Abstract
Purpose
This study sought to examine whether perceived interpersonal racism in the form of racial micro aggressions was associated with preterm birth (PTB) and whether the presence of depressive symptoms and perceived stress modified the association.
Methods
Data stem from a cohort of 1410 Black women residing in Metropolitan Detroit, Michigan enrolled into the Life-course Influences on Fetal Environments (LIFE) Study. The Daily Life Experiences of Racism and Bother (DLE-B) scale measured the frequency and perceived stressfulness of racial micro aggressions experienced during the past year. Severe past-week depressive symptomatology was measured by the Centers for Epidemiologic Studies-Depression scale (CES-D) dichotomized at ≥23. Restricted cubic splines were used to model non-linearity between perceived racism and PTB. We used the Perceived Stress Scale (PSS) to assess general stress perceptions.
Results
Stratified spline regression analysis demonstrated that among those with severe depressive symptoms, perceived racism was not associated with PTB. However, perceived racism was significantly associated with PTB among women with mild to moderate (CES-D score ≤22) depressive symptoms. Perceived racism was not associated with PTB among women with or without high amounts of perceived stress.
Conclusions
Our findings suggest that racism, at least in the form of racial micro aggressions, may not further impact a group already at high risk for PTB (those with severe depressive symptoms), but may increase the risk of PTB for women at lower baseline risk.
Keywords: Premature birth, Racism, Depression, Stress, Psychological
INTRODUCTION
Reducing the rate of preterm birth (PTB) has been a national priority in the United States for decades.[1, 2] Efforts to better understand PTB and implement interventions have only led to a small decrease in the PTB rate (2006: 12.8% vs. 2013: 11.4%).[3] Yet racial disparities persist; 2013 US vital records show Blacks have a PTB rate of 16.3% compared to 10.2% for Whites.[3] A better understanding of the mechanisms that underlie the disadvantage of Black women with regard to PTB is needed.
In a race-conscious society like the United States, racism likely plays an important role in health disparities.[4–8] Racism is a system of oppression that structures opportunity and assigns value for interpersonal exchange based on someone’s perceived race.[4, 6, 7] Racism operates at multiple levels: institutional, interpersonal, internalized and cultural.[6, 7] The focus in this manuscript is interpersonal racism, which is defined as prejudiced assumptions about an individual’s abilities, motives, and intentions due to the individual’s race and discrimination, defined as unfair treatment of an individual due to his/her race.[6, 7] Experiences of interpersonal racism and racial discrimination can be stressful; it has been suggested that these racism-related stressors lead to heightened states of psychological and physiological stress responses, and result in poor physical health outcomes.[6, 9] For example, induced stress responses may increase risk of PTB via adoption of adverse health behaviors (e.g., smoking, poor diet) known to be risk factors for PTB as a way of coping; as well as psychological pathways such as depression; and/or immune/infection pathways.[10]
Recent literature reviews on interpersonal racism or racial discrimination and birth outcomes report mixed results with both null and adverse findings.[11, 12] For example, Dole et al.,[13] Rosenberg et al.,[14] Mustillo et al.,[15] and Rankin et al. [16] each found perceived experiences of racial discrimination increased Black women’s risk of PTB with excess risk ranging from 1.3 to 3 fold.[12] However, other studies have not found a significant association with PTB[17, 18] or gestational age.[19, 20] The heterogeneity in findings may be due in part to the application of different scales or instruments and their conceptualization and measurement of individual’s experiences of interpersonal racism and racial discrimination.[21] Racism-related stress is multidimensional. Minorities may experience interpersonal racism or racial discrimination through significant but acute or discrete, observable life events (e.g, being denied a loan); these are often called major experiences of discrimination.[6, 21, 22] They may also experience interpersonal racism or discrimination via racial micro aggressions or micro experiences, -chronic or episodic daily race-related hassles or events[21] that are “subtle, innocuous, preconscious or unconscious degradations and putdowns.”[23] Racism is fundamental and embedded in all aspects of Black women’s lives, which transfers to differential stressors and health risks with potentially consequential racially-disparate perinatal health outcomes.[19]
The majority of studies examining the relationship between interpersonal racism or racial discrimination and birth outcomes have focused on the impact of major experiences of discrimination, rather than on micro aggressions.[12] Racial micro aggressions are often encountered with greater frequency than major experiences, and “create an atmosphere of expectation that something racist will happen.”[6] While a single perceived event may not be perceived as serious, accumulation of these seemingly-innocuous events on a weekly or even daily basis over the lifecourse may more readily overtax an individual’s stress response systems than major experiences of racial discrimination.[6, 23]
Beyond the measurement of interpersonal racism or racial discrimination, the variation in associations with birth outcomes could be due to underlying effect modification. Research suggests [24]that other psychosocial risk factors may moderate the relationship between interpersonal racism and PTB, such that the impact of racism on PTB may only be expressed in the presence or absence of these other psychosocial factors. For example, in work by our team[24] in a low-income cohort of Black women residing in Baltimore, MD, there appeared to be no effect of lifetime exposure to interpersonal racism in the form of major experiences of discrimination. However, the interpersonal racism-PTB association was modified by the presence of depressive symptoms and perceived stress. Among all women, except those reporting low levels of stress and depressive symptoms, perceived racism was associated with a sizeable increased risk of PTB. This suggests that the impact of racism on PTB may be missed when examined in isolation without considering the influence of psychosocial factors in women’s lives, an idea which is also supported in the developmental literature for outcomes influenced by other social causes.[25]
The aim of this study was to assess the association between perceived interpersonal racism in the form of racial micro aggressions and the rate of PTB in a cohort of Black women. We also investigated whether the relationship between racial micro aggressions and the rate of PTB was modified by psychosocial risk factors during pregnancy.
METHODS
Sample and Study Design
The Life-course Influences of Fetal Environments (LIFE) study, a retrospective cohort study, was conducted between June 2009 and December 2011. Women were eligible for this study if they self-identified as Black or African-American, were 18–45 years old, and recently gave birth to a singleton at a suburban hospital in Metropolitan Detroit, Michigan. Women eligible to participate in the LIFE study were approached for enrollment (N=1999). A total of 1410 (70.6%) women consented and participated in structured interviews within 24–48 hours post-delivery during their postpartum hospitalization. Black women born outside of the U.S. were eligible to participate in LIFE, however, they accounted for less than 2% of enrolled participants. All interviewers were Black females to reduce the possibility of bias as a result of race-of-interviewer effects.[26] Additional information was obtained about the woman and her newborn via medical record abstraction by trained study staff. LIFE was approved by university and hospital institutional review boards.
Measures
Exposure
Racism
Racism was operationalized with the Daily Life Experiences of Racism and Bother (DLE-B) scale,[27] which measures the extent to which daily racial micro aggressions are perceived to occur and bother an individual during the index pregnancy and up to one year prior to the index pregnancy. Examples of micro aggressions assessed include: being ignored or overlooked, being treated rudely or disrespectfully, being mistaken for a server, and overhearing an offensive joke. Using a 6-point Likert scale, participants were asked to report how often (1-“never” 2-“< once a year”, 3-“few times a year”, 4-“about once a month”, 5-“few times per year”, 6-“once a week or more”) because of race they experienced each of the 20 listed racial micro aggressions in their daily life; and how much the experience(s) bothered them (1-“never happened to me”, 2-“not at all”, 3-“a little”, 4-“somewhat”, 5-“a lot”,6-“extremely”). To create the DLE-B summary score, the frequency of occurrence for each micro aggressor was weighted by the participant’s response to how much the micro aggressor bothered them. The 20 items were summed; summary scores ranged from 20 (low) to 720 (high). The DLE-B has been shown to be a valid and reliable instrument for use with historically oppressed racial/ethnic groups.[27] In the LIFE study, the DLE-B had a Cronbach’s α of 0.92.
Since some literature has found independent effects of racism exposure, from the appraisal of that exposure,[28] we did disaggregate and test these two constructs in sensitivity analyses but found similar associations with PTB (not shown). Therefore, we present results from the overall measure here.
Outcome
Preterm Birth
PTB was defined as birth < 37 completed week’s gestation. Based on the American Congress of Obstetricians and Gynecologists recommendations,[29] the following algorithm was used to estimate the “best” gestational age (GA) using information abstracted from the medical record. GA based on early ultrasound (6–20 week’s gestation) was prioritized as the gold standard. In the event that the early ultrasound-based GA was implausible or not available, GA was based on the last menstrual period (LMP). On the rare occasion when neither the early ultrasound-based nor LMP-based GA were plausible or available, a later ultrasound-based GA (after 20 week’s gestation) or the clinician’s estimate of GA at birth was used.
Covariates
Depressive Symptomology
The Centers for Epidemiologic Studies Depression Scale (CES-D) was used to measure depressive symptomology. The 20-item instrument was administered during the postpartum interview; women reported how often during the past week they experienced depressive symptoms using a 4-point Likert scale (0-“rarely” to 3-“most or all of the time”)[30–32]. The CES-D summary score ranges from 0 to 60; a score ≥23 reflected severe depressive symptomology. A CES-D score ≤ 22 reflected mild to moderate depressive symptoms[14, 32] The Cronbach’s α⊤ for the CES-D for LIFE participants was 0.87.
Perceived Stress
The Perceived Stress Scale (PSS) is a 14-item instrument used to assess the extent to which situations or events occurring in an individual’s life are appraised as stressful in the past month.[33] Each item on the PSS was measured with a 5-point Likert scale ranging from 1-“never” to 5-“very often”; scores ranged from 14 to 64. Higher scores reflected higher levels of perceived stress (Cronbach’s α = 0.87).
Other Covariates
Potential confounders from structured postpartum interview and abstracted medical records were: maternal age, educational attainment, current subjective financial situation (coded as 1-“very poor, not enough to get by”, 2-“barely enough to get by”, 3-“enough to get by but no extras”, 4-“more than enough to get by” and 5-“well to do”), prenatal smoking and self-rated physical health (See Table 1 for additional detail).
Table 1.
Distribution of Maternal Characteristics: Univariate and Bivariate Distribution with Preterm Birth in the LIFE Study (N=1232)
| Variable | Total Sample N (%) | Preterm Birth
|
||
|---|---|---|---|---|
| N | % | Crude PR (95% CI) | ||
| Preterm Birth | 204 (16.6) | - | - | - |
| Age | ||||
| 18–19 | 105 (8.5) | 13 | 12.4 | 0.87 (0.49, 1.54) |
| 20–24 | 373 (30.3) | 68 | 18.2 | 1.30 (0.91, 1.80) |
| 25–29 | 337 (27.4) | 48 | 14.2 | Referent |
| 30–34 | 235 (19.1) | 36 | 15.3 | 1.08 (0.72, 1.60) |
| 35 or older | 182 (14.8) | 39 | 21.4 | 1.50 (1.03, 2.20) |
| Current Financial Situation | ||||
| Very poor/barely enough | 93 (7.6) | 20 | 21.5 | 1.32 (0.86, 2.02) |
| Enough to get by | 624 (50.7) | 102 | 16.4 | Referent |
| More than enough | 390 (31.7) | 65 | 16.7 | 1.02 (0.77, 1.35) |
| Well to do | 125 (10.2) | 17 | 13.6 | 0.83 (0.52–1.34) |
| Educational attainment | ||||
| No college | 344 (27.9) | 56 | 16.3 | Referent |
| Some college | 888 (72.1) | 148 | 16.7 | 1.02 (0.77, 1.36) |
| Prenatal smokinga | ||||
| Never | 906 (73.5) | 154 | 17.0 | 1.32 (0.89, 1.98) |
| Smoked, but not in pregnancy | 187 (15.2) | 24 | 12.8 | Referent |
| Smoked during pregnancy | 139 (11.3) | 26 | 18.7 | 1.47 (0.88, 2.43) |
| Overall Self-rated Physical Health | ||||
| Excellent/Very Good | 520 (42.2) | 67 | 12.9 | Referent |
| Good | 413 (33.5) | 74 | 17.9 | 1.39 (1.03, 1.89) |
| Fair/Poor | 299 (24.3) | 63 | 21.1 | 1.64 (1.20, 2.24) |
| Daily Life Experiences of Racism & Bother Scale (DLE-B)a | ||||
| 1st quartile (20–38) | 305 (24.8) | 39 | 12.8 | Referent |
| 2nd quartile (39–72) | 305 (24.8) | 65 | 21.3 | 1.67 (1.16, 2.40) |
| 3rd quartile (73–128) | 307 (24.9) | 52 | 16.9 | 1.32 (0.90, 1.94) |
| 4th quartile (129–637) | 315 (25.6) | 48 | 15.2 | 1.19 (0.81, 1.76) |
| Centers for Epidemiologic Depression Scale (CES-D) | ||||
| Mild/Moderate symptoms (score≤22) | 980 (79.6) | 143 | 14.6 | Referent |
| Severe symptoms (score≥23) | 252 (20.5) | 61 | 24.2 | 1.66 (1.27, 2.16) |
| Perceived Stress Scale (PSS) | ||||
| Less Stressed (score ≤ 34) | 570 (46.3) | 88 | 15.4 | Referent |
| More Stressed (score >35) | 662 (53.7) | 116 | 17.5 | 1.14 (0.88,1.46) |
DLE-B Higher score indicates more experiences of racial discrimination.
Note: PR, Prevalence Ratio; CI, Confidence Interval
Statistical Analyses
Statistical analyses were conducted using SAS version 9.3 (Cary, NC). To examine the distribution of PTB by maternal characteristics and racism we conducted bivariate analyses by employing log-binomial regression models to estimate the unadjusted and adjusted prevalence ratio (PR) and associated 95% confidence interval (CI).[34] Log-binomial models were used to approximate PRs instead of logistic regression since the PTB rate in the cohort (16.4%) does not meet the rare disease assumption (outcome prevalence <10%).[35]
To better examine non-linearities in the relationship between the DLE-B scale and PTB, suggested by initial assessments using quartiles of the DLE-B, restricted cubic spline transformations were used. Restricted cubic splines allow for a high degree of flexibility when modeling the non-linear relationship between a predictor and outcome variables, but also provide constraints to ensure a smooth curve and linearity in the tails of the function.[36] Spline transformations with 4 degrees of freedom were run using the SAS Macros made available by Harrell.[37] Knots were based at the 5th, 35th, 65th and 95th quantiles of the DLE-B score using the SAS Macro DASPLINE. The transformations were then incorporated into log-binomial regression models.
The DLE-B spline was used in unadjusted and adjusted regression models; adjusted models controlled for maternal age, maternal education, current financial situation, smoking, overall self-reported physical health, depressive symptoms, and perceived stress. Spline significance was determined via likelihood ratio test.
To test whether depressive symptoms or perceived stress modified the relationship between the DLE-B and the rate of PTB, we ran the adjusted regression models with the inclusion of an interaction term between DLE-B and either modifier (depressive symptoms or perceived stress). Significance of the interaction term was assessed using a Chi-squared test. Additionally, we stratified our adjusted spline regression model by the potential modifier (e.g. severe vs. mild to moderate depressive symptomology).
All variables were assessed for missing values. Less than 1% of women had missing data on the outcome, while 7.5% of women had missing information on the exposure, DLE-B. The remaining covariates displayed low amounts (<4%) of missing data. For all covariates, the exposure variables, and outcomes measures, list-wise deletion was performed. A total of 1232 women (87.8% of the cohort) were included in the analysis. Women with missing data were not significantly different from those in the final analytic sample.
RESULTS
Sample Characteristics
Descriptive statistics of participants are shown in Table 1. Approximately 39% of the women were <25 years old, 50.5% report they had enough finances to get by but no extras, and 72% of the women had at least some college education. The mean DLE-B was 96.5, sd=80.1. The mean CES-D score, 15.3, sd=9.8, and PSS score, 35.5, sd=8.1, were slightly higher than mean CES-D and PSS scores of population-based samples of women. [38, 39] The prevalence of PTB in the analytic sample was 16.6%.
Bivariate Associations with PTB
There was a significant association between the DLE-B racism score and PTB. Women in the 2nd DLE-B quartile exhibited a greater probability of PTB than women with higher or lower scores. For example, women in the 2nd DLE-B quartile were 1.67 times (95% CI: 1.16–2.40) as likely to have a PTB than women whose DLE-B scores were in the 1st quartile. Women in the 3rd and 4th quartiles had higher probabilities of PTB compared to the 1st quartile, although these differences were nonsignificant (Table 1).
Regression Models
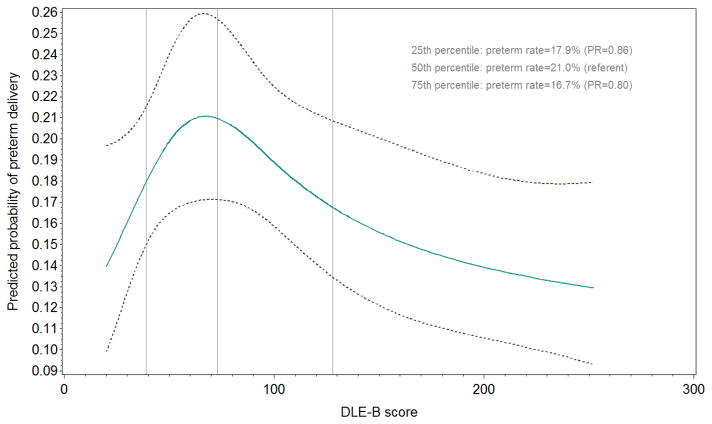
In unadjusted spline regression analyses, the DLE-B racism measure was not significantly associated with PTB rate; however, after adjustment for maternal age, education, financial situation, smoking during pregnancy, overall self-rated physical health severe depressive symptoms and perceived stress, the DLE-B spline was marginally significantly associated with PTB. Figure 1 illustrates the nonlinear adjusted relationship between the DLE-B and the probability of having a PTB. The predicted probability (PP) of PTB increased from a DLE-B score of 20 (PP=0.14, 95%CI: 0.10–0.20), peaked when the DLE-B score was 73 (PP=0.21, 95% CI:0.17–0.26), then decreased continuously as the DLE-B score increased. Also, in the adjusted main effects model severe depressive symptomology was significantly associated with PTB (adjusted PR=1.75 (1.29–2.36); while perceived stress was not (adjusted PR=0.89, 95% CI: 0.37–1.19), data not shown in tables.
Figure 1.
Nonlinear effect of the Daily Life Experiences of Racism and Bother (DLE-B) score on preterm delivery rates among women (N=1232).
X axis represents the Daily Life Experiences of Racism and Bother (DLE-B) score. The Y axis represent the predicted probability of preterm birth. Solid line represents the predicted probability of preterm birth among women. Dashed line represents 95% confidence interval. Estimates are adjusted for maternal age, subjective financial situation, prenatal smoking, overall self-reported physical health, depressive symptoms, and perceived stress. Note: DLE-B scores above the 95th percentile are not shown.
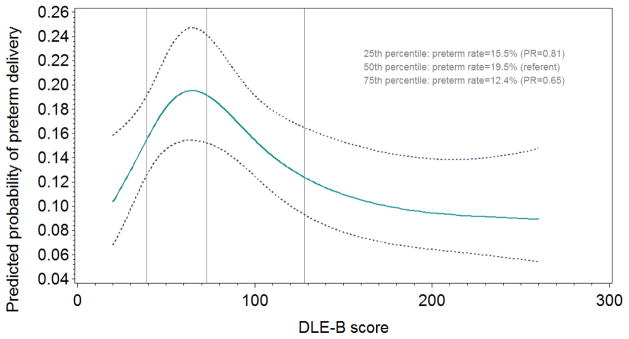
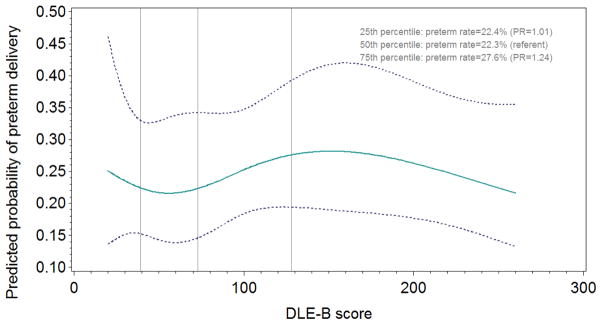
Next using separate spline regression models, we tested whether severe depressive symptomology or perceived stress modified the relationship between the DLE-B racism measure and PTB. The racism-depressive symptoms interaction term approached significance (p=0.134), while the racism-perceived stress interaction term was non-significant. We further explored the interaction between the DLE-B racism measure and each psychosocial factor (in separate models) via stratification. Figure 2 illustrates this nonlinear adjusted relationship among women with mild to moderate depressive symptoms, while Figure 3 illustrates the association among women with severe depressive symptoms. In spite of the non-significant interaction, the patterns of these associations appear qualitatively different. For women with mild to moderate depressive symptoms, the PP of PTB increased steeply from a DLE-B racism score of 20 to approximately 72 (at which PP=0.19, 95% CI:0.15–0.24), then decreased until the DLE-B score was approximately 200 (PP=0.10, 95% CI: 0.06–0.14) after which the PP of PTB plateaued (Figure 2). For women with severe depressive symptoms, the PP of PTB is at its lowest when the DLE-B racism score was 56 (PP=0.22, 95% CI: 0.14–0.33) and then increased slightly until the DLE-B was approximately 150 (PP=0.28, 95% CI: 0.19–0.42, Figure 3).
Figure 2.
Nonlinear effect of the Daily Life Experiences of Racism and Bother (DLE-B) score on preterm delivery rates among women with mild to moderate depressive symptomology.
X axis represents the Daily Life Experiences of Racism and Bother (DLE-B) score. The Y axis represent the predicted probability of preterm birth. Solid line represents the predicted probability of preterm birth among women with mild to moderate depressive symptoms (n=980). Dashed line represents 95% confidence interval. Estimates are adjusted for maternal age, subjective financial situation, prenatal smoking, overall self-reported physical health and perceived stress. Note: DLE-B scores above the 95th percentile are not shown.
Figure 3.
Nonlinear effect of the Daily Life Experiences of Racism and Bother (DLE-B) score on preterm delivery rates among women with severe depressive symptomology.
X axis represents the Daily Life Experiences of Racism and Bother (DLE-B) score. The Y axis represent the predicted probability of preterm birth. Solid line represents the predicted probability of preterm birth among women with mild to moderate depressive symptoms (n=252). Dashed line represents 95% confidence interval. Estimates are adjusted for maternal age, subjective financial situation, prenatal smoking, overall self-reported physical health and perceived stress. Note: DLE-B scores above the 95th percentile are not shown.
In our exploration of the racism-perceived stress interaction, the stratified spline regression analysis showed that the DLE-B was not significantly associated with PTB among women with lower perceived stress or among women with higher perceived stress. Supplemental Figure S1 shows the nonlinear adjusted relationship among women with lower perceived stress, while Supplemental Figure S2 shows the association among women with higher perceived stress.
DISCUSSION
We explored whether racial micro aggressions were associated with PTB and whether this association was modified by depressive symptoms or perceived stress among Black women. Interpersonal racism in the form of racial micro aggressions was associated with PTB in bivariate models in a non-linear fashion. We also found that depressive symptoms modified the racism-PTB association, such that moderate levels of daily experiences of racism were associated with increased PTB rates (compared with low racism exposure) among women with mild to moderate depressive symptomology, but not among women with severe depressive symptoms. These results taken together suggest that racism, at least in the form of racial micro aggressions, may not further impact a group already at high risk for PTB based on other exposures, however, it may increase the risk of PTB for women with a lower baseline risk.
Only a handful of published studies have examined interpersonal racism or racial discrimination as a risk factor for adverse birth outcomes.[13, 15, 16, 18, 24, 41–42] For example, Dole and colleagues[13] found that Black women who reported ever experiencing racial discrimination had a 40% greater PTB risk (RR = 1.4, 95% CI: 1.0, 2.0) than Black women who did not report experiences of discrimination. More recently, Rankin and colleagues[16] found that Black women who reported high amounts of perceived racial discrimination during the past year were 2.5 (95% CI: 1.5–5.2) times as likely to have a PTB or low birthweight infant than Black women who perceived low to moderate levels of racial discrimination. However neither they nor other investigators have previously reported on whether the presence of other psychosocial factors moderated the association between racism and PTB or other birth outcomes.
Effect modification of racism on birth outcomes is supported theoretically. For example, developmental scientists often posit contingent and nonlinear effects resulting from social causation, since humans develop within dynamic, complex systems where interactions emerge from accumulation of different exposures over time.[25] Prior work by our team has also documented effect modification empirically.[24] This work, however, focused on lifetime effects of major experiences of racism, as we did not have measures of daily life hassles of interpersonal racism during more discrete periods such as pregnancy. Our findings in this study roughly align with our prior findings in that the association between interpersonal racism and PTB was moderated by depressive symptoms. However, the direction in which depressive symptoms modified the relationship in this study differed. This may be due in part to the differences in the types of racism measured in each study, as well as differences in the socioeconomic composition of Black women in each study. Women in the Baltimore study were all from socioeconomically disadvantaged backgrounds, whereas women in the LIFE study were higher SES in terms of education and perceived financial situation.
In a review of the literature on interpersonal racism and birth outcomes,[13–15, 18, 19, 20, 42, 43–45] whether focused on lifetime or daily experiences, we were unable to find a study that reported on analyses that explored nonlinearity of effects. In past studies, the racism variables were modeled as dichotomous or linear predictors. This assumes that the effect of racism would operate in the same way across the range of the scale. Yet the literature on racism and blood pressure suggests that those who report very low levels of racism (those in so called “denial”), as well as those who report high levels, might both be at increased risk for hypertension.[40] Rather than using an arbitrary cut point for our measure, we used spline models to empirically identify points at which the PTB risk changed. Subsequently, we found that women with mild to moderate depressive symptoms had the greatest risk for PTB when they reported less exposure to racism, perhaps suggesting ineffective coping when such rare experiences were encountered.
Our study has limitations that should be considered. First, as with any observational study, we are not able to infer causality. We also cannot assess the impact of time-varying covariates on the PTB-perceived racism association, since our study was not longitudinal in nature. However, recruiting women immediately during their postpartum hospital stay may increase the generalizability of our results since we were able to include women with late, interrupted, or sporadic prenatal care with our retrospective cohort approach. Next, as always, unmeasured confounding cannot be ruled out, and a randomized trial for a racism exposure is not feasible. There is potential for measurement error in key constructed variables, including our measure of gestational age; however, nearly all women in our cohort had some contact with medical professionals during the index pregnancy, and had ultrasound measures of their gestational age in their medical records, reducing measurement error. Further, our measures of depressive symptomology and perceived stress were not assessed over the same recall window as our measure of racism; thus, temporal order cannot be established among our variables. The different recall windows could also have contributed to differences in our effect modification estimation if, for example, one-month recall generated more measurement error than in one-week recall. With respect to our exposure racism, research suggests that gendered racism and the context around stress experiences are important for Black women,[46, 47] however, our measure does not take into account the intersection between gender and racism. Additionally, perceived racism in our study (and others) seeking to assess its impact on health may be susceptible to recall bias, with individuals underreporting racist or discriminatory events. This error is likely non-differential with respect to PTB, and potential bias would produce measures of association closer to the null, since studies[48–50] on adverse birth outcomes like congenital malformations[49,50] show little evidence of differential recall by mothers. Lastly, separating exposure to racism from stress appraisal of that racism could theoretically inform mechanisms, however our sensitivity analyses demonstrated similar effects of each subscale to the overall DLE-B scale.
Our study has at the same time several strengths including a sample comprised entirely of Black women, which allowed us to explore potential mechanisms underlying the increased burden of PTB experienced by this group. For example, our analyses included an assessment of moderation by depressive symptoms on the PTB-racism association, which adds to the literature by identifying a group of Black women who may be at greater risk of having an adverse birth event. We also measured perceived interpersonal racism and how much the incidents bothered the study participants during the year prior to the index pregnancy, which improves upon prior measures of racism that sum the incidence of racism during a certain period.[22] Furthermore, our study measures interpersonal racism immediately following pregnancy to assess the pregnancy reference period, whereas in some prior studies[15, 42] collection of racism measures was conducted years after the pregnancy, and as a result could not provide as complete an assessment of potential confounders nor measure current exposure to discrimination. Lastly, our study contributes to the small number of studies that have examined the effect of interpersonal racism or racial discrimination on current birth outcomes.
In summary, perceived experiences of interpersonal racism in the form of racial micro aggressors was found to be associated with PTB rates among Black women with mild to moderate depressive symptoms after adjusting for potential confounders. This association was not evident among women with severe depressive symptoms. Our results suggest that research on the intersection of racism and psychosocial factors like depressive symptomology may provide additional insight into the complex and persistent racial disparities in birth outcomes.
Supplementary Material
Acknowledgments
FUNDING
This research was funded by NIH grant no. [R01HD058510]. Dr. Platt is a Chercheur-national of the Fonds de Recherche en Santé du Quebec (FRSQ), and a member of the McGill University Health Centre Research Institute, which receives core funding from the FRSQ.
Abbreviations
- CES-D
Centers for Epidemiologic Studies Depression scale
- CI
Confidence Interval
- DLE-B
Daily Life Experiences of Racism and Bother scale
- GA
Gestational Age
- LIFE
Life-course Influences of Fetal Environments study
- LMP
Last Menstrual Period
- PTB
Preterm Birth
- PP
Predicted Probability
- PR
Prevalence Ratio
- PSS
Perceived Stress Scale
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.US Department of Health Human Services. Office of Disease Prevention Health Promotion. Healthy People 2020. Washington, DC: US Department of Health and Human Services; 2012. [Google Scholar]
- 2.US Department of Health and Human Services. Healthy People 2010. Washington, DC: US Department of Health and Human Services; 2000. [Google Scholar]
- 3.Martin JA, Hamilton BE, Osterman M, Curtin SC, Matthews T. Births: final data for 2013. National Vital Statistics Reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2015;64(1):1. [PubMed] [Google Scholar]
- 4.Bonilla-Silva E. Rethinking racism: Toward a structural interpretation. Am Sociol Rev. 1997:465–80. [Google Scholar]
- 5.Dion K. Handbook of Psychology. New York: John Wiley & Sons; 2003. Prejudice, racism, and discrimination; pp. 507–36. [Google Scholar]
- 6.Harrell SP. A multidimensional conceptualization of racism-related stress: Implications for the well-being of people of color. Am J Orthopsychiatry. 2000;70(1):42–57. doi: 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- 7.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slaughter-Acey JC, Caldwell CH, Misra DP. The Influence of personal and group racism on entry into prenatal care among African American women. Womens Health Issues. 2013;23(6):e381–e7. doi: 10.1016/j.whi.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. Am Psychol. 1999;54(10):805. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- 10.National Research Council. Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: The National Academies Press; 2007. p. 792. [PubMed] [Google Scholar]
- 11.Acevedo-Garcia D, Rosenfeld LE, Hardy E, McArdle N, Osypuk TL. Future directions in research on institutional and interpersonal discrimination and children’s health. Am J Public Health. 2013;103(10):1754–63. doi: 10.2105/AJPH.2012.300986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giurgescu C, McFarlin BL, Lomax J, Craddock C, Albrecht A. Racial discrimination and the black-white gap in adverse birth outcomes: A review. J Midwifery Womens Health. 2011;56(4):362–70. doi: 10.1111/j.1542-2011.2011.00034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dole N, Savitz DA, Siega-Riz AM, Hertz-Picciotto I, McMahon MJ, Buekens P. Psychosocial factors and preterm birth among African American and White women in central North Carolina. Am J Public Health. 2004;94(8):1358–65. doi: 10.2105/ajph.94.8.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosenberg L, Palmer JR, Wise LA, Horton NJ, Corwin MJ. Perceptions of racial discrimination and the risk of preterm birth. Epidemiology. 2002;13(6):646–52. doi: 10.1097/00001648-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Mustillo S, Krieger N, Gunderson EP, Sidney S, McCreath H, Kiefe CI. Self-reported experiences of racial discrimination and Black-White differences in preterm and low-birthweight deliveries: the CARDIA Study. Am J Public Health. 2004;94(12):2125–31. doi: 10.2105/ajph.94.12.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rankin KM, David RJ, Collins JW., Jr African American women’s exposure to interpersonal racial discrimination in public settings and preterm birth: The effect of coping behaviors. Ethn Dis. 2011;21(3):370. [PubMed] [Google Scholar]
- 17.Mendez DD, Hogan VK, Culhane JF. Institutional racism, neighborhood factors, stress, and preterm birth. Ethn Health. 2014;19(5):479–99. doi: 10.1080/13557858.2013.846300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giurgescu C, Zenk SN, Dancy BL, Park CG, Dieber W, Block R. Relationships among neighborhood environment, racial discrimination, psychological distress, and preterm birth in African American women. J Obstet Gynecol Neonatal Nurs. 2012;41(6):E51–61. doi: 10.1111/j.1552-6909.2012.01409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dominguez TP, Dunkel-Schetter C, Glynn LM, Hobel C, Sandman CA. Racial differences in birth outcomes: the role of general, pregnancy, and racism stress. Health Psychol. 2008;27(2):194. doi: 10.1037/0278-6133.27.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murrell N. Stress, self-esteem, and racism: relationships with low birth weight and preterm delivery in African American women. J Natl Black Nurses Assoc. 1995;8(1):45–53. [PubMed] [Google Scholar]
- 21.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: Findings from community studies. Am J Public Health. 2003;93(2):200–8. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pierce C. Stress analogs of racism and sexism: Terrorism, torture, and disaster. In: Willie C, Reiker P, Kramer B, Brown B, editors. Mental Health, Racism, and Sexism. Pittsburgh: University of Pittsburgh Press; 1995. pp. 277–93. [Google Scholar]
- 24.Misra D, Strobino D, Trabert B. Effects of social and psychosocial factors on risk of preterm birth in black women. Paediatr Perinat Epidemiol. 2010;24(6):546–54. doi: 10.1111/j.1365-3016.2010.01148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hertzman C, Boyce T. How experience gets under the skin to create gradients in developmental health. Annu Rev Public Health. 2010;31:329–47. doi: 10.1146/annurev.publhealth.012809.103538. [DOI] [PubMed] [Google Scholar]
- 26.Davis RE, Couper MP, Janz NK, Caldwell CH, Resnicow K. Interviewer effects in public health surveys. Health Educ Res. 2010;25(1):14–26. doi: 10.1093/her/cyp046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bond M, Kalaja A, Markkanen P, Cazeca D, Daniel S, Tsurikova L, et al. Expanding our understanding of the psychosocial work environment: a compendium of measures of discrimination, harassment and work-family issues. Cincinnati, OH: National Institute for Occupational Safety and Health (NIOSH); 2008. NIOSH Publication No. 2008-104. [Google Scholar]
- 28.Dominguez TP, Schetter CD, Mancuso R, Rini CM, Hobel C. Stress in African American pregnancies: testing the roles of various stress concepts in prediction of birth outcomes. Ann Behav Med. 2005;29(1):12–21. doi: 10.1207/s15324796abm2901_3. [DOI] [PubMed] [Google Scholar]
- 29.Committee opinion no 611: method for estimating due date. Obstet Gynecol. 2014;124(4):863–6. doi: 10.1097/01.AOG.0000454932.15177.be. [DOI] [PubMed] [Google Scholar]
- 30.Canady RB, Stommel M, Holzman C. Measurement properties of the Centers for Epidemiological Studies Depression Scale (CES-D) in a sample of African-American and non-Hispanic White pregnant women. J Nurs Meas. 2009;17(2):91. doi: 10.1891/1061-3749.17.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 32.Orr ST, James SA, Prince CB. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. Am J Epidemiol. 2002;156(9):797–802. doi: 10.1093/aje/kwf131. [DOI] [PubMed] [Google Scholar]
- 33.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983:385–96. [PubMed] [Google Scholar]
- 34.Deddens J, Petersen MR, Endahl L. Prevalence proportion ratios: estimation and hypothesis testing. Int J Epidemiol. 1998;27(1):91–5. doi: 10.1093/ije/27.1.91. [DOI] [PubMed] [Google Scholar]
- 35.Barros A, Hirakata V. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21–33. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stone CJ, Koo C-Y. Additive splines in statistics. Proc Stat Comp Sect Am Statist Assoc. 1985;27:45–8. [Google Scholar]
- 37.Harrell F. SAS Macros for Assisting with Survival and Risk Analysis, and Some SAS Procedures Useful for Multivariable Modeling. 2003 [updated January 31, 2003; cited 2014 May 20, 2012]. Available from: http://biostat.mc.vanderbilt.edu/wiki/Main/SasMacros.
- 38.Ko JY, Farr SL, Dietz PM, Robbins CL. Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005–2009. J Womens Health. 2012;21(8):830–6. doi: 10.1089/jwh.2011.3466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohen S, Janicki-Deverts D. Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 20091. J Appl Soc Psychol. 2012;42(6):1320–34. [Google Scholar]
- 40.Holzman C, Eyster J, Tiedje L, Roman L, Seagull E, Rahbar M. A life course perspective on depressive symptoms in mid-pregnancy. Matern Child Health J. 2006;10(2):127–38. doi: 10.1007/s10995-005-0044-0. [DOI] [PubMed] [Google Scholar]
- 41.Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal stress and preterm birth. Am J Epidemiol. 2003;157(1):14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- 42.Collins JW, Jr, David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am J Public Health. 2004;94(12):2132–8. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Collins JW, Jr, David RJ, Symons R, Handler A, Wall SN, Dwyer L. Low-income African-American mothers’ perception of exposure to racial discrimination and infant birth weight. Epidemiology. 2000;11(3):337–9. doi: 10.1097/00001648-200005000-00019. [DOI] [PubMed] [Google Scholar]
- 44.Dailey DE. Social stressors and strengths as predictors of infant birth weight in low-income African American women. Nurs Res. 2009;58(5):340–7. doi: 10.1097/NNR.0b013e3181ac1599. [DOI] [PubMed] [Google Scholar]
- 45.Korte JE. Psychosocial stress and its relationship to weight for gestational age and gestational age at delivery [doctoral dissertation] Chapel Hill, North Carolina: University of North Carolina at Chapel Hill; 1999. Dissertation Abstracts International. 1999. [Google Scholar]
- 46.Jackson FM, Phillips MT, Hogue CJR, Curry-Owens TY. Examining the burdens of gendered racism: Implications for pregnancy outcomes among college-educated African American women. Matern Child Health J. 2001;5(2):95–107. doi: 10.1023/a:1011349115711. [DOI] [PubMed] [Google Scholar]
- 47.Jackson FM, Rowley DL, Owens TC. Contextualized stress, global stress, and depression in well-educated, pregnant, African-American women. Womens Health Issues. 2012;22(3):e329–e36. doi: 10.1016/j.whi.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 48.Mackenzie SG, Lippman A. An investigation of report bias in a case-control study of pregnancy outcome. Am J Epidemiol. 1989;129(1):65–75. doi: 10.1093/oxfordjournals.aje.a115125. [DOI] [PubMed] [Google Scholar]
- 49.Klemetti A, Saxen L. Prospective versus retrospective approach in the search for environmental causes of malformations. Am J Public Health Nations Health. 1967;57(12):2071–5. doi: 10.2105/ajph.57.12.2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zierler S, Rothman KJ. Congenital heart disease in relation to maternal use of Bendectin and other drugs in early pregnancy. N Engl J Med. 1985;313(6):347–52. doi: 10.1056/NEJM198508083130603. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.