444 | 0.126 | -0.570 |
| Col1a1 † | 29.56 ± 0.21 | -0.953 | 0.671 | -1.624 | 4.894 * | 0.349 | 4.655 * | -0.306 | 4.914 * | 0.534 | -0.747 | -0.223 | -0.524 |
| Loxl1 † | 29.77 ± 0.18 | -0.088 | 0.172 | -0.261 | 1.518 | 1.255 | 1.147 | 1.518 | 2.978 * | -0.067 | 0.049 | 0.064 | -0.014 |
| Tgfb1 † | 28.97 ± 0.16 | 0.316 | 0.329 | -0.014 | 2.336 * | 0.309 | 0.983 | 1.514 | 2.450 * | -0.003 | 0.118 | 0.181 | -0.063 |
| Col5a1 † | 32.47 ± 0.23 | -1.296 | 0.050 | -1.346 | 1.573 | 1.698 | 2.074 * | 1.065 | 3.823 * | 1.038 | 0.293 | -0.082 | 0.376 |
| Pdgfb † | 29.29 ± 0.22 | 0.640 | 0.237 | 0.404 | 1.701 * | 0.897 | 1.189 | 1.077 | 1.682 * | 0.191 | -0.085 | -0.094 | 0.010 |
| Fbln5 † | 28.53 ± 0.14 | -0.462 | -0.029 | -0.433 | 0.824 | 0.238 | 0.905 | -0.134 | 1.575 * | 0.136 | 0.186 | -0.321 | 0.507 |
| Fmod † | 31.42 ± 0.10 | -1.316 * | -0.260 | -1.057 * | 0.309 | 0.057 | 0.768 | -0.384 | 1.217 * | -0.284 | -0.750 | -0.242 | -0.508 |
| Mmp9 † | 34.56 ± 0.24 | 0.568 | 0.864 | -0.296 | 2.160 * | 1.186 | 0.967 | 2.494 | 5.068 | -2.000 | 0.289 | 0.980 | -0.690 |
| Fbln1 † | 30.71 ± 0.17 | 0.374 | 0.763 | -0.389 | 1.666 | 1.588 | 1.223 | 1.119 | 2.411 * | -0.161 | -0.629 | -0.148 | -0.481 |
| Timp2 † | 29.50 ± 0.13 | 0.319 | 0.488 | -0.169 | 1.455 * | 0.797 | 0.952 | 0.885 | 1.424 * | 0.308 | -0.201 | 0.072 | -0.274 |
| Col5a2 † | 30.88 ± 0.18 | -0.571 | 0.346 | -0.917 | 1.280 | 1.092 | 0.856 | 1.236 | 2.922 * | -0.026 | -0.048 | 0.065 | -0.114 |
| Itga2 † | 34.10 ± 0.25 | -0.603 | 0.568 | -1.171 | 3.203 * | 0.285 | 2.148 | -0.567 | 3.516 * | -0.231 | -0.807 | -1.340 | 0.532 |
| Lgals3 | 27.31 ± 0.20 | -0.079 | 0.289 | -0.368 | 1.423 | 0.684 | 0.699 | 1.264 | 2.212 | -0.271 | -0.245 | 0.144 | -0.389 |
| Timp1 | 31.18 ± 0.42 | -0.642 | 0.328 | -0.970 | 3.155 | 4.151 | 3.867 | 3.489 | 7.435 | -0.743 | -1.256 | 0.378 | -1.634 |
| Itgb3 | 33.51 ± 0.22 | -0.273 | 0.262 | -0.534 | 1.860 | 0.322 | 0.406 | 1.516 | 2.377 | 0.911 | 0.833 | 0.002 | 0.831 |
| Pdgfa | 31.10 ± 0.14 | 0.383 | 0.366 | 0.017 | 0.975 | 0.782 | 0.815 | 0.511 | 1.418 | -0.204 | -0.159 | -0.064 | -0.095 |
| Il1b | 32.40 ± 0.19 | -0.147 | 0.259 | -0.406 | 1.526 | 1.701 | 1.332 | 1.269 | 3.335 | -0.494 | -0.533 | -0.368 | -0.166 |
| Pgk1 | 26.20 ± 0.12 | 0.040 | -0.164 | 0.204 | -0.438 | -0.175 | 0.007 | -0.611 | -0.886 | -0.002 | -0.235 | -0.155 | -0.080 |
| Itgav | 27.80 ± 0.19 | 0.081 | -0.048 | 0.129 | 0.953 | 0.236 | 0.942 | 0.410 | 1.513 | -0.128 | 0.277 | 0.115 | 0.162 |
| Vegfa | 27.77 ± 0.08 | -0.238 | -0.073 | -0.165 | -0.459 | -0.148 | -0.196 | -0.469 | -0.769 | 0.295 | -0.104 | -0.131 | 0.027 |
| Gapdh | 22.53 ± 0.21 | -0.034 | -0.031 | -0.003 | -0.162 | -0.205 | 0.033 | -0.434 | -0.439 | -0.202 | -0.308 | -0.065 | -0.243 |
| Vegfc | 32.97 ± 0.11 | 0.159 | 0.458 | -0.299 | 0.649 | 0.427 | 0.557 | -0.275 | 0.766 | -0.072 | -0.224 | -0.337 | 0.113 |
| Nkap | 30.48 ± 0.09 | 0.329 | 0.132 | 0.197 | 0.557 | 0.061 | 0.628 | -0.052 | 0.247 | -0.090 | -0.132 | 0.089 | -0.221 |
| Itga10 | 34.71 ± 0.12 | 0.009 | 0.341 | -0.331 | 0.506 | -0.373 | 0.308 | -0.190 | 1.233 | -0.230 | 0.880 | 0.326 | 0.554 |
| Vegfb | 29.01 ± 0.12 | 0.489 | 0.056 | 0.434 | -0.465 | 0.116 | -0.082 | -0.249 | -0.814 | 0.074 | 0.098 | 0.074 | 0.024 |
| Itga11 | 34.60 ± 0.16 | -0.295 | 0.767 | -1.062 | 1.445 | 0.832 | 1.340 | 0.034 | 2.641 | -0.138 | -0.069 | -0.136 | 0.067 |
| Pdgfc | 30.78 ± 0.11 | 0.203 | 0.140 | 0.063 | -0.036 | -0.123 | 0.309 | -0.418 | -0.412 | 0.191 | 0.140 | 0.190 | -0.049 |
| Tbp | 30.20 ± 0.70 | 0.161 | 0.001 | 0.160 | 0.322 | 0.089 | 0.375 | -0.218 | 0.144 | -0.070 | -0.175 | -0.252 | 0.077 |
| Ppia | 23.73 ± 0.10 | 0.214 | 0.221 | -0.007 | 0.294 | 0.060 | 0.217 | -0.175 | 0.014 | -0.017 | -0.142 | -0.090 | -0.052 |
| Itgb1bp1 | 29.15 ± 0.06 | 0.272 | 0.086 | 0.186 | 0.322 | -0.196 | 0.161 | -0.029 | -0.197 | 0.001 | -0.051 | 0.092 | -0.142 |
| Tff3 | 35.70 ± 0.14 | NA | NA | NA | NA | NA | NA | NA | 0.253 | 0.679 | NA | NA | 1.029 |
| Il1a | 35.93 ± 0.31 | -0.429 | 1.094 | -1.523 | 1.657 | -1.016 | -0.533 | 0.624 | 1.242 | -0.540 | -0.368 | 0.544 | -0.912 |
| Matn1 | 33.92 ± 1.25 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
Cntrl denotes kidneys from control animals without obstruction.
† denotes significant variations between all groups, P<0.05 by ANOVA.
* denotes P<0.05 for the individual comparison.
The greatest difference in gene expressions was seen when comparing the OK and CL in the Mmp2+/+ mice, where 25 genes were significantly altered (Table 2). A comparison of Mmp2-/- OK vs Mmp2-/- CL identified 18 significantly altered genes. Mmp2+/- OK displayed 12 significantly altered genes when compared to Mmp2+/- CL. Cntrl+/- did not differ from Cntrl+/+ in any of the 48 tested genes. After UUO, Mmp2 expression was 7-fold and 5.5-fold induced in Mmp2+/+ OK and Mmp2+/- OK, respectively, when compared to Mmp2-/- OK. Comparisons between Mmp2-/- OK vs Mmp2-/- CL, and Mmp2+/- OK vs Mmp2+/- CL showed that five genes in common did not respond in the same manner as in the Mmp2+/+ OK vs Mmp2+/+ CL comparison. These genes are Loxl1, Fbln5, Fmod, Fbln1 and Col5a2. None of these genes were significantly altered after UUO in Mmp2 -/- and Mmp2+/- mice. In contrast, all five genes were upregulated in Mmp2+/+ mice. Fmod is downregulated in both Mmp2-/- and Mmp2+/- OK groups compared to Mmp2+/+ OK. Mmp9 showed a 2.2-fold upregulation in Mmp2-/- OK when compared to Mmp2-/- CL mice. Only Mmp2 was differentially regulated when comparing Mmp2-/- OK and Mmp2+/- OK. In addition to the housekeeping genes, 17 genes were not differentially expressed between any of the groups.
Discussion
The present study demonstrates that Mmp2-/- and Mmp2+/- mice display less pelvic-remodelling and fibrosis compared to Mmp2+/+ mice after UUO. Both Mmp2-/- and Mmp2+/- mice are protected, which may indicate an important effect of gene-dose. Furthermore, Mmp2+/+ mice displayed more histological damage and showed the highest response in gene expression following UUO, with 25 genes significantly altered when comparing OK to CL. Both Mmp2-/- and Mmp2+/- animals gave a milder response to UUO, showing 18 and 12 significantly altered genes after UUO, respectively. The main findings in this study are similar to those of Du et al., described in a comprehensive paper in which they also reported reduced infiltration of immune cells, and improved immunohistochemistry for a number of collagens and renal injury markers [21]. Our RT-PCR results correlate to those of Du et al with similar expression patterns for Mmp2, Mmp9, Timp1 and Timp2. However, our study presents a wider range of molecular markers, and also data from heterozygotes beyond what has been previously reported.
When comparing the control kidneys between the groups, the lack of Mmp2 does not seem to affect the amount of collagen when the kidney is not under stress (Fig 4). As expected, the level of Mmp2 in both Cntrl+/- and Cntrl+/+ animals is higher relative to the Cntrl-/- group. There is no significant difference in Mmp2 expression between wild type and heterozygotes under control conditions. Mmp2 gene expression in Mmp2+/- mice is not upregulated in OK as much as in the Mmp2+/+ OK. This could suggest that there is a threshold level of Mmp2 necessary for damage and fibrosis to occur and this level might not be reached in the Mmp2+/- mice, thus resulting in protection of the kidneys in Mmp2+/- mice as well. Taken together with the fact that Mmp2 upregulation is required for regulation of several of the genes studied here, this could point towards a cascade effect where a threshold level of Mmp2 is important for initiation of fibrogenesis.
Some of the genes utilised in our study have been investigated previously in similar settings, and could help elucidate the role of Mmp2 after UUO. The effect of pharmacological inhibition of Mmp2 seems to be dependent on the time of administration in UUO-induced renal fibrosis. Late administration of an inhibitor of Mmp2, TISAM, decreased the level of macrophage infiltration, while early administration did not, and contrary to our findings both early and late inhibition of Mmp2 resulted in accelerated fibrosis in the mouse kidney [19]. Inhibition by He4, an Mmp2/Mmp9 inhibitor and a pan-serine protease which has been shown to directly interact with and inhibit Mmp2 and Mmp9, improved the outcome after UUO [22]. He4-inhibition, and thus an increase in Mmp2 and Mmp9 mediated collagen I digestion, resulted in less fibrosis compared to the control group. Taken together, this suggests that genetic deficiency of Mmp2 affects the development of fibrosis by a different mechanism than pharmacological inhibition of Mmp2. This time dependency has also been described in a mouse model of Alport syndrome [10]. Early combination therapy with inhibitors of Mmp2, Mmp3 and Mmp9 significantly delayed the onset of proteinuria, while treatment after onset of proteinuria accelerated renal disease.
In addition, Mmp2 has been shown to affect vascular reactivity. For example endothelin-1 requires cleavage to produce the active hormone and Mmp2 contributes to this process [23]. Mmp2 has also been found to cleave adrenomedullin, resulting in production of a vasoconstrictor peptide [24], and this may be an underlying mechanism that leads to kidney damage [25]. One may suggest that Mmp2 deficiency decreases vasoconstriction and thus reduces kidney damage in UUO.
Mmp9 deficiency seems to have a positive effect during UUO [26], while pharmacological inhibition of Mmp9 has a time-dependent effect, with reduced epithelial to mesenchymal transition and fibrosis at the early or chronic stage, but not during the establishment of fibrosis [11]. The present data show upregulation of Mmp9 in the obstructed kidney in Mmp2-/- mice compared to CL, which may be a compensatory increase due to the lack of Mmp2 [10]. However, Mmp9 was not upregulated after UUO in Mmp2+/- animals, and since both strains showed less damage, it is unlikely that Mmp9 alone is responsible for the decreased fibrosis after UUO.
Decorin (Dcn) deficient mice have been reported to show greater damage than WT after UUO [27]. This could indicate that an upregulation of Dcn is a protective mechanism. However, while the expression of Dcn mRNA was increased after UUO in wild type and knockout mice, there was no effect in heterozygous animals. These results, therefore, do not allow one to draw firm conclusions regarding the potential protective role of Dcn. Timp2 is not differentially expressed between the groups, yet there is an upregulation of Timp2 in the OK kidney compared to the CL kidney in both Mmp2+/+ and Mmp2-/- mice, but not in the Mmp2+/- group. However, we do not have any basis to explain why Mmp2+/- mice regulate Timp2 differently under the stress of UUO. Earlier data showed that Timp2 promotes injury through activating Mmp2 [28]. In both Mmp2-/- and Mmp2+/- animals Timp2 has less Mmp2 to activate, which could be a mechanism behind the reduced rate of fibrosis and remodelling. Thus, even though Timp2 expression in OK and CL in Mmp2-/- and Mmp2+/- mice differ, the limited possibility of an increase in Mmp2 at the level of expression would probably reduce this effect. This may be the reason why they are also protected. In our study, Timp1 was not affected by UUO, and this is supported by evidence that elimination of Timp1 alone was not found to be sufficient in order to alter the severity of fibrosis during UUO [29].
The present results did not show consistent findings in the Pdgf system. This is not entirely surprising since the Pdgf system is important in kidney fibrosis [30] and in UUO [31,32], but it is not necessary for the development of fibrosis in the kidney [33]. There was no differential expression of Pdgfa or Pdgfc. On the other hand Pdgfb was differentially expressed after UUO in Mmp2-/- and Mmp2+/+ mice but not in Mmp2+/- animals. This is difficult to explain, especially since antagonists have a positive effect in several models of renal disease. Pdgfb, however, also plays a role in the repair of cellular damage [34].
Tff3, Vgfa, Vgfb, Vgfc, Il1b and Lgals3 were not differentially expressed in the present study even though they have been implicated in kidney disease. Specifically, Tff3 has been suggested as a diagnostic marker in CKD since it increases in both serum and urine during CKD progression [35]. Vegfs have been demonstrated to slow down the progression of renal injury in experimental models and can be administered in renoprotective therapy [36], but overstimulation can induce glomerular pathology. Il1b is known to stimulate proliferation of human renal fibroblasts as well as production of matrix proteins, while Lhals3 has been shown to protect against fibrosis [37,38].
The clinical treatment of ureteral obstruction is primarily surgical, but as a strategy for limiting the destruction of kidney tissue in progressive or recurring disease, some intervention against Mmp2 may be useful. It is further unlikely that reduced Mmp2 expression provides complete protection from the damage in UUO. There is no doubt that a longer period of UUO would lead to more severe damage, even in mice with decreased Mmp2 expression.
In conclusion, both homozygous and heterozygous genetic inactivation of Mmp2 protect mice against hydronephrosis and kidney fibrosis after UUO, as indicated by both histology and gene expression. The genetic mechanism seems to be a reduced ability to respond with Mmp2 upregulation under stress, and this may suggest that there is a threshold level of Mmp2 necessary for pelvic remodelling and genetic events leading to activation of fibrosis.
Acknowledgments
The study was supported by the Western Health Authority of Norway (Helse Vest), and the Swedish Society for Medical Research (SSMF).
Parts of this study were presented at Experimental Biology 2012 and published as a meeting abstract [39].
Bjarne M. Iversen passed away before the submission of the final version of this manuscript. Michael Hultström accepts responsibility for the integrity and validity of the data collected and analysed.
Data Availability
All relevant data are within the paper.
Funding Statement
The study was supported by the Western Health Authority of Norway (Helse Vest) (project no: 911685) www.helsevest.no, and the Swedish Society For Medical Research (SSMF) www.ssmf.se. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Heikkila J, Holmberg C, Kyllonen L, Rintala R, Taskinen S (2011) Long-term risk of end stage renal disease in patients with posterior urethral valves. J Urol 186: 2392–2396. 10.1016/j.juro.2011.07.109 [DOI] [PubMed] [Google Scholar]
- 2. Hamdi A, Hajage D, Van Glabeke E, Belenfant X, Vincent F, Gonzalez F, et al. (2012) Severe post-renal acute kidney injury, post-obstructive diuresis and renal recovery. BJU Int 110: E1027–1034. 10.1111/j.1464-410X.2012.11193.x [DOI] [PubMed] [Google Scholar]
- 3. Chevalier RL, Forbes MS, Thornhill BA (2009) Ureteral obstruction as a model of renal interstitial fibrosis and obstructive nephropathy. Kidney Int 75: 1145–1152. 10.1038/ki.2009.86 [DOI] [PubMed] [Google Scholar]
- 4. Nangaku M (2004) Mechanisms of tubulointerstitial injury in the kidney: final common pathways to end-stage renal failure. Intern Med 43: 9–17. [DOI] [PubMed] [Google Scholar]
- 5. Aimes RT, Quigley JP (1995) Matrix metalloproteinase-2 is an interstitial collagenase. Inhibitor-free enzyme catalyzes the cleavage of collagen fibrils and soluble native type I collagen generating the specific 3/4- and 1/4-length fragments. J Biol Chem 270: 5872–5876. [DOI] [PubMed] [Google Scholar]
- 6. Hultstrom M, Leh S, Skogstrand T, Iversen BM (2008) Upregulation of tissue inhibitor of metalloproteases-1 (TIMP-1) and procollagen-N-peptidase in hypertension-induced renal damage. Nephrol Dial Transplant 23: 896–903. [DOI] [PubMed] [Google Scholar]
- 7. Flamant M, Placier S, Dubroca C, Esposito B, Lopes I, Chatziantoniou C, et al. (2007) Role of matrix metalloproteinases in early hypertensive vascular remodeling. Hypertension 50: 212–218. [DOI] [PubMed] [Google Scholar]
- 8. Catania JM, Chen G, Parrish AR (2007) Role of matrix metalloproteinases in renal pathophysiologies. Am J Physiol Renal Physiol 292: F905–911. [DOI] [PubMed] [Google Scholar]
- 9. Skogstrand T, Leh S, Paliege A, Reed RK, Vikse BE, Bachmann S, et al. (2013) Arterial damage precedes the development of interstitial damage in the nonclipped kidney of two-kidney, one-clip hypertensive rats. J Hypertens 31: 152–159. [DOI] [PubMed] [Google Scholar]
- 10. Zeisberg M, Khurana M, Rao VH, Cosgrove D, Rougier JP, Werner MC, et al. (2006) Stage-specific action of matrix metalloproteinases influences progressive hereditary kidney disease. PLoS Med 3: e100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tan TK, Zheng G, Hsu TT, Lee SR, Zhang J, Zhao Y, et al. (2013) Matrix metalloproteinase-9 of tubular and macrophage origin contributes to the pathogenesis of renal fibrosis via macrophage recruitment through osteopontin cleavage. Lab Invest 93: 434–449. 10.1038/labinvest.2013.3 [DOI] [PubMed] [Google Scholar]
- 12. Kalluri R, Neilson EG (2003) Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest 112: 1776–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kaneko T, Shimizu A, Mii A, Fujita E, Fujino T, Kunugi S, et al. (2012) Role of matrix metalloproteinase-2 in recovery after tubular damage in acute kidney injury in mice. Nephron Exp Nephrol 122: 23–35. 10.1159/000346569 [DOI] [PubMed] [Google Scholar]
- 14. Kunugi S, Shimizu A, Kuwahara N, Du X, Takahashi M, Terasaki Y, et al. (2011) Inhibition of matrix metalloproteinases reduces ischemia-reperfusion acute kidney injury. Lab Invest 91: 170–180. 10.1038/labinvest.2010.174 [DOI] [PubMed] [Google Scholar]
- 15. Itoh T, Ikeda T, Gomi H, Nakao S, Suzuki T, Itohara S (1997) Unaltered secretion of beta-amyloid precursor protein in gelatinase A (matrix metalloproteinase 2)-deficient mice. J Biol Chem 272: 22389–22392. [DOI] [PubMed] [Google Scholar]
- 16. Ohno-Matsui K, Uetama T, Yoshida T, Hayano M, Itoh T, Morita I, et al. (2003) Reduced retinal angiogenesis in MMP-2-deficient mice. Invest Ophthalmol Vis Sci 44: 5370–5375. [DOI] [PubMed] [Google Scholar]
- 17. Takamiya Y, Fukami K, Yamagishi S, Kaida Y, Nakayama Y, Obara N, et al. (2013) Experimental diabetic nephropathy is accelerated in matrix metalloproteinase-2 knockout mice. Nephrol Dial Transplant 28: 55–62. 10.1093/ndt/gfs387 [DOI] [PubMed] [Google Scholar]
- 18. Suofu Y, Clark JF, Broderick JP, Kurosawa Y, Wagner KR, Lu A (2012) Matrix metalloproteinase-2 or -9 deletions protect against hemorrhagic transformation during early stage of cerebral ischemia and reperfusion. Neuroscience 212: 180–189. 10.1016/j.neuroscience.2012.03.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nishida M, Okumura Y, Ozawa S, Shiraishi I, Itoi T, Hamaoka K (2007) MMP-2 inhibition reduces renal macrophage infiltration with increased fibrosis in UUO. Biochem Biophys Res Commun 354: 133–139. [DOI] [PubMed] [Google Scholar]
- 20. Goulter AB, Harmer DW, Clark KL (2006) Evaluation of low density array technology for quantitative parallel measurement of multiple genes in human tissue. BMC Genomics 7: 34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Du X, Shimizu A, Masuda Y, Kuwahara N, Arai T, Kataoka M, et al. (2012) Involvement of matrix metalloproteinase-2 in the development of renal interstitial fibrosis in mouse obstructive nephropathy. Lab Invest 92: 1149–1160. 10.1038/labinvest.2012.68 [DOI] [PubMed] [Google Scholar]
- 22. LeBleu VS, Teng Y, O'Connell JT, Charytan D, Muller GA, Muller CA, et al. (2013) Identification of human epididymis protein-4 as a fibroblast-derived mediator of fibrosis. Nat Med 19: 227–231. 10.1038/nm.2989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fernandez-Patron C, Radomski MW, Davidge ST (1999) Vascular matrix metalloproteinase-2 cleaves big endothelin-1 yielding a novel vasoconstrictor. Circ Res 85: 906–911. [DOI] [PubMed] [Google Scholar]
- 24. Martinez A, Oh HR, Unsworth EJ, Bregonzio C, Saavedra JM, Stetler-Stevenson WG, et al. (2004) Matrix metalloproteinase-2 cleavage of adrenomedullin produces a vasoconstrictor out of a vasodilator. Biochem J 383: 413–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ledbetter S, Kurtzberg L, Doyle S, Pratt BM (2000) Renal fibrosis in mice treated with human recombinant transforming growth factor-beta2. Kidney Int 58: 2367–2376. [DOI] [PubMed] [Google Scholar]
- 26. Wang X, Zhou Y, Tan R, Xiong M, He W, Fang L, et al. (2010) Mice lacking the matrix metalloproteinase-9 gene reduce renal interstitial fibrosis in obstructive nephropathy. Am J Physiol Renal Physiol 299: F973–982. 10.1152/ajprenal.00216.2010 [DOI] [PubMed] [Google Scholar]
- 27. Schaefer L, Macakova K, Raslik I, Micegova M, Grone HJ, Schonherr E, et al. (2002) Absence of decorin adversely influences tubulointerstitial fibrosis of the obstructed kidney by enhanced apoptosis and increased inflammatory reaction. Am J Pathol 160: 1181–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wang Z, Famulski K, Lee J, Das SK, Wang X, Halloran P, et al. (2014) TIMP2 and TIMP3 have divergent roles in early renal tubulointerstitial injury. Kidney Int 85: 82–93. 10.1038/ki.2013.225 [DOI] [PubMed] [Google Scholar]
- 29. Kim H, Oda T, Lopez-Guisa J, Wing D, Edwards DR, Soloway PD, et al. (2001) TIMP-1 deficiency does not attenuate interstitial fibrosis in obstructive nephropathy J Am Soc Nephrol 12: 736–748. [DOI] [PubMed] [Google Scholar]
- 30. Kishioka H, Fukuda N, Wen-Yang H, Nakayama M, Watanabe Y, Kanmatsuse K (2001) Effects of PDGF A-chain antisense oligodeoxynucleotides on growth of cardiovascular organs in stroke-prone spontaneously hypertensive rats. Am J Hypertens 14: 439–445. [DOI] [PubMed] [Google Scholar]
- 31. Eitner F, Buecher E, van Roeyen C, Kunter U, Rong S, Seikrit C, et al. (2008) PDGF-C is a proinflammatory cytokine that mediates renal interstitial fibrosis. Journal of the American Society of Nephrology 19: 281–289. 10.1681/ASN.2007030290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Martin IV, Borkham-Kamphorst E, Zok S, van Roeyen CRC, Eriksson U, Boor P, et al. (2013) Platelet-Derived Growth Factor (PDGF)-C Neutralization Reveals Differential Roles of PDGF Receptors in Liver and Kidney Fibrosis. American Journal of Pathology 182: 107–117. 10.1016/j.ajpath.2012.09.006 [DOI] [PubMed] [Google Scholar]
- 33. Tang WW, Ulich TR, Lacey DL, Hill DC, Qi M, Kaufman SA, et al. (1996) Platelet-derived growth factor-BB induces renal tubulointerstitial myofibroblast formation and tubulointerstitial fibrosis. Am J Pathol 148: 1169–1180. [PMC free article] [PubMed] [Google Scholar]
- 34. Ostendorf T, Boor P, Van Roeyen CRC, Floege J (2014) Platelet-derived growth factors (PDGFs) in glomerular and tubulointerstitial fibrosis. Kidney International Supplements 4: 65–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Du TY, Luo HM, Qin HC, Wang F, Wang Q, Xiang Y, et al. (2013) Circulating Serum Trefoil Factor 3 (TFF3) Is Dramatically Increased in Chronic Kidney Disease. Plos One 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chade AR (2012) VEGF: Potential therapy for renal regeneration. F1000 Med Rep 4: 1 10.3410/M4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Vesey DA, Cheung C, Cuttle L, Endre Z, Gobe G, Johnson DW (2002) Interleukin-1beta stimulates human renal fibroblast proliferation and matrix protein production by means of a transforming growth factor-beta-dependent mechanism. J Lab Clin Med 140: 342–350. [DOI] [PubMed] [Google Scholar]
- 38. Henderson NC, Mackinnon AC, Farnworth SL, Kipari T, Haslett C, Iredale JP, et al. (2008) Galectin-3 expression and secretion links macrophages to the promotion of renal fibrosis. Am J Pathol 172: 288–298. 10.2353/ajpath.2008.070726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tveitarås MK S T, Helle F, Leh S, Reed RK, et al. (2012) MMP2 deficient mice are protected from hydronephrosis after unilateral ureteral obstruction. FASEB Journal 26: 868.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.