Abstract
Historically, cancer has occurred at a lower rate in aboriginal populations; however, it is now dramatically increasing. Unless preventive measures are taken, cancer rates among aboriginal peoples are expected to soon surpass those in non-aboriginal populations. Because a large proportion of malignant disorders are preventable, primary prevention through socioeconomic interventions, environmental changes, and lifestyle modification might provide the best option for reducing the increasing burden of cancers. Such efforts can be further amplified by making use of effective cancer screening programs for early detection of cancers at their most treatable stage. However, compared with non-aboriginal Canadians, many aboriginal Canadians lack equal access to cancer screening and prevention programs. In this paper, we discuss disparities in cancer prevention and screening in aboriginal populations in Canada. We begin with the relevant definitions and a theoretical perspective of disparity in health care in aboriginal populations. A framework of health determinants is proposed to explain the pathways associated with an increased risk of cancer that are potentially avoidable. Major challenges and knowledge gaps in relation to cancer care for aboriginal populations are addressed, and we make recommendations to eliminate disparities in cancer control and prevention.
Keywords: Cancer prevention, cancer screening, aboriginal populations, disparity, inequity, Canadian health care
INTRODUCTION
Cancer is a leading cause of death worldwide. Each year, tens of millions of people are diagnosed with—and more than half eventually die from—cancer1–3. In the year 2008, cancer accounted for 7.6 million deaths globally (13%), which surpasses deaths from hiv/aids, malaria, and tuberculosis3. About 70% of all cancer deaths occurred in low- and middle-income countries. According to the Global Status Report on Noncommunicable Diseases 2010, cancer rates could further increase by 50% to 15 million new cases in the year 20203. Cancer has surpassed cardiovascular disease as the leading cause of death in Canada. The expectation is that 40% of men and boys and 45% of women and girls will develop cancer during their lifetime and that 24% and 29% respectively will die from their disease2. An estimated 191,300 new cases of cancer and 76,600 deaths occurred in Canada in 2014.
Despite major breakthroughs in cancer research, screening, and treatment, the burden of cancer is unequally distributed in specific population groups. “Disparity in cancer care” is defined as systematic differences in cancer incidence, prevalence, and mortality in specific population groups4,5.
An assessment of cancer incidence rates according to socioeconomic, racial, and ethnic groups can uncover significant differences. For instance, a 14% reduction in the overall rate of cancer-related death was noted between the years 1991 and 2004, and yet compared with their white counterparts, racial and ethnic minorities continued to die from cancer at disproportionate rates1,2. Likewise, ample evidence supports the fact that people with a lower socioeconomic status experience a greater cancer incidence and shorter survival after a cancer diagnosis5.
It is noteworthy that a large proportion of malignant disorders are preventable. Consequently, primary prevention through socioeconomic interventions, environmental changes, and lifestyle modification could be the best option for reducing the increasing burden of cancers. Those efforts can be further amplified by utilizing effective cancer screening programs for the early detection of cancers at their most treatable stage. In Canada, however, not all citizens have equal access to cancer screening and prevention programs6–8, and even the disparities are differentially distributed among the high-risk groups (socioeconomically disadvantaged people, aboriginal populations, ethnic minorities with language barriers, and people living in rural and remote areas).
Among the groups at high risk for cancer, the aboriginal peoples of Canada face unique health challenges. They have a lower life expectancy and experience higher rates of coronary artery disease, diabetes, tuberculosis, and hiv infection9. Although cancer has historically occurred at a lower rate in aboriginal populations, it is now dramatically increasing (Table i). Challenging life circumstances such as poverty and the negative social conditions experienced by many aboriginal peoples affect cancer incidence, survival, and prevention. Unless preventive measures are taken, cancer rates among aboriginal peoples are expected to soon surpass those in the non-aboriginal population.
TABLE I.
Cancer incidence and mortality for First Nations compared with other Canadians in various Canadian provinces10–13
| Region | Rates | Comments |
|---|---|---|
| British Columbia | The rate of cervical cancer is higher in the First Nations female population than the general female population | Breast cancer is diagnosed at a later stage in First Nations women |
| Manitoba and Saskatchewan | The rates of cervical cancer in women and kidney cancer in men and women are higher in the First Nations population than in the general population | Breast cancer survival is poorer in northern First Nations populations than in southern non–First Nations populations, even after adjustment for stage |
| Ontario | The incidences for all cancers combined and for the four most common cancers (breast, prostate, lung, and colorectal) are increasing in the First Nations population; rates for colorectal and lung cancers are approaching rates in the Ontario general population | Survival for all cancers combined is significantly worse for the First Nations populations compared with the Ontario general population |
Here, we discuss disparities in cancer prevention and screening among aboriginal Canadians. We start with the relevant definitions and a theoretical perspective of disparity. A framework of health determinants is proposed to explain the pathways associated with increased risks of cancers that are potentially avoidable. We also address major challenges and knowledge gaps in relation to cancer care for aboriginal populations, and end with recommendations to eliminate disparities in cancer control and prevention.
DEFINITIONS
To have significant impact on health policy, explicit definitions are important. “Disparity” is defined as “lack of similarity or equality; inequality; difference or the condition or fact of being unequal”14. In health, disparity is concerned with the health of disadvantaged groups. No definition of health disparity has yet been universally accepted; various definitions have been proposed. In the early 1990s, Whitehead described “health disparity” as differences in health that “are not only unnecessary and avoidable but, in addition, are considered unfair and unjust”15. Braveman aimed to further clarify the concept of health disparity and described it as “a particular type of potentially avoidable difference in health or in important influences on health that can be shaped by policies; it is a difference in which a disadvantaged social group or groups experience worse health or greater health risks than the most advantaged social groups”16.
“Aboriginal people” is the term used to describe the people (and their descendants) who inhabited North America before European settlers arrived. In the 2006 Canadian census, 1.2 million people (3.8%) identified themselves as aboriginal17. However, new data from the Canadian National Household Survey show that, in 2011, 1,400,685 people had an aboriginal identity, representing 4.3% of the total Canadian population18. Section 35 of the Constitution Act, 1982 defines aboriginal peoples as registered (“status”) Indians under the Indian Act, Métis, and Inuit, each with unique heritages, languages, cultural practices, and spiritual beliefs19. “First Nations” is a term that registered Indians proposed in the 1970s to replace the term “Indian.” It refers to the status and non-status Indian peoples in Canada. The First Nations are the largest aboriginal group in Canada, constituting 64% of the aboriginal population. Currently, 62% of First Nations people live on-reserve, in one of 617 communities throughout Canada20. The Métis are descendants of First Nations people and early Europeans who identify themselves as Métis, as distinct from First Nations people, Inuit, or non-aboriginal people. The Inuit are a people indigenous to Northern Canada who live in Nunavut, the Northwest Territories, northern Quebec, and northern Labrador.
THEORETICAL PERSPECTIVE OF HEALTH DISPARITY
In comparison with non-aboriginal people, aboriginal people are less likely to receive equal health care; they also experience more health-related problems8–10. For instance, aboriginal people die younger and at a higher rate than non-aboriginal people; their infant mortality rate is higher; they shoulder a disproportionate burden of infectious and sexually transmitted diseases; and they are experiencing a rising level of life-threatening chronic conditions.
Theories are important constructs for understanding the origins and causes of health disparities and how social structures operate to oppress some people, while systematically privileging others. Theoretical approaches such as the “critical theory,” the “postcolonial theory,” and the “social–ecological model” are important to reaching an understanding of health disparities in aboriginal people21–23. Critical theory includes many perspectives and suggests a process that can help to liberate people from the constraints of irrational and unjust structures placed on them by race, class, and sex, and that empowers them to gain more control over threatening conditions21. Postcolonial theory is a family of theories that shares a social, political, and moral concern about the history and legacy of colonialism and how it continues to shape people’s lives, well-being, and life opportunities22. The critical and postcolonial theories underscore how health disparity in aboriginal peoples is a result of centuries-old colonization practices and assimilation policies that sought to undermine and destroy aboriginal cultures and dispossess people from their traditional lands. The social–ecological model helps in understanding how various determinants in the social and physical environment—including poverty, unemployment, and pollution—shape individual response and how the quality of a social environment (compared with a lack of such resources) can have a direct, health-promoting influence on individual actions, consequently leading to better health23. The study of “historical trauma” (a state of chronic trauma and unresolved grief) explains why some aboriginal people might engage in self-destructive behavior or be unable to trust health care providers and thereby be reluctant to engage in treatment24.
FRAMEWORK OF CANCER PREVENTION AND SCREENING
Although most cancer is the result of a complex interaction of genetic susceptibility and environmental factors, there is sufficient evidence that a major proportion of malignant diseases are preventable25,26. It has been estimated that more than 30% of cancer deaths could be prevented by modifying or avoiding key risk factors, including tobacco abuse, overweight or obesity, an unhealthy diet with low fruit and vegetable intakes, lack of physical activity, chronic alcohol use, infection with the sexually transmitted human papilloma virus (hpv), urban air pollution, and indoor smoke from household use of solid fuels. Given that genetics and environment are difficult to modify, the burden of cancer can be reduced by implementing strategies for cancer prevention and early detection of cancer and by eliminating variable access to resources, health services, and social programs.
Although a range of frameworks and models have been proposed to address various public health problems, no specific framework for cancer prevention and screening in the aboriginal population has yet emerged. We propose a conceptual framework that elucidates biologic and environmental factors and their interactions with socioeconomic status, access to resources, and the individual’s knowledge and belief that collectively shape the individual response in relationship with modifiable determinants (Figure 1). Those determinants work at the individual, organizational, community, and societal levels. Differential exposure to the modifiable determinants can result in differential cancer incidences and mortality rates. A broad vision—with a focus on the environmental and social determinants of health, changes to inequitable resource distribution, and dedicated and coordinated efforts—is prerequisite for reducing the rising cancer burden in aboriginal communities.
FIGURE 1.
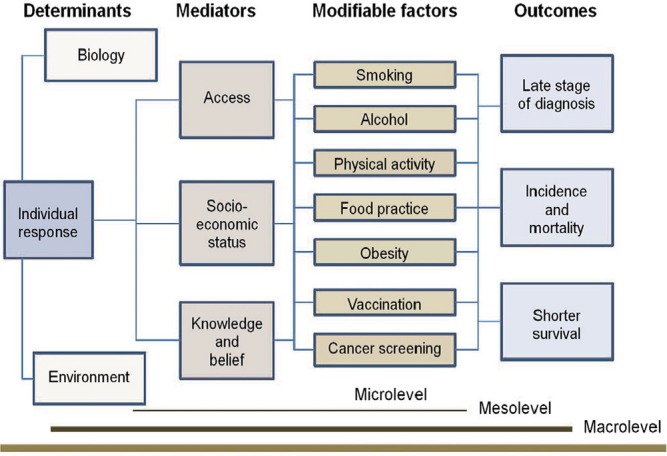
Framework for cancer prevention and screening in aboriginal peoples.
In the next section, we review some key modifiable factors (proposed in the framework) that correlate with a rising risk of cancer and result in differential outcomes in aboriginal populations.
PRIMARY PREVENTION
Smoking
Smoking is the leading cause of preventable death in the world, killing 5 million people every year. Smoking is causally related to various cancers, including those of lung, head and neck, upper gastrointestinal tract, colon and rectum, and genitourinary tract27. The risk is proportional to the duration and intensity of smoking. Estimates suggest that tobacco smoking is responsible for about one third of all fatal cancers. Smoking risk has either been confounded or modified by heavy alcohol consumption.
Many aboriginal peoples, and specifically First Nations, have traditional uses for tobacco in ceremonies, rituals, prayer, communication with the spirits, and purification of the mind. Although tobacco is sacred, the recreational or non-traditional uses of tobacco such as smoking cigarettes, chewing tobacco, or smoking cigars is considered by First Nations people to be dangerous and harmful.
Various aboriginal population surveys, including the First Nations Regional Health Longitudinal Survey 2002/2003, the 2006 Aboriginal Peoples Survey, and the 2004 Baseline Study Among First Nations On-Reserve and Inuit in the North (Environics Research Group) have shown that smoking is more common among aboriginal people than among other Canadians8,9,28. For instance, 59% of on-reserve First Nations people smoke, and most of the on-reserve First Nations people who smoke began smoking between the ages of 13 and 16. The smoking rates for aboriginal adolescents 15–17 years of age are triple those of non-aboriginal adolescents in the same age category.
Approximately 70% of the adult Inuit population reported that they smoke at more than 3 times the self-reported rate of 17% for all adults in Canada. Almost half the Inuit who smoke began smoking at age 14 or younger. Lung cancer rates among the Inuit are now the highest in the world29.
Various political, economic, and social factors correlate with smoking30. Hence, targeted smoking cessation strategies have the potential not only to reduce the risk of cancer, but also to improve the risks for development of chronic diseases, including coronary artery disease, cerebrovascular accident, and chronic obstructive lung disease9.
Alcohol
Chronic alcohol consumption has been linked to increased risks for several cancers. Risks of oral, pharyngeal, laryngeal, esophageal, and liver cancer are higher among alcohol drinkers and correlate with the amount consumed. In addition, alcohol increases the risk for colorectal and breast cancers31. There is evidence that socioeconomically disadvantaged individuals experience greater levels of alcohol-related death32.
Alcohol use has been identified as a problem in aboriginal communities, and in addition to an increased risk of alcohol-related cancers, alcohol use can lead to violence, sexual and physical abuse, accidents, self-inflicted injury, and death32,33. Risk factors linked to alcohol use in aboriginal populations include poverty, depression, history of attendance at residential schools, childhood abuse, being a victim of physical or sexual violence, and history of family violence34. However, data on the extent of alcohol use and its impact on the cancer burden in aboriginal communities are lacking.
Obesity
Obesity continues to be one of the critical health issues worldwide. Approximately one third of the world population is considered to be overweight or obese (defined as a body mass index of 25 or greater), with 25 to less than 30 being classed as overweight and 30 or greater being classed as obesity35,36. The link between obesity and cancer has been demonstrated in numerous cohort studies36–38. Sufficient evidence has accumulated to demonstrate an association between obesity and cancer of the breast, colon, uterus, kidney, and esophagus36,37,39. Additionally, obesity has been linked with other cancers, such as those of liver, pancreas, lymph system (non-Hodgkin lymphoma), and marrow (myeloma). Overweight and obesity account for 14% of all deaths from cancer in men and 20% of those in women36.
Obesity is an important health issue among First Nations, Inuit, and Métis populations. Compared with other ethnic groups in Canada, aboriginal Canadians have the highest prevalence of obesity. Self-reported data from the 2007 Canadian Community Health Survey demonstrated that obesity rates were higher among off-reserve aboriginal adults than among non-aboriginal people (24.8% vs. 16.6%)40. Self-reported data from the 2002–2003 First Nations Regional Longitudinal Health Survey revealed that the prevalence of obesity was particularly high among on-reserve First Nations people: 31.8% of adult men, 41.1% of adult women, 14.0% of adolescents, and 36.2% of children were considered obese41.
Robertson et al. showed the presence of a consistent and profound social gradient in the prevalence of obesity42. About 20%–25% of obesity in men and 40%–50% of obesity in women can be attributed to differences in socioeconomic status. Hence, efforts to address the roots causes are clearly warranted to optimize cancer control.
Food Insecurity
“Food insecurity” refers to lack of access to sufficient, safe, and nutritious food that fulfills the dietary needs and food preferences for living a healthy life. There is evidence suggesting a relationship between specific dietary components and risk of cancers at various anatomic sites25,26,43. For instance, a high intake of red meat appears to be an important causative factor in colorectal cancer, and a high intake of fruits and vegetables might have a protective role44. Current data also suggest a modest association between risk of breast cancer and a high intake of fat, meat, and dairy products and a low intake of fruits and vegetables45.
Aboriginal peoples living in remote rural and reserve communities face substantial food insecurity related to challenges in acquiring both market and traditional foods46–49.
The costs of transporting market foods to remote communities mean that healthful, nutritious food is not affordable for most families. Poverty not only limits the extent to which individuals and families can access market foods, but also makes the costs associated with contemporary hunting out of reach for many49–51. The Canadian Community Health Survey 2.2 revealed that, compared with non-aboriginal households, aboriginal households experience more, and more severe, food insecurity (33% vs. 9% and 3% vs. 14% respectively)52. The survey also revealed a greater prevalence of sociodemographic risk factors for household food insecurity among the aboriginal households. After adjustment for the sociodemographic factors, the risk for food insecurity remained higher for aboriginal households than for non-aboriginal households (odds ratio: 2.6; 95% confidence interval: 2.1 to 3.2). Consequently, efforts to alleviate food insecurity in aboriginal communities should take cultural, environmental, and socioeconomic circumstances into consideration.
HPV Vaccination
The human papillomavirus is associated with cervical, anal canal, and oropharyngeal cancers. Vaccination against hpv is approved for girls and women 9–26 years of age to protect against infection with hpv types 6, 11, 16, and 18, which are responsible for approximately 70% of all cervical cancers and for more than 90% of anogenital warts53.
Information about the incidence of hpv, Pap screening, and cervical cancer rates among First Nations, Inuit, and Métis peoples in Canada are limited. The published reports have demonstrated a higher prevalence of hpv infection among aboriginal peoples than in the non-aboriginal population. A 2008 collaborative project between Nunavut and the Public Health Agency of Canada, involving 4043 women, revealed a hpv prevalence of about 30%, with 9.5% of all the women having multiple types of the virus, 22.1% having at least 1 of the high-risk hpv types, and 4.9% having multiple high-risk types54. Furthermore, compared with other Canadian women, aboriginal women have a cervical cancer prevalence that is higher by up to a factor of 3 and a cervical cancer mortality rate that is higher by up to a factor of 454–56.
In Nunavut, hpv vaccine uptake has been approximately 58% since the initiation, in 2010, of a publicly funded, school-based program for grade 6 girls (12-year-olds)54. Currently, however, little is known about the uptake of the vaccine in aboriginal populations, and there is a need for improved content and delivery of sexual health education among aboriginal women in the Canadian North57.
SECONDARY PREVENTION: CANCER SCREENING
In addition to measures for cancer prevention that can potentially reduce the cancer incidence by 35%, early detection is one of the most effective ways to reduce the morbidity and mortality from cancer25. Detection of cancer at an early stage, by screening of the healthy population, has been proved to be effective in reducing mortality from cervical, breast, and colorectal cancers.
The geographic distribution and cultural diversity of aboriginal populations is a key factor in the delivery of screening services. The current status of cancer screening in aboriginal populations is not known because no health surveillance system in Canada captures information on ethnicity. Most health surveys of aboriginal people do not distinguish between First Nations, Métis, and Inuit populations. However, indirect evidence suggests that access by aboriginal populations to screening services lags that in comparable non-aboriginal populations. The 2002–2003 First Nations Regional Longitudinal Health Survey reported inadequate access to cancer screening services among First Nations peoples10.
Cervical Cancer Screening
Several studies have reported that cervical cancer is more common among aboriginal than non-aboriginal women55,56,58,59. In Quebec, for example, the prevalence of cervical cancer in the aboriginal population was found to be 3 times that in other Canadians, and the cervical cancer mortality rate was found to be 4 times that in other Canadian women58. In the early 1990s in British Columbia, cervical cancer mortality among aboriginal women was 6 times that among non-aboriginal women59. During 1991–2010, that mortality gap declined, but the mortality for aboriginal women was still double that for non-aboriginal women.
Pap tests can be administered by many trained health professionals. Most provinces and territories recommend annual testing initially, followed by triennial smears after 2 years of normal tests10. Although the incidence of cervical cancer has declined by 70% in Canada since the early 1960s (largely because of provincial screening programs), the rates of participation in Pap test screening for cervical cancer in many Canadian provinces have been lower among aboriginal women10,60. Barriers to participation by those women in cervical cancer screening included, but were not limited to, a knowledge gap, lack of culture-sensitive care, prevention as an abstract concept, embarrassment caused by the procedure, and fear of cancer60,61.
Breast Cancer Screening
Of all types of cancer affecting Canadian women, breast cancer has the highest incidence. Although breast cancer has been shown to be less prevalent in indigenous women, the overall breast cancer incidence among aboriginal women is on the rise. A low screening rate is considered to be a key explanatory factor in the recent rise of breast cancer– related mortality in First Nations women62. Compared with non-aboriginal women, aboriginal women are more likely to be diagnosed at a later stage of the disease, which is likely a consequence of limited access to breast cancer screening. For instance, a survey involving 5 First Nations communities in New Brunswick found that only 29% of female residents were aware of the provincial self-referral program. Overall, 65% of women 50–69 years of age had undergone mammography within the preceding 2 years, a rate lower than the 77% observed in non-aboriginal women63.
Organized breast cancer screening programs are in place in all provinces and territories and can be accessed directly by eligible women; a physician’s referral is not required10. All provinces have mobile breast screening clinics that travel to remote communities on a regular basis. However, the impact of mobile mammography clinics on breast cancer screening rates among aboriginal women is currently unknown. In Manitoba, a province-wide breast cancer screening program was organized in 1995–1996. However, from 1999 to 2008, rates of mammography in the preceding 2 years were 37% among First Nations women and 59% among non-aboriginal women. Regardless of area of residence, First Nations women were less likely than non-aboriginal women to have undergone mammography (relative rates: 0.69 in the North, 0.55 in the rural south, and 0.53 in urban areas)64.
Colorectal Cancer Screening
The incidence and mortality rates for colorectal cancer in aboriginal populations are high and approaching the incidence in the non-aboriginal population. For example, colorectal cancer was uncommon in First Nations people (compared with the general population) in Ontario in the 1970s. However, incidence rates have increased and are now similar to those in the Ontario population as a whole13,65. Similar rises have been noted in other parts of Canada10,56,66. Organized stepwise colorectal cancer screening programs are relatively new in Canada, and participation rates for aboriginal populations are currently not known.
BARRIERS, GAPS, AND CHALLENGES
Aboriginal peoples face unique challenges and barriers related to cancer prevention and early detection of cancer. Furthermore, research methodologies contain major gaps with respect to aboriginal people. The barriers are complex and include systemic, cultural, and personal factors. They operate in respect to knowledge, personal beliefs, and access.
Identification of First Nations, Métis, and Inuit
Health care delivery in Canada involves a variety of jurisdictions. Information about ethnicity is not captured by most health information databases. Research and cancer surveillance data for aboriginal populations are lacking. In large population surveys and in provincial cancer registries, respondents are not identified by race or ethnicity. Most health surveys of aboriginal people do not distinguish between First Nations, Métis, and Inuit populations. Studies generally collect data from on- or off-reserve First Nations, but are rarely inclusive of all First Nations in Canada, and surveys often rely on self-identification. Moreover, data-sharing between jurisdictions is difficult or impossible because of disparate information systems and privacy legislation13. To overcome the challenges, researchers use various methods, including linking data from cancer registries with federal Indian status numbers, using postal codes as a proxy for the identity of “Registered Indians” (First Nations), matching health card numbers that belong to individuals with “Registered Indian” status, and checking death certificate data13 (Table ii). However, each method has its own limitations. Furthermore, such strategies capture only Registered Indians and Inuit, and not non-status Indians or Métis.
TABLE II.
Methods for identifying aboriginal populations and their limitations
| Method | Description | Limitations |
|---|---|---|
| Residence on a reserve | There are specific postal (or other area) codes for reserves that are included on some files |
|
| Health card number belongs to a First Nations individual | In some provinces, First Nations individuals can be identified by health card number |
|
| Aboriginal ethnicity on death certificate | Some provinces collect this information at the time of death |
|
| Linkage with the SVS (Status Verification System)a | The SVS includes all registered First Nations individuals living on or off reserve who are eligible for federal benefits |
|
Maintained by Indigenous and Northern Affairs Canada.
Integration Gaps and Jurisdictional Issues
Health services for aboriginal individuals are complex and below the standard of those delivered to non-aboriginal populations. Services are fragmented and lack coordination. Moreover, the division of responsibility between the federal and provincial or territorial governments is unclear9,10,13. Promotion of cancer control in the aboriginal population is greatly challenged by a lack of integrated services in a single location and a distinct gap between mainstream and traditional approaches.
Access
The availability of services, the financial and nonfinancial costs associated with presentation of health care needs, and the existence of equitable treatment can all constitute barriers to health care access.
Many aboriginal communities lack longitudinal community and public health programs. Residents in such communities usually do not have a primary care provider for health maintenance and continuity of care and are forced to seek primary care through emergency rooms. Many individuals reside in remote and isolated communities. To access screening and diagnostic follow-up, most have to travel long distances outside of their communities, away from family and work.
Knowledge and Beliefs
Many aboriginal people have limited awareness of screening and prevention programs. Health literacy is very low in some communities. In addition to language barriers and lower literacy, culturally relevant materials about cancer prevention and screening are lacking. At present, First Nations, Métis, and Inuit communities have no dedicated staff to provide cancer education. Furthermore, experiences at residential school affect attitudes to conventional medicine and health and screening behaviors. A mistrust of the health care system can be present. Screening can be viewed as a treatment rather than as prevention.
INTERVENTIONS
Social disparities and inequities in health for aboriginal people across Canada favour a broader social welfare provision to reduce disparities in cancer prevention and screening. Interventions to reduce new cases of cancer among aboriginal Canadians and to reduce cancer-related mortality in aboriginal people are needed67. We propose a conceptual framework that uses critical theory (empowerment model) and social–ecological and community engagement models to promote cancer prevention and screening in aboriginal populations (Figure 2). The major components of the framework include research and its application in the development of strategies and policies, and community partnership and empowerment at the individual and community level.
FIGURE 2.
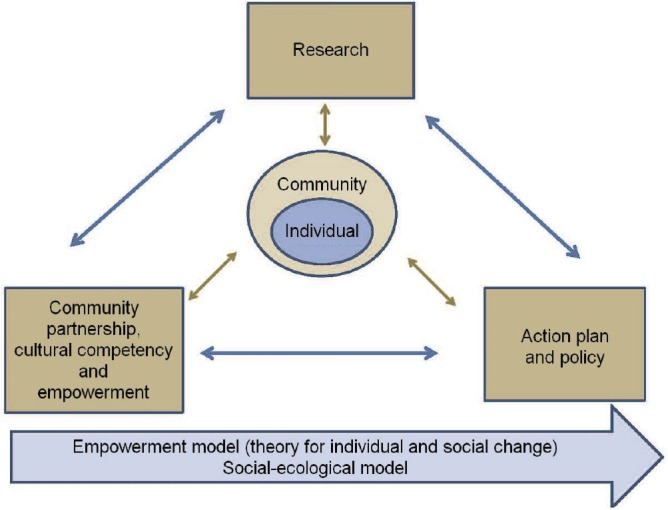
Framework of potential interventions to reduce disparity in cancer prevention and screening in aboriginal peoples.
Research and Knowledge Translation
Although research has improved our understanding of disparities in cancer prevention and screening among aboriginal people, many questions remain unanswered. Interdisciplinary research with effective cross-disciplinary dialogue is crucial to advancing knowledge and promoting health for aboriginal peoples (Figure 3). Cancer surveillance research is key to assisting in the development of cancer control priorities and evaluating the success of prevention and screening programs. National surveillance data can be used to address the magnitude of problem, to detect priority areas, to evaluate prevention, to assess prognosis, and to monitor changes in cancer rates over time. The poorer survival (for at least some cancers) among aboriginal people is not entirely attributable to a less-favourable distribution of cancer stage at diagnosis, and hence qualitative and quantitative research seeking reasons for that survival disadvantage are both required to shape programs, policies, and systems that will reduce the inequalities in cancer control and prevention in aboriginal populations.
FIGURE 3.

Interdisciplinary research with effective cross-disciplinary dialogue is crucial to advance knowledge and to promote health for aboriginal peoples.
Participatory action research—with implementation plans, active engagement of aboriginal people, and ocap (ownership, control, access, possession) provisions at its core—is crucial for success. Efforts to increase the participation of aboriginal people in research and clinical trials should be part of a broad-based initiative to remove barriers to access for the entire Canadian population. Facilitation of knowledge creation and development of strategies for sharing information at various levels are important steps to eliminate unequal access to cancer screening and prevention.
Action Plan and Policy
A life-course perspective (with an integrative approach, planning, implementation, evaluation, reformulation, and generalization) is important to reduce disparities. A national system—one that permits aggregation of communities across provincial boundaries, that generates routinely collected high-quality and timely data for action planning, and that increases collaboration and reduces duplication (that is, it works across organizations, sectors, and diseases regardless of province or territory) so as to integrate cancer prevention and other chronic disease prevention strategies, while at the same time identifying key partners and adequate support—is vital for consequential interventions.
Improvement of cancer control among First Nations, Inuit, and Métis peoples will require inter-sectoral policy development with a focus on socioeconomic determinants including poverty, education, food insecurity, housing, and environmental contamination; identification of new models of care for rural and remote communities; common standards for data collection, access, and reporting; and access to existing resources. Examples include providing funding for disease-prevention interventions that target broad social or environmental determinants; developing culturally appropriate services; addressing barriers to screening, including transportation and distance; recruiting aboriginal people into cancer screening programs; and promoting community-level programs to achieve healthier weights. Actions must be tied to measurable outcomes, with ongoing evaluation and progress monitoring.
Community Partnership, Cultural Competency, and Empowerment
Cancer prevention strategies depend on improving nutrition, achieving healthy body weight, increasing physical activity, and eliminating the use of commercial tobacco. In aboriginal tradition, the health and well-being of an individual flows largely from the health and social make-up of the community. The success of cancer control programs in aboriginal populations lies in accessible information, lifestyle education, continuity of care, role modelling, non-smoking initiatives, and strong partnerships with aboriginal communities.
Although the provincial and territorial governments are primarily responsible for creating awareness of cancer screening and prevention for aboriginal people, effective implementation of cancer education, awareness, and control programs can be achieved only in collaboration with aboriginal communities at multiple levels. Respect, acknowledgment, and active listening and responsiveness to the needs of aboriginal people in a culturally appropriate manner are prerequisites to culturally sensitive cancer prevention and screening service. Promotion of cancer control for aboriginal people requires the use of culturally and linguistically appropriate techniques. Cultural competence includes, but is not limited to, the use of interpreters, to racially or linguistically concordant staffing, and to health education and training that can facilitate effective communication, build trust, and promote better understanding of cancer prevention and screening services68,69. Several tobacco cessation initiatives have been developed. However, to be successful, such initiatives must to be culturally relevant, locally oriented, flexible, and responsive to the needs of the community. The Assembly of First Nations has recently begun developing a draft First Nations and Inuit Tobacco Control Strategy70. The Inuit Tobacco-Free Network (http://www.naho.ca/inuittobaccofree/inuit/itn/whatsNew.php) aims to keep Inuit health workers and their colleagues up to date on tobacco reduction resources, research, and events. A new strategy informed, designed, and controlled by First Nations will result in more widespread and long-lasting outcomes of public health programming [](Table iii).
TABLE III.
Examples of cancer and chronic disease prevention strategies in First Nations, Métis, and Inuit
| Example | Comments |
|---|---|
| National First Nations Tobacco Control Network, Assembly of First Nations (http://www.afn.ca/) | First Nations Tobacco Control Strategy |
| Cancer Care Ontario, Department of Prevention and Screening65, Nunavut Tobacco Reduction Campaign66 | Aboriginal cancer strategies: a 5-year plan to set the stage for many actions engaging First Nation, Métis, and Inuit populations in Ontario Media campaign, poster contests in schools, training of local people, in partnership with Pauktuutit, in smoking cessation programs |
| Aboriginal Health Surveillance (Public Health Agency of Canada)66 | PHAC has funded health surveillance initiatives with several Métis nations in British Columbia, Alberta, Manitoba and Ontario to create data linkages using existing records. |
| Northern Ontario School of Medicine71 | Mandate to be responsive to the needs of the people and communities of northern Ontario |
| The Northern Cancer Control Strategy66 | A joint initiative between the Provincial Health Services Authority/ BC Cancer Agency and Northern Health |
Some of the key steps in promoting community engagement and empowerment are the establishment of community-governed health services and community-driven programs; the incorporation of cancer prevention and screening programs into community-based programs and services; the ability to deliver models of care that embrace indigenous knowledge systems; and a robust indigenous managerial and clinical workforce, with strategies to enhance the supply of aboriginal physicians who can advance cancer control in a culturally respectful and safe manner.
The Northern Ontario School of Medicine is an example of a community engagement model71. It was established with a social accountability mandate to be responsive to the needs of the people and communities of northern Ontario72. The school’s community engagement model is defined by the active participation of communities in shaping and delivering medical education. The school has engaged aboriginal communities in all its activities from curriculum development to the admissions process, and it is working toward improved health outcomes for aboriginal peoples71–73.
CONCLUSIONS
Cancer has become a third leading cause of death in aboriginal populations, who are now facing steady rising incidences of cancer and shorter survival after a cancer diagnosis. Health disparity in aboriginal peoples is the result of centuries-old colonization practices and assimilation policies and is shaped by various determinants in the social and physical environment, including poverty, unemployment, and pollution. Many cancers are preventable or treatable in their early stages. Hence, primary and secondary prevention are vital to lower the rising burden of cancer. Interventions that target participatory action research, national cancer surveillance data, knowledge translation, action plans, inter-sectoral policy development, and community empowerment are needed to reduce the numbers of new cases of cancer among aboriginal Canadians and to reduce cancer-related mortality. Community-based interventions are required to achieve long-term and meaningful improvements across a wide range of health problems faced by aboriginal people. To reduce the rising burden of cancer in present and future generations, the provision of community-centred care that is culturally appropriate is imperative.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.United States Department of Health and Human Services. National Institutes of Health. National Cancer Institute, Surveillance, Epidemiology, and End Results Program (seer) Cancer Stat Fact Sheets [Web page] Bethesda, MD: SEER; n.d. [Available at: http://seer.cancer.gov/statfacts; cited 27 May 2015] [Google Scholar]
- 2.Canadian Cancer Society . Cancer statistics at a glance [Web page] Toronto, ON: Canadian Cancer Society; n.d. [Available at: http://www.cancer.ca/en/cancer-information/cancer-101/cancer-statistics-at-a-glance/?region=sk; cited 13 June 2014] [Google Scholar]
- 3.World Health Organization(who) Global Status Report on Noncommunicable Diseases 2010. Geneva, Switzerland: WHO; 2010. [Available online at: http://apps.who.int/iris/bitstream/10665/44579/1/9789240686458_eng.pdf; cited 15 April 2014] [Google Scholar]
- 4.United States, Department of Health and Human Services. National Institutes of Health. National Cancer Institute (nci . About Cancer Health Disparities [Web page] Bethesda, MD: NCI; 2015. [Available at: http://www.cancer.gov/about-nci/organization/crchd/about-health-disparities; cited 27 May 2015] [Google Scholar]
- 5.International Atomic Energy Agency (iaea) Inequality in Cancer Care: A Global Perspective. Vienna, Austria: IAEA; 2011. IAEA Human Health Reports No. 3. [Available online at: http://www-pub.iaea.org/MTCD/Publications/PDF/Pub1471_web.pdf; cited 1 June 2014] [Google Scholar]
- 6.Katz SJ, Hofer TP. Socioeconomic disparities in preventive care persist despite universal coverage. Breast and cervical cancer screening in Ontario and the United States. JAMA. 1994;272:530–4. doi: 10.1001/jama.1994.03520070050037. [DOI] [PubMed] [Google Scholar]
- 7.Cerigo H, Macdonald ME, Franco EL, Brassard P. Inuit women’s attitudes and experiences towards cervical cancer and prevention strategies in Nunavik, Quebec. Int J Circumpolar Health. 2012;71:17996. doi: 10.3402/ijch.v71i0.17996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Health Canada . A Statistical Profile on the Health of First Nations in Canada: Determinants of Health, 1999 to 2003. Ottawa, ON: Health Canada; 2009. [Available online at: http://www.hc-sc.gc.ca/fniah-spnia/pubs/aborig-autoch/2009-stats-profil/index-eng.php; cited 1 June 2015] [Google Scholar]
- 9.Reading J. The Crisis of Chronic Disease Among Aboriginal Peoples: A Challenge for Public Health, Population Health and Social Policy. Victoria, BC: University of Victoria, Centre for Aboriginal Health Research; n.d. [Available online at: http://cahr.uvic.ca/nearbc/documents/2009/CAHR-B2-Chronic-Disease.pdf; cited 31 May 2013] [Google Scholar]
- 10.Assembly of First Nations (afn) Access to Cancer Screening and First Nations. Ottawa, ON: AFN; 2009. [Available online at: http://s3.amazonaws.com/zanran_storage/64.26.129.156/ContentPages/2467254705.pdf; cited 25 October 2013] [Google Scholar]
- 11.Elias B, Kliewer EV, Hall M, et al. The burden of cancer risk in Canada’s indigenous population: a comparative study of known risks in a Canadian region. Int J Gen Med. 2011;4:699–709. doi: 10.2147/IJGM.S24292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenberg T, Martel S. Cancer trends from 1972–1991 for registered Indians living on Manitoba reserves. Int J Circumpolar Health. 1998;57(suppl 1):391–8. [PubMed] [Google Scholar]
- 13.Marrett LD, Jones CR, Wishart K. First Nations Cancer Research and Surveillance Priorities for Canada. Toronto, ON: Cancer Care Ontario; 2004. [Available online at: https://www.cancercare.on.ca/common/pages/UserFile.aspx?fileId=13688; cited 27 October 2013] [Google Scholar]
- 14. Dictionary.com . Disparity [Web resource] Oakland, CA: Dictionary.com; n.d. [Available at: http://dictionary.reference.com/browse/disparity; cited 28 May 2015] [Google Scholar]
- 15.Whitehead M. The Concepts and Principles of Equity and Health. Copenhagen, Denmark: World Health Organization; 2000. [Available online at: http://salud.ciee.flacso.org.ar/flacso/optativas/equity_and_health.pdf; cited 30 May 2015] [DOI] [PubMed] [Google Scholar]
- 16.Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–94. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- 17.Statistics Canada . 2006 Census release topics: Aboriginal Peoples [archived Web page] Ottawa, ON: Statistics Canada; 2013. [Available online at: https://www12.statcan.gc.ca/census-recensement/2006/rt-td/ap-pa-eng.cfm; cited 31 October 2015] [Google Scholar]
- 18.Statistics Canada . Analytical products, 2011: Aboriginal Peoples in Canada: First Nations People, Métis and Inuit [Web page] Ottawa, ON: Statistics Canada; 2015. [Available online at: http://www12.statcan.gc.ca/nhs-enm/2011/as-sa/99-011-x/99-011-x2011001-eng.cfm; cited 4 November 2015] [Google Scholar]
- 19.University of British Columbia (ubc), First Nations Studies Program . Constitution Act, 1982 Section 35 [Web page] Vancouver, BC: UBC; 2009. [Available at: http://indigenousfoundations.arts.ubc.ca/home/government-policy/constitution-act-1982-section-35.html; cited 8 June 2015] [Google Scholar]
- 20.Aboriginal Affairs and Northern Development Canada (aandc) First Nations People in Canada [Web page] Gatineau, QC: AANDC; 2014. [Available at: https://www.aadnc-aandc.gc.ca/eng/1303134042666/1303134337338; cited 31 October 2015] [Google Scholar]
- 21.Steven PE, Hall JM. Applying critical theories to nursing in communities. Pub Health Nurs. 1992;9:2–9. doi: 10.1111/j.1525-1446.1992.tb00065.x. [DOI] [PubMed] [Google Scholar]
- 22.Browne AJ, Smye VL, Varcoe C. The relevance of postcolonial theoretical perspectives to research in aboriginal health. Can J Nurs Res. 2005;37:16–37. [PubMed] [Google Scholar]
- 23.Waldram JB, Herring DA, Young TK. Aboriginal Health in Canada: Historical, Cultural, and Epidemiological Perspectives. 2nd ed. Toronto, ON: University of Toronto Press; 2006. [Google Scholar]
- 24.Brave Heart MY, DeBruyn LM. The American Indian Holocaust: healing historical unresolved grief. Am Indian Alsk Native Ment Health Res. 1998;8:59–78. [PubMed] [Google Scholar]
- 25.World Cancer Research Fund. American Institute for Cancer Research (aicr) Policy and Action for Cancer Prevention. Food, Nutrition, and Physical Activity: A Global Perspective. Washington DC: AICR; 2009. [Google Scholar]
- 26.Danaei G, Vander Hoorn S, Lopez AD, et al. Causes of cancer in the world: comparative risk assessment of nine behavioral and environmental risk factors. Lancet. 2005;366:1784–93. doi: 10.1016/S0140-6736(05)67725-2. [DOI] [PubMed] [Google Scholar]
- 27.Sasco AJ, Secretan MB, Straif K. Tobacco smoking and cancer: a brief review of recent epidemiological evidence. Lung Cancer. 2004;45(suppl 2):S3–9. doi: 10.1016/j.lungcan.2004.07.998. [DOI] [PubMed] [Google Scholar]
- 28.Health Canada. First Nations and Inuit Health: Tobacco [Web page] Ottawa, ON: Health Canada; 2014. [Available at: http://www.hc-sc.gc.ca/fniah-spnia/substan/tobac-tabac/index-eng.php; cited 17 November 2014] [Google Scholar]
- 29.Carriere GM, Tjepkema M, Pennock J, Goedhuis N. Cancer patterns in Inuit Nunangat: 1998–2007. Int J Circumpolar Health. 2012;71:1858. doi: 10.3402/ijch.v71i0.18581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kogevinas M, Pearce N, Susser M, Boffetta P. Social Inequality and Cancer. Vol. 138. Lyon, France: International Agency for Research on Cancer; 1997. pp. 1–15. iarc Scientific Publication No. 138. [Google Scholar]
- 31.Boffetta P, Hashibe M. Alcohol and cancer. Lancet Oncol. 2006;7:149–56. doi: 10.1016/S1470-2045(06)70577-0. [DOI] [PubMed] [Google Scholar]
- 32.van Oers JA, Bongers IM, van de Goor LA, Garretsen HF. Alcohol consumption, alcohol-related problems, problem drinking, and socioeconomic status. Alcohol Alcohol. 1999;34:78–88. doi: 10.1093/alcalc/34.1.78. [DOI] [PubMed] [Google Scholar]
- 33.Korhonen M. Alcohol and Inuit communities: Current Services and New Directions. Ottawa, ON: National Aboriginal Heath Organization; 2005. [Available online at: http://www.naho.ca/documents/it/2005_Alcohol_CCSA_presentation.pdf; cited 17 November 2014] [Google Scholar]
- 34.Koss MP, Yuan NP, Dightman D, et al. Adverse childhood exposures and alcohol dependence among seven Native American tribes. Am J Prev Med. 2003;25:238–44. doi: 10.1016/S0749-3797(03)00195-8. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization (who) Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. Geneva, Switzerland: WHO; 2009. [Available online at: http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf; cited 20 January 2014] [Google Scholar]
- 36.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–38. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 37.Druesne-Pecollo N, Touvier M, Barrandon E, et al. Excess body weight and second primary cancer risk after breast cancer: a systematic review and meta-analysis of prospective studies. Breast Cancer Res Treat. 2012;135:647–54. doi: 10.1007/s10549-012-2187-1. [DOI] [PubMed] [Google Scholar]
- 38.Basen-Engquist K, Chang M. Obesity and cancer risk: recent review and evidence. Curr Oncol Rep. 2011;13:71–6. doi: 10.1007/s11912-010-0139-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vainio H, Bianchini F. IARC Handbooks of Cancer Prevention. Lyon, France: IARC Press; 2002. Volume 6: Weight control and physical activity. [Google Scholar]
- 40.Public Health Agency of Canada (phac) Obesity in Canada – Snapshot [Web page] Ottawa, ON: PHAC; 2012. [Available at: http://www.phac-aspc.gc.ca/publicat/2009/oc/index-eng.php#apc; cited 26 December 2014] [Google Scholar]
- 41.First Nations Information Governance Centre . First Nations Regional Longitudinal Health Survey (RHS) 2002/03. Results for Adults, Youth and Children Living in First Nations Communities. Ottawa, ON: First Nations Information Governance Centre; 2005. [Available online at: http://fnigc.ca/sites/default/files/ENpdf/RHS_2002/rhs2002-03-technical_report.pdf; cited 1 June 2015] [Google Scholar]
- 42.Robertson A, Tirado C, Lobstein T, et al., editors. Food and Health in Europe: A New Basis for Action. Copenhagen, Denmark: World Health Organization; 2004. who Regional Publications, European Series, No. 96. [Available online at: http://www.euro.who.int/__data/assets/pdf_file/0005/74417/E82161.pdf; cited 23 January 2014] [PubMed] [Google Scholar]
- 43.Anderson A. Evidence-Based Cancer Prevention: Strategies for NGOs: A UICC Handbook for Europe. Geneva, Switzerland: International Union Against Cancer; 2004. Evaluating cancer prevention activities; pp. 60–71. [Google Scholar]
- 44.International Agency for Cancer Research (iarc) Fruit and Vegetables. Lyon, France: IARC Press; 2003. iarc Working Group on the Evaluation of Cancer-Preventive Strategies. iarc Handbooks of Cancer Prevention, No. 8. [Google Scholar]
- 45.Thiébaut AC, Kipnis V, Chang SC, et al. Dietary fat and post-menopausal invasive breast cancer in the National Institutes of Health–AARP Diet and Health Study cohort. J Natl Cancer Inst. 2007;99:451–62. doi: 10.1093/jnci/djk094. [DOI] [PubMed] [Google Scholar]
- 46.Chan HM, Fediuk K, Hamilton S, et al. Food security in Nunavut, Canada: barriers and recommendations. Int J Circumpolar Health. 2006;65:416–31. doi: 10.3402/ijch.v65i5.18132. [DOI] [PubMed] [Google Scholar]
- 47.Lambden J, Receveur O, Marshall J, Kuhnlein HV. Traditional and market food access in Arctic Canada is affected by economic factors. Int J Circumpolar Health. 2006;65:331–40. doi: 10.3402/ijch.v65i4.18117. [DOI] [PubMed] [Google Scholar]
- 48.Moffatt ME. Current status of nutritional deficiencies in Canadian aboriginal people. Can J Physiol Pharmacol. 1995;73:754–8. doi: 10.1139/y95-100. [DOI] [PubMed] [Google Scholar]
- 49.proof . Aboriginal peoples and food insecurity [Web page] Toronto, ON: PROOF; n.d. [Available at: http://nutritionalsciences.lamp.utoronto.ca/resources/research-publications/aboriginal-peoples-and-food-insecurity; cited 1 June 2015. [Google Scholar]
- 50.Lawn J, Langner N, Brulé D, Thompson N, Lawn P, Hill F. Food consumption patterns of Inuit women. Int J Circumpolar Health. 1998;57(suppl 1):198–204. [PubMed] [Google Scholar]
- 51.Lawn J, Harvey D. Nutrition and Food Security in Kugaaruk, Nunavut: Baseline Survey for the Food Mail Pilot Project. Ottawa, ON: Ministry of Indian Affairs and Northern Development; 2003. [Google Scholar]
- 52.Health Canada . Food and Nutrition: Canadian Community Health Survey [Web resource] Ottawa, ON: Health Canada; 2012. [Data accessible at: http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/index-eng.php; cited 1 December 2013] [Google Scholar]
- 53.Smith JS, Lindsay L, Hoots B, et al. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update. Int J Cancer. 2007;121:621–32. doi: 10.1002/ijc.22527. [DOI] [PubMed] [Google Scholar]
- 54.Wurtak G. Final Report: Enhancing HPV Prevention among Indigenous Populations. International Perspectives on Health. Montreal, QC: International Centre for Infectious Diseases; 2010. [Available online at: http://cdn.metricmarketing.ca/www.icid.com/files/HPV_Prevention_Aboriginal_Peoples/IPV_Final_Report_July52010_-_final_Jan28-11_logos_removed.pdf; cited 21 June 2014] [Google Scholar]
- 55.Young TK, Kliewer E, Blanchard J, Mayer T. Monitoring disease burden and preventive behavior with data linkage: cervical cancer among aboriginal people in Manitoba, Canada. Am J Public Health. 2000;90:1466–8. doi: 10.2105/AJPH.90.9.1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marrett LD, Chaudhry M. Cancer incidence and mortality in Ontario First Nations, 1968–1991 (Canada) Cancer Causes Control. 2003;14:259–68. doi: 10.1023/A:1023632518568. [DOI] [PubMed] [Google Scholar]
- 57.Lys C, Reading C. Northwest Territories understands the barriers and facilitators to positive, empowers, and safer sexual health. Int J Circumpolar Health. 2012;71:18957. doi: 10.3402/ijch.v71i0.18957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Louchini R, Beaupré M. Cancer incidence and mortality among aboriginal people living on reserves and northern villages in Quebec, 1988–2004. Int J Circumpolar Health. 2008;67:445–51. doi: 10.3402/ijch.v67i5.18355. [DOI] [PubMed] [Google Scholar]
- 59.Hislop TG, Clarke HF, Deschamps M, et al. Cervical cytology screening: how can we improve rates among First Nations women in urban British Columbia? Can Fam Physician. 1996;42:1701–8. [PMC free article] [PubMed] [Google Scholar]
- 60.Black AT. Cervical cancer screening strategies for aboriginal women. Pimatisiwin. 2009;7:157–80. [Google Scholar]
- 61.Clarke HF, Joseph R, Deschamps M, Hislop TG, Band PR, Atleo R. Reducing cervical cancer among First Nations women. Can Nurse. 1998;94:36–41. [PubMed] [Google Scholar]
- 62.Giuliano A, Papenfuss M, de Guernsey de Zapien J, Tilousi S, Nuvayestewa L. Breast cancer screening among southwest American Indian women living on-reservation. Prev Med. 1998;27:135–43. doi: 10.1006/pmed.1997.0258. [DOI] [PubMed] [Google Scholar]
- 63.Tatemichi S, Miedema B, Leighton S. Breast cancer screening. First Nations communities in New Brunswick. Can Fam Physician. 2002;48:1084–9. [PMC free article] [PubMed] [Google Scholar]
- 64.Demers AA, Decker KM, Kliewer EV, et al. Mammography rates for breast cancer screening: a comparison of First Nations women and all other women living in Manitoba, Canada, 1999–2008. Prev Chronic Dis. 2015;12:E82. doi: 10.5888/pcd12.140571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cancer Care Ontario, Department of Prevention and Screening . Aboriginal Cancer Strategy: Honouring the Aboriginal Path of Well-being. Toronto, ON: Cancer Care Ontario; n.d. [Available online at: https://www.cancercare.on.ca/common/pages/UserFile.aspx?fileId=72830; cited 28 December 2014] [Google Scholar]
- 66.Northwest Territories (nwt), Health and Social Services . Cancer in the Northwest Territories 1990–2000: A Descriptive Report. Yellowknife, NT: NWT, Health and Social Services; 2003. [Available online at: http://pubs.aina.ucalgary.ca/health/60744E.pdf; cited 1 June 2015] [Google Scholar]
- 67.Canadian Partnership Against Cancer (cpac) First Nations, Inuit and Métis Action Plan on Cancer Control. Toronto, ON: CPAC; 2011. [Available online at: http://www.cancerview.ca/idc/groups/public/documents/webcontent/fnim_action_plan_nov11.pdf; cited 23 November 2013] [Google Scholar]
- 68.Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000;57(suppl 1):181–217. doi: 10.1177/107755800773743655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Brach C, Fraser I. Reducing disparities through culturally competent health care: an analysis of the business case. Qual Manag Health Care. 2002;10:15–28. doi: 10.1097/00019514-200210040-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mitchell S. Tobacco Cessation Strategies for First Nations, Inuit and Métis: An Environmental Scan and Annotated Bibliography. Prince George, BC: National Collaborating Centre for Aboriginal Health; 2007. [Available online at: http://nbatc.ca/en/uploads/Aboriginal%20ActNow%20Tobacco%20Report%20-%20Final%20April%20.2009.pdf; cited 4 June 2015. [Google Scholar]
- 71.Centre for Rural and Northern Health Research (crnhr) Exploring the Socio-economic Impact of the Northern Ontario School of Medicine. Thunder Bay and Sudbury, ON: CRNHR; 2009. [Available online at: https://www.nosm.ca/uploadedFiles/About_Us/Media_Room/Publications_and_Reports/FINAL_Report_%28NOSM_Socioeconomic_Impact_Study-2009-11%29.pdf; cited 4 June 2015] [Google Scholar]
- 72.Jacklin K, Strasser R, Peltier I. From the community to the classroom: the aboriginal health curriculum at the Northern Ontario School of Medicine. Can J Rural Med. 2014;20:143–50. [PubMed] [Google Scholar]
- 73.Cooper LA, Beach MC, Johnson RL, Inui TS. Delving below the surface: understanding how race and ethnicity influence relationships in health care. J Gen Intern Med. 2006;21(suppl 1):S21–7. doi: 10.1111/j.1525-1497.2006.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


