Abstract
Background:
Ulnar collateral ligament reconstruction (UCLR) is a common procedure in both professional and high-level athletes.
Purpose:
To determine the effect of technique and level of play with UCLR on return to sport (RTS).
Hypothesis:
When comparing different surgical techniques or preoperative level of sports participation, there is no difference in rate of RTS after UCLR.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review was registered with PROSPERO and performed following PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines using 3 publicly available free databases. Therapeutic clinical outcome investigations reporting UCLR outcomes with level of evidence 1 through 4 were eligible for inclusion. All study, subject, and surgical technique demographics were analyzed and compared between continents and countries. Descriptive statistics were calculated, and 2-proportion 2-sample z-test calculators with α = .05 were used to compare RTS between level of play and technique.
Results:
Twenty studies (2019 patients/elbows; mean age, 22.13 ± 4 years; 97% male; mean follow-up, 39.9 ± 16.2 months) were included. The majority of patients were baseball players (94.5%), specifically pitchers (80%). The most common level of play was collegiate (44.6%). Palmaris longus (71.2%) and the American Sports Medicine Institute (ASMI) technique (65.6%) were the most common graft choice and surgical technique, respectively. There was a pooled 86.2% RTS rate, and 90% of players scored excellent/good on the Conway-Jobe scale. RTS rates were higher among collegiate athletes (95.5%) than either high school (89.4%, P = .023) or professional athletes (86.4%, P < .0001). RTS rates were higher for the docking technique (97.0%, P = .001) and the ASMI technique (93.3%, P = .0034) than the Jobe technique (66.7%).
Conclusion:
UCLR is performed most commonly in collegiate athletes. Collegiate athletes have the highest RTS rate after UCLR of all levels of competition. The docking and ASMI techniques had higher RTS rates than the Jobe technique.
Keywords: ulnar collateral ligament (UCL) reconstruction, Tommy John, elbow, baseball, pitcher, return to sports (RTS) rate
Ulnar collateral ligament reconstruction (UCLR) is a proven treatment option for patients with a symptomatic, deficient ulnar collateral ligament (UCL), particularly in the overhead throwing athlete.6,33 Over the past 10 to 15 years, the number of UCLRs performed on both professional as well as high school and college-level athletes and baseball pitchers has significantly increased.6,15 While the reason for the increase in the number of UCLRs is unknown, risk factors for sustaining a UCL tear have been identified and include glenohumeral internal rotation deficit, pitching more than 100 innings per year, pitching year round, and growing up in warm weather states, among others.10,16,17
Since the initial description of UCLR by Dr Frank Jobe in 1986, there have been several modifications to this technique.4,5,19,23,43 These modifications have included different surgical approaches, such as splitting the flexor pronator mass, different graft fixation methods such as interference screws, and different graft configurations.4,19,23,37 While biomechanical studies have shown promising results from these techniques, comparative clinical data are lacking.20,21,30 Furthermore, while the historic results of UCLR have generally been accepted as good, no recent studies have stratified clinical outcomes by technique and athletic level.4,7,23
The purpose of this study was to determine the effect of technique and preoperative level of play on return to sport (RTS) after UCLR. The authors hypothesize that there is no difference in RTS rate with regard to preoperative athletic level or surgical technique after UCLR.
Methods
A systematic review was conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines using a PRISMA checklist.26 Systematic review registration was performed using the PROSPERO international prospective register of systematic reviews (registration number CRD42015016494).42 Two reviewers independently conducted the search on April 8, 2015, using the following databases: Medline, Cochrane Central Register of Controlled Trials, SportDiscus, and CINAHL. The electronic search citation algorithm utilized was the following: (((ulnar collateral ligament) NOT thumb) NOT hand). Studies reporting treatment of UCL injuries with UCLR or UCL repair until April 8, 2015, were eligible for inclusion. English-language clinical studies of evidence levels 1 through 4 (2011 update by the Oxford Centre for Evidence-Based Medicine41) were eligible for inclusion. All references within included studies were cross-referenced for inclusion if missed by the initial search. Studies from every country, provided they were written in English, were eligible for inclusion. If duplicate subject populations were found, the study reporting the greater number of subjects was used for inclusion. Level 5 evidence reviews, letters to the editor, reviews of topics or of public databases, and basic science, biomechanical, cadaver, non-UCLR open elbow surgery, imaging, surgical technique, and classification studies were excluded.
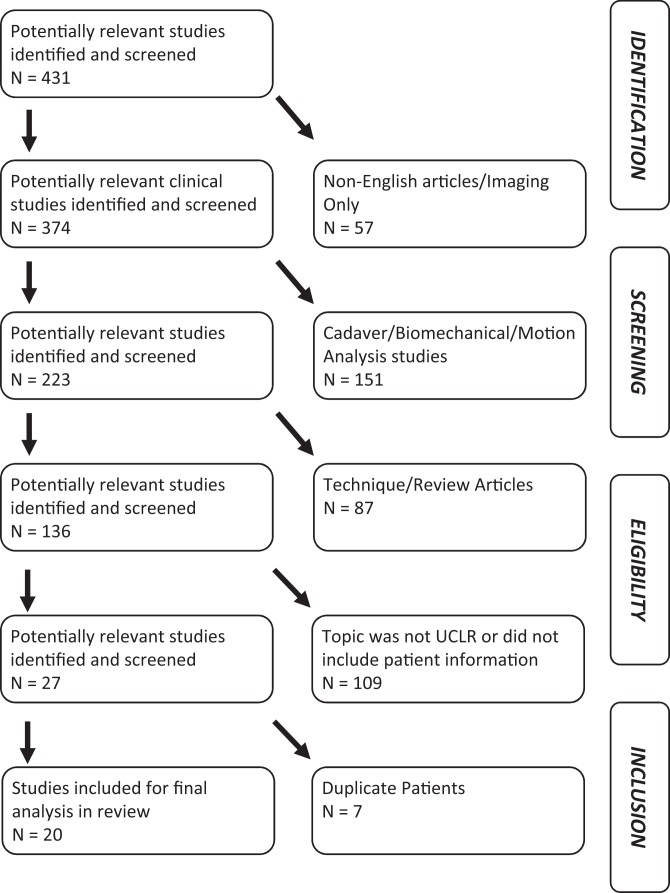
A total of 431 studies were located, and, after implementation of the inclusion criteria, 20 studies were included in the final analysis (Figure 1). Patients of interest in this systematic review underwent either primary or revision UCLR or UCL repair for a symptomatic, deficient UCL. There was no minimum follow-up or specific rehabilitation requirement. Study and subject demographic parameters analyzed included year of publication, years of subject enrollment, presence of study financial conflict of interest, number of subjects and elbows, sex, age, surgical technique, graft choice, presence/absence of preoperative ulnar nerve symptoms, whether the ulnar nerve was transposed intraoperatively, whether arthroscopy was performed, and whether any concomitant procedures were performed. Clinical outcome measures included RTS rates, Conway-Jobe score, Timmerman and Andrews score, and Kerlan-Jobe Orthopaedic Clinic shoulder and elbow score (KJOC). Complications were recorded. Study methodological quality was evaluated using the Modified Coleman Methodology Score (MCMS).8
Figure 1.
PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) flowchart. UCLR, ulnar collateral ligament reconstruction.
Statistical Analysis
All analyses were conducted using Excel X (Microsoft) and SPSS 21 (IBM). Data were extracted from sources in their original form. Descriptive statistics were calculated with mean ± SDs weighted by sample size. Return-to-play rates were subdivided based on level of play (high school, collegiate, and professional) and technique (American Sports Medicine Institute [ASMI] modification, Docking, Jobe, modified Jobe, modified Docking, hybrid, and DANE-TJ [David Altcheck, Neal ElAttrache, Tommy John]). The ASMI modification of the Jobe technique involves 3 differences from the original technique described by Dr Frank Jobe: (1) the flexor pronator mass is retracted anteriorly rather than detached, (2) all patients undergo concomitant elbow arthroscopy to confirm valgus instability, and (3) the ulnar nerve is transposed subcutaneously instead of submuscularly.4,7,23 Only those techniques reported by at least 3 studies were included, with the exception of the ASMI modification of the Jobe technique due to the size of the series reporting outcomes with this technique. The docking and modified docking techniques were combined, as were the Jobe and modified Jobe techniques as these modifications are relatively subtle. Two-proportion, 2-sample z-test calculators were used with α = .05. These tests allow comparison with a difference in sample sizes between the groups compared.
Results
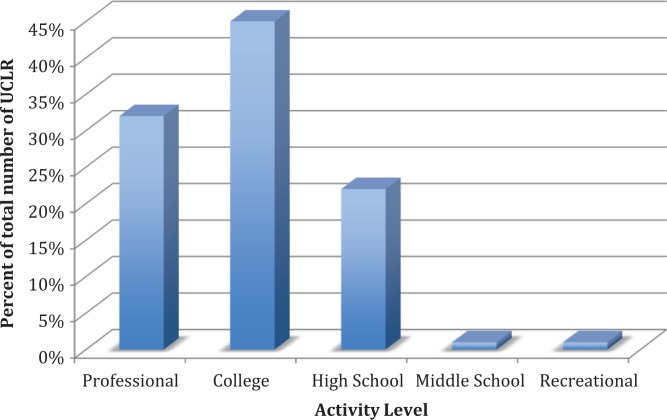
Twenty studies met inclusion and exclusion criteria.‡ Overall study quality was low; all included studies were single-center retrospective case series (level 4 evidence). Of all studies included, 95% were published from the United States, while 1 study was from Asia. With regard to conflicts of interest, 75% of studies had no conflict of interest, 20% had a conflict of interest present, and 5% did not mention whether a conflict of interest existed. Results did not differ based on presence/absence of conflict of interest. Of the included studies, the mean MCMS was 34.7 ± 5.2.8 Total number of included patients was 2019 (one-third of whom came from a single study6), of whom 97.4% were male, 1998 (99%) were primary surgeries, and 1929 (95.5%) were reconstructions instead of repairs. The mean age was 21.4 ± 1.7 years. The mean follow-up was 40.3 ± 9.7 months. Of the included patients, 94.5% were baseball players and 79.6% were pitchers. The remainder were athletes in a variety of other overhead sports (Table 1). Athletes were from a variety of skill levels, with 862 (44.6%) collegiate athletes, 613 (31.7%) professional athletes, 437 (22.6%) high school athletes, 13 (0.7%) middle school athletes, and 7 (0.4%) recreational athletes (Figure 2). Preoperative ulnar neuropathy was encountered in 363 (18.0%) cases.
Table 1.
Patients in Nonbaseball Sports Who Underwent Ulnar Collateral Ligament Reconstruction
| Sport | No. of Athletes | % of Nonbaseball Cohort |
|---|---|---|
| Gymnastics | 7 | 6.7 |
| Lacrosse | 1 | 1.0 |
| Golf | 1 | 1.0 |
| Football | 17 | 16.3 |
| Hockey | 1 | 1.0 |
| Javelin | 38 | 36.5 |
| Basketball | 2 | 1.9 |
| Soccer | 2 | 1.9 |
| Wrestling | 2 | 1.9 |
| Divers | 1 | 1.0 |
| Softball | 11 | 10.6 |
| Tennis | 11 | 10.6 |
| Cheerleaders | 9 | 8.7 |
| Pole vaulting | 1 | 1.0 |
Figure 2.
Percentage of ulnar collateral ligament reconstructions (UCLRs) performed by athletic level.
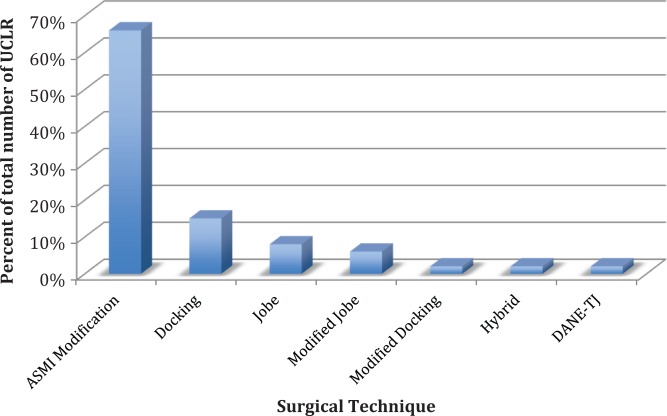
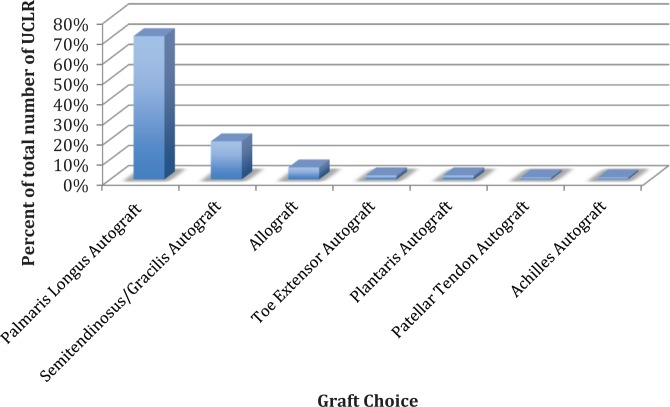
Surgical technique varied between studies. Some of the differences between techniques can be found in Table 2.3,7,9,19,29,37,43 The ASMI variation of the Jobe technique3 was the most frequently utilized (1266, 65.6%), with the Docking technique37 being the second most frequently reported (293, 15.1%), the Jobe technique7 being the third most frequently reported (144, 7.4%), and the modified Jobe technique43 being the fourth most frequently reported (115, 6.0%) (Figure 3). Graft choice also varied from study to study, with palmaris longus autograft being the most frequently reported (1378, 71.2%), hamstring autograft being the second most frequently reported (372, 19.2%), and allograft being the third most frequently reported (118, 6.0%) (Figure 4). Most patients underwent both concomitant ulnar nerve transposition (1411, 69.9%) and concomitant elbow arthroscopy (1553, 76.9%). Other concomitant procedures, primarily posteromedial olecranon osteophyte excision, were also commonly reported (509, 25.2%).
Table 2.
Differences Between Ulnar Collateral Ligament Reconstruction Surgical Techniquesa
| Technique | Ulna | Humerus | Ulnar Fixation | Humeral Fixation | Graft Configuration | Management of FP Mass | Management of Ulnar Nerve | Routine Arthroscopy |
|---|---|---|---|---|---|---|---|---|
| Jobe | Tunnel | Tunnel | None | Sutured to itself | Figure-of-8 | Transection | Submuscular transposition | No |
| Modified Jobe | Tunnel | Tunnel | None | Sutured to itself | Figure-of-8 | Split | Only if symptomatic | No |
| Docking | Tunnel | Socket | None | Sutured over bone bridge | Triangle | Split | Only if symptomatic | Yes |
| Modified Docking | Tunnel | Socket | None | Sutured and graft over bone bridge | Figure-of-8 | Split | Only if symptomatic | No |
| DANE-TJ | Socket | Socket | Interference screw | Docking over bone bridge | Linear | Split | Only if symptomatic | No |
| Hybrid | Tunnel | Anchor | None | Suture anchor, sutured to itself | Triangle | Split | Only if symptomatic | No |
| ASMI modification | Tunnel | Tunnel | None | Sutured to itself | Figure-of-8 | Split | Subcutaneous transposition | Yes |
aASMI, American Sports Medicine Institute; DANE-TJ, David Altcheck, Neal ElAttrache, Tommy John; FP, flexor-pronator.
Figure 3.
Percentage of ulnar collateral ligament reconstructions (UCLRs) performed by surgical technique. ASMI, American Sports Medicine Institute; DANE-TJ, David Altcheck, Neal ElAttrache, Tommy John.
Figure 4.
Percentage of ulnar collateral ligament reconstructions (UCLRs) performed by graft choice.
Outcomes were generally excellent; 1797 (86.2%) were able to return to play. Of those studies that reported outcomes using the Conway-Jobe rating system,7,40 82% of patients had excellent outcomes, 8% had good outcomes, 6% had fair outcomes, and 4% had poor outcomes. Other standardized outcome scores were infrequently reported, with only 2 studies reporting Timmerman-Andrews scores44 with a mean final follow-up score of 87.5 ± 6.5.24,25 Only 2 studies reported Kerlan-Jobe Orthopaedic Clinic scores,2 with a mean final follow-up score of 83.5 ± 5.8.24,33 Complications were infrequent (213, 10.4%), with transient ulnar neuritis being the most frequently encountered (159, 75.4% of complications) followed by donor site issues including pain, wound dehiscence, weakness, and paresthesia (27, 12.8% of complications), the need for revision UCLR (14, 6.6%), stiffness (6, 2.8%), reactive synovitis (3, 1.4%), postoperative hematoma (2, 0.9%), and ulnar tunnel fracture (2, 0.9%). The need for subsequent elbow surgery was infrequent (94, 4.7%), with most revision surgery performed for osteophyte excision (59, 62.8%).
When rates of return to play were compared between levels of play, collegiate athletes (95.5%) were more likely to return to play than either high school (89.4%, P = .023, z = –2.28) or professional athletes (86.4%, P < .0001, z = 4.36). Rates of return to play did not differ between high school and professional athletes (P = .346, z = 0.942). When rates of return to play were compared between techniques, both the docking technique (97.0%, P = .001, z = 3.28) and the ASMI technique (93.3%, P = .0034, z = 2.93) had higher rates of return to play than the Jobe technique (66.7%). The docking technique had a higher rate of return to play than the ASMI technique (P = .056, z = –1.92), but the difference did not reach statistical significance. Return to play rates could not be differentiated based on position as some studies did not separate out pitchers from nonpitchers in their results. Two studies reported results of both UCLR and UCL repair.6,7 Results for repair were inferior to reconstruction in these 2 studies6,7; however, results of only UCL repair by Savoie et al39 showed good to excellent results in 93% of patients. Many studies did not stratify results based on graft choice or treatment of the ulnar nerve, so differences in RTS rates between these variables could not be assessed.
Discussion
Ulnar collateral ligament reconstruction has become a common treatment for patients with symptomatic, deficient UCL tears. The purpose of this review was to determine the overall patient demographic, RTS rate, most common graft choice, most common surgical technique, and complication rate after UCLR. The results of this study indicate that the majority of patients who underwent a UCLR were male (97%) baseball pitchers (80%), and the most common graft choice was a palmaris longus autograft (71.2%), with the ASMI modification of the Jobe technique as the most common surgical technique (65.6%). The overall RTS rate was 86.2% while the complication rate was 10.5%, although the majority of these complications involved transient ulnar neurapraxia (75.4%). Contrary to our hypothesis, collegiate athletes (95.5%) had a higher RTS rate than either high school (89.4%) or professional athletes (86.4%), and the docking (97.0%) and ASMI (93.3%) techniques had higher rates of return to play than the Jobe technique (66.7%).
Vitale and Ahmad45 performed a systematic review of UCLR from 1950 until November 1, 2007. This review included 8 studies, totaling 493 patients—405 of whom underwent UCLR. In the current study, if the literature was isolated from November 2, 2007, until April 8, 2015, an additional 14 studies were available. Hence, in the past 8 years, the number of studies reporting outcomes after UCLR has almost doubled the entire literature of studies from 1950 until November 1, 2007.
There were similarities as well as several differences between the current study and that of Vitale and Ahmad,45 including the demographics of patients undergoing UCLR. An interesting difference between the prior review by Vitale and Ahmad45 and the current study involves the athletic level of patients who underwent UCLR. In the prior study, the majority of UCLRs had been performed in professional athletes (47%), with fewer performed in collegiate athletes (36%), and even fewer performed in high school/recreational athletes (17%).45 In contrast, in the current study, the most common level of play in which UCLR was performed was among collegiate athletes (862 patients, 44.3%), with fewer performed in professional (612, 31.7%) and high school (437, 22.6%) athletes, although the percent of high school athletes has increased since the prior review. Furthermore, UCLR has been reported in middle school (junior high) athletes.39 This trend of younger patients undergoing UCLR is concerning, especially since this trend is a recent phenomenon.
Despite significant efforts at reducing elbow injuries in youth baseball pitchers, including pitch count limitations, increased awareness of elbow injuries, and an attempt to limit pitchers to less than 9 months of pitching per year, injury rates appear to be increasing.17 It is unclear as to why these efforts have been unsuccessful. The current rules may not be stringent enough, or, more likely, youth pitchers, coaches, and parents are not properly following the current guidelines.1,14,17 The task of ensuring adolescent pitchers adhere to these regulations falls on the parents and coaches who may not understand the nature of youth pitcher injuries. Ahmad et al1 surveyed coaches, parents, and players (youth, high school, and collegiate) about their perceptions of UCLR. The authors discovered that the public perception regarding UCLR differs vastly from the current literature. In the study, the majority of those surveyed believed that UCLR increased pitching velocity, accuracy, and performance, and that players would return to play from the surgery in less than 1 year.1,18,22 Unfortunately, these expectations are not supported by the literature to date.15,22,27 Future efforts should be made to ensure compliance with these guidelines.
Within our study, RTS rate for high school athletes (89.4%) was significantly less than that of collegiate athletes (95.5%). High school athletes may not have access to the same rehabilitation resources, training staff, and so on. They may also be more likely to switch sports or give up baseball entirely than collegiate athletes, who have invested more time. Furthermore, high school athletes do not have the ability to obtain a medical redshirt as in college, so if a senior in high school undergoes UCLR, they do not get an extra year of eligibility, as is the case in college. The greater heterogeneity in skill level among high school athletes also plays a role, as a majority of high school pitchers will not be sufficiently skilled to play in college.31 Research has shown that the likelihood of a high school baseball player advancing to the collegiate level is 6.8%, while that of a high school baseball player advancing to the professional level is only 0.5%; the likelihood of a college athlete advancing to professional is 9.4%.31 Similar explanations, however, cannot explain the significantly lower rate of return to play among professional athletes, which may be due to the chronic nature of the injury, age of the athlete, higher level of competition, and the higher frequency of concomitant pathology. While our study did find higher RTS rates with the docking (97.0%) and ASMI (93.3%) techniques compared with the Jobe technique (66.7%), the majority of patients across all athletic levels underwent UCLR using the ASMI technique, so surgical technique alone was not the cause of this significantly different RTS rate between athletic levels.
Several potential explanations exist for the improved RTS offered by the docking and ASMI techniques as compared with the Jobe technique. One of these includes how the flexor pronator mass is treated for each technique. While the Jobe technique involves transection of the flexor pronator mass, the ASMI and docking techniques involve splitting the flexor pronator mass.3,7,23,37 Furthermore, the ASMI technique involves a subcutaneous transposition and a routine elbow arthroscopy while the Jobe technique calls for a submuscular ulnar nerve transposition and does not include a routine elbow arthroscopy. The docking technique, however, does not require an ulnar nerve transposition or a routine elbow arthroscopy. No studies have evaluated the utility of an elbow arthroscopy in UCLR, and as such, the utility of this is unclear. It does seem that based on the results of this study, a split in the flexor pronator mass provides better RTS than transection. The higher complication rate with the original Jobe technique may also play a role in the lower RTS rate.46 In addition, many studies using the Jobe technique were published early on in the development of UCLR, and there have been advances in all portions of perioperative and postoperative care that may also play a role. Future studies examining postoperative rehabilitation as well as causes for failure after UCLR are necessary to better understand these findings.
With regard to common graft choice and surgical technique, palmaris longus autograft was and still is the most common graft choice (71.2% currently and 82% in the prior study), and the ASMI modification of the Jobe technique was the most common surgical technique. While allograft was not used in any patient in the study by Vitale and Ahmad,45 6.0% of patients included in this study underwent UCLR with allograft. Recent evidence has shown allograft—commonly hamstring—to be a viable option for graft choice in UCLR. One series demonstrated 100% RTS after UCLR with allograft, with 88% returning at the same or higher performance level.38 Unfortunately, the majority of studies included in this review did not stratify results by graft, so RTS rates and performance could not be compared between the various graft choices.
In the current study, 69.9% of patients had a concomitant ulnar nerve transposition and 76.9% underwent concomitant arthroscopy. Interestingly, only 18.0% of patients had preoperative ulnar nerve symptoms, indicating that the majority of transpositions occur as part of routine exposure during UCLR. The prior review found that 46% of patients had an ulnar nerve transposition, indicating the current trend is to perform an ulnar nerve transposition with UCLR. Furthermore, 45% of patients in the prior study underwent concomitant elbow arthroscopy compared with 76.9% in the current study. However, further prospective clinical study is required to determine whether routine ulnar nerve transposition results in improved outcomes with regard to return to play.
Finally, the overall RTS rate and complication rate between the 2 studies were very similar. The complication rates between both studies were identical at 10.7%. In both studies, the majority of complications involved the ulnar nerve. Similarly, Vitale and Ahmad45 reported an RTS rate of 83%, while the RTS rate in this study was 86.2%. It should be mentioned that the majority of these studies were from high-volume surgeons/centers; surgical results from lower volume surgeons/centers may not be as good as those reported in this study. Despite advances in surgical techniques and changes in rehabilitation protocols, the RTS rate has not significantly improved. Further studies are necessary to determine the root causes of failure after UCLR to improve the overall RTS rate after UCLR in athletes of all levels of competition.
Limitations
As this study was a review of the literature, it is subject to the limitations of all of the included studies, all of which were level 4 evidence. As the majority of patients included in this study underwent UCLR by a single surgeon, this must be taken into account with regard to the outcomes, graft choice, and surgical technique. Furthermore, other limitations also include heterogeneity between studies, publication bias, the lack of long-term follow-up, and the lack of generalizability to patients in other countries given that only 1 study was published outside the United States. There was also a relative homogeneity among the patients in this study as the majority were male overhead athletes (baseball players, mostly pitchers). Given this homogeneity, the results of this study may not be generalizable to all athletes. The outcome scores reported by the papers included in this study do not take into account how effective players were when they returned to sport (wins, losses, hits, etc), so it is unclear exactly how the players performed on RTS. Finally, although 2 authors performed the literature search, it is possible that some articles were missed. Moving forward, it is our opinion that studies reporting outcomes after UCLR should report all surgical details as well as the KJOC score to allow better assessment of performance on return to play.2 Now that the RTS rates have been well defined, it is necessary to delve deeper into the results to determine whether players performed at the same level after UCLR.
Conclusion
Ulnar collateral ligament reconstruction is performed most commonly in collegiate athletes. Collegiate athletes have the highest RTS rate after UCLR of all levels of competition. The docking and ASMI techniques had higher RTS rates than the Jobe technique.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: N.N.V. receives research support from Arthex, Arthrosurface, DJ Orthopaedics, Smith & Nephew, Athletico, Conmed Linvatec, Miomed, and Mitec; holds stock or stock options in Cymedica, Minivasive, and Omeros; is a paid consultant for Minivasive and Smith & Nephew; and receives royalties from Smith & Nephew and Vindico Medical-Orthopedics Hyperguide. A.A.R. receives royalties from Arthex and SLACK Inc; receives research support from DJO Surgical, Ossur, and Smith & Nephew; and is a paid consultant for Arthrex.
References
- 1. Ahmad CS, Grantham WJ, Greiwe RM. Public perceptions of Tommy John surgery. Phys Sportsmed. 2012;40:64–72. [DOI] [PubMed] [Google Scholar]
- 2. Alberta FG, ElAttrache NS, Bissell S, et al. The development and validation of a functional assessment tool for the upper extremity in the overhead athlete. Am J Sports Med. 2010;38:903–911. [DOI] [PubMed] [Google Scholar]
- 3. Andrews JR, Timmerman LA. Outcome of elbow surgery in professional baseball players. Am J Sports Med. 1995;23:407–413. [DOI] [PubMed] [Google Scholar]
- 4. Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28:16–23. [DOI] [PubMed] [Google Scholar]
- 5. Bowers AL, Dines JS, Dines DM, Altchek DW. Elbow medial ulnar collateral ligament reconstruction: clinical relevance and the docking technique. J Shoulder Elbow Surg. 2010;19(2 suppl):110–117. [DOI] [PubMed] [Google Scholar]
- 6. Cain EL, Jr, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38:2426–2434. [DOI] [PubMed] [Google Scholar]
- 7. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74:67–83. [PubMed] [Google Scholar]
- 8. Cowan J, Lozano-Calderon S, Ring D. Quality of prospective controlled randomized trials. Analysis of trials of treatment for lateral epicondylitis as an example. J Bone Joint Surg Am. 2007;89:1693–1699. [DOI] [PubMed] [Google Scholar]
- 9. Dines JS, ElAttrache NS, Conway JE, Smith W, Ahmad CS. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;35:2039–2044. [DOI] [PubMed] [Google Scholar]
- 10. Dines JS, Frank JB, Akerman M, Yocum LA. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament insufficiency. Am J Sports Med. 2009;37:566–570. [DOI] [PubMed] [Google Scholar]
- 11. Dines JS, Jones KJ, Kahlenberg C, Rosenbaum A, Osbahr DC, Altchek DW. Elbow ulnar collateral ligament reconstruction in javelin throwers at a minimum 2-year follow-up. Am J Sports Med. 2012;40:148–151. [DOI] [PubMed] [Google Scholar]
- 12. Dines JS, Yocum LA, Frank JB, ElAttrache NS, Gambardella RA, Jobe FW. Revision surgery for failed elbow medial collateral ligament reconstruction. Am J Sports Med. 2008;36:1061–1065. [DOI] [PubMed] [Google Scholar]
- 13. Dodson CC, Thomas A, Dines JS, Nho SJ, Williams RJ, 3rd, Altchek DW. Medial ulnar collateral ligament reconstruction of the elbow in throwing athletes. Am J Sports Med. 2006;34:1926–1932. [DOI] [PubMed] [Google Scholar]
- 14. Erickson BJ. The epidemic of Tommy John surgery: the role of the orthopedic surgeon. Am J Orthop (Belle Mead NJ). 2015;44:E36–E37. [PubMed] [Google Scholar]
- 15. Erickson BJ, Gupta AK, Harris JD, et al. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am J Sports Med. 2014;42:536–543. [DOI] [PubMed] [Google Scholar]
- 16. Erickson BJ, Harris JD, Tetreault M, Bush-Joseph C, Cohen MS, Romeo AA. Is Tommy John surgery performed more frequently in Major League Baseball pitchers from warm weather areas? Orthop J Sports Med. 2014;2:2325967114553916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fleisig GS, Andrews JR. Prevention of elbow injuries in youth baseball pitchers. Sports Health. 2012;4:419–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fortenbaugh D, Fleisig GS, Andrews JR. Baseball pitching biomechanics in relation to injury risk and performance. Sports Health. 2009;1:314–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hechtman KS, Zvijac JE, Wells ME, Botto-van Bemden A. Long-term results of ulnar collateral ligament reconstruction in throwing athletes based on a hybrid technique. Am J Sports Med. 2011;39:342–347. [DOI] [PubMed] [Google Scholar]
- 20. Jackson A, Maerz T, Koueiter DM, Andrecovich CJ, Baker KC, Anderson K. Strength of ulnar fixation in ulnar collateral ligament reconstruction: a biomechanical comparison of traditional bone tunnels to the tension-slide technique. J Shoulder Elbow Surg. 2012;21:1674–1679. [DOI] [PubMed] [Google Scholar]
- 21. Jackson TJ, Adamson GJ, Peterson A, Patton J, McGarry MH, Lee TQ. Ulnar collateral ligament reconstruction using bisuspensory fixation: a biomechanical comparison with the docking technique. Am J Sports Med. 2013;41:1158–1164. [DOI] [PubMed] [Google Scholar]
- 22. Jiang JJ, Leland JM. Analysis of pitching velocity in Major League Baseball players before and after ulnar collateral ligament reconstruction. Am J Sports Med. 2014;42:880–885. [DOI] [PubMed] [Google Scholar]
- 23. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68:1158–1163. [PubMed] [Google Scholar]
- 24. Jones KJ, Dines JS, Rebolledo BJ, et al. Operative management of ulnar collateral ligament insufficiency in adolescent athletes. Am J Sports Med. 2014;42:117–121. [DOI] [PubMed] [Google Scholar]
- 25. Koh JL, Schafer MF, Keuter G, Hsu JE. Ulnar collateral ligament reconstruction in elite throwing athletes. Arthroscopy. 2006;22:1187–1191. [DOI] [PubMed] [Google Scholar]
- 26. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–e34. [DOI] [PubMed] [Google Scholar]
- 27. Makhni EC, Lee RW, Morrow ZS, Gualtieri AP, Gorroochurn P, Ahmad CS. Performance, return to competition, and reinjury after Tommy John surgery in Major League Baseball pitchers: a review of 147 cases. Am J Sports Med. 2014;42:1323–1332. [DOI] [PubMed] [Google Scholar]
- 28. Mauro CS, Hammoud S, Altchek DW. Ulnar collateral ligament tear and olecranon stress fracture nonunion in a collegiate pitcher. J Shoulder Elbow Surg. 2011;20:e9–e13. [DOI] [PubMed] [Google Scholar]
- 29. McGraw MA, Kremchek TE, Hooks TR, Papangelou C. Biomechanical evaluation of the docking plus ulnar collateral ligament reconstruction technique compared with the docking technique. Am J Sports Med. 2013;41:313–320. [DOI] [PubMed] [Google Scholar]
- 30. Morgan RJ, Starman JS, Habet NA, et al. A biomechanical evaluation of ulnar collateral ligament reconstruction using a novel technique for ulnar-sided fixation. Am J Sports Med. 2010;38:1448–1455. [DOI] [PubMed] [Google Scholar]
- 31. NCAA. Estimated probability of competing in athletics beyond the high school interscholastic level. September 24, 2013 https://www.ncaa.org/sites/default/files/Probability-of-going-pro-methodology_Update2013.pdf. Accessed May 19, 2015.
- 32. Nissen CW. Effectiveness of interference screw fixation in ulnar collateral ligament reconstruction. Orthopedics. 2008;31:646. [PubMed] [Google Scholar]
- 33. O’Brien DF, O’Hagan T, Stewart R, et al. Outcomes for ulnar collateral ligament reconstruction: a retrospective review using the KJOC assessment score with two-year follow-up in an overhead throwing population. J Shoulder Elbow Surg. 2015;24:934–940. [DOI] [PubMed] [Google Scholar]
- 34. Osbahr DC, Swaminathan SS, Allen AA, Dines JS, Coleman SH, Altchek DW. Combined flexor-pronator mass and ulnar collateral ligament injuries in the elbows of older baseball players. Am J Sports Med. 2010;38:733–739. [DOI] [PubMed] [Google Scholar]
- 35. Paletta GA, Jr, Wright RW. The modified docking procedure for elbow ulnar collateral ligament reconstruction: 2-year follow-up in elite throwers. Am J Sports Med. 2006;34:1594–1598. [DOI] [PubMed] [Google Scholar]
- 36. Park JY, Oh KS, Bahng SC, Chung SW, Choi JH. Does well maintained graft provide consistent return to play after medial ulnar collateral ligament reconstruction of the elbow joint in elite baseball players? Clin Orthop Surg. 2014;6:190–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rohrbough JT, Altchek DW, Hyman J, Williams RJ, 3rd, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002;30:541–548. [DOI] [PubMed] [Google Scholar]
- 38. Savoie FH, 3rd, Morgan C, Yaste J, Hurt J, Field L. Medial ulnar collateral ligament reconstruction using hamstring allograft in overhead throwing athletes. J Bone Joint Surg Am. 2013;95:1062–1066. [DOI] [PubMed] [Google Scholar]
- 39. Savoie FH, 3rd, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36:1066–1072. [DOI] [PubMed] [Google Scholar]
- 40. Smith MV, Calfee RP, Baumgarten KM, Brophy RH, Wright RW. Upper extremity–specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg Am. 2012;94:277–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. The University of Oxford Center for Evidence-Based Medicine Levels of Evidence Oxford Centre for Evidence-Based Medicine. 2012. http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/. Accessed May 27, 2015.
- 42. The University of York Center for Reviews and Dissemination Iprosr-v. http://www.crd.york.ac.uk/PROSPERO/. 2014. Accessed May 27, 2015.
- 43. Thompson WH, Jobe FW, Yocum LA, Pink MM. Ulnar collateral ligament reconstruction in athletes: muscle-splitting approach without transposition of the ulnar nerve. J Shoulder Elbow Surg. 2001;10:152–157. [DOI] [PubMed] [Google Scholar]
- 44. Timmerman LA, Andrews JR. Arthroscopic treatment of posttraumatic elbow pain and stiffness. Am J Sports Med. 1994;22:230–235. [DOI] [PubMed] [Google Scholar]
- 45. Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008;36:1193–1205. [DOI] [PubMed] [Google Scholar]
- 46. Watson JN, McQueen P, Hutchinson MR. A systematic review of ulnar collateral ligament reconstruction techniques. Am J Sports Med. 2014;42:2510–2516. [DOI] [PubMed] [Google Scholar]