Abstract
Background
During radiotherapy for breast cancer, patients are greatly affected by pain, infection, and delayed healing of wounds caused by radiodermatitis. In the present study, we aimed to determine the efficacy of Liu-He-Dan in treating radiodermatitis.
Methods
In 26 breast cancer patients who experienced moist decrustation while receiving radiotherapy, 5 g Liu-He-Dan was applied externally once daily after the wound surface had been cleaned and dried. The healing time was recorded, and a Kaplan–Meier survival curve was applied to analyze the treatment course. Meanwhile, a pain assessment using the Numeric Rating Scale (nrs) recorded the pain level experienced by patients after application of the Liu-He-Dan.
Results
After application of Liu-He-Dan, the average healing time for the surface of the moist decrustation wounds was 14.17 ± 2.03 days (range: 5–22 days). Inflammatory seepage decreased significantly and exudation almost disappeared in 3 days. The pain trend line indicated that the average nrs score declined with treatment in all patients. The average nrs scores at days 1, 4, and 7 were 6.13, 3.62, and 2.58 respectively. After 3 days of treatment, pain was remarkably alleviated in 80.76% of patients. After treatment for 1 week, the pain remission rate was 96.15%, without any obvious adverse reactions.
Conclusions
Liu-He-Dan was efficacious in treating radiation skin injury with little toxicity and few side effects; the economic efficiency of the treatment was also favourable. The Liu-He-Dan was generally well tolerated by patients. In future, randomized control trials will be established for further observation of the value of Liu-He-Dan in treating radiodermatitis in breast cancer.
Keywords: Liu-He-Dan, radiodermatitis, breast cancer
INTRODUCTION
Breast cancer, a malignant tumour with high morbidity in women, ranks as the 2nd most frequent in women in developing countries, including China1. Radiotherapy to the wall of the chest is an important adjuvant therapy for some breast cancer patients after surgery. With progress in radiotherapy techniques, the local breast cancer recurrence rate has declined, and lifespans have been prolonged. However, patients still experience various adverse reactions during therapy, with radiodermatitis occurring in most cases.
Radiodermatitis manifests as varying degrees of erythema, dry or moist decrustation, ulceration, and the like2,3. Among patients who have received concurrent radio-chemotherapy, the radiodermatitis occurrence rate is relatively high and can reach 46%4. This adverse reaction not only leads to an increased risk of local skin lesions, pain, and infection, but can also result in ulceration and delayed healing if not treated in a timely manner. Some women undergo a second operation or skin grafting, which severely affects the process of radiotherapy, lowers the therapeutic effect, and at the same time imposes an additional physical or psychological trauma and economic burden for patients. Although radiodermatitis, especially moist decrustation, is very common and causes great harm, a uniform standard therapy for treating the complication is still lacking.
Traditional Chinese Medicine (tcm) for dermatitis combines many kinds of Chinese herbs to exploit their strengths and avoid their shortcomings, with the aim of promoting circulation so as to address blood stasis, inflammation, and tumescence and to reduce side effects. In the present study, 26 breast cancer patients who presented with moist decrustation after radiotherapy were treated with Liu-He-Dan, a traditional Chinese herbal paste, with the aim of observing its therapeutic effects on adverse reactions such as pain and inflammation.
METHODS
Clinical Data
From January 2011 to March 2014, 26 breast cancer patients who had received adjuvant radiotherapy after surgery were recruited. Patients who might be sensitive to components of tcm were excluded, as were women who were pregnant or breastfeeding. All patients participated in the clinical trial voluntarily and had the right to withdraw at any time. The research conformed to the Declaration of Helsinki and was approved by our institution’s ethics committee.
Radiotherapy targets in the women included the mammary glands, the walls of the chest, and the fossa axillaris. According to the U.S. National Cancer Institute’s Common Terminology Criteria for Adverse Events, version 4.3, all patients developed grade 3 moist decrustation. The administration of tcm in treating radiodermatitis did not influence the course of radiotherapy. If the moist decrustation did not recover during the tcm treatment course, the tcm was stopped and other treatments were adopted to control inflammation.
Radiotherapy
All patients received postoperative adjuvant radiotherapy, and some patients received concomitant chemotherapy. The areas treated with radiotherapy included the operative area, the chest wall, and the lymph gland drainage area. The radiotherapy fractionation schedule was 1.8–2 Gy, once daily for 5 days, followed by 2 days’ rest, to a total of 25 fractions, for a total radiologic dose of 5000 cGy. If necessary, a boost dose was given.
Preparation and Use of Liu-He-Dan
Liu-He-Dan was prepared by the tcm department of the West China Hospital of Sichuan University. Briefly, more than 10 tcms (including but not limited to rheum officinale, golden cypress, radix angelicae, smoked plum, bletilla, mint leaf, Wujinsan, and Chenxiaofen) were dried, ground to a powder, and mixed with water and honey into a paste. Each day, after participants had received their radiotherapy, Liu-He-Dan paste was applied to the area of moist decrustation as next described.
A piece of paper 1–2 cm2 larger than the area of dermatitis was dipped into liquid wax, and a tongue depressor was used to smear 5 g Liu-He-Dan paste onto the paper at a thickness of 0.3–0.5 mm. The paper was then applied to the skin. Subsequently, the surface of the paper was covered with a sterile dressing and then a layer of plastic film. Before the next radiotherapy treatment, the Liu-He-Dan was cleaned away.
The Liu-He-Dan was used continuously after radio-therapy completion. For some patients with obvious exudation, normal saline was used to clean the inflamed area before the Liu-He-Dan was applied. Liu-He-Dan was used once daily until the dermatitis recovered or an adverse reaction occurred.
Assessment
In the treatment of radiodermatitis, the major observational indicator is full recovery from the inflammation. When calculating healing time, moist decrustation should disappear completely, and skin trauma should heal. In the present study, great attention was also paid to inflammatory pain reported by the patients, with improvement in the pain score being considered an effective index. Pain was assessed according to the Numeric Rating Scale (nrs) for pain. This 0–10 score gradually increases from full analgesia to extreme pain, with scores of 1–3 representing mild pain, 4–6 representing moderate pain, and 7–10 representing severe pain. The average nrs scores reported by all patients in the group were compared to track changes after the application of Liu-He-Dan.
Statistical Analysis
The statistical analyses were performed using IBM SPSS Statistics (version 19.0: IBM, Armonk, NY, U.S.A.), and a Kaplan-Meier survival curve was used to assess dermatitis healing time. Alleviation of pain was determined by comparing the average nrs scores on each day.
RESULTS
Of the 26 study participants (age range: 33–71 years), 19 had invasive ductal carcinoma, 3 had carcinoma simplex, 3 had lobular carcinoma, and 1 had carcinoma spongiosum. Table i presents baseline patient information.
TABLE I.
Clinical and treatment characteristics of the study patients
| Characteristic | Value |
|---|---|
| Sex [n (%)] | |
| Women | 26 (100) |
| Men | 0 |
| Age (years) | |
| Median | 56 |
| Range | 33–71 |
| Location of the cancer [n (%)] | |
| Left breast | 16 (61.5) |
| Right breast | 10 (38.5) |
| KPS score | |
| Median | 80 |
| Range | 60–90 |
| Therapy received [n (%)] | |
| Surgery | 26 (100) |
| Chemotherapy | 22 (84.6) |
| Initial | 20 (76.9) |
| Recurrence | 6 (23.1) |
| Radiotherapy dose (cGy) | |
| Median | 5000 |
| Range | 4800–6600 |
| Radiotherapy fractions | |
| Median | 25 |
| Range | 25–34 |
| Pain score on the NRS [n (%)] | |
| Severe (7–10) | 7 (26.9) |
| Moderate (4–6) | 14 (53.8) |
| Mild (1–3) | 5 (19.2) |
| Skin damage area (cm2) | |
| Average | 9.2 |
| Range | 4–21 |
KPS = Karnofsky performance status; NRS = Numeric Rating Scale.
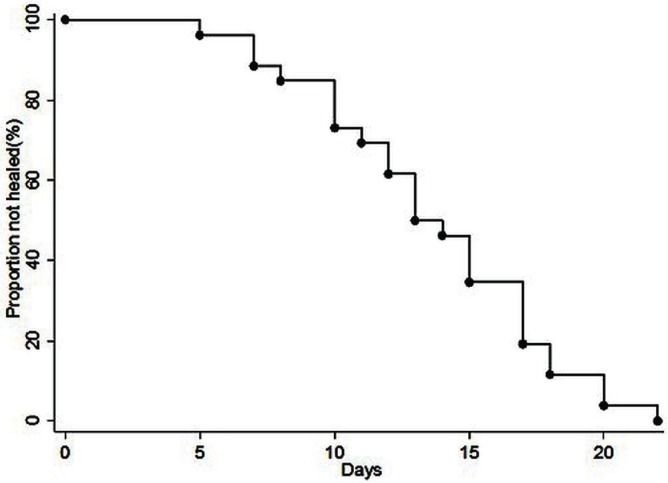
The Kaplan–Meier curve for the radiodermatitis treatment (Figure 1) shows that, after the moist decrustation experienced by these patients had been treated with Liu-He-Dan, patients appeared to heal gradually, with an average healing time of 14.17 ± 2.03 days (range: 5–22 days). Seepage of the inflammatory exudation in treated patients declined and disappeared completely after 3 days.
FIGURE 1.
Kaplan–Meier analysis of the course of radiodermatitis treated with Liu-He-Dan. Patients are seen to heal gradually, with an average healing time of 14.17 ± 2.03 days.
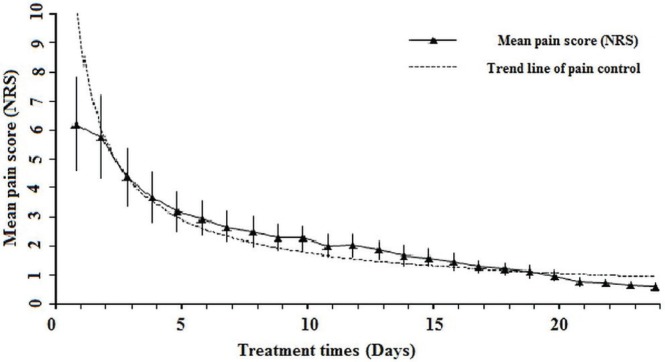
At the beginning of treatment, 7 patients were experiencing severe pain (score: 7–9), for an average nrs score of 8.17; 14 were experiencing moderate pain (score: 4–6), for an average nrs score of 5.42; and 5 patients were experiencing mild pain (score: 1–3) for an average nrs score of 2.31. After the dermatitis was treated with Liu-He-Dan, the overall average nrs score showed a declining trend, with the average scores at days 1, 4, and 7 being 6.13, 3.62, and 2.58 respectively. After treatment for 3 days, pain had been alleviated in 21 patients (80.76%), and after treatment for 1 week, pain had been alleviated in 25 (96.15%, Figure 2).
FIGURE 2.
Effect of Liu-He-Dan in the treatment of radiodermatitis with pain. The average pain score on the Numeric Rating Scale (NRS: 0 = full analgesia, 10 = extreme pain) as reported by the patients was recorded every day. The dotted line shows the pain control trend.
All patients tolerated the treatment well, and no medication-related adverse reactions, including fever, nausea, or vomiting occurred. No obvious adverse reactions in respect of the hematopoietic function of bone marrow, liver or kidney metabolism, or cardiotoxicity were observed. Only 1 patient required extra pain relief (a mild opiate in the form of tramadol in a sustained-release tablet) for 8 days because of failure of pain relief at the start of treatment. The opiate was stopped when the patient’s inflammation was alleviated; Liu-He-Dan treatment was then resumed until the dermatitis healed.
DISCUSSION
Radiotherapy plays a key role in the comprehensive treatment of breast cancer. With the progress of radiotherapy, survival rates have greatly improved. However, adverse reactions such as radiodermatitis occur during therapy and should not be ignored. Inflammatory skin exudation in the irradiation field, delayed wound healing, and pain during radiotherapy can affect treatment tolerance, resulting in interruption of radiotherapy, a prolonged treatment course, and insufficient dose, which directly affects efficacy5.
Skin is a fast-reacting tissue in which radiation can easily induce the production of damaging oxygen radicals. “Acute radiation damage” is defined as skin lesions that appear within 6 months of radiotherapy. Such lesions often occur at 2–3 weeks after therapy and can last for 1 month after completion of therapy6. The severity of the reaction depends on the total radiation dose, the single-fraction dose, therapy time, type and energy of the radiation, and the size of the irradiated area. Early-stage manifestations include local redness, swelling, and congestion. With an increasing radiation dose, those manifestations can gradually develop into dry or moist decrustation, and 20%–25% of patients can experience a more severe reaction, such as unhealed ulceration and fibrosis, which affects skin function7.
Current methods for treating radiodermatitis include cleaning, surgical dressings, and Western medicines such as Biafine (Ortho–McNeil Pharmaceuticals, Titusville, NJ, U.S.A.) and GeneTime (Hua-Shengyuan Gene Pharmaceuticals, Shenzhen, P.R.C.)8–10. Physical methods can also be adopted to reduce wound exudation, thus keeping it dry to promote healing. However, an effective standard therapy is currently lacking. In China, tcm is becoming widely used in the therapy of radiodermatitis.
In the theory of tcm, radioactive lesions are usually caused by excessive heat and toxicity; therapy and prevention should therefore select heat-clearing, detoxifying, tonic- and blood-activating, and stasis-eliminating compounds. Among the components of Liu-He-Dan, golden cypress and rhubarb remove heat and invigorate the circulation of blood, reduce inflammation, and remove stasis. The effective component in golden cypress is berberine, which has broad-spectrum antibacterial effects, directly inhibiting the formation of bacterial coagulase and strengthening the phagocytic ability of the reticuloendothelial system. In the formula, mint leaf is cool in nature, and radix angelicae is warm. Cool combined with warm can stimulate menstrual flow, remove stasis, and invigorate the circulation of blood. When added to the acid of smoked plum, Chenxiaofen can remove stagnation, and honey can clear heat toxicity and alleviate irritation. Lastly, bletilla—with starch, honey, and water as an excipient—forms a soft, glutinous, sticky paste that does not easily dry and is convenient for surface application. It can also open the pores to allow the medicine to permeate the locally inflamed area. Liu-He-Dan is therefore formulated in a way that should resolve hard lumps, clear heat and toxins, and relieving swelling and pain. In China, Liu-He-Dan has been widely used in treating acute pancreatitis and has also been tested in research using a rat pancreatitis model11. Its range of applications are currently being gradually popularized.
In observing the primary efficacy of Liu-He-Dan in the treatment of radiodermatitis, we also found that Liu-He-Dan has little toxicity and few side effects, is well tolerated, and has favourable economic efficiency. In future, a larger number of patients should be studied, and randomized placebo-controlled clinical research should be conducted to further determine the value of Liu-He-Dan in treating radiodermatitis.
CONCLUSIONS
Liu-He-Dan was efficacious in treating skin injury from radiation with low toxicity, few side effects, and favourable economic efficiency. The compound was generally well tolerated by patients experiencing radiodermatitis during treatment for breast cancer.
ACKNOWLEDGEMENTS
This work was financially supported by grants from the Sichuan Scientific Department Program (2011JYZ034) and the Sichuan Province Program (120035). The authors acknowledge the contributions of Dr. Wang Li in the tcm department of West China Hospital.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. CA Cancer J Clin. 2014;64:52–62. doi: 10.3322/caac.21203. [DOI] [PubMed] [Google Scholar]
- 2.Ryu SH, Kim YH, Lee SW, Hong JP. The preventive effect of recombinant human growth factor (rhegf) on the recurrence of radiodermatitis. J Radiat Res. 2010;51:511–17. doi: 10.1269/jrr.10010. [DOI] [PubMed] [Google Scholar]
- 3.Zhang Y, Zhang S, Shao X. Topical agent therapy for prevention and treatment of radiodermatitis: a meta-analysis. Support Care Cancer. 2013;21:1025–31. doi: 10.1007/s00520-012-1622-5. [DOI] [PubMed] [Google Scholar]
- 4.Schnur JB, Love B, Scheckner BL, Green S, Wernicke AG, Montgomery GH. A systematic review of patient-rated measures of radiodermatitis in breast cancer radiotherapy. Am J Clin Oncol. 2011;34:529–36. doi: 10.1097/COC.0b013e3181e84b36. [Erratum in: Am J Clin Oncol 2012;35:166] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olascoaga A, Vilar-Compte D, Poitevin-Chacón A, Contreras-Ruiz J. Wound healing in radiated skin: pathophysiology and treatment options. Int Wound J. 2008;5:246–57. doi: 10.1111/j.1742-481X.2008.00436.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koukourakis GV, Kelekis N, Kouvaris J, Beli IK, Kouloulias VE. Therapeutics interventions with anti-inflammatory creams in post radiation acute skin reactions: a systematic review of most important clinical trials. Recent Pat Inflamm Allergy Drug Discov. 2010;4:149–58. doi: 10.2174/187221310791163099. [DOI] [PubMed] [Google Scholar]
- 7.Benomar S, Boutayeb S, Lalya I, et al. Treatment and prevention of acute radiation dermatitis. Cancer Radiother. 2010;14:213–16. doi: 10.1016/j.canrad.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Costa MM, Silva SB, Quinto AL, et al. Phototherapy 660 nm for the prevention of radiodermatitis in breast cancer patients receiving radiation therapy: study protocol for a randomized controlled trial. Trials. 2014;15:330. doi: 10.1186/1745-6215-15-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Becker-Schiebe M, Mengs U, Schaefer M, Bulitta M, Hoffmann W. Topical use of a silymarin-based preparation to prevent radiodermatitis: results of a prospective study in breast cancer patients. Strahlenther Onkol. 2011;187:485–91. doi: 10.1007/s00066-011-2204-z. [DOI] [PubMed] [Google Scholar]
- 10.Salvo N, Barnes E, van Draanen J, et al. Prophylaxis and management of acute radiation-induced skin reactions: a systematic review of the literature. Curr Oncol. 2010;17:94–112. doi: 10.3747/co.v17i4.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao XL, Xiang J, Wan MH, et al. Effect of acute pancreatitis on the pharmacokinetics of Chinese herbal ointment Liu-He-Dan in anaesthetized rats. J Ethnopharmacol. 2013;145:94–9. doi: 10.1016/j.jep.2012.10.036. [DOI] [PubMed] [Google Scholar]