Abstract
Objectives:
Poisonings and snake bites constitute major health-care problems worldwide. This observational study was conducted to identify factors associated with outcomes in such cases and to suggest strategies to improve them.
Methods:
This is a prospective study conducted in the emergency medicine department of a tertiary care hospital. The study included 102 poisoning and 64 snake bite cases. Data regarding demographics, mode of poisoning, lag time in treatment, first aid, outside and indoor treatment, co-morbid illness, duration of hospitalisation and final outcome were collected in a prestructured proforma.
Results:
The age of the patients ranged from 11 to 68 years and incidence was more common among males (69.9%) compared to females (30.1%). The major types of poisonings included organophosphorus compounds (16.3%), aluminium phosphide (12%), drug overdose (10.8%) and corrosives (6%). There were 18 (18.6%) and 1 (1.6%) deaths in poisoning and snake bite cases, respectively. In poisoning cases, the duration of hospitalisation was significantly decreased if patient received outside treatment (p = 0.02) and if he or she had lesser lag time in reaching the hospital (p = 0.009).
Conclusions:
Measures to reduce lag time and provide immediate treatment at initial encounter may be effective in reducing duration of hospitalisation and possibly mortality in poisoning and snake bite cases.
Keywords: Poisoning, snake bite, antidote, organophosphorus, oxime, drug overdose
Introduction
Poisonings and snake bites constitute a major cause of hospitalisation and mortality in developed as well as developing nations. The severity and outcome in such cases are determined by a number of factors such as chemical and physical properties of the poison, amount consumed, mode of poisoning and individual characteristics like the functional reserve of the individual or target organ, which is further influenced by age and pre-existing disease.
Among the various causes of poisonings, pesticides are the most common cause of self-poisoning worldwide,1–3 with the proportion ranging from 4% in the European region to over 50% in the Western Pacific region.4 Approximately 258,000 fatal cases of pesticide self-poisoning are reported globally each year,4 most from Asia, and the figure is greatly exceeded by the number of poisoned patients who seek treatment at health facilities. Data about the other kinds of poisonings are limited and are quite variable depending on the geographical area, socioeconomic factors and cultural diversity.5–9 In a previous retrospective study from South India, organophosphorus compounds (OPC) were reported as the most common cause of poisoning (36.0%) followed by snake bite (16.2%), drugs (11.0%), rat poison (7.3%) and others.10 Another study from North India also reported OPC and celphos as the most common poisonings although a majority (76.60%) were unknown poisonings.11 Organophosphate compounds were also implicated in 68.7% of the total poisoning-related fatalities in another study.12
Snake bite is also a major problem worldwide. According to estimates, more than 5 million venomous snake bites occur every year, and nearly, 125,000 of those who suffer snake bite die, with the majority of the deaths occurring in the rural population because of inadequate primary treatment and lack of tertiary care facilities.13
The treatment goals in poisoning and snake bite include support of vital signs, prevention of further poison/toxin absorption, enhancement of elimination, administration of antidote and prevention of re-exposure. Besides, to achieve early treatment initiation which is utmost crucial, various first aid steps are practised by people like finger- or saline-induced emesis in poisoning and proximal joint tourniquet application in snake bite cases.
The huge burden of poisoning and snake bite cases demands comprehensive strategies for reducing deaths. Hence, this prospective observational study was conducted with an aim to identify factors related to outcomes in such cases and to suggest strategies to reduce associated morbidity and mortality.
Methods
The study was conducted prospectively in the emergency medicine department of our tertiary care hospital. All patients who presented with any type of poisoning and snake bite from April to October 2009 were included in the study. The patients who were brought dead or died immediately upon arrival before receiving any indoor treatment were excluded. The study was conducted after getting approval from Institute Ethics Committee and confidentiality of data was ensured.
A case of poisoning was defined as the overdose of drugs, medicaments and biological substances and/or a wrong substance given or taken in error (T36-T50, International Statistical Classification of Diseases and Related Health Problems–10th Revision (ICD-10)). A case was considered as snake bite on the basis of history and presentation.
Data obtained included demographic details such as age, sex, marital status, residence, educational qualification, occupation and monthly income. The time of poisoning/snake bite, time of hospital arrival, lag time in reaching the hospital and reasons for the same, brought by whom and mode of transportation were noted down. Data pertaining to diagnosis, any co-morbid illness, any previous history of poisoning, mode of poisoning whether accidental/suicidal/homicidal and any recent precipitating event were also recorded. The patients/attendants were asked about first aid received, the details of first aid, timing and by whom. The records of any outside treatment, setting and qualification of treating doctor were checked. The details of indoor treatment; door-to-needle time (defined as time from hospital arrival to administration of first treatment); requirement of antidote, including reasons for the same; and the availability of antidote, whether in hospital supply or procured by patient were recorded. Finally, the duration of hospital stay and recovery status were noted.
All data were presented as numbers, percentages, mean ± standard deviation (SD) and median (interquartile range (IQR)). Logistic regression and univariate analysis were used to predict the effect of different variables on the outcome and duration of hospital stay, respectively. A p-value < 0.05 was considered statistically significant.
Results
Study population demographics
Approximately 70% patients were males. The age of the patients ranged from 11 to 68 years with a mean (SD) age of 29 (10.53) years. Almost identical representation of the study population from urban and rural areas was noted. Less than one-fourth of the patients were illiterate. There was a wide representation of various occupations among study population. Of all the patients, 19 (11%) were suffering from some co-morbid medical condition (Table 1).
Table 1.
Demographic profile of the patients presenting with poisonings and snake bite.
| N = 166 | |
|---|---|
| Poisonings, n (%) | 102 (61.5) |
| Snake bites, n (%) | 64 (38.5) |
| Age, mean ± SD | 29.1 ± 10.5 |
| Poisonings | 28.6 ± 10.1 |
| Snake bites | 29.8 ± 11 |
| Male/female, n (%) | 116 (69.9)/50 (30.1) |
| Married, n (%) | 92 (55.4) |
| Residence, n (%) | |
| Urban | 66 (39.8) |
| Rural | 100 (60.2) |
| Qualification, n (%) | |
| Illiterate | 38 (22.9) |
| Primary | 45 (27.1) |
| Secondary | 57 (34.3) |
| Graduate | 22 (13.2) |
| Postgraduate | 4 (2.4) |
| Occupation, n (%) | |
| Business | 33 (19.9) |
| Government job | 7 (4.2) |
| Private job | 34 (20.5) |
| Unemployed | 5 (3) |
| Student | 32 (19.3) |
| Housewife | 29 (17.5) |
| Others | 26 (15.7) |
| Monthly income (INR), median (IQR) | 4000 (3000–8000) |
SD: standard deviation; INR: Indian National Rupee; IQR: interquartile range.
Distribution of cases
The distribution of various poisoning and snake bite cases in the studied population is depicted in Figure 1. Poisonings comprised more than 60% of the total cases (102/166; 61.5%). The major types of poisonings included OPC (16.3%), aluminium phosphide/celphos (12%), drug overdose (10.8%) and corrosives (6%). Benzodiazepines (6), acetaminophen (4), opioids (2) and antiepileptics (2) comprised major drug overdoses. Of these, two patients presented with mixed opioid and benzodiazepine overdose and one came with mixed drugs overdose; one patient who was already on digoxin treatment for atrial fibrillation for the last 7 years presented with signs of digoxin toxicity.
Figure 1.
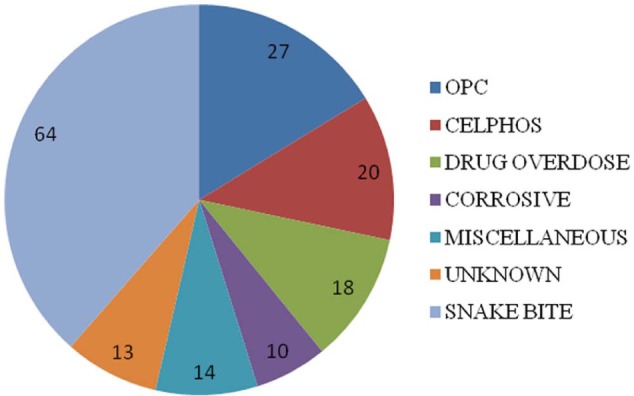
The distribution (numbers) of various poisoning and snake bite cases in the studied population.
OPC: organophosphorus compounds.
Some miscellaneous causes of poisonings (14/166, 8.4%) included zinc phosphide (3), antitermite (2), naphthalene balls (2), organo-chlorine (2), oleander (1), methanol (1), lead (1), copper sulphate (1) and HgCl2 + ethylenediaminetetraacetic acid (EDTA) + NaCl reagent (1). The cause of poisoning could not be determined in few cases (7.2%).
Of the total 166 cases, 64 (38.5%) presented with snake bite: neurotoxic (35), vasculotoxic (9) and non-specific (20).
Proximal joint tourniquet application at home was done in 39% snake bite cases (25/64), while few patients with poisonings (12/102; 11.7%) received first aid in the form of finger insertion in mouth and saline-induced emesis. First aid was mostly administered by some close relative living with the patient. The median (IQR) lag time in hospital arrival in poisoning and snake bite cases was 3 (1.5–7.7) and 3.9 (2.2–7.3) h, respectively. Transportation time and referral from some other hospital were mainly responsible for delay in reaching the hospital. The mode of transportation was ambulance in about half of cases and by personal/private vehicles in remaining. The proportion of suicidal poisonings (48/102; 47%) was substantial and almost similar to accidental (51/102; 50%). History of any recent precipitating event, mainly emotional, was there in >60% suicidal cases (30/48; 62.5%).
Outside treatment
Around 70% of patients in both poisoning (71/102) and snake bite groups (45/64) had received outside treatment by graduate/postgraduate doctors in private/civil/government hospital settings. Outside treatment was mainly in the form of lavage, intravenous fluids and injectable antibiotics, inotropes, and so on. A total of 10% of snake bite patients (6/64) had received anti-snake venom, while antidote (pralidoxime) was given in more than 20% of OPC poisonings (6/27; 22.2%).
Indoor treatment
The median (IQR) door to needle time was 32.5 (29.25–55) and 35 (30–52.5) min in poisoning and snake bite cases, respectively. Polyvalent anti-snake venom was given in 90% snake bite patients (58/64); rest of the patients had received it outside. Depending on the case, the number of vials of antivenom administered ranged from 1 to 6 (median: 3). In poisoning cases, only 26 patients received antidote (26/102; 25.5%) (Table 2). Atropine, being the major drug to reverse the cholinergic symptoms, was prescribed to all patients with OPC poisonings. Anti-snake venom was available in hospital supply, while in other poisoning cases, the antidote was procured by the patient.
Table 2.
Antidotes given indoor in various poisoning cases.
| Poisoning (N, %) | Antidote (N) |
|---|---|
| Drug overdose (14/18; 77.8%) | |
| Acetaminophen | N-acetyl cysteine (4) |
| Opioids | Naloxone (2) |
| Benzodiazepine | Flumazenil (6) |
| Mixed opioids and benzodiazepine | Naloxone + flumazenil (2) |
| OPC (10/27; 37%) | Pralidoxime |
| Copper sulphate (1/1; 100%) | BAL |
| Lead (1/1; 100%) | BAL |
BAL: British anti-lewsite; OPC: organophosphorus compounds.
Effect of various factors on patient outcome and duration of hospital stay
We studied the effect of various confounding factors (e.g. age, sex, any first aid, any outside treatment and lag time in reaching the hospital and in receiving treatment after arrival in hospital) on outcome and duration of hospital stay in all cases.
Poisoning
A total of 18 patients out of 102 (18.6%) poisoning cases died, mostly because of cardiopulmonary arrest. For outcome, none of the factors showed statistically significant results, although the odds ratios for male gender (0.843; 95% confidence interval (CI): 0.265, 2.679), receipt of first aid (0.421; 95% CI: 0.045, 3.939) and any outside treatment (0.918; 95% CI: 0.284, 2.964) demonstrated a trend towards increased chances of survival (Table 3).
Table 3.
Logistic regression analysis of poisoned patients for outcome.
| Predictor | B | SE | Wald | Df | Sig. | Exp (B) | 95% CI for exp (B) |
|---|---|---|---|---|---|---|---|
| Constant | −0.982 | 1.098 | 0.800 | 1 | 0.371 | 0.374 | NA |
| Groups | −0.247 | 0.186 | 1.775 | 1 | 0.183 | 0.781 | 0.543, 1.124 |
| Age | 0.028 | 0.025 | 1.294 | 1 | 0.255 | 1.029 | 0.98, 1.08 |
| Sex | −0.171 | 0.59 | 0.084 | 1 | 0.772 | 0.843 | 0.265, 2.679 |
| First aid | −0.864 | 1.14 | 0.574 | 1 | 0.449 | 0.421 | 0.045, 3.939 |
| Arrival lag | −0.002 | 0.009 | 0.071 | 1 | 0.79 | 0.998 | 0.98, 1.015 |
| Outside Rx | −0.086 | 0.598 | 0.02 | 1 | 0.886 | 0.918 | 0.284, 2.964 |
| Indoor lag | 0.000 | 0.005 | 0.002 | 1 | 0.963 | 1.000 | 0.991, 1.009 |
| Model summary section | |||||||
| −2 log likelihood | 91.464 | ||||||
| Cox & Snell R2 | 0.049 | ||||||
| Nagelkerke R2 | 0.078 | ||||||
| Test | Chi-square | Df | p-value | ||||
| Omnibus test of model coefficients | 4.928 | 7 | 0.669 | ||||
| Hosmer and Lemeshow’s goodness-of-fit test | 4.632 | 8 | 0.796 | ||||
| Classification table | |||||||
| Observed | Predicted |
||||||
| Recovered | Died | % Correct | |||||
| Recovered | 79 | 0 | 100 | ||||
| Died | 19 | 0 | 0 | ||||
| Overall percentage | 80.6 | ||||||
| Cut value = 0.500 | |||||||
CI: confidence interval; Df: degrees of freedom.
Out of the various determinants (for corrected model: F = 2.741; p = 0.017), shorter lag time in reaching the hospital was found to directly correlate with duration of hospital stay (F = 7.053; p = 0.009). Any treatment initiated outside was also found to significantly decrease the duration of hospital stay (F = 5.269; p = 0.02).
Snake bite
There was one mortality (1.6%) due to cardiac arrest among all snake bite cases. Statistical assessment of factors influencing outcome was not carried out. Out of the various determinants (for corrected model: F = 1.255; p = 0.293), only receipt of outside treatment showed a trend towards decreasing the duration of hospital stay although this also could not achieve statistical significance (F = 2.978; p = 0.09).
Discussion
This study intended to look into the factors which may be modified to improve outcomes and duration of hospital stay in poisoning and snake bite cases apart from studying their profile characteristics.
In poisoning cases, we noticed a trend for better survival chances in patients who had received first aid at home and some outside treatment before reaching hospital, which was statistically nonsignificant. The receipt of outside treatment, however, significantly decreased the duration of hospitalisation in poisoning cases, thereby implying the need and importance of early treatment in these cases. The duration of hospital stay also had a direct correlation with lag time in reaching the hospital. Hence, there is a need to strengthen the importance of first aid and develop adequate strategies to improve the quality of treatment prior to referral to higher centre. Early access to treatment, increasing community health awareness and counselling can prove to be useful steps in this direction.
In poisoning cases, a trend towards increased chances of survival, although not to a significant extent, was observed in males. This was in contrast to the findings by Eddleston et al.14 who reported male gender and increasing age to be associated with fatal outcome in pesticide self-poisoning cases. However, this observation was explained by the higher incidence of alcohol consumption in their population as co-ingestion of alcohol increases the risk of aspiration, coma and respiratory failure. The findings observed may not be applicable to our small study population. However, delay in receiving medical help in females might be postulated as one of the reasons for higher mortality.
Despite the current controversial role of oximes in OPC poisonings and an insufficient evidence for their benefit-risk ratio,15–17 pralidoxime was used in the management of 37% (10/27) OPC poisoning cases. Considering the high cost of pralidoxime, there is a need for evidence generation regarding pralidoxime use in OPC poisoning. For other poisonings, appropriate antidotes were prescribed according to the recommendations. The rational use of antidotes requires correct diagnosis and supportive evidence for their use. Prompt availability of antidotes is a matter of concern. Hence, strategies need to be implemented in order to improve the affordability and availability of antidotes, and improved evidence for their use in order to ensure a rational and cost-effective approach.
Legislative measures to enforce the use of pesticides with low human toxicity and slow onset of action, reducing the bottle size and pesticide concentration might be helpful in decreasing the associated mortality burden. Implementation of integrated pest and vector management practices will reduce pesticide use in rural communities and therefore reduce their availability for self-harm. Also, steps can be taken to educate public about pesticide use and its harmful effects on body systems. Besides, there is a continuous need to provide a more locally available and affordable hospital care at community level.
Conclusion
The huge burden of poisoning and snake bite cases encountered in emergency department demands the identification of factors causing high mortality and implementation of comprehensive strategies to improve outcomes. Few appropriate measures observed in this study include early referral to hospital and provision of first aid. Besides, legislative measures to reduce hazards associated with pesticide use need to be enforced. Also, there is a need to improve techniques for early and accurate diagnosis in poisoning cases for provision of prompt and adequate treatment and to improve evidence for ensuring the rational and more cost-effective use of antidotes.
Footnotes
Declaration of conflicting interests: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Bertolote JM, Fleischmann A, Butchart A, et al. Suicide, suicide attempts and pesticides: a major hidden public health problem. Bull World Health Organ 2006; 84: 260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Khan NA, Rahman A, Sumon SM, et al. Pattern of poisoning in a tertiary level hospital. Mymensingh Med J 2013; 22: 241–247. [PubMed] [Google Scholar]
- 3. Mandour RA. Environmental risks of insecticides cholinesterase inhibitors. Toxicol Int 2013; 20: 30–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gunnell D, Eddleston M, Phillips MR, et al. The global distribution of fatal pesticide self-poisoning: systematic review. BMC Public Health 2007; 7: 357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Das RK. Epidemiology of insecticide poisoning at A.I.I.M.S Emergency Services and role of its detection by gas liquid chromatography in diagnosis. Med Leg Update 2007; 7: 49–60. [Google Scholar]
- 6. Unnikrishnan B, Singh B, Rajeev A. Trends of acute poisoning in south Karnataka. Kathmandu Univ Med J 2005; 3: 149–154. [PubMed] [Google Scholar]
- 7. Dash SK, Aluri SR, Mohanty MK, et al. Sociodemographic profile of poisoning cases. JIAFM 2005; 27: 133–138. [Google Scholar]
- 8. Srivastava A, Peshin SS, Kaleekal T, et al. An epidemiological study of poisoning cases reported to the National Poisons Information Centre, All India Institute of Medical Sciences, New Delhi. Hum Exp Toxicol 2005; 24: 279–285. [DOI] [PubMed] [Google Scholar]
- 9. Thomas M, Anandan S, Kuruvilla PJ, et al. Profile of hospital admissions following acute poisoning – experiences from a major teaching hospital in south India. Adverse Drug React Toxicol Rev 2000; 19: 313–317. [PubMed] [Google Scholar]
- 10. Ramesha KN, Rao KB, Kumar GS. Pattern and outcome of acute poisoning cases in a tertiary care hospital in Karnataka, India. Indian J Crit Care Med 2009; 13: 152–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Garg R, Aggarwal S, Singh H, et al. Study of the relation of clinical and demographic factors with morbidity in a tertiary care teaching hospital in India. Int J Crit Illn Inj Sci 2013; 3: 12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kanchan T, Menezes RG, Kumar TS, et al. Toxicoepidemiology of fatal poisonings in Southern India. J Forensic Leg Med 2010; 17: 344–347. [DOI] [PubMed] [Google Scholar]
- 13. Aggarwal P, Jamshed N. What’s new in emergencies, trauma, and shock? Snake envenomation and organophosphate poisoning in the emergency department. J Emerg Trauma Shock 2008; 1: 59–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Eddleston M, Buckley NA, Gunnell D, et al. Identification of strategies to prevent death after pesticide self-poisoning using a Haddon matrix. Inj Prev 2006; 12: 333–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Peter JV, Moran JL, Graham P. Oxime therapy and outcomes in human organophosphate poisoning: an evaluation using meta-analytic techniques. Crit Care Med 2006; 34: 502–510. [DOI] [PubMed] [Google Scholar]
- 16. Buckley NA, Eddleston M, Szinicz L. Oximes for acute organophosphate pesticide poisoning. Cochrane Database Syst Rev 2005; 1: CD005085. [DOI] [PubMed] [Google Scholar]
- 17. Eddleston M, Szinicz L, Eyer P, et al. Oximes in acute organophosphorus pesticide poisoning: a systematic review of clinical trials. QJM 2002; 95: 275–283. [DOI] [PMC free article] [PubMed] [Google Scholar]


