Abstract
Background
Regionalized trauma care improves outcomes; however access to care is not uniform across the US. The objective was to evaluate whether geographic distribution of trauma centers correlates with injury mortality across state trauma systems.
Methods
Level I/II trauma centers in the contiguous US were mapped. State-level age-adjusted injury fatality rates/100,000people were obtained and evaluated for spatial autocorrelation. Nearest neighbor ratios (NNR) were generated for each state. A NNR<1 indicates clustering, while NNR>1 indicates dispersion. NNR were tested for difference from random geographic distribution. Fatality rates and NNR were examined for correlation. Fatality rates were compared between states with trauma center clustering versus dispersion. Trauma center distribution and population density were evaluated. Spatial-lag regression determined the association between fatality rate and NNR, controlling for state-level demographics, population density, injury severity, trauma system resources, and socioeconomic factors.
Results
Fatality rates were spatially autocorrelated (Moran's I=0.35, p<0.01). Nine states had a clustered pattern (median NNR 0.55, IQR 0.48–0.60), 22 had a dispersed pattern (median NNR 2.00, IQR 1.68–3.99), and 10 had a random pattern (median NNR 0.90, IQR 0.85–1.00) of trauma center distribution. Fatality rate and NNR were correlated (ρ=0.34, p=0.03). Clustered states had a lower median injury fatality rate compared to dispersed states (56.9 [IQR 46.5–58.9] versus 64.9 [IQR 52.5–77.1], p=0.04). Dispersed compared to clustered states had more counties without a trauma center that had higher population density than counties with a trauma center (5.7% versus 1.2%, p<0.01). Spatial-lag regression demonstrated fatality rates increased 0.02/100,000persons for each unit increase in NNR (p<0.01).
Conclusions
Geographic distribution of trauma centers correlates with injury mortality, with more clustered state trauma centers associated with lower fatality rates. This may be a result of access relative to population density. These results may have implications for trauma system planning and requires further study to investigate underlying mechanisms
Keywords: Geospatial, Spatial, Trauma systems, Fatality rate, Nearest neighbor
BACKGROUND
Injury is the leading cause of death age 46 and younger in the United States (US), making trauma a leading public health problem.1 Regionalization of trauma systems has led to improvements in trauma care and outcomes.2–4 Despite this, access to trauma care is not uniform across the US and there is geographic variation in outcomes among trauma systems.5–10 Oversight and organization of trauma systems has fallen to individual states, further contributing to variation in structure and access to the trauma system.11
Several authors have shown that geographic factors impact outcomes following injury. Our group demonstrated significant variation in outcome after helicopter transport based on US census region, while others reported mortality from motor vehicle collisions (MVC) is influenced by geographic region, population density, and vehicle miles traveled.9, 12–15 Some have also demonstrated that geospatial analysis can aid trauma system design and enhance resource allocation.16, 17 Jensen and colleagues have used sophisticated geospatial evaluation to help plan optimal trauma system resource placement in Scotland and provide detailed injury surveillance.18, 19
Although data has shown that geographic factors can influence patient-level outcomes after trauma, it remains unclear what influence geospatial factors may have on outcome from a system perspective of existing resources. Thus, it was our objective to evaluate whether the geographic distribution of trauma centers correlates with injury mortality across state trauma systems in the US. We hypothesized that a more evenly dispersed pattern of trauma centers would be associated with lower mortality.
METHODS
Data Sources
State characteristics including population density, land area classified as an urban, educational attainment, unemployment rate, poverty rate, and median income in 2010 were obtained from the US census bureau. Additionally, county-level population density was obtained to evaluate population density within states. Age-adjusted injury fatality rates from 2008–2010, expressed as the number of injury fatalities per 100,000 persons, were obtained from the Centers for Disease Control (CDC) Web-based Injury Statistics Query and Reporting System for each state.20 The location of trauma centers were obtained from the University of Pennsylvania Cartographic Modeling Laboratory 2010 Trauma center maps and the American Trauma Society Trauma Information Exchange Program.17 The 2010 Atlas and Database of Air Medical Services was used to determine the number of medical helicopter bases within each state.21
The 2010 National Inpatient Sample was used to generate state-level mean injury severity scores (ISS). All patients with an external cause of injury code were included. International Classification of Diseases, ninth revision (ICD-9) diagnosis codes were translated into ISS using ICDPIC software.22 The ISS for each patient was averaged at the state-level by hospital location, generating a mean ISS for 44 states.
Geospatial Analysis
The location of level I and II trauma centers were mapped within the contiguous 48 states. Injury fatality rates were tested for spatial autocorrelation using Moran's I. Spatial autocorrelation is the degree to which similar data values are grouped together geographically. Moran's I is a measure of spatial autocorrelation, ranging from −1 (completely dispersed in space) to +1 (perfectly correlated in space), and can be interpreted similarly to a correlation coefficient. This represents a measure of how dissimilar or similar a state's injury fatality rate is when compared to neighboring states. In other words, it evaluates whether states with similar injury fatality rates are grouped closer together or spread farther apart from each other.
A nearest neighbor analysis evaluated the geographic distribution of trauma centers within each state. This produced a nearest neighbor ratio (NNR) for each state, which is a measure of how clustered or dispersed trauma centers are within the state. The NNR is calculated as the observed mean distance between each trauma center and its nearest neighboring center divided by the expected mean distance between each center and its nearest neighbor assuming the centers are distributed in a random geographic pattern. The expected mean distance takes into account the total number of centers and the land area containing all centers in the state. A NNR<1 indicates trauma center clustering within the state, because the actual distance between centers is less than what would be expected if distributed randomly and therefore centers are closer together. A NNR>1 indicates trauma center dispersion within the state, because the actual distance between centers is greater than what would be expected if distributed randomly and therefore centers are farther apart. Each state NNR was tested for significant difference from a random geographic pattern of trauma center distribution. A p value<0.05 for the NNR indicated a state was significantly clustered if the NNR was <1 or significantly dispersed if the NNR was >1. A non-significant p value>0.05 indicated a state had a random geographic pattern of trauma center distribution.
County-level population density data was used to create a continuous surface of population density throughout the US. Trauma centers were mapped to the continuous population density map to examine the location of trauma centers relative to within state population density.
Statistical Analysis
The primary outcome was age-adjusted injury fatality rate. Spearman correlation was used to evaluate the relationship between state injury fatality rates and NNR. Median fatality rates were compared between states with significant trauma center clustering and states with significant trauma center dispersion. To evaluate the interaction with population density, Spearman correlation was also used to evaluate state population density and injury fatality rates. Median population density was compared between states with trauma center clustering and dispersion. The number of trauma centers per 1million persons in each state was correlated with fatality rates, as well as compared between clustered and dispersed states.
At the county-level, median population density was compared between counties with and without one or more level I/II trauma centers, as well as between clustered and dispersed states. Additionally, the proportion of counties without a trauma center that have a population density higher than the median population density of counties with a trauma center was compared between clustered and dispersed states as a measure of how well trauma centers are matched to the population distribution within states.
To evaluate the potential effect of lower level trauma center availability on injury fatality rates, the proportion of each state's population living in counties with a state-designated level III-V trauma center but no level I-II center was correlated with fatality rates, as well as compared between clustered and dispersed states.
Ordinary least squares (OLS) regression was used to determine the association between injury fatality rate and NNR, controlling for state-level factors including population density, proportion of state classified as urban, mean ISS, medical helicopter bases per 1million persons, trauma centers per 1million persons, median household income, poverty rate, educational attainment, proportion of state population served by level III–V trauma centers, and ratio of level I:II trauma centers. The same model was performed using spatial-lag regression, and compared to the OLS results using R2, Akaike information criteria (AIC), and the likelihood ratio test (LRT). The spatial-lag model accounts for that fact that an outcome value at any given geographic location is affected by the outcome value at neighboring geographic locations.23 If the outcome is spatially autocorrelated, a spatial-lag model will better explain variability in outcome values, evidenced by a higher R2 value, lower AIC, and significant LRT.
Geospatial analysis was performed using ArcGIS v10.2 (ESRI; Redlands, CA) and GeoDa v1.6 (Arizona State University; Tempe, AZ). Data analysis was conducted using Stata v13 (StataCorp; College Station, TX). Continuous data are presented as median (interquartile range [IQR]). Continuous data were compared using Mann-Whitney U tests, and categorical data compared using Chi-square. A two-tailed p value ≤0.05 was considered significant.
Subgroup Analysis
The analyses above were performed separately in four subgroups of injury fatality rates available from the CDC. These included deaths from firearm related injuries, violence related injuries by any mechanism, MVC, and traumatic brain injury (TBI).
RESULTS
State injury fatality rates were spatially autocorrelated within the US, with a Moran's I=0.35 (p<0.01), indicating state injury fatality rates are more similar to geographically closer states than those farther away. When evaluating the NNR by state, 9 states had a significantly clustered pattern (median NNR 0.55 [IQR 0.48, 0.60]), 22 had a significantly dispersed pattern (median NNR 2.00 [IQR 1.68, 3.99]), and 10 had a random pattern (median NNR 0.90 [IQR 0.85, 1.00]) of trauma center geographic distribution. Seven states had ≤1 centers, and a NNR could not be calculated. Figure 1 illustrates state injury fatality rates and trauma center distribution pattern.
Figure 1.
State injury fatality rate and geographic distribution of trauma centers in the United States. Injury fatality rate is represented by color ramp, with higher values represented in red and lower values represented in blue. Trauma center geographic distribution based on significance of the NNR is represented by patterned overlay. Level I or II trauma center geographic locations are represented by black stars.
Injury fatality rates and NNR had a significant positive correlation (Spearman ρ=0.34, p=0.03), indicating as the NNR increases and represents more dispersion of trauma centers, injury fatality rates also increase. States with a clustered pattern of trauma centers had a significantly lower median injury fatality rate than states with a dispersed pattern (Table 1, p=0.04).
Table 1.
Median injury fatality rates by trauma center geographic distribution pattern
| Injury type/intent* | Clustered n=9 |
Dispersed n=22 |
p value |
|---|---|---|---|
| All injuries | 56.9 (46.5, 58.9) | 64.9 (52.5, 77.1) | 0.04 |
| Firearm | 8.9 (6.8, 11.0) | 12.3 (8.0, 14.9) | 0.13 |
| Violence | 16.7 (14.2, 17.7) | 19.1 (15.4, 23.4) | 0.12 |
| MVC | 8.3 (7.9, 12.8) | 12.4 (9.8, 18.3) | 0.03 |
| TBI | 15.7 (11.3, 18.5) | 19.4 (17.3, 21.3) | 0.03 |
fatality rate/100,000 persons, expressed as median (IQR)
IQR, interquartile range; MVC, motor vehicle collision; TBI, traumatic brain injury
Injury fatality rates and population density were inversely correlated (ρ= −0.60, p<0.01), indicating as population density increased injury fatality rates decreased. States with a dispersed pattern of trauma centers also had a significantly lower median population density than states with a clustered pattern (84.1 [IQR 40.0, 153.9] vs. 231.1 [IQR 101.2, 282.3] persons/square mile, p=0.02). The number of trauma centers per 1million persons was inversely but not significantly correlated with injury fatality rates (ρ= −0.10, p=0.51). The median number of level I-II centers per 1million persons was not significantly different between clustered and dispersed states (0.64 [IQR 0.36, 1.01] vs. 0.41 [IQR 0.36, 0.77], p=0.51; Supplemental Digital Content 1).
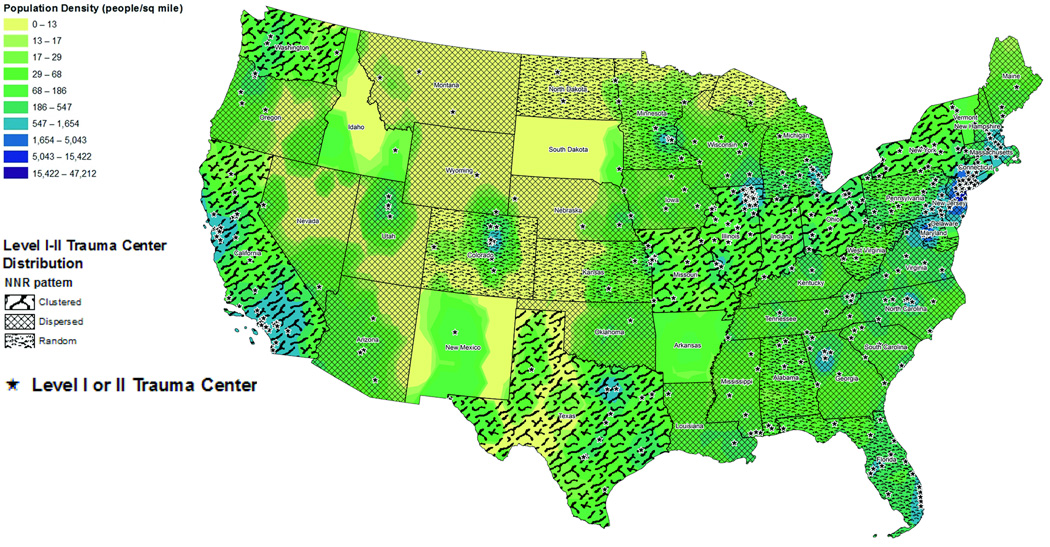
Trauma centers were largely located in areas of each state with higher population density (Fig. 2). The median population density was higher for counties with one or more trauma centers located within it compared to counties without a trauma center (475.2 [IQR 211.9, 1133.9] vs. 37.5 [IQR 14.7, 84.0] persons/square mile, p<0.01). The median population density in counties with a trauma centers present was higher but not significantly different in clustered states when compared to dispersed states (569.5 [IQR 233.6, 1335.1] vs. 405.7 [IQR 184.4, 1116.3] persons/square mile, p=0.21). However, dispersed states compared to clustered states had a significantly greater proportion of counties without a trauma center that had a higher population density than the median population density of counties with a trauma center (5.7% vs. 1.2%, p<0.01). This indicates clustered states nearly exclusively have trauma centers located in areas of highest population density, while dispersed states more often have centers in areas of lower population density relative to potential areas without a trauma center.
Figure 2.
Continuous population density across the United States using county population density. Population density is represented by color ramp, with higher values represented in blue and lower values represented in yellow. Trauma center geographic distribution based on significance of the NNR is represented by patterned overlay. Level I or II trauma center geographic locations are represented by black stars.
The proportion of state population living in counties served only by level III-V centers did not correlate with state injury fatality rates (ρ=0.26, p=0.10). Dispersed states had a higher median population proportion in counties served only by level III–V centers; however this was not significantly different from clustered states (12% [IQR 1%, 40%] vs. 6% [IQR 0%, 8%], p=0.29; Supplemental Digital Content 2).
In OLS regression, NNR was associated with injury fatality rate (p<0.01). Spatial-lag regression outperformed OLS regression with higher R2 (0.86 vs. 0.73), lower AIC (273.0 vs. 282.8), and a significant LRT (p<0.01). In spatial-lag regression, each one unit increase NNR was independently associated with a 0.016 increase in injury fatality rate per 100,000 persons (p<0.01) after adjusting for state-level confounders.
Fatality rates remained spatially autocorrelated across all subgroups (Table 2, p<0.01 for all subgroups), indicating clustering of similar fatality rate values geographically. Injury fatality rates and NNR had a significant positive correlation for MVC and TBI fatality rates, but not for firearm or violent fatality rates (Table 2). MVC and TBI median fatality rates were also significantly lower among clustered states compared to dispersed states, but there was no significant difference for firearm and violent fatality rates (Table 1). In regression analysis, spatial-lag models again outperformed OLS regression (LRT p<0.01 for all subgroups). After adjusting for state-level factors, increasing NNR remained significantly associated with higher fatality rates in each subgroups; however the size of these effects were an order of magnitude smaller (Table 2).
Table 2.
Subgroup analysis results
| Injury type/intent |
Moran's I | Spearman ρ (95%CI) |
Spearman ρ p value |
NNR spatial-lag regression coefficient |
Regression coefficient p value |
|---|---|---|---|---|---|
| Firearm | 0.46 | 0.29 (−0.03, 0.55) | 0.07 | 0.004 | <0.01 |
| Violence | 0.38 | 0.30 (−0.02, 0.56) | 0.06 | 0.004 | <0.01 |
| MVC | 0.50 | 0.36 (0.05, 0.61) | 0.02 | 0.005 | <0.01 |
| TBI | 0.46 | 0.39 (0.09, 0.63) | 0.01 | 0.005 | <0.01 |
95%CI, 95% confidence interval; MVC, motor vehicle collision; TBI, traumatic brain injury
DISCUSSION
This data demonstrate US injury fatality rates are spatially autocorrelated, indicating state fatality rates are more similar to geographically neighboring states than more distant states. Most states in the US have a dispersed pattern of trauma center distribution. Despite this, states with a clustered pattern of trauma center distribution had a lower injury fatality rate on average.
Spatial-lag regression was superior to OLS, which is not surprising given fatality rates are spatially autocorrelated. Thus, spatial models should be considered when spatial dependencies are present in the data being modeled. The spatial-lag model demonstrated increasing NNR values, which represent increasing dispersion of trauma centers, were independently associated with increasing injury fatality rates. This further suggests that geographic clustering of trauma centers at the state-level is associated with improved outcomes.
Subgroup analysis demonstrated the association between trauma center clustering and improved outcome remained for MVC and TBI mortality, while this relationship was no longer seen for firearm and violent injury fatality rates. Regression again demonstrated increasing NNR was associated with increasing injury fatality rates with a much smaller effect size, likely given the smaller fatality rates in each subgroup.
These findings are contrary to our original hypothesis. We originally hypothesized a dispersed pattern of trauma centers would be associated with better outcome, reasoning trauma centers more evenly distributed geographically would provide wider coverage of trauma care within the state, and thus reduce injury fatality rates. However, the current results are likely due to differences in geographic trauma center distribution based on land area as represented by the NNR, and population distribution throughout states. Populations are not uniformly distributed across land area. Thus, the association between trauma center clustering and lower fatality rates may represent improved access to trauma care through better matching of system resources with the main population centers within these states. This is highlighted in Figure 2, as trauma centers are generally located in areas of higher population density within states. However, dispersed states have more centers located in lower population density areas than clustered states, and thus may represent differential population access to trauma care. Access to care has been widely implicated in outcomes after injury, with variations based on geography.5–7
Further, these results are likely due to the scale of geography studied. Although trauma systems are legislated at the state-level, they may not operate as a single trauma system.4 When evaluated from the perspective of state-wide mortality, it may be that clustering of trauma centers best serves the population centers, while if evaluated on a smaller regional level, mortality may be lower in areas that have a more uniform distribution of trauma centers over a catchment area. Further study of the relationship between geographic distribution of trauma centers and outcome is warranted to elucidate the underlying mechanisms of these findings, and expand our understanding of the geographic distribution of resources at varying levels within trauma systems.
MVC and TBI fatality rates exhibited improved mortality for clustered trauma centers, while this was not seen for firearm and violent injury rates. This may be due to the fact that firearm and violent injury, as predominantly penetrating mechanisms, concentrate in urban areas with at least one trauma center. Thus, these patients would have rapid access to a trauma center and the overall state-level distribution of trauma centers would play less of a role in outcome. Conversely, MVC and TBI are predominantly blunt mechanisms that are not restricted in urban centers but will occur more frequently in higher population density areas. Thus, outcome in these injuries may depend more on trauma system access, and clustering of trauma centers at the state-level may provide better matching of resources to population centers.
This study is the first to evaluate geographic distribution pattern of trauma centers and injury fatality rates. Thus, there is little existing literature to compare these results to; however the influence of geospatial factors on outcome after trauma is well documented. Minei et al reported significant variations in outcome among severely injured patients across several geographic regions in North America.8 Our group demonstrated significant geographic variation in outcomes after helicopter transport for trauma.9 Some have found higher injury and mortality rates for MVC in the Southern US.13, 15 Washington et al noted an eight state Southeast region comprised of Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Tennessee consistently have higher fatal MVC than other areas of the US.24 Similarly, our findings demonstrate a clustering of higher injury fatality rates within the Southeast US among these eight states. Further, none of these eight states have a clustered pattern of trauma centers. Six have a dispersed trauma center pattern, while two have a random pattern. Authors have postulated this disparity may exist as a result of differences in seat-belt use, alcohol use, vehicle miles traveled, speed limits, and access to emergency medical services.12, 14, 24 These factors deserve further investigation as potential mediators of the association between geographic trauma center distribution and injury fatality rates.
Rural versus urban location has also been strongly implicated in outcomes after injury. Several groups have shown that the risk of death is higher for MVC occurring in rural locations.14, 15 Travis and colleagues reported similar findings, noting that higher speeds, lower seat-belt use, and other pre-crash factors may be more important than limitations in emergency care.25 Gomez et al performed a population-based study in Canada, reporting a disproportionate number of deaths in rural versus urban non-trauma center emergency departments, suggesting delay in trauma center access contributes to poorer outcomes in rural areas.6 Further, Hsia and colleagues have shown that patients in rural areas have significant barriers to trauma center access in the US.7, 10, 26 These issues also factor in the results of this study, as seen by the interaction of population density, trauma center distribution, and injury fatality rates. Injury fatality rates rose as population density decreased, and dispersed states had a lower population density compared to clustered states. More rural states are less likely to have multiple large population centers to support higher level trauma centers, leading to more dispersed patterns across these states. Dispersed states also appear to have greater availability of lower level centers in areas where level I or II centers are not present; however this was not significantly different from clustered states and coverage by lower level centers was not correlated with fatality rates. This factor was also controlled for in regression analysis, and it does not appear lower fatality rates in clustered states are due to a more developed network of rural lower level centers that stabilize patients for transfer to higher level centers clustered in urban areas. Our regression analysis also adjusted for population density and proportion of urban versus rural area, and thus the rurality of states does not appear to exclusively explain the association between distribution of trauma centers and injury fatality rates.
Further, analysis at the county level indicates dispersed states may not have maximized placement of trauma centers in areas of highest population density when compared to clustered states. This also underscores the importance of population density to trauma system configuration and suggests that differences in state rurality may not be the sole factor driving the relationship between geographic trauma center distribution and injury related mortality seen here.
Finally, although the number of trauma centers per 1million persons is an important measure of trauma center distribution relative to the population, it did not correlate with injury fatality rates and was not significantly different between clustered and dispersed states. These results suggests the specific geographic location of centers relative to the population density within trauma systems is potentially an equally important metric of trauma center distribution to consider in addition to an aggregate measure such as number of centers per 1million persons.
These results are intriguing, but should be interpreted with caution. It is unlikely that clustering of trauma centers at the state-level intrinsically drives lower fatality rates. More likely, it is a marker of several other system-level factors, such as population distribution and access to trauma care on a wider scale as noted above. These results cannot define the optimal number of trauma centers for a given area or population, nor the optimal number of population centers within states that should be served by level I or II trauma centers. Further, it assesses existing centers in their current configuration and cannot predict outcomes if centers were placed in different geographic distributions. Thus, these results should not be interpreted as a call to re-organize existing state trauma systems to force clustering of trauma centers. Rather, these results should been seen as support for a rational approach to trauma system design. The American College of Surgeons Committee on Trauma recently released a statement on trauma center designation based on system need, which advocates consideration of overall trauma system characteristics and population needs rather than solely evaluating individual hospital capabilities.27 These results support that approach, in that geographic factors and distribution of trauma center relative to population density should be consider among other factors as trauma systems in the US mature.
Several groups have used geospatial analysis to optimize trauma system development. Branas et al developed the Trauma Resource Allocation Model for Ambulances and Hospitals, which used a spatial model of injured patients in Maryland to optimally place trauma centers and medical helicopter bases.16 They reported improved access to trauma care within 30 minutes for the state population using their algorithm to relocate trauma centers and helicopter bases. Jansen et al designed the Geospatial Evaluation of Systems of Trauma Care (GEOS) model to help plan and optimize national trauma resource allocation in Scotland.19 The authors note the GEOS model has several advantages over others, including use of prehospital triage guidelines to guide patient flow and the ability to model constraints based on center resources, bed capacities, and helicopter availability. This group has also employed incident specific geospatial profiling of injuries in Scotland to further aid trauma system planning.18 Others have also used geographic information system approaches to optimize the time benefits of helicopter versus ground transport of trauma patients.28, 29
This study has several limitations. First, this is a retrospective ecological study. We were limited to obtaining data available for the study time period from several sources. This limited the data available for potential confounders and interactions among factors related to injury mortality. Second, data was evaluated at the state-level, thus the complexities of individual patients are not captured. Moreover, the current analysis cannot fully examine the potential mechanisms underlying the findings here. As noted above, analysis was at the state-level; however regional trauma systems more commonly regional exist within states and catchment areas may include portions of neighboring states which would not be captured here. Thus, different geographic distribution patterns may be associated with mortality when evaluated at different geographic levels. The NNR analysis considers land area in determining geographic distribution; however these results clearly show geographic population distribution is an important factor in trauma center distribution. The use of aggregated state-level data also assumes uniform geographic distribution of injuries across the state, while injuries cluster in population centers as well.18 Unfortunately, more granular county-level injury fatality rates were not available for the study time period. We only considered trauma centers; however the geographic distribution of other trauma system resources such as helicopter bases can also influence outcome.30 In addition to the geospatial configuration of trauma centers, appropriate triage and utilization of these resources varies geographically and impacts outcomes.
Despite these limitations, we believe this exploratory analysis demonstrates a compelling argument that geographic factors at the system-level are associated injury related mortality in the US, and more directed study can begin to elucidate key elements of this relationship going forward.
CONCLUSION
The geographic distribution of trauma centers correlates with injury related mortality, with clustering of state trauma centers associated with lower injury fatality rates. This may be due to superior access to trauma care through improved matching of system resources to population centers; however further study is needed to investigate the mechanisms underlying these exploratory findings. These results point to the importance of geospatial factors in outcome after injury and may have implications for rational trauma system planning as this domain of work advances.
Supplementary Material
Trauma center density by population in the United States. Number of level I or II trauma center per 1 million persons is represented by color ramp, with higher values represented in darker red and lower values represented in lighter red. Trauma center geographic distribution based on significance of the NNR is represented by patterned overlay. Level I or II trauma center geographic locations are represented by black stars.
Continuous population density and geographic distribution of all trauma centers in the United States. Population density is represented by color ramp, with higher values represented in blue and lower values represented in yellow. Trauma center geographic distribution based on significance of the NNR is represented by patterned overlay. Level I or II trauma center geographic locations are represented by black stars; Level III-V trauma center geographic locations are represented by green stars. Shaded areas represent counties with a level III-V trauma center but without a level I or II trauma center.
Acknowledgments
No funding or support was directly received to perform the current study. Dr. Brown receives support from an institutional T-32 Ruth L. Kischstein National Research Service Award training grant (5-T32-GM-008516-20) from the National Institutes of Health. Dr. Sperry receives support from a career development award (K23GM093032) from the National Institute of General Medical Sciences.
Footnotes
There are no conflicts of interest for the current study
This paper was presented as an oral podium presentation at the 74th annual meeting of the American Association for the Surgery of Trauma, September 9–12, 2015, in Las Vegas, Nevada.
AUTHOR CONTRIBUTIONS: J.B.B. designed the study, performed the literature search, data collection, and data analysis. J.B.B., M.R.R., and J.L.S. participated in initial manuscript preparation. All authors contributed to data interpretation and critical revision of the manuscript.
Contributor Information
Joshua B. Brown, Email: brownjb@upmc.edu.
Matthew R. Rosengart, Email: rosengartmr@upmc.edu.
Timothy R. Billiar, Email: billiartr@upmc.edu.
Andrew B. Peitzman, Email: peitzmanab@upmc.edu.
Jason L. Sperry, Email: sperryjl@upmc.edu.
REFERENCES
- 1.Rhee P, Joseph B, Pandit V, Aziz H, Vercruysse G, Kulvatunyou N, Friese RS. Increasing trauma deaths in the United States. Ann Surg. 2014;260:13–21. doi: 10.1097/SLA.0000000000000600. [DOI] [PubMed] [Google Scholar]
- 2.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. 2006/01/27. [DOI] [PubMed] [Google Scholar]
- 3.MacKenzie EJ, Weir S, Rivara FP, Jurkovich GJ, Nathens AB, Wang W, Scharfstein DO, Salkever DS. The value of trauma center care. J Trauma. 2010;69:1–10. doi: 10.1097/TA.0b013e3181e03a21. [DOI] [PubMed] [Google Scholar]
- 4.Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000;48:25–30. doi: 10.1097/00005373-200001000-00005. discussion 30–21. 2000/01/27. [DOI] [PubMed] [Google Scholar]
- 5.Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, Blatt AJ, ReVelle CS. Access to trauma centers in the United States. JAMA. 2005;293:2626–2633. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 6.Gomez D, Haas B, Doumouras AG, Zagorski B, Ray J, Rubenfeld G, McLellan BA, Boyes DM, Nathens AB. A population-based analysis of the discrepancy between potential and realized access to trauma center care. Ann Surg. 2013;257:160–165. doi: 10.1097/SLA.0b013e31827b9649. [DOI] [PubMed] [Google Scholar]
- 7.Hsia RY, Wang E, Torres H, Saynina O, Wise PH. Disparities in trauma center access despite increasing utilization: data from California, 1999 to 2006. J Trauma. 2010;68:217–224. doi: 10.1097/TA.0b013e3181a0e66d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Minei JP, Schmicker RH, Kerby JD, Stiell IG, Schreiber MA, Bulger E, Tisherman S, Hoyt DB, Nichol G Resuscitation Outcome Consortium I. Severe traumatic injury: regional variation in incidence and outcome. Ann Surg. 2010;252:149–157. doi: 10.1097/SLA.0b013e3181df0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown JB, Gestring ML, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. Geographic Variation in Outcome Benefits of Helicopter Transport for Trauma in the United States. Annals of Surgery. 2015:1. doi: 10.1097/SLA.0000000000001047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsia R, Shen YC. Possible geographical barriers to trauma center access for vulnerable patients in the United States: an analysis of urban and rural communities. Arch Surg. 2011;146:46–52. doi: 10.1001/archsurg.2010.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mann NC, MacKenzie E, Teitelbaum SD, Wright D, Anderson C. Trauma System Structure and Viability in the Current Healthcare Environment: A State-by-State Assessment. The Journal of Trauma: Injury, Infection, and Critical Care. 2005;58:136–147. doi: 10.1097/01.ta.0000151181.44658.0a. [DOI] [PubMed] [Google Scholar]
- 12.Clark DE. Effect of population density on mortality after motor vehicle collisions. Accid Anal Prev. 2003;35:965–971. doi: 10.1016/s0001-4575(02)00104-5. [DOI] [PubMed] [Google Scholar]
- 13.Clark DE, Cushing BM. Predicting regional variations in mortality from motor vehicle crashes. Acad Emerg Med. 1999;6:125–130. doi: 10.1111/j.1553-2712.1999.tb01050.x. 1999/03/03. [DOI] [PubMed] [Google Scholar]
- 14.Clark DE, Cushing BM. Rural and urban traffic fatalities, vehicle miles, and population density. Accid Anal Prev. 2004;36:967–972. doi: 10.1016/j.aap.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 15.Goldstein GP, Clark DE, Travis LL, Haskins AE. Explaining regional disparities in traffic mortality by decomposing conditional probabilities. Inj Prev. 2011;17:84–90. doi: 10.1136/ip.2010.029249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Branas CC, MacKenzie EJ, Revelle CS. A Trauma Resource Allocation Model for Ambulances and Hospitals. Health Services Research. 2000;35:489–507. [PMC free article] [PubMed] [Google Scholar]
- 17.Carr B, Branas C. TraumaMaps.org Trauma Center Maps. University of Pennsylvania Cartographic Modeling Laboratory. [Accessed: February 28, 2014];Copyright © 2006 Trustees of the University of Pennsylvania. Available at: www.traumamaps.org. [Google Scholar]
- 18.Jansen JO, Morrison JJ, Wang H, He S, Lawrenson R, Campbell MK, Green DR. Feasibility and utility of population-level geospatial injury profiling: prospective, national cohort study. J Trauma Acute Care Surg. 2015;78:962–969. doi: 10.1097/TA.0000000000000617. [DOI] [PubMed] [Google Scholar]
- 19.Jansen JO, Morrison JJ, Wang H, Lawrenson R, Egan G, He S, Campbell MK. Optimizing trauma system design: the GEOS (Geospatial Evaluation of Systems of Trauma Care) approach. J Trauma Acute Care Surg. 2014;76:1035–1040. doi: 10.1097/TA.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Injury Prevention & Control: Data & Statistics (WISQARS): Fatal Injury Data. [Accessed: Dec 8, 2014]; Available at: http://www.cdc.gov/injury/wisqars/fatal.html.
- 21.Flanigan M, Blatt A. Atlas and Database of Air Medical Services (ADAMS) National and State Maps Showing Coverage Areas for Air Medical Rotor and Fixed Wing Services, 8th Edition. Center for Transportation Injury Research. 2010 [Google Scholar]
- 22.Clark DE, Osler TM, DR H. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. [Accessed: Dec 10, 2014]; Available at: https://ideas.repec.org/c/boc/bocode/s457028.html. [Google Scholar]
- 23.Ward MD, Skrede-Gleditsch K. Spatial Regression Models. Thousand Oaks, CA: SAGE; 2008. [Google Scholar]
- 24.Washington S, Metarko J, Fomunung I, Ross R, Julian F, Moran E. An inter-regional comparison: fatal crashes in the southeastern and non-southeastern United States: preliminary findings. Accid Anal Prev. 1999;31:135–146. doi: 10.1016/s0001-4575(98)00055-4. 1999/03/20. [DOI] [PubMed] [Google Scholar]
- 25.Travis LL, Clark DE, Haskins AE, Kilch JA. Mortality in rural locations after severe injuries from motor vehicle crashes. J Safety Res. 2012;43:375–380. doi: 10.1016/j.jsr.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hsia RY, Shen YC. Rising closures of hospital trauma centers disproportionately burden vulnerable populations. Health Aff (Millwood) 2011;30:1912–1920. doi: 10.1377/hlthaff.2011.0510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American College of Surgeons. Statement on trauma center designation based upon system need. [Accessed: Sept 6, 2015]; Available at: http://bulletin.facs.org/2015/01/statement-on-trauma-center-designation-based-upon-system-need/ [PubMed] [Google Scholar]
- 28.Shaw JJ, Psoinos CM, Santry HP. It's All About Location, Location, Location: A New Perspective on Trauma Transport. Ann Surg. 2015 doi: 10.1097/SLA.0000000000001265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Widener MJ, Ginsberg Z, Schleith D, Floccare DJ, Hirshon JM, Galvagno S. Ground and Helicopter Emergency Medical Services Time Tradeoffs Assessed with Geographic Information. Aerosp Med Hum Perform. 2015;86:620–627. doi: 10.3357/AMHP.4173.2015. [DOI] [PubMed] [Google Scholar]
- 30.Rhinehart ZJ, Guyette FX, Sperry JL, Forsythe RM, Murdock A, Alarcon LH, Peitzman AB, Rosengart MR. The association between air ambulance distribution and trauma mortality. Ann Surg. 2013;257:1147–1153. doi: 10.1097/SLA.0b013e31827ee6b0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trauma center density by population in the United States. Number of level I or II trauma center per 1 million persons is represented by color ramp, with higher values represented in darker red and lower values represented in lighter red. Trauma center geographic distribution based on significance of the NNR is represented by patterned overlay. Level I or II trauma center geographic locations are represented by black stars.
Continuous population density and geographic distribution of all trauma centers in the United States. Population density is represented by color ramp, with higher values represented in blue and lower values represented in yellow. Trauma center geographic distribution based on significance of the NNR is represented by patterned overlay. Level I or II trauma center geographic locations are represented by black stars; Level III-V trauma center geographic locations are represented by green stars. Shaded areas represent counties with a level III-V trauma center but without a level I or II trauma center.