Abstract
Background
Recent evidence suggests that amblyopia results in fixation instability and atypical saccades. Reading is a vision-reliant ability that requires sequential eye movements, including forward and regressive saccades. This study investigated reading and associated eye movements in school-age amblyopic children.
Methods
Amblyopic children with strabismus and/or anisometropia (n = 29) were compared to nonamblyopic children treated for strabismus (n = 23) and normal control children (n = 21). While fitted with the ReadAlyzer, an eye movement recording system, children silently read a grade-level paragraph of text during binocular viewing. Reading rate, number of forward and regressive saccades per 100 words, and fixation duration were determined. Comprehension was evaluated with a 10-item quiz; only data from children with at least 80% correct responses were included.
Results
Amblyopic children read more slowly and had more saccades compared with nonamblyopic children with treated strabismus and normal controls. Fixation duration did not differ significantly for amblyopic children versus normal controls. Treated strabismic children without amblyopia did not differ significantly from normal controls on any reading measure. Amblyopic eye visual acuity was not correlated with any reading measure.
Conclusions
Amblyopia was associated with slower reading in school-age children. Treatment for monocular amblyopia visual acuity impairment could improve reading speed and efficiency.
A growing body of evidence indicates that amblyopia is associated with impaired oculomotor function, including fixation instability1–3 and abnormal saccade initiation and execution.4,5 Deficits in oculomotor function in children with amblyopia are likely to adversely affect abilities that rely heavily on eye movements, including reading. Reading consists of a series of saccades that allow the eyes to move forward and backward (regression) through lines of text. Fixations, or pauses, also occur during reading as decoding of phonemes occurs. Studies of eye movements in normally sighted6 and visually impaired7,8 adults have reported an association between increased fixation instability and slower reading.
Previous studies of binocular reading in amblyopia have reported slower reading in adults and school-age children compared with normal controls.9–11 However, none of these studies used natural reading conditions; participants were required to orally read short sentences or to silently read paragraphs on a large, distant screen. Only two of the three studies assessed eye movements and the results were inconsistent despite being conducted by the same research group; one reported more regressive saccades and longer fixations than controls,9 but the other reported more forward saccades than controls.10 Another limitation of earlier studies9–11 is that only patients with both strabismus and amblyopia were enrolled, making it impossible to address whether the reading impairment was a consequence of the strabismus, amblyopia, or both. In the present study subjects read a grade-appropriate paragraph of text silently under natural conditions of binocular viewing and at the child’s habitual reading distance. An eye movement recording system was used to examine whether reading deficits previously found in strabismic amblyopia are due to a history of strabismus or current amblyopia. We compared quantitative measures of reading, including reading rate, number of forward and regressive saccades, and fixation duration for amblyopic children, nonamblyopic children treated for strabismus, and normal control children. We predicted that amblyopic children would be slower at reading and would produce more saccades compared with the other groups.
Methods
The research protocol was approved by the Institutional Review Board of the University of Texas Southwestern Medical Center and conformed to the requirements of the US Health Insurance Portability and Privacy Act of 1996. Informed consent was obtained from a parent or legal guardian prior to testing and after explanation of the nature and possible consequences of the study.
Nonamblyopic and amblyopic school-age children treated for strabismus and/or anisometropia were diagnosed and referred to the Retina Foundation of the Southwest by 18 pediatric ophthalmologists in the Dallas-Fort Worth area. Based on medical records, children were categorized into two groups: amblyopia or treated strabismus without amblyopia. Amblyopia was defined as an interocular difference in visual acuity of ≥0.2 units of logarithm of the minimum angle of resolution (logMAR), best-corrected visual acuity in the nonpreferred eye of ≥0.2 logMAR (≥20/32), and best-corrected visual acuity in the preferred eye of ≤0.1 logMAR (≤20/25). All strabismic children were initially diagnosed with esotropia but had been aligned surgically and/or by spectacle correction within 4Δ of orthotropia at near at the time of the reading test. Treated strabismic children were studied because (1) they are more typical of US school-age children with a history of strabismus, and (2) we wanted to ensure that both eyes were working together—misalignment >4Δ–6Δ disrupts binocularity,12 and tracking reliability may be affected. Children with combined mechanism amblyopia (strabismus + anisometropia) were categorized as strabismic. A group of age-similar, normal control children was also enrolled. These subjects had no history of vision disorders, normal visual acuity, and normal Randot stereoacuity. None of the children were born preterm (<32 weeks’ postmenstrual age) or had coexisting ocular or systemic disease, congenital infections/malformations, or developmental delay. None of the children were dyslexic or enrolled in school reading intervention programs. English was the primary language for all children.
Prior to reading, monocular best-corrected visual acuity was obtained for each eye using the e-ETDRS system.13,14 Reading was assessed during binocular viewing using the ReadAlyzer (Compevo AB, Stockholm, Sweden), an infrared eye movement recording system mounted in goggles worn over the child’s habitual spectacle correction. The child sat eye level at a comfortable, habitual reading distance (35–40 cm) and was required to silently read paragraphs of text from a booklet. The first paragraph was at grade-level 1 and served as a practice run, allowing the tester to determine whether the goggles were tracking properly. If there was a problem with the position of the goggles or reflections from the child’s glasses, the goggles were adjusted before proceeding with the test. Once the grade-level 1 pretest was completed, the child was tested with a paragraph at the last grade-level completed. Each paragraph averaged 12 lines and 100 words. After reading the paragraph, the child was asked 10 yes-or-no comprehension questions. Recordings were considered acceptable for analyses if comprehension was ≥80% and tracking reliability was ≥70%. Tracking reliability may be lowered by ≥5% artifact time, excessive blinking, too much head movement, and occlusion of one infrared sensor by glasses frames. Outcome measures obtained from the recordings were reading rate (words per minute), number of forward saccades (per 100 words), number of regressive saccades (per 100 words), and mean fixation duration (seconds).
Statistical Analysis
Statistical significance of differences among groups (amblyopia, treated strabismus without amblyopia, normal control) in reading rate, number of forward saccades, number of regressive saccades, and fixation duration were evaluated using one-way analysis of variance (ANOVA). Significant ANOVAs were followed with post hoc Bonferroni pairwise group comparisons. Kruskal-Wallis ANOVA15 was used if the data were not normally distributed, followed by post hoc Mann Whitney U tests.16 When normality is violated, these tests are commonly used nonparametric alternatives to a one-way ANOVA and Bonferroni t tests for pairwise group comparisons, respectively. Partial correlations controlling for last grade completed were conducted to determine relationships of nonpreferred eye best-corrected visual acuity with each reading measure for amblyopic children.
Results
A total of 73 children met the comprehension and tracking reliability criteria; 29 amblyopia (15 males; mean age with standard deviation [SD], 9.4 ± 1.2 years; age range, 8.0–12.4 years), 23 treated strabismus without amblyopia (7 males; mean age, 9.8 ± 1.4 years; range, 8.2–12.3 years), and 21 normal controls (11 males; mean age, 10.1 ± 1.4 years; range, 8.1–12.5 years). Four children (1 normal control, 2 with amblyopia, 1 with treated strabismus without amblyopia) were excluded in the analysis due to scoring below 80% comprehension, and 5 children were excluded due to <70% tracking reliability. Low reliability was due to head movement and glasses (occlusion of infrared tracker, bifocals).
No sex differences in reading measures were found for any group (P values, 0.18–0.99). Groups did not differ in last grade completed (H2,73 = 1.74, P = 0.42) or comprehension (H2,73 = 3.42, P = 0.18). Descriptive statistics for amblyopic children, strabismic children without amblyopia, and normal controls for last grade completed, comprehension, and nonpreferred and preferred eye visual acuity are provided in Table 1.
Table 1.
Last grade completed, comprehension, and best-corrected visual acuity for amblyopic children, treated strabismic children without amblyopia and normal control children
| Last grade completed | Comprehension (%) | Nonpreferred eye BCVA, logMAR a | Preferred eye BCVA, logMARa | |||||
|---|---|---|---|---|---|---|---|---|
| Group | Mean ± SD | Range | Mean ± SD | Range | Mean ± SD | Range | Mean ± SD | Range |
| Amblyopia | 2.8 ± 1.1 | 1–6 | 92 ± 7 | 80–100 | 0.3 ± 0.1 (20/40) | 0.2 to 0.6 | 0.0 ± 0.1 (20/20) | −0.1 to 0.1 |
| Strabismus without amblyopiab | 3.0 ± 1.6 | 1–6 | 90 ± 7 | 80–100 | 0.0 ± 0.1 (20/20) | −0.1 to 0.2 | 0.0 ± 0.1 (20/20) | −0.1 to 0.1 |
| Normal control | 3.1 ± 1.5 | 1–6 | 93 ± 7 | 80–100 | −0.1 ± 0.1 (20/16) | −0.1 to 0.1 | −0.1 ± 0.1 (20/16) | −0.1 to 0.1 |
BCVA, best-corrected visual acuity; LogMAR, logarithm of the minimum angle of resolution; SD, standard deviation.
For strabismic children without amblyopia, either the previously amblyopic eye or the right eye (if the child was never amblyopic) is listed for nonpreferred eye visual acuity. For normal control children, the right eye is listed for nonpreferred eye visual acuity.
In children treated strabismus without amblyopia, no differences were found on any reading measure between children who were never amblyopic (n = 8) and children who were previously treated for amblyopia (n = 15); P values ranged from 0.54 to 0.84).
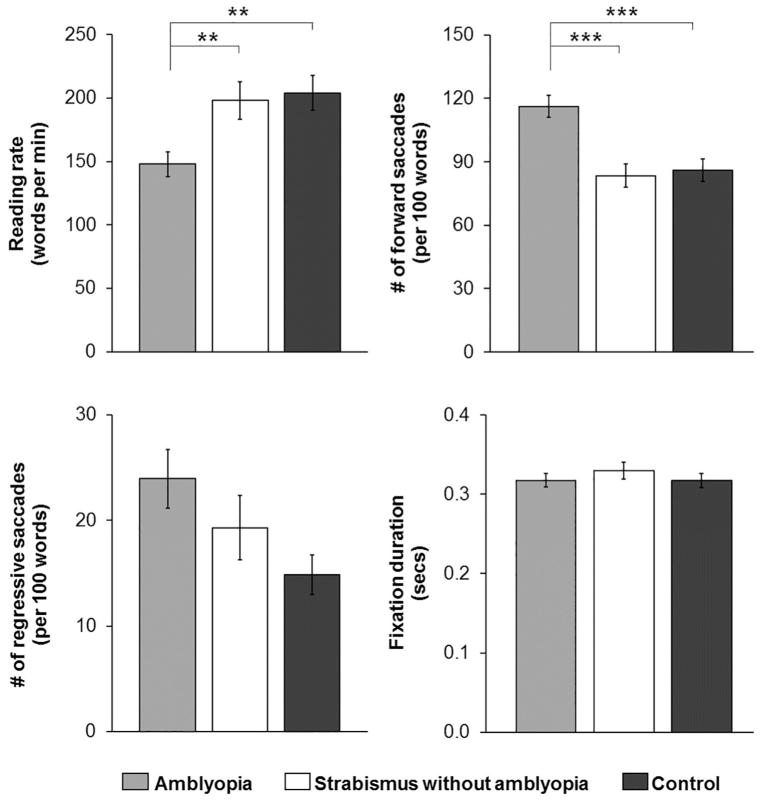
Reading rate, number of forward saccades, number of regressive saccades, and fixation duration for each group of children are summarized in Figure 1. Reading rate was significantly different between groups (F2,70 = 6.58, P = 0.002). Amblyopic children read significantly more slowly (mean, 148 ± 52 words/minute) than strabismic children without amblyopia (mean, 198 ± 71 words/minute; P = 0.004), and normal control children (mean, 204 ± 62 words/minute; P = 0.002). Strabismic children without amblyopia and normal control children did not differ in reading rate (P = 0.76).
FIG 1.
Bar graphs depicting group means for reading rate, number of forward saccades, number of regressive saccades, and fixation duration for amblyopic children (light gray bars), treated strabismic (or combined mechanism) children without amblyopia (white bars), and normal control children (dark gray bars). Amblyopic children were significantly slower at reading and produced more forward saccades compared with treated strabismic children without amblyopia and normal control children. Error bars represent ± standard error of the mean (SEM). *P < 0.05, **P < 0.01, *** P < 0.001.
Similarly, the number of forward saccades differed significantly between groups (F2,70 = 12.38, P < 0.001). Amblyopic children made significantly more forward saccades (mean, 116 ± 28 forward saccades/100 words) compared with strabismic children without amblyopia (mean, 84 ± 27 forward saccades/100 words; P < 0.001) and normal control children (mean, 86 ± 25 forward saccades/100 words; P < 0.001). Number of forward saccades did not differ significantly between strabismic children without amblyopia and normal control children (P = 0.75).
Number of regressive saccades did not differ significantly between groups (mean, 24 ± 15 regressive saccades/100 words for amblyopic children, 19 ± 15 regressive saccades/100 words for strabismic children without amblyopia, 15 ± 9 regressive saccades/100 words for normal control children; F2,70 = 2.85, P = 0.064). Mean fixation duration did not differ significantly between groups (amblyopic children, 0.32 ± 0.05 seconds; strabismic children without amblyopia, 0.33 ± 0.05 seconds; normal controls, 0.32 ± 0.04; H2,73 = 0.86, P = 0.65).
Amblyopic eye visual acuity was not significantly correlated with reading rate (r = 0.17; P = 0.39; 95% CI, −0.21 to 0.51), number of forward saccades (r = −0.20; P = 0.32; 95% CI, −0.53 to 0.18), number of regressive saccades (r = −0.01; P = 0.95; 95% CI, −0.38 to 0.36), or fixation duration (r = −0.15; P = 0.45; 95% CI, −0.49 to 0.23) in amblyopic children.
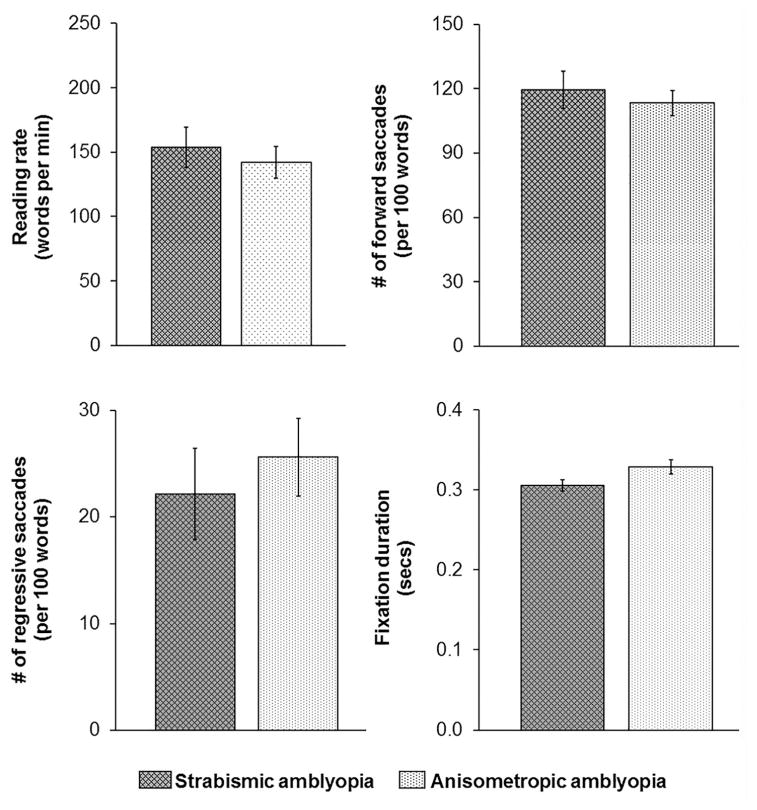
In secondary analyses, we further divided the amblyopic group into subtypes based on a diagnosis of strabismic or combined mechanism amblyopia (n = 14) and anisometropic amblyopia (n = 15) to determine whether groups differed in reading measures. Both groups were comparable in last grade completed (P = 0.50), amblyopic eye visual acuity (P = 0.88), and comprehension (P = 0.25). Independent t tests revealed that reading rate, number of forward saccades, number of regressive saccades, and fixation duration did not differ significantly between groups (P = 0.19–0.57 for all comparisons; Figure 2).
FIG 2.
Bar graphs depicting group means for reading rate, number of forward saccades, number of regressive saccades, and fixation duration for children with strabismic (or combined mechanism) amblyopia (diamond gray bars) and anisometropic amblyopia (dotted white bars). There were no group differences for any reading measure. Error bars represent SEM.
Discussion
We report for the first time that amblyopia, not strabismus, is the key factor in poorer reading in school-age children with amblyopia. The amblyopic children in our study were slower at binocular silent reading compared with treated strabismic children without amblyopia and normal control children, consistent with previous studies that reported slower reading in children and adults with strabismic amblyopia.9–11 However, previous studies did not emulate natural reading conditions that the child would normally encounter in school, that is, binocular silent reading of grade-appropriate paragraphs at habitual reading distance. Lastly, these studies evaluated subjects who had both amblyopia and strabismus and therefore were unable to evaluate the effect of strabismus alone on reading or the effect of anisometropic amblyopia on reading. Our comparison among these diagnostic groups allowed us to verify that reading rate did not differ based on whether amblyopia was due to strabismus or anisometropia and further supports our conclusion that slower reading is a consequence of amblyopia and not of strabismus.
Slower reading in amblyopic children may result from oculomotor dysfunction that accompanies amblyopia, as evidenced by our finding of an increase in the number of forward saccades. This finding is consistent with prior reports of more saccades during reading in adults with strabismic amblyopia than in normal controls.10 Similar increases in the number of saccades have been observed with simulated small central scotomas17; therefore, the ocular motor changes observed in the current study may be the result of a monofixation scotoma associated with mild esotropic amblyopia.18,19 Small central scotomas reduce the visual span, resulting in poor saccadic accuracy and increased number of saccades during binocular reading.20
Alternatively, it is possible that slower reading is instead a consequence of the visual acuity deficit, and the oculomotor deficit (ie, increased forward saccades) is secondary to the visual acuity deficit. A potential indirect effect of the visual acuity deficit in amblyopia is fixation instability. Fixation instability increases with the severity of amblyopia3 and is associated with slower reading in adults with macular disease.7,8,20 We did not directly assess fixation instability in the current study. Yet, at least within the range of moderate amblyopia in our study (0.2–0.6 logMAR [20/32 to 20/80] best-corrected visual acuity), there was no relationship between any reading measure and severity of amblyopia. Thus, the presence, not severity, of amblyopia was sufficient to cause slower reading in our patients. Because the range of amblyopia was moderate, our study may not have been sufficiently powered to make any statement regarding the relationship between the reading deficit and severity of amblyopia. Future studies should include a larger range of visual acuity to further investigate this relationship.
It is important to note that our finding of impaired reading in amblyopic children is unlikely to be due to comprehension difficulties. Only data from children who scored 80% or higher on the comprehension questions were included in the analyses. Second, children with dyslexia and those enrolled in school reading intervention programs were not eligible for the current study. Third, previous studies have shown that comprehension difficulties are associated with increases in fixation duration and regressive saccades.21 Consistent with good comprehension among all groups of children in the current study, there were no group differences in fixation duration or regressive saccades. The lack of group differences on these measures contrasts with one previous report of adults with strabismic amblyopia who had more regressive saccades and longer fixation durations during reading compared with normal controls.9 This inconsistency may be attributed to differences between the previous study and the current study, including reading conditions (paragraphs of text projected on a screen at 1.2 m versus printed paragraphs in a booklet at the habitual reading distance of about 40 cm), and differences in ocular alignment at the time of testing (most in the previous study were exotropic at the time of testing, whereas all treated strabismic patients in the current study had a history of esotropia but were aligned within 4Δ of orthotropia at the time of testing). Further, our strabismic children included those with combined mechanism; we were unable to assess combined mechanism and strabismus only separately due to small sample sizes. Finally, we included only those with esotropia, and children with other forms of strabismus (eg, exotropia) may perform differently on this reading test. Future studies should investigate reading in subtypes of strabismus.
Under natural, binocular silent reading conditions, school-age amblyopic children read slowly. Slow reading in amblyopic children appears to be a consequence of oculomotor dysfunction. Reading is a vision-reliant ability that affords many benefits, including promoting imagination and learning, and is fundamental to academic achievement. Slow reading can be detrimental to academic performance and learning. Parents and educators of amblyopic children may be unaware that a child’s reading may be affected by amblyopia because the child may have 20/20 vision when tested binocularly. Currently, academic accommodations for visually impaired children are limited to those with bilateral visual impairment. In addition to treatment for the monocular visual acuity impairment, it is important to provide amblyopic children with proper academic accommodations. Possible accommodations include more time to complete tests and enrollment in speed reading classes.
Acknowledgments
Supported by the Knights Templar Eye Foundation (16-2015-CS), Fight for Sight (PD15002), the National Eye Institute (EY02313), the ExxonMobil Community Summer Jobs Program.
The authors thank Faye C. Briggs for generously donating funds to purchase the ReadAlyzer, Kenneth Ciuffreda and Preethi Thiagarajan for loaning a ReadAlyzer to us for training and pilot work, and Kirby Mateja and John F Gilmore III for collecting pilot data as ExxonMobil Community Summer Jobs Program interns.
Footnotes
Presented at the 41st Annual Meeting of the American Association for Pediatric Ophthalmology and Strabismus, New Orleans, Louisiana, March 25–29, 2015.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Birch EE, Subramanian V, Weakley DR. Fixation instability in anisometropic children with reduced stereopsis. J AAPOS. 2013;17:287–90. doi: 10.1016/j.jaapos.2013.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.González EG, Wong AMF, Niechwiej-Szwedo E, Tarita-Nistor L, Steinbach MJ. Eye position stability in amblyopia and in normal binocular vision. Invest Ophthalmol Vis Sci. 2012;53:5386–94. doi: 10.1167/iovs.12-9941. [DOI] [PubMed] [Google Scholar]
- 3.Subramanian V, Jost RM, Birch EE. A quantitative study of fixation stability in amblyopia. Invest Ophthalmol Vis Sci. 2013;54:1998–2003. doi: 10.1167/iovs.12-11054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Niechwiej-Szwedo E, Chandrakumar M, Goltz HC, Wong AMF. Effects of strabismic amblyopia and strabismus without amblyopia on visuomotor behavior, I: saccadic eye movements. Invest Ophthalmol Vis Sci. 2012;53:7458–68. doi: 10.1167/iovs.12-10550. [DOI] [PubMed] [Google Scholar]
- 5.Niechwiej-Szwedo E, Goltz HC, Chandrakumar M, Hirji ZA, Wong AMF. Effects of anisometropic amblyopia on visuomotor behavior, I: saccadic eye movements. Invest Ophthalmol Vis Sci. 2010;51:6348–54. doi: 10.1167/iovs.10-5882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Falkenberg HK, Rubin GS, Bex PJ. Acuity, crowding, reading and fixation stability. Vision Res. 2007;47:126–35. doi: 10.1016/j.visres.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 7.Amore FM, Fasciani R, Silvestri V, et al. Relationship between fixation stability measured with MP-1 and reading performance. Ophthalmic Physiol Opt. 2013;33:611–17. doi: 10.1111/opo.12048. [DOI] [PubMed] [Google Scholar]
- 8.Crossland MD, Culham LE, Rubin GS. Fixation stability and reading speed in patients with newly developed macular disease. Ophthalmic Physiol Opt. 2004;24:327–33. doi: 10.1111/j.1475-1313.2004.00213.x. [DOI] [PubMed] [Google Scholar]
- 9.Kanonidou E, Proudlock F, Gottlob I. Reading strategies in mild to moderate strabismic amblyopia: an eye movement investigation. Invest Ophthalmol Vis Sci. 2010;51:3502–8. doi: 10.1167/iovs.09-4236. [DOI] [PubMed] [Google Scholar]
- 10.Kanonidou E, Gottlob I, Proudlock FA. The effect of font size on reading performance in strabismic amblyopia: an eye movement investigation. Invest Ophthalmol Vis Sci. 2014;55:451–9. doi: 10.1167/iovs.13-13257. [DOI] [PubMed] [Google Scholar]
- 11.Stifter E, Burggasser G, Hirmann E, Thaler A, Radner W. Monocular and binocular reading performance in children with microstrabismic amblyopia. Br J Ophthalmol. 2005;89:1324–9. doi: 10.1136/bjo.2005.066688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Braddick O. Binocularity in infancy. Eye. 1996;10:182–8. doi: 10.1038/eye.1996.45. [DOI] [PubMed] [Google Scholar]
- 13.Beck R, Moke P, Turpin A, et al. A computerized method of visual acuity testing: Adaptation of the early treatment of diabetic retinopathy study testing protocol. Am J Ophthalmol. 2003;135:194–205. doi: 10.1016/s0002-9394(02)01825-1. [DOI] [PubMed] [Google Scholar]
- 14.Cotter SA, Chu RH, Chandler DL, et al. Reliability of the electronic early treatment diabetic retinopathy study testing protocol in children 7 to <13 years old. Am J Ophthalmol. 2003;136:655–61. doi: 10.1016/s0002-9394(03)00388-x. [DOI] [PubMed] [Google Scholar]
- 15.Kruskal W, Wallis W. Use of ranks in one-criterion variance analysis. J Am Stat Assoc. 1952;47:583–621. [Google Scholar]
- 16.Mann H, Whitney D. On a test of whether one of two random variables is stochastically larger than the other. Ann Math Stat. 1947;18:50–60. [Google Scholar]
- 17.Fine EM, Rubin GS. The effects of simulated cataract on reading with normal vision and simulated central scotoma. Vision Res. 1999;39:4274–85. doi: 10.1016/s0042-6989(99)00132-7. [DOI] [PubMed] [Google Scholar]
- 18.Parks MM. The monofixation sundrome. Trans Am Ophthalmol Soc. 1969;67:609–57. [PMC free article] [PubMed] [Google Scholar]
- 19.Tychsen L. Can ophthalmologists repair the brain in infantile esotropia? Early surgery, stereopsis, monofixation syndrome, and the legacy of Marshall Parks. J AAPOS. 2005;9:510–21. doi: 10.1016/j.jaapos.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 20.McMahon TT, Hansen M, Viana M. Fixation characteristics in macular disease: relationship between saccadic frequency, sequencing, and reading rate. Invest Ophthalmol Vis Sci. 1991;32:567–74. [PubMed] [Google Scholar]
- 21.Underwood G, Hubbard A, Wilkinson H. Eye fixations predict reading comprehension: the relationships between reading skill, reading speed, and visual inspection. Lang Speech. 1990;33:69–81. doi: 10.1177/002383099003300105. [DOI] [PubMed] [Google Scholar]