Abstract
Background
This study aimed to evaluate the clinical efficacy of use of a 3D printing guide plate in posterior lumbar pedicle screw fixation.
Material/Methods
We enrolled 43 patients receiving posterior lumbar pedicle screw fixation. The experimental group underwent 3D printing guide plate-assisted posterior lumbar pedicle screw fixation, while the control group underwent traditional x-ray-assisted posterior lumbar pedicle screw fixation. After surgery, CT scanning was done to evaluate the accuracy of screw placement according to the Richter standard.
Results
All patients were followed up for 1 month. The mean time of placement for each screw and the amount of hemorrhage was 4.9±2.1 min and 8.0±11.1 mL in the experimental group while 6.5±2.2 min and 59.9±13.0 mL in the control group, respectively, with significant differences (p<0.05). The fluoroscopy times of each screw placement was 0.5±0.4 in the experimental group, which was significantly lower than that in the control group 1.2±0.7 (p<0.05). The excellent and good screw placement rate was 100% in the experimental group and 98.4% in the control group, without any statistical difference (P>0.05). No obvious complications were reported in either group.
Conclusions
Compared with the traditional treatment methods, the intra-operative application of 3D printing guide plate can shorten the operation time and reduce the amount of hemorrhage. It can also reduce the fluoroscopy times compared with the traditional fluoroscopy, which cannot improve the accuracy rate of screw placement.
MeSH Keywords: Bone Screws, Controlled Clinical Trial, Treatment Outcome
Background
The pedicle screw was first introduced in treating unstable thoracolumbar fractures by Roy-Camile in France in 1963. Pedicle screw internal fixation has been widely applied in treating conditions such as protrusion of lumbar intervertebral disc, lumbar spinal stenosis, and lumbar spondylolisthesis, which greatly promotes development of spinal surgeries [1]. Although most spinal surgeons can master the pedicle screw placement technique, there still remains a challenge for spinal surgeons to place pedicle screws precisely and reduce complications, because of a diversity of pedicle anatomy structures and potential complications (e.g., injuries of nerve root, vessel, or viscera) caused by inappropriate screw placement positions [2].
Three-dimensional (3D) printing, also termed rapid proto-typing technology, has gradually penetrated into the field of clinical medicine [3]. In cervicothoracic vertebral operations using a spinal surgical guide plate produced by 3D printing, the diameter and length of placed screws can be estimated pre-operatively, and the pedicle screws can be placed under the assistance of 3D printing guide plates. The personalized design can shorten operation time, promote accuracy of screw placement, and reduce complications [4–6]. In this study, 3D printing guide plate technique was applied in posterior lumbar pedicle screw fixation, and amount of hemorrhage, mean placement time for each screw, mean fluoroscopy times, and accuracy of placement between the experimental and control groups were compared with the traditional intraoperative x-ray positioning-assisted screw placement through anatomic landmarks.
Material and Methods
General information
Patients receiving posterior lumbar pedicle screw fixation in our department from Aug 2014 to Mar 2015 were enrolled in this study. Types of diseases included protrusion of lumbar intervertebral disc, lumbar spinal stenosis, and lumbar spondylolisthesis. Patients in the experimental group received posterior lumbar pedicle screw fixation assisted by 3D printing guide plate, while patients in the control group underwent traditional x-ray-assisted fixation.
Among the 20 patients (9 males and 11 females, mean age 52.3 years [range, 35–70 years]) in the experimental group, 10 had protrusion of lumbar intervertebral disc, 7 had lumbar spinal stenosis, and 3 had lumbar spondylolisthesis. Of the 23 patients (12 males and 11 females, mean age 55.4 years [range, 37–72 years]) in the control group, 12 had protrusion of lumbar intervertebral disc, 8 had lumbar spinal stenosis, and 3 had lumbar spondylolisthesis. Results of independent t test used for comparing age, sex, affected segments, and number of placed screws, showed that there was no significant difference between the 2 groups, which were comparable.
Inclusion criteria
The inclusion criteria were: (1) Patients who did not responded to the conservative therapy for half a year and had surgery indications; (2) Those who only used operation methods of posterior lumbar decompression or 3D printing guide plate-assisted pedicle screw placement and intervertebral bone graft fusion; (3) Those who were fully informed of treatment protocol and who signed the informed consent form. This trial was approved by the ethics committee of our hospital.
Random methods
All patients were randomly assigned into the experimental group and the control group based on the patient number on admission by using a random number generated by computer.
Allocation concealment
The patients had no idea which group they were in. A specially-assigned person was in charge of the enrollment and grouping of the patients to avoid selective bias and ensure allocation concealment.
Pre-operative preparation
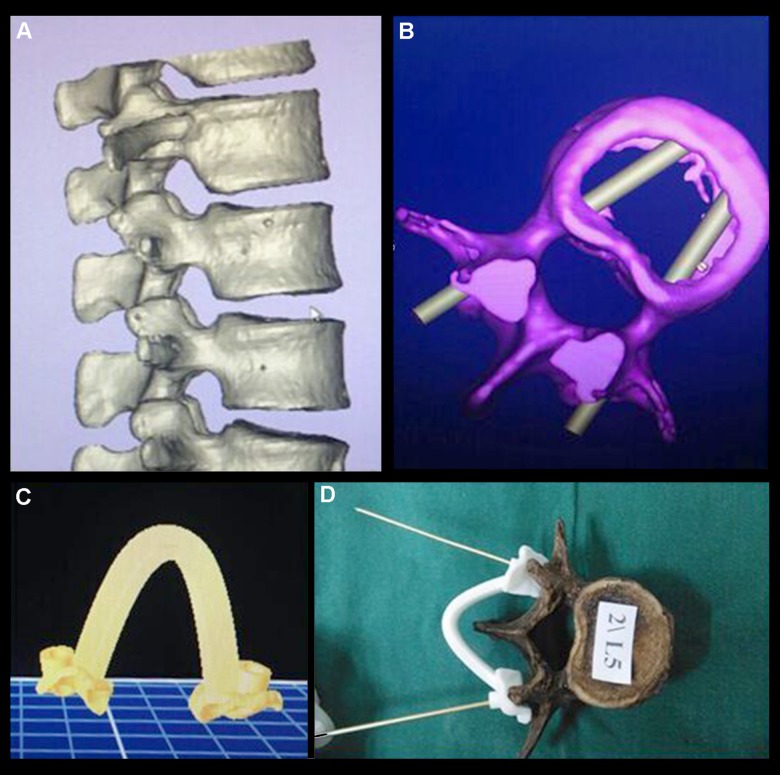
All patients received imaging tests, such as lumbar posterior-anterior/lateral radiographs, flexion-extension radiographs, lumbar MRI, and lumbar CT for protopathic certification (Figure 1). The experimental group received lumbar CT 3D reconstruction with a layer of 1 mm. The P100 3D printer from German EOS was used and the printing material was polyamide PA220 (Figure 2).
Figure 1.
(A–C) Pre-operative lumbar MRI images.
Figure 2.
A) The pre-operative 3D CT reconstruction images; (B) A virtual screw path was established on the operational vertebral body model using the MedCAD, making the path parallel to the long axis of the pedicle; (C) 3D pedicle screw guide plates corresponding to the surgical vertebral were reconstructed according to the image data. (D) The pedicle screw path was established with the assistance of the corresponding pedicle screw guide plate, which was performed for the opposite side by the same method.
Operational methods
The operations in both groups were completed by the same surgeon. The skin and fascia lumbodorsalis were cut regularly, and paravertebral muscles were peeled to fully expose posterior column bony structures, such as spinous processes, vertebral plates, and articular processes of the affected vertebral columns. Following that, the soft tissues attached to the bony structures were cleared. After full exposure, the 3D printing guide plate was tightly attached to the operational segmental lumbar vertebral plate, and Kirschner wire was inserted into the pinhole on the guide plate to obtain a placement angle. The inserting point was determined through the 3D printing guide plate and marked by electrotome, and the vertebral incision was opened. First, the guide plate was slightly moved to one side, complete preparation of the screw path was done referring to the contralateral direction of the Kirschner wire, and then the pedicle screw was placed. The pedicle screw on the other side was inserted in the same way. The angle, position, and length of the placed screw were confirmed through intraoperative C-arm fluoroscopy. If the pedicle screw was malpositioned, the screw path and angle were adjusted for repeat screw placement. The nerve root decompression and infusion was preformed routinely. Control group patients received traditional x-ray-assisted posterior lumbar pedicle screw fixation.
Evaluation of efficacy
The intraoperative amount of hemorrhage, mean placement time for each screw, mean fluoroscopy times, and accuracy of placement in both groups were recorded. The in-operation hemorrhage was calculated by total fluid volume in the suction apparatus minus the fluid volume used for washing. The total time was from completion of 3D printing guide plate placement after operational area was completely visible (experimental group) and structures posterior to vertebral body was completely visible (control group), respectively, to the last pedicle screw satisfactorily placed in proper position. The total time was divided by the number of placed screws to obtain the mean placement time for each screw. The accuracy of placement was evaluated by Richter method [7] and divided into 3 categories: (1) Excellent: the screws were completely positioned in the pedicle; (2) Good: only screw thread went through the cortex of the pedicle isthmus of vertebral arch (less than 1/4 of the screw diameter), without danger to surrounding nerves and vessels; (3) Poor: the screws penetrated the cortex of pedicle isthmus of vertebral arch obviously (more than 1/4 of the screw diameter), which damaged surrounding nerves and vessels.
Statistical analysis
Statistical analysis was performed with SPSS 19.0 Statistical software. Data are presented as mean ±SD (x±s), and inter-group comparison was done with the independent-samples t test. The enumeration data is expressed as ratio, and inter-group comparison was done with the χ2 test; α=0.05 was used as the statistics inspection standard.
Results
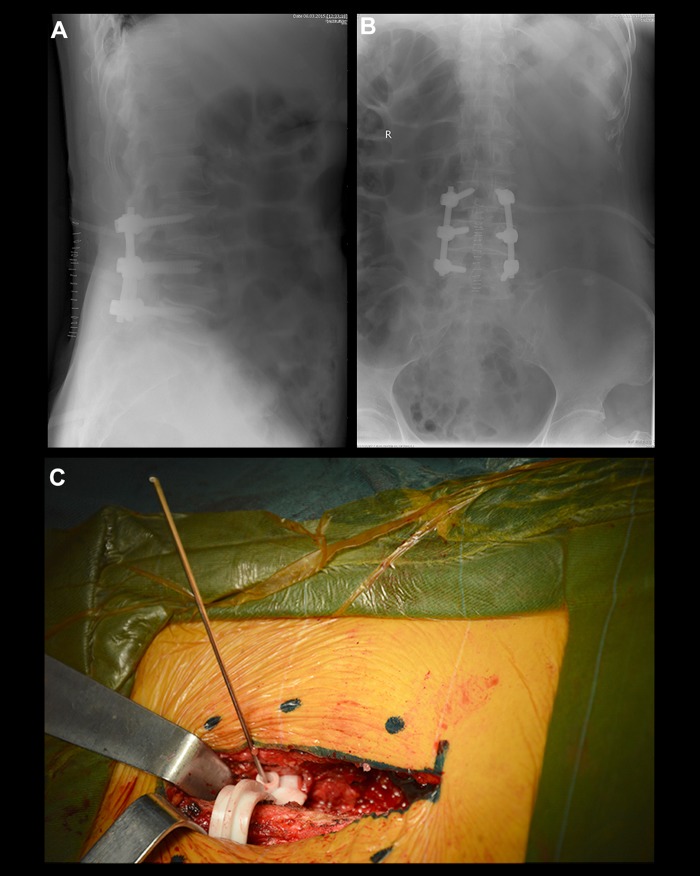
All the patients were followed up for 1 month. No obvious complications of nerves, vessels, or viscera were reported in either group. A total of 118 pedicle screws were placed in the experimental group and 122 in the control group. The placement effect was evaluated by post-operative anteroposterior and lateral x-ray film and lumbar CT scan (Figure 3).
Figure 3.
A) The post-operative lateral x-ray films; (B) The post-operative anterior-posterior x-ray films. Both revealed a good position of pedicle screw. (C) The pedicle screw path was established under the assistance of individualized 3D pedicle screw guide plate during the operation.
The mean time of placement for each screw was 4.9±2.1 min in the experimental group and 6.5±2.2 min in the control group, which were significantly different from each other (P<0.05). The amount of hemorrhage was 8.0±11.1 mL and 59.9±13.0 mL in the experimental and control groups, respectively, with significant difference (P<0.05). The fluoroscopy times for each screw placement was 0.5±0.4 in the experimental group, which was significantly lower than that in the control group (1.2±0.7) (p<0.05).
A total of 118 pedicle screws were placed into experimental group patients; the accuracy of placement was excellent in 108 (91.5%) and good in 10 (8.5%), with an excellent and good rate of 100%. In the control group 122 pedicle screws were placed; the accuracy of placement was excellent in 99 (81.1%), good in 21 (17.2%), and poor in 2 (1.6%), with an excellent and good rate of 98.4%. There was no significant difference in the excellent and good rate of screw placement between the 2 groups (p>0.05).
Discussion
With rapid progress in digital technology, 3D printing technique has been increasingly applied in treatment of spine diseases. The 3D printing technique is based on 3D design models and uses computer software and CNC forming system to pile up and bond the special materials, such as metal powder, ceramic powder, and cellular tissue, layer by layer, and thus produce a physical product. In spinal surgery, this technique is based on the reverse engineering principle. That is, based on the CT scan image, to rebuild the targeted vertebral bodies with the software and design the corresponding female mold of the bony structures, such as vertebral plates and spinous processes, with the computer. After the female mold of vertebral bodies is printed, the surgeons can perform the placement operation under direct observation. Some researchers have used the 3D printing technique in internal screw fixation of axis vertebral plates, and the individualized guide plate for screw placement was established based on the CT scan images to improve the accuracy of placement [8]. Yang et al. reported the use of 3D printing technique in patients with Lenke I adolescent idiopathic scoliosis to make vertebral body molds during the operation. The 3D printing group, compared with the control group, had shorter operation time and less hemorrhage, but did not significantly increase the accuracy of placement [9]. This study used 3D printing technique to produce the lumbar vertebral female mold and evaluated the clinical efficacy of a 3D printing guide plate in posterior lumbar pedicle screw fixation.
Steinmann et al. started to use the computer-assisted surgical navigation system in spinal surgery in the 1990s [10], which increased the accuracy of pedicle screw placement. Nevertheless, according to some reports, the adoption of computer-assisted navigation equipment was difficult in primary hospitals [10,11] due to very high price, a complex operation system, and high operating costs. The 3D printing technique, with simple and rapid operations, lower costs, and has other advantages, emerged at an opportune time. In the present study, the 3D printing guide plate could be produced in 1 day after obtaining the CT scan data of a patient. Moreover, the intraoperative procedure for 3D guide plate use is very simple. Because of long learning curve of lumbar pedicle screw fixation and high risk of the operation, some researches have reported use of computer-assisted fixation [12–14]. Miyomoto et al. adopted CT technique, but could only confirm the entry point, not the angle [15]. Kawaguchi et al. acquired patient data through CT scans, and used rapid prototyping technology to print out a guide plate-assisted screw-matching centrum [16]. However, the guide plate only attached to 1 side of the lumbar pedicle, which shifts easily, especially when a bone landmark was missing due to vertebral abnormality, thus the guide plate was hard to accurately place. But the 3D printing guide plate used in this study attached the both sides of the lumbar pedicle. The bone landmark was easy to find, and the contact area is sufficiently large. Thus, the screw does not easily shift. The screws could be placed bilaterally at the same time. Results of this study have shown that the mean time of placement for each screw and the amount of hemorrhage was 4.9±2.1 min and 8.0±11.1 mL in the experimental group (using 3D printing guide plate) versus 6.5±2.2 min and 59.9±13.0 mL in the control group (using the traditional fluoroscopy), There were statistically significant differences between the 2 groups (p<0.05). The fluoroscopy times for each screw placement was 0.5±0.4 in the experimental group, which was significantly lower than that of control group 1.2±0.7, with a significant difference (p<0.05). These results indicate that the intraoperative application of 3D printing guide plates was easy, and could shorten operation time and reduce amount of hemorrhage. It can reduce the fluoroscopy times compared with the traditional treatment group, and may indirectly increase the success rate of first-time placement and decrease x-ray exposure in patients. Successful first-time placement leads to more a successful operation because the second-time puncture can damage the bony structures, and the pseudo-channel left by the first puncture will interfere with the second puncture, which makes the second operation difficult and decreases the screw-holding force.
In lumbar internal fixation of the spinal surgery field, since the surgeon is utterly dependent on the location of vertebral plate anatomical marks, the accuracy of screw placement is greatly affected by subjective factors such as the experience of surgeons. The 3D printing technique transforms the operation from being experience-based to a digital, precise, and individualized approach that shortens the learning curve of spinal surgery and surgical risks. There are 2 major points in application of 3D printing guide-assisted lumbar internal fixation: a. The production of guide plates, which serves as a guidance of the placement, must be based on the bone data obtained from high-speed and thin-layer CT to the greatest extent in order to produce a female mold of vertebral bodies as precisely as possible and match the vertebral body perfectly. b. When vertebral plates are being exposed, the peeled surface of soft tissue is required to have complete clearance without damaging bony structures. Otherwise, the screw path is easily deviated, causing the screw to penetrate the cortex of vertebral plates. In this study, a total of 118 and 112 pedicle screws are placed in the experimental group and the control group, with the excellent and good rate of 100% and 98.4%, respectively. No statistically significant difference was found in the excellent and good rate of screw placement between the 2 groups (p>0.05). The reasons for this might be that, for those patients without anatomical abnormality needing routine lumbar surgeries, the accuracy rate of placement can be satisfied depending on the surgeon’s experience, and cannot be increased significantly by using the 3D printing guide plates.
Our study has the following deficiencies: a. The number of enrolled patients is relatively small due to increased expense for 3D printing guide plates. b. The subjects enrolled in this study are those without obvious anatomical abnormality needing routine lumbar surgeries, which might not reflect the advantages of 3D printing guide plates in improving the accuracy of placement.
Conclusions
So far, the 3D printing guide plate has not been widely applied in spinal surgery, and there are few related reports. According to this study, compared with the traditional treatments, the intraoperative application of a 3D printing guide plate could shorten the operation time and reduce the amount of hemorrhage. Compared to traditional fluoroscopy, it can reduce the fluoroscopy times, but does not increase the accuracy rate of screw placement.
Footnotes
Source of support: Departmental sources
References
- 1.Siewe J, Bredow J, Oppermann J, et al. Evaluation of efficacy of a new hybrid fusion device: a randomized, two-centre controlled trial. BMC Musculoskelet Disord. 2014;15:294. doi: 10.1186/1471-2474-15-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laine T, Lund T, Ylikoski M, et al. Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J. 2000;9:235–40. doi: 10.1007/s005860000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guarino J, Tennyson S, McCain G, et al. Rapid prototyping technology for surgeries of the pediatric spine and pelvis: benefits analysis. J Pediatr Orthop. 2007;27:955–60. doi: 10.1097/bpo.0b013e3181594ced. [DOI] [PubMed] [Google Scholar]
- 4.Hu Y, Yuan ZS, Spiker WR, et al. Deviation analysis of C2 translaminar screw placement assisted by a novel rapid prototyping drill template: a cadaveric study. Eur Spine J. 2013;22:2770–76. doi: 10.1007/s00586-013-2993-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lu S, Xu YQ, Lu WW, et al. A novel patient-specific navigational template for cervical pedicle screw placement. Spine (Phila Pa 1976) 2009;34:E959–66. doi: 10.1097/BRS.0b013e3181c09985. [DOI] [PubMed] [Google Scholar]
- 6.Lu S, Zhang YZ, Wang Z, et al. Accuracy and efficacy of thoracic pedicle screws in scoliosis with patient-specific drill template. Med Biol Eng Comput. 2012;50:751–58. doi: 10.1007/s11517-012-0900-1. [DOI] [PubMed] [Google Scholar]
- 7.Richter M, Mattes T, Cakir B. Computer-assisted posterior instrumentation of the cervical and cervico-thoracic spine. Eur Spine J. 2004;13:50–59. doi: 10.1007/s00586-003-0604-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lu S, Xu YQ, Zhang YZ, et al. A novel computer-assisted drill guide template for placement of C2 laminar screws. Eur Spine J. 2009;18:1379–85. doi: 10.1007/s00586-009-1051-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang M, Li C, Li Y, et al. Application of 3D rapid prototyping technology in posterior corrective surgery for Lenke 1 adolescent idiopathic scoliosis patients. Medicine (Baltimore) 2015;94:e582. doi: 10.1097/MD.0000000000000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nottmeier EW, Foy AB. Placement of C2 laminar screws using three-dimensional fluoroscopy-based image guidance. Eur Spine J. 2008;17:610–15. doi: 10.1007/s00586-007-0557-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rajasekaran S, Avadhani A, Shetty AP. Axial translaminar screw placement using three-dimensional fluoroscopy-based navigation. Singapore Med J. 2011;52:15–18. [PubMed] [Google Scholar]
- 12.Lang Z, Tian W, Liu Y, et al. Minimally invasive pedicle screw fixation using intraoperative three-dimensional fluoroscopy-based navigation (CAMISS Technique) for Hangman’s fracture. Spine (Phila Pa 1976) 2015 doi: 10.1097/BRS.0000000000001111. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.Ruatti S, Dubois C, Chipon E, et al. Interest of intra-operative 3D imaging in spine surgery: a prospective randomized study. Eur Spine J. 2015 doi: 10.1007/s00586-015-4141-5. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Kraus M, Weiskopf J, Dreyhaupt J, et al. Computer-aided surgery does not increase the accuracy of dorsal pedicle screw placement in the thoracic and lumbar spine: a retrospective analysis of 2,003 pedicle screws in a level I trauma center. Global Spine J. 2015;5:93–101. doi: 10.1055/s-0034-1396430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miyamoto H, Uno K. Cervical pedicle screw insertion using a computed tomography cutout technique. J Neurosurg Spine. 2009;11:681–87. doi: 10.3171/2009.6.SPINE09352. [DOI] [PubMed] [Google Scholar]
- 16.Kawaguchi Y, Nakano M, Yasuda T, et al. Development of a new technique for pedicle screw and Magerl screw insertion using a 3-dimensional image guide. Spine (Phila Pa 1976) 2012;37:1983–88. doi: 10.1097/BRS.0b013e31825ab547. [DOI] [PubMed] [Google Scholar]