Abstract
Purpose
To study the effect of maternal psychiatric disorders (depression, anxiety disorder, bipolar disease, schizophrenia, unspecified psychiatric disorder, and comorbid conditions) and odds of preterm birth.
Methods
The Consortium on Safe Labor (2002-2008), an observational cohort with 12 centers from across the U.S. included 223,394 singleton pregnancies with clinical data obtained from electronic medical records and maternal diagnoses of psychiatric disorders from maternal discharge summaries. Length of gestation was based on the best clinical estimate and categorized as birth <39, <37, <34 and <28 weeks’ gestation. The adjusted odds ratios (ORs) with 95% confidence intervals of birth were estimated by logistic regression with generalized estimating equations.
Results
Any maternal psychiatric disorder was associated with odds of birth <39 weeks’ gestation (OR=1.32, 95% confidence interval 1.28-1.37), <37 weeks’ gestation (OR=1.45, 1.38-1.52), <34 weeks’ gestation (OR=1.47, 1.35-1.59) and <28 weeks’ gestation (OR=1.57, 1.36-1.82). Specifically, odds of birth <37 weeks’ gestation were associated with maternal depression (OR=1.31, 1.23-1.40), anxiety disorder (OR=1.68, 1.41-2.01), depression with anxiety disorder (OR=2.31, 1.93-2.78), bipolar disease (OR=1.54, 1.22-1.94), bipolar disease with depression and=or anxiety disorder (OR=1.70, 1.30-2.22) and unspecified psychiatric disorder (OR=1.52, 1.41-1.64).
Conclusions
Maternal psychiatric disorders, especially comorbid psychiatric conditions, were associated with increased likelihood of preterm birth.
Keywords: Preterm Birth, Psychiatric Diagnosis, Depression, Anxiety, Bipolar Disorder, Schizophrenia
Introduction
Maternal psychiatric disorders are common among women of childbearing age [1-3]. During pregnancy, up to 10% and 13% have depression and anxiety disorder, respectively, while 3% have bipolar disorder and <1% have psychotic disorders [4,5]. Women with untreated psychiatric disorders are less likely to access care, including prenatal care, and may be more prone to substance abuse before and during pregnancy [6]. Treatment of maternal psychiatric disorders during pregnancy requires consideration, including the severity of the maternal condition, the medication to be used and the potential effects of the medication on the mother and the fetus [7,8]. While pregnancy is considered a vulnerable period for psychiatric disorders, most of the focus in the literature is on the postpartum period [5,9,10].
In 2012, 11.5% of infants in the U.S. were born preterm at <37 weeks’ gestation [11]. Preterm neonates are at higher risk of morbidity and mortality as well as increased risk for psychiatric disorders later in life [12,13]. Pregnant women with any psychiatric disorder have a shorter gestational length [14] and are at increased risk for preterm birth [15-18]. One previous study has shown that the associations between preterm birth and maternal psychiatric morbidity seemed to be independent of familial relationships and measured covariates [19].
However, data on specific psychiatric disorders and preterm birth risk is less consistent. The risk of preterm birth has been associated with maternal depression or antidepressant use during pregnancy in some [20-24], but not all studies [25-27]. A recent study suggests that underlying psychiatric disorders might confound the association between antidepressant use and preterm birth, as women who received selective serotonin reuptake inhibitors had lower risk of preterm birth than women with psychiatric disorders without exposure to these medications [28]. Findings are somewhat less inconsistent between maternal anxiety disorders and preterm birth risk [29], whereas maternal schizophrenia and bipolar disease are more consistently associated with preterm births [30,31]. The effect of comorbid maternal psychiatric disorders is seldom studied.
In our study from a large, contemporary pregnant U.S. population, we investigated the effect of a full range of maternal psychiatric disorders, including comorbid psychiatric conditions, on odds of preterm birth.
Methods
The Consortium on Safe Labor (2002-2008, with 87% of births occurring 2005-2007) was an observational nationwide U.S. cohort including 12 clinical centers with 19 hospitals, chosen due to their geographic distribution and the availability of electronic medical records [32]. The study included 228,668 women with 233,844 newborns (including multiples) [32]. We excluded 230 deliveries due to errors of identification and all multi-fetal pregnancies (N=5,044), rendering a final sample size of 203,999 women with 223,394 singleton deliveries. Most women (N=185,422; 90.9%) contributed only one pregnancy. Data on maternal demographics, medical, reproductive, and prenatal history, labor and delivery, and postpartum data were collected from the hospital delivery admission electronic medical records, supplemented with electronic maternal discharge summaries in International Classification of Diseases, version 9 (ICD9) codes. The institutional review boards of all participating institutions approved the study. Data linkage, cleaning, recording, and validation have been previously described, with the medical chart review and the electronic data providing good agreement [32].
Exposure data
Data on maternal psychiatric disorders were abstracted from the electronic medical records and supplemented with data from the maternal discharge summaries. Women were considered to have a psychiatric disorder during pregnancy if they had any of the following disorders recorded in the electronic medical record or in the discharge summary:
1. Depression (N=8,354), pregnancies with diagnoses of major depressive disorder (ICD9 codes 296.2 and 296.3) or depressive disorder not elsewhere classified (ICD9 code 311) recorded in the maternal hospital discharge summaries (N=1,437; 17.2%), or pregnancies with history of depression recorded in the electronic medical records (N=4,695; 56.2%), or pregnancies with both indications of depression (N=2,222; 26.6%). No other specific psychiatric disorders recorded in either database.
2. Anxiety (N=689), pregnancies with diagnoses of anxiety state (ICD9 code 300.0) recorded in the maternal hospital discharge summaries. No other specific psychiatric disorders recorded in either database.
3. Bipolar disorder (N=515), pregnancies with diagnoses of bipolar or manic disorder (ICD9 codes 296.0, 296.2, or 296.4 to 296.8) recorded in the maternal hospital discharge summaries. No other specific psychiatric disorders recorded in either database.
4. Depression with anxiety (N=885), pregnancies with both the aforementioned diagnoses of depression and anxiety or pregnancies with diagnoses of dysthymic disorder (ICD9 code 300.4) recorded in the maternal hospital discharge summaries.
5. Bipolar disorder with depression and=or anxiety (N=321), pregnancies with the aforementioned diagnoses of bipolar disorders and with the diagnoses of depression and=or anxiety.
6. Schizophrenia (N=134), women with schizophrenic disorder (ICD-9 code 295) recorded in the maternal hospital discharge summaries with=without any other psychiatric disorders.
7. Unspecified psychiatric disorder (N=5,500), pregnancies with diagnoses of psychiatric disorders affecting the pregnancy (ICD9 code 648.4) in the maternal hospital discharge summaries. No other specific psychiatric disorders were recorded in either database.
Women without these diagnoses were considered to be unexposed (no psychiatric disorder, N=206,996, 92.7%). We also evaluated a composite category ‘any psychiatric disorder’ (N=16,398; 7.3%) to study the overall effect of psychiatric disorders on preterm birth.
Outcome data
Data on gestational age was derived from the electronic medical records and was based on the best obstetrical estimate of gestational length. We explored clinically relevant cut-offs of preterm birth: total preterm births at <37 weeks’ gestation, early preterm births at <34 weeks’ gestation and very early preterm births at <28 weeks’ gestation. We also used a cut-off of <39 weeks’ gestation given the recent recognition that infants born at 37 and 38 weeks have increased neonatal morbidity [33,34]. We also classified the subtype of preterm delivery as spontaneous or indicated using a method previously described by our group [35]. Spontaneous preterm deliveries included women who presented in preterm labor or with premature rupture of the membranes. Indicated preterm deliveries were identified as inductions and prelabor cesareans for fetal, maternal or obstetrical indications.
Statistics
Pregnancy was the unit of analysis in all statistical testing. The demographics of the population were tabulated using contingency tables. Missing categorical data were included in the analyses as their own category. Women with missing continuous data were excluded from the analyses.
We used logistic regression with generalized estimating equations to estimate the odds ratios (ORs) with 95% confidence intervals (CI) of birth at certain gestational week (<39 vs. ≥39 weeks’ gestation, <37 vs. ≥37 weeks’ gestation, <34 vs. ≥34 weeks’ gestation, <28 vs. ≥28 weeks’ gestation) associated with maternal psychiatric disorders. The generalized estimating equations with autoregressive correlation matrix accounted for correlation between repeat pregnancies within a woman. The analyses were adjusted for maternal age, race=ethnicity, prepregnancy body-mass index (kg=m2), insurance and marital status, smoking during pregnancy, maternal substance abuse and alcohol use during pregnancy, parity, other chronic maternal illnesses (diabetes, chronic hypertension, thyroid diseases, asthma, chronic gastrointestinal disorders, chronic cardiovascular diseases and chronic renal diseases) and clinical site. We performed additional analyses not adjusting for maternal substance abuse and alcohol use during pregnancy, as these factors can be potential mediators in the pathway from maternal psychiatric disorder to preterm birth. As the results were very similar to the fully adjusted analyses, we only present the results of the full models.
We also studied the effect of maternal psychiatric disorders on spontaneous and indicated preterm births by stratifying the data into three groups: spontaneous births, indicated births and births with prelabor cesarean delivery. For the sensitivity analyses, we only included women with psychiatric disorders identified via the ICD9 discharge diagnosis codes. All analyses were performed with SAS 9.3 (SAS Institute Inc., Cary, North Carolina, US).
Results
Altogether 16,398 of pregnancies (7.3%) were affected by one or more maternal psychiatric disorder. Prevalence of individual disorders among pregnant women was: 3.7% depression, 0.3% anxiety, 0.2% bipolar disorder, 0.1% bipolar disorder with depression and=or anxiety, 0.1% schizophrenia, and 2.5% unspecified. Women with psychiatric disorders were somewhat younger and heavier, and were more often non-Hispanic white and not married. They were less likely to have private insurance or to be nulliparous, but were more likely to have a chronic disease during pregnancy and to smoke, use alcohol or illicit drugs during pregnancy (Table 1).
Table 1.
The demographic characteristics of pregnancies with and without maternal psychiatric disorders, the Consortium on Safe Labor (2002-2008).
| Demographics | No psychiatric disorders (N=206,996; 92.7%) |
Any psychiatric disorder (N=16,398; 7.3%) |
Depression (N=8,354; 3.7%) |
Anxiety (N=689; 0.3%) |
Bipolar disorder (N=515; 0.2%) |
Depression with anxiety (N=885; 0.4%) |
Bipolar disorder with depression and/or anxiety (N=321; 0.1%) |
Unspecified psychiatric disorder (N=5,500; 2.5%) |
Schizophrenia (N=134; 0.1%) |
|---|---|---|---|---|---|---|---|---|---|
|
Maternal age
in years |
|||||||||
| <20 | 18,945 (9.2) | 1,751 (10.7) | 796 (9.5) | 39 (5.7) | 91 (17.7) | 47 (5.3) | 37 (11.5) | 727 (13.2) | 14 (10.5) |
| ≥20 but <25 | 51,930 (25.1) | 4,659 (28.4) | 1,993 (23.9) | 156 (22.6) | 154 (29.9) | 200 (22.6) | 115 (35.8) | 2,009 (36.5) | 32 (23.8) |
| ≥25 but <30 | 57,759 (27.9) | 4,455 (27.2) | 2,384 (28.5) | 208 (30.2) | 143 (27.8) | 259 (29.3) | 80 (24.9) | 1,357 (24.7) | 24 (17.9) |
| ≥30 but <35 | 46,924 (22.7) | 3,226 (19.7) | 1,900 (22.7) | 162 (23.5) | 77 (15.0) | 221 (25.0) | 61 (19.0) | 776 (14.1) | 29 (21.6) |
| >35 | 31,161 (15.1) | 2,277 (13.9) | 1,260 (15.1) | 123 (17.9) | 50 (9.7) | 153 (17.3) | 28 (8.7) | 628 (11.4) | 35 (26.1) |
| Unknown | 277 (0.1) | 30 (0.2) | 21 (0.3) | 1 (0.3) | 0 | 5 (1.6) | 0 | 3 (1.0) | 0 |
|
Number of
pregnancies |
|||||||||
| 1 | 189,082 (91.3) | 14,917 (91.0) | 7,470 (89.4) | 649 (94.2) | 478 (92.8) | 770 (87.0) | 272 (84.7) | 5,158 (93.8) | 120 (89.6) |
| 2 | 17,073 (8.3) | 1,375 (8.4) | 811 (9.7) | 40 (5.8) | 35 (6.8) | 104 (11.8) | 46 (14.3) | 326 (5.9) | 13 (9.7) |
| ≥3 | 841 (0.4) | 106 (0.6) | 73 (0.9) | 0 | 2 (0.4) | 11 (1.2) | 3 (0.9) | 16 (0.3) | 1 (0.8) |
| Race/ethnicity | |||||||||
| Non-Hispanic white |
99,944 (48.3) | 10,504 (64.1) | 5,408 (64.7) | 533 (77.4) | 366 (71.1) | 692 (78.2) | 218 (67.9) | 3,255 (59.2) | 32 (23.9) |
| Non-Hispanic black |
46,790 (22.6) | 3,448 (21.0) | 1,366 (16.4) | 71 (10.3) | 111 (21.6) | 74 (8.4) | 63 (19.6) | 1,680 (30.6) | 83 (61.9) |
| Hispanic | 37,337 (18.0) | 1,702 (10.4) | 1,156 (13.8) | 49 (7.1) | 24 (4.7) | 75 (8.5) | 28 (8.7) | 356 (6.5) | 14 (10.5) |
| Asian/Pacific Islander |
9,091 (4.4) | 116 (0.7) | 59 (0.7) | 11 (1.6) | 5 (1.0) | 3 (0.3) | 1 (0.3) | 35 (0.6) | 2 (1.5) |
| Other | 5,089 (2.5) | 206 (1.3) | 109 (1.3) | 3 (0.4) | 4 (0.8) | 5 (0.6) | 2 (0.6) | 83 (1.5) | 0 |
| Unknown | 8,745 (4.2) | 422 (2.6) | 256 (3.1) | 22 (3.2) | 5 (1.0) | 36 (4.1) | 9 (2.8) | 91 (1.7) | 3 (2.2) |
| Marital status | |||||||||
| Married | 124,563 (60.2) | 6,616 (40.4) | 4,206 (50.4) | 420 (61.0) | 157 (30.5) | 476 (53.8) | 93 (29.0) | 1,239 (22.5) | 25 (18.7) |
| Single | 72,954 (35.2) | 8,504 (51.9) | 3,530 (42.3) | 213 (30.9) | 319 (61.9) | 330 (37.3) | 194 (60.4) | 3,829 (69.6) | 89 (66.4) |
| Other | 2.829 (1.4) | 713 (4.4) | 309 (3.7) | 30 (4.4) | 33 (6.4) | 32 (3.6) | 24 (7.5) | 269 (4.9) | 16 (11.9) |
| Unknown | 6,650 (3.2) | 565 (3.5) | 309 (3.7) | 26 (3.8) | 6 (1.2) | 47 (5.3) | 10 (3.1) | 163 (3.0) | 4 (3.0) |
|
Insurance
status |
|||||||||
| Private | 117,618 (56.8) | 7.296 (44.5) | 4,701 (56.3) | 423 (61.4) | 160 (31.1) | 591 (66.8) | 97 (30.2) | 1,309 (23.8) | 15 (11.2) |
| Public | 63,827 (30.8) | 8,325 (50.8) | 3,323 (39.8) | 231 (33.5) | 332 (64.5) | 281 (31.8) | 210 (65.4) | 3,847 (70.0) | 101 (75.4) |
| Self-pay | 2,405 (1.2) | 258 (1.6) | 116 (1.4) | 4 (0.6) | 1 (0.2) | 1 (0.1) | 6 (1.9) | 127 (2.3) | 3 (2.2) |
| Other | 289 (0.1) | 30 (0.2) | 12 (0.1) | 1 (0.2) | 1 (0.2) | 0 | 3 (0.9) | 10 (0.2) | 3 (2.2) |
| Unknown | 22,857 (11.0) | 489 (3.0) | 202 (2.4) | 30 (4.4) | 21 (4.1) | 12 (1.4) | 5 (1.6) | 207 (3.8) | 12 (9.0) |
|
Pre-pregnancy
body mass index, kg/m2 |
|||||||||
| ≥25 | 81,717 (39.5) | 5,352 (32.6) | 2,689 (32.2) | 233 (33.8) | 143 (27.8) | 251 (28.4) | 91 (28.4) | 1,913 (34.8) | 32 (23.9) |
| ≥25 but <30 | 30,975 (15.0) | 2,501 (15.3) | 1,382 (16.5) | 106 (15.4) | 70 (13.6) | 118 (13.3) | 40 (12.5) | 762 (13.9) | 23 (17.2) |
| ≥30 but <35 | 14,391 (7.0) | 1,381 (8.4) | 792 (9.5) | 45 (6.5) | 49 (9.5) | 61 (6.9) | 22 (6.9) | 401 (7.3) | 11 (8.2) |
| ≥35 | 10,807 (5.2) | 1,345 (8.2) | 814 (9.7) | 43 (6.2) | 45 (8.7) | 55 (6.2) | 30 (9.4) | 345 (6.3) | 13 (9.7) |
| Unknown | 69,106 (33.4) | 5,819 (35.5) | 2,677 (32.0) | 262 (38.0) | 208 (40.4) | 400 (45.2) | 138 (43.0) | 2,079 (37.8) | 55 (41.0) |
|
Nulliparous
Maternal risk factors during pregnancy |
83,685 (40.4) | 5,349 (32.6) | 2,583 (30.9) | 269 (39.0) | 223 (43.3) | 332 (37.5) | 119 (37.1) | 1,781 (32.4) | 42 (31.3) |
| Chronic disease | 5,900 (2.9) | 703 (4.3) | 468 (5.6) | 34 (4.9) | 27 (5.2) | 49 (5.5) | 14 (4.4) | 106 (1.9) | 5 (3.7) |
| Alcohol use | 3,154 (1.5) | 936 (5.7) | 323 (3.9) | 26 (3.8) | 42 (8.2) | 31 (3.5) | 25 (7.8) | 482 (8.9) | 7 (5.2) |
| Smoking | 10,317 (5.0) | 4,614 (28.1) | 1,490 (17.8) | 84 (12.2) | 116 (22.5) | 160 (18.1) | 105 (32.7) | 2,617 (47.6) | 42 (31.3) |
| Illicit drug use | 2,572 (1.2) | 1,592 (9.7) | 489 (5.9) | 28 (4.1) | 63 (12.2) | 39 (4.4) | 56 (17.5) | 890 (16.2) | 27 (20.2) |
|
Gestational age
at birth, weeks |
|||||||||
| ≥39 | 122,468 (59.2) | 8,212 (50.1) | 4,227 (50.6) | 442 (49.9) | 254 (49.3) | 301 (43.7) | 148 (46.1) | 2,787 (50.7) | 53 (39.6) |
| ≥37 but <39 | 61,315 (29.6) | 5,269 (32.1) | 2,826 (33.8) | 288 (32.5) | 165 (32.0) | 234 (34.0) | 102 (31.8) | 1.602 (29.1) | 52 (38.8) |
| ≥34 but <37 | 15,485 (7.5) | 1,878 (11.5) | 899 (10.8) | 88 (9.9) | 53 (10.3) | 88 (12.8) | 47 (14.6) | 685 (12.5) | 18 (13.4) |
| ≥28 but <34 | 5,642 (2.7) | 759 (4.6) | 306 (3.7) | 51 (5.8) | 33 (6.4) | 49 (7.1) | 18 (5.6) | 295 (5.4) | 7 (5.2) |
| <28 | 2,086 (1.0) | 280 (1.7) | 96 (1.2) | 16 (1.8) | 10 (1.9) | 17 (2.5) | 6 (1.9) | 131 (2.4) | 4 (3.0) |
|
Delivery
characteristics |
|||||||||
| Spontaneous labor |
111,171 (53.7) | 9,213 (56.2) | 4.625 (55.4) | 335 (48.6) | 267 (51.8) | 469 (53.0) | 157 (48.9) | 3,289 (59.8) | 71 (53.0) |
| Induced labor | 72,064 (34.8) | 5,089 (31.0) | 2,700 (32.3) | 255 (37.0) | 174 (33.8) | 278 (31.4) | 113 (35.2) | 1,535 (27.9) | 34 (25.4) |
| Prelabor section | 23,761 (11.5) | 2,096 (12.8) | 1,029 (12.3) | 99 (14.4) | 74 (14.4) | 138 (15.6) | 51 (15.9) | 676 (12.3) | 29 (21.6) |
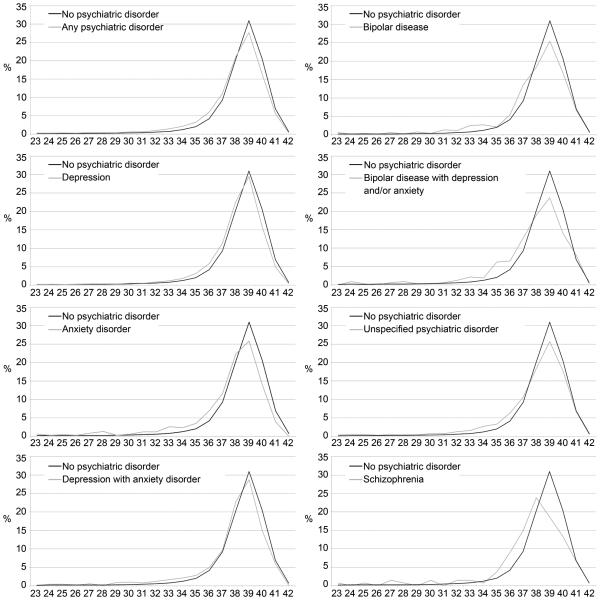
The distribution of births seemed to be shifted towards earlier gestational weeks among all women with psychiatric disorders (Figure 1). Overall, 17.8% and 11.2% of all births were preterm <37 weeks’ gestation among women with and without psychiatric disorders during pregnancy, respectively. Women with anxiety disorders, bipolar disease and schizophrenia had the highest rates of births at <34 weeks’ gestation with 7.6% to 8.2% of births being born early preterm, compared to only 3.7% among women without psychiatric disorders (Table 1 and Figure 1).
Figure 1.
The prevalence of birth at different gestational weeks by maternal psychiatric disorders.
Odds of birth <39 weeks’ gestation were associated with any maternal psychiatric disorder and all specific maternal psychiatric disorders (Table 2). Any maternal psychiatric disorder was associated with an OR 1.45 (95% CI 1.28-1.37) of preterm birth <37 weeks’ gestation (Table 2). When evaluating this association with specific maternal psychiatric disorders, all disorders except schizophrenia were associated with increased odds of preterm birth <37 weeks' gestation. The highest odds of preterm birth were observed among women with depression with anxiety disorder (OR 2.31, 95% CI 1.93-2.78), although the confidence intervals overlapped with those of other psychiatric disorders (Table 2). Similarly, most maternal psychiatric disorders were associated with increased odds of births at <34 and <28 weeks’ gestation (Table 2). Again, women with depression with anxiety disorder had the highest odds of preterm birth <34 weeks (OR 3.06, 95% CI 2.36-3.97) and <28 weeks’ gestation (OR 2.99, 95% CI 1.83-4.90) (Table 2).
Table 2.
The odds of birth at certain gestational age, by maternal psychiatric disorders.
| Exposure | Birth <39 vs. ≥39 weeks’ gestation OR (95% CI) |
Birth <37 vs. ≥37 weeks’ gestation OR (95% CI) |
Birth <34 vs. ≥34 weeks’ gestation OR (95% CI) |
Birth <28 vs. ≥28 weeks’ gestation OR (95% CI) |
|---|---|---|---|---|
| Any psychiatric disorder | 1.32 (1.28-1.37) | 1.45 (1.38-1.52) | 1.47 (1.36-1.59) | 1.57 (1.36-1.82) |
| Depression | 1.32 (1.26-1.38) | 1.31 (1.23-1.40) | 1.18 (1.05-1.31) | 1.18 (0.95-1.47) |
| Anxiety | 1.46 (1.28-1.67) | 1.68 (1.41-2.01) | 2.20 (1.70-2.84) | 2.36 (1.42-3.91) |
| Bipolar disease | 1.40 (1.17-1.67) | 1.54 (1.22-1.94) | 2.15 (1.54-3.00) | 1.90 (1.01-3.60) |
| Depression with anxiety | 1.79 (1.54-2.09) | 2.31 (1.93-2.78) | 3.06 (2.36-3.97) | 2.99 (1.83-4.90) |
| Bipolar disease with depression and/or anxiety |
1.47 (1.17-1.83) | 1.70 (1.30-2.22) | 1.51 (0.99-2.31) | 1.50 (0.66-3.43) |
| Unspecified psychiatric disorder | 1.22 (1.15-1.30) | 1.52 (1.41-1.64) | 1.60 (1.42-1.80) | 1.83 (1.49-2.26) |
| Schizophrenia | 1.57 (1.08-2.27) | 1.15 (0.73-1.80) | 1.09 (0.55-2.16) | 1.33 (0.47-3.76) |
The odds are estimated using logistic regression with generalized estimating equations, adjusting for maternal age, body-mass index (calculated as weight/height2 in kg/m2), insurance status, marital status, smoking during pregnancy, substance abuse and alcohol use during pregnancy, parity, other chronic maternal illnesses and clinical site.
All results were similar when stratifying the data by preterm delivery subtype indicating that psychiatric disorders were associated with an increased risk of both spontaneous and indicated preterm delivery, with some loss of precision due to smaller power (data not shown). Similar results were also obtained when the exposure groups were restricted to women with psychiatric diagnosis data obtained only via the recorded discharge diagnoses (data not shown).
Discussion
In this study from a large contemporary pregnancy cohort from the U.S., we found that all maternal psychiatric disorders were associated with increased odds of delivery <39 weeks’ gestation, including odds of preterm birth <37, <34 and <28 weeks’ gestation. Maternal comorbid psychiatric disorders, especially depression with anxiety seemed to pose the highest risks for shorter gestational length and preterm birth, although the odds ratio estimates overlapped.
Approximately 7% of women in our study were affected by some psychiatric disorder during pregnancy. This prevalence is lower than that of reported in other studies [1-5]. We used electronic medical records to identify maternal psychiatric disorders, and as such, we may be subject to underreporting of psychiatric disorders compared to studies with interview data [36]. Our observed association between psychiatric disorders and preterm birth <37 weeks' gestation was also smaller than that found in other studies [16,18], also supporting the notion of underreporting of psychiatric disorders in our obstetric population. Therefore our results can be considered to be conservative.
We observed that all maternal psychiatric disorders were associated with increased odds of delivery <39 weeks' gestation, which is a novel finding. This association is clinically important given that infants born at 37+0 to 38+7 weeks’ gestation are at higher risk of neonatal morbidity than those born 39+0 weeks’ gestation [33,34]. The Eunice Kennedy Shriver National Institute of Child Health and Human Development now suggests defining term births as 39+0 to 40+6 weeks’ gestation [37]. Children born <37 weeks' gestation have been found to have more psychiatric symptoms and diagnoses later in life [12,13], but it is unclear if such intergenerational effects are also observed with children born at 37+0 to 38+7 weeks’ gestation.
Additionally, we observed that any maternal psychiatric disorder was associated with preterm birth <37, <34 and <28 weeks’ gestation. Anxiety, bipolar disease, depression with anxiety disorder and unspecified psychiatric disorder were statistically significantly associated with preterm birth <37, <34 and <28 weeks’ gestation, whereas depression was significantly only associated preterm birth <37 and <34 weeks’ gestation. Interestingly, maternal schizophrenia was not associated with increased odds of preterm birth <37 weeks’ gestation in our study, but we acknowledge that the numbers in the schizophrenia group are small.
Previous studies have associated maternal depression and=or selective serotonin reuptake inhibitor use to increased risk of preterm birth [20-24], but contradictory findings have also been reported [25-27]. A more recent study found a protective effect between preterm birth and exposure to selective serotonin reuptake inhibitors when exposed women were compared to women with psychiatric diagnoses without medication exposure [28]. In that study, women with psychiatric diagnoses without medication had higher odds of preterm birth when compared to healthy women [28], a finding similar to our study.
A novel finding in our study was the observed association between comorbid maternal psychiatric disorders and preterm birth. Our results indicate that especially anxiety disorders were associated with preterm birth or birth <39 weeks' gestation, which is consistent with the results of a recent meta-analysis of prospective cohort studies [41], and an earlier review [42]. Historically more attention may be given to depression clinically, especially during the postpartum period when suicidality or postpartum psychosis may be a concern. The American College of Obstetricians and Gynecologists has not yet made a firm recommendation to screen for depression or anxiety disorders during or after pregnancy, though depression is common and has been incorporated into the care of high risk women [40]. Although depression and anxiety disorder share some symptoms and may coexist, stress reactions are thought to be higher among women with anxiety disorders [38]. Maternal stress, on the other hand, has been associated with preterm birth via behavioral or inflammation mediated mechanisms [39]. Whether stress reactions explain the observed association between preterm birth and maternal anxiety disorders need further studies.
We observed an association between both spontaneous and indicated preterm delivery and maternal psychiatric disorders. This was most pronounced for earlier gestational ages (<34 and <28 weeks’ gestation). There are several potential mechanisms through which maternal psychiatric disorders may associate with shorter gestational length. Women with psychiatric disorders have been shown to be less likely to access prenatal care and are more likely to smoke or use alcohol or illicit drugs during pregnancy [4-6]. The latter was also observed in our data, although we may be subject to underreporting of substance abuse compared to other studies and interview data [17,36]. However, we assume that the most severe cases of substance abuse are reported in the pregnancy-related medical records and most women are truly non-users. A previous report has shown minimal bias in relation to misclassification of substance abuse when most of the population are truly non-users [43]. Our observed association between maternal psychiatric disorders and preterm birth remained even after adjusting for substance abuse. However, as some women with psychiatric disorders may alleviate their symptoms via substance abuse, the relationship between maternal psychiatric disorders, substance abuse and shorter gestational length may be more complex than our statistical model assumes. This too merits further studies.
Women with psychiatric disorders were also more likely to have other chronic diseases, which could elevate preterm birth risk, but accounting for chronic disease did not change the observed findings. The observed association between increased odds of preterm birth was also not fully explained by increased risk of pregnancy complications such as preeclampsia as the odds of preterm birth were similar in women with maternal psychiatric disorders with spontaneous and indicated preterm birth. There is also evidence that suggests the pharmacological treatment itself for depression may be associated with preterm delivery [44], although this association is confounded by indication in that women with more severe disease are more likely to be treated [28]. Our study did not collect information on psychiatric medication use, and we cannot therefore evaluate the effect of treatment on the odds of preterm birth among women with psychiatric disorders.
Our study was based on a large and contemporary cohort of pregnancies across the U.S., allowing us to capture pregnancies of women from all social class and racial=ethnic groups. In our study the prevalence of maternal psychiatric disorders during pregnancy was relatively low. Our large sample size allowed us to observe an association between increased odds of early birth associated with the understudied maternal disorders of bipolar disease and schizophrenia. We believe our findings are generalizable to the broader population, particularly those whose disease was severe enough to be recorded in their medical record. However, our study is limited to data recorded in the medical record, including the lack of medication data.
In summary, deliveries complicated by maternal psychiatric disorders, particularly when complicated by anxiety disorders, were associated with an increased risk of both spontaneous and indicated preterm delivery. This is most worrisome for earlier gestational ages less than 34 and 28 weeks. These findings have important public health implications given that 7.3% of women in our study had a psychiatric diagnosis recorded in their medical record or discharge summary.
Acknowledgements
Institutions involved in the Consortium include, in alphabetical order: Baystate Medical Center, Springfield, MA; Cedars-Sinai Medical Center Burnes Allen Research Center, Los Angeles, CA; Christiana Care Health System, Newark, DE; Georgetown University Hospital , MedStar Health, Washington, DC; Indiana University Clarian Health, Indianapolis, IN; Intermountain Healthcare and the University of Utah, Salt Lake City, Utah; Maimonides Medical Center, Brooklyn, NY; MetroHealth Medical Center, Cleveland, OH.; Summa Health System, Akron City Hospital, Akron, OH; The EMMES Corporation, Rockville MD (Data Coordinating Center); University of Illinois at Chicago, Chicago, IL; University of Miami, Miami, FL; and University of Texas Health Science Center at Houston, Houston, Texas.
This research was supported by the Intramural Research Program of the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). The Consortium on Safe Labor was funded by the Intramural Research Program of the NICHD, through Contract No. HHSN267200603425C.
Abbreviations
- ICD9
International Classification of Diseases, version 9
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Tuija Männistö, Email: tuija.mannisto@thl.fi, tuija.mannisto@fimnet.fi.
Pauline Mendola, Email: pauline.mendola@nih.gov.
Michele Kiely, Email: Michele.kiely@sph.cuny.edu.
Jennifer O’Loughlin, Email: jennifer.oloughlin@gmail.com.
Emily Werder, Email: ewerder@email.unc.edu.
Zhen Chen, Email: chenzhe@mail.nih.gov.
Deborah B Ehrenthal, Email: ehrenthal@wisc.edu.
References
- [1].Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, et al. Perinatal depression: Prevalence, screening accuracy, and screening outcomes. Evid Rep Technol Assess (Summ) 2005;(119):1–8. doi: 10.1037/e439372005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- [3].Goldstein DJ, Corbin LA, Fung MC. Olanzapine-exposed pregnancies and lactation: Early experience. J Clin Psychopharmacol. 2000;20(4):399–403. doi: 10.1097/00004714-200008000-00002. [DOI] [PubMed] [Google Scholar]
- [4].Andersson L, Sundström-Poromaa I, Bixo M, Wulff M, Bondestam K, Åstrom M. Point prevalence of psychiatric disorders during the second trimester of pregnancy. A population-based study. Am J Obstet Gynecol. 2003;189(1):148–54. doi: 10.1067/mob.2003.336. [DOI] [PubMed] [Google Scholar]
- [5].Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65(7):805–15. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Farr SL, Bish CL. Preconception health among women with frequent mental distress: A population-based study. J Womens Health (Larchmt) 2013;22(2):153–8. doi: 10.1089/jwh.2012.3722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].American College of Obstetricians and Gynecologists (ACOG) ACOG practice bulletin; no 92. Use of psychiatric medications during pregnancy and lactation. Obstet Gynecol. 2008;111(4):1001–20. doi: 10.1097/AOG.0b013e31816fd910. [DOI] [PubMed] [Google Scholar]
- [8].Galbally M, Snellen M, Power J. Antipsychotic drugs in pregnancy: A review of their maternal and fetal effects. Ther Adv Drug Saf. 2014;5(2):100–9. doi: 10.1177/2042098614522682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Eberhard-Gran M, Eskild A, Tambs K, Samuelsen SO, Opjordsmoen S. Depression in postpartum and nonpostpartum women: Prevalence and risk factors. Acta Psychiatr Scand. 2002;106(6):426–33. doi: 10.1034/j.1600-0447.2002.02408.x. [DOI] [PubMed] [Google Scholar]
- [10].Eberhard-Gran M, Tambs K, Opjordsmoen S, Skrondal A, Eskild A. A comparison of anxiety and depressive symptomatology in postpartum and non-postpartum mothers. Soc Psychiatry Psychiatr Epidemiol. 2003;38(10):551–6. doi: 10.1007/s00127-003-0679-3. [DOI] [PubMed] [Google Scholar]
- [11].Hamilton BE, Martin JA, Ventura SJ. Births: Preliminary data for 2012. Natl Vital Stat Rep. 2013;62(3):1–20. [PubMed] [Google Scholar]
- [12].Yang P, Chen YH, Yen CF, Chen HL. Psychiatric diagnoses, emotional-behavioral symptoms and functional outcomes in adolescents born preterm with very low birth weights. Child Psychiatry Hum Dev. 2015;46:358–66. doi: 10.1007/s10578-014-0475-1. [DOI] [PubMed] [Google Scholar]
- [13].Vohr B. Long-term outcomes of moderately preterm, late preterm, and early term infants. Clin Perinatol. 2013;40(4):739–51. doi: 10.1016/j.clp.2013.07.006. [DOI] [PubMed] [Google Scholar]
- [14].Hironaka M, Kotani T, Sumigama S, Tsuda H, Mano Y, Hayakawa H, et al. Maternal mental disorders and pregnancy outcomes: A clinical study in a Japanese population. J Obstet Gynaecol Res. 2011;37(10):1283–9. doi: 10.1111/j.1447-0756.2010.01512.x. [DOI] [PubMed] [Google Scholar]
- [15].Auger N, Le TU, Park AL, Luo ZC. Association between maternal comorbidity and preterm birth by severity and clinical subtype: Retrospective cohort study. BMC Pregnancy Childbirth. 2011;11:67. doi: 10.1186/1471-2393-11-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Kitai T, Komoto Y, Kakubari R, Konishi H, Tanaka E, Nakajima S, et al. A comparison of maternal and neonatal outcomes of pregnancy with mental disorders: Results of an analysis using propensity score-based weighting. Arch Gynecol Obstet. 2014;290(5):883–9. doi: 10.1007/s00404-014-3304-7. [DOI] [PubMed] [Google Scholar]
- [17].Niemi M, Falkenberg T, Petzold M, Chuc NT, Patel V. Symptoms of antenatal common mental disorders, preterm birth and low birthweight: A prospective cohort study in a semi-rural district of Vietnam. Trop Med Int Health. 2013;18(6):687–95. doi: 10.1111/tmi.12101. [DOI] [PubMed] [Google Scholar]
- [18].Wiencrot A, Nannini A, Manning SE, Kennelly J. Neonatal outcomes and mental illness, substance abuse, and intentional injury during pregnancy. Matern Child Health J. 2012;16(5):979–88. doi: 10.1007/s10995-011-0821-x. [DOI] [PubMed] [Google Scholar]
- [19].D'Onofrio BM, Class QA, Rickert ME, Larsson H, Langstrom N, Lichtenstein P. Preterm birth and mortality and morbidity: A population-based quasi-experimental study. JAMA Psychiatry. 2013;70(11):1231–40. doi: 10.1001/jamapsychiatry.2013.2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Kim DR, Sockol LE, Sammel MD, Kelly C, Moseley M, Epperson CN. Elevated risk of adverse obstetric outcomes in pregnant women with depression. Arch Womens Ment Health. 2013;16(6):475–82. doi: 10.1007/s00737-013-0371-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Grzeskowiak LE, Gilbert AL, Morrison JL. Neonatal outcomes after late-gestation exposure to selective serotonin reuptake inhibitors. J Clin Psychopharmacol. 2012;32(5):615–21. doi: 10.1097/JCP.0b013e31826686bc. [DOI] [PubMed] [Google Scholar]
- [22].Oberlander TF, Warburton W, Misri S, Aghajanian J, Hertzman C. Neonatal outcomes after prenatal exposure to selective serotonin reuptake inhibitor antidepressants and maternal depression using population based linked health data. Arch Gen Psychiatry. 2006;63(8):898–906. doi: 10.1001/archpsyc.63.8.898. [DOI] [PubMed] [Google Scholar]
- [23].Roca A, Garcia-Esteve L, Imaz ML, Torres A, Hernández S, Botet F, et al. Obstetrical and neonatal outcomes after prenatal exposure to selective serotonin reuptake inhibitors: The relevance of dose. J Affect Disord. 2011;135(1-3):208–15. doi: 10.1016/j.jad.2011.07.022. [DOI] [PubMed] [Google Scholar]
- [24].El Marroun H, Jaddoe VW, Hudziak JJ, Roza SJ, Steegers EA, Hofman A, et al. Maternal use of selective serotonin reuptake inhibitors, fetal growth, and risk of adverse birth outcomes. Arch Gen Psychiatry. 2012;69(7):706–14. doi: 10.1001/archgenpsychiatry.2011.2333. [DOI] [PubMed] [Google Scholar]
- [25].Gawlik S, Waldeier L, Muller M, Szabo A, Sohn C, Reck C. Subclinical depressive symptoms during pregnancy and birth outcome--a pilot study in a healthy German sample. Arch Womens Ment Health. 2013;16(2):93–100. doi: 10.1007/s00737-012-0320-0. [DOI] [PubMed] [Google Scholar]
- [26].Bindt C, Guo N, Bonle MT, Appiah-Poku J, Hinz R, Barthel D, et al. No association between antenatal common mental disorders in low-obstetric risk women and adverse birth outcomes in their offspring: Results from the CDS study in Ghana and Cote D'ivoire. PLoS One. 2013;8(11):e80711. doi: 10.1371/journal.pone.0080711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Nordeng H, van Gelder MM, Spigset O, Koren G, Einarson A, Eberhard-Gran M. Pregnancy outcome after exposure to antidepressants and the role of maternal depression: Results from the Norwegian mother and child cohort study. J Clin Psychopharmacol. 2012;32(2):186–94. doi: 10.1097/JCP.0b013e3182490eaf. [DOI] [PubMed] [Google Scholar]
- [28].Malm H, Sourander A, Gissler M, Gyllenberg D, Hinkka-Yli-Salomäki S, McKeague I, Artama M, Brown AS. Pregnancy complications following prenatal exposure to SSRIs or maternal psychiatric disorders: results from population-based national register data. Am J Psychiatry. doi: 10.1176/appi.ajp.2015.14121575. in press. doi: http://dx.doi.org/10.1176/appi.ajp.2015.14121575. [DOI] [PubMed]
- [29].Ding XX, Wu YL, Xu SJ, Zhu RP, Jua XM, Zhang SF, et al. Maternal anxiety during pregnancy and adverse birth outcomes: A systematic review and meta-analysis of prospective cohort studies. J Affect Disord. 2014;159:103–10. doi: 10.1016/j.jad.2014.02.027. [DOI] [PubMed] [Google Scholar]
- [30].Vigod SN, Kurdyak PA, Dennis CL, Gruneir A, Newman A, Seeman MV, et al. Maternal and newborn outcomes among women with schizophrenia: A retrospective population-based cohort study. BJOG. 2014;121(5):566–74. doi: 10.1111/1471-0528.12567. [DOI] [PubMed] [Google Scholar]
- [31].Boden R, Lundgren M, Brandt L, Reutfors J, Andersen M, Kieler H. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: Population based cohort study. BMJ. 2012;345:e7085. doi: 10.1136/bmj.e7085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Zhang J, Troendle J, Reddy UM, Laughon SK, Branch DW, Burkman R, et al. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol. 2010;203(4):326.e1–10. doi: 10.1016/j.ajog.2010.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Spong CY, Mercer BM, D'alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated latepreterm and early-term birth. Obstet Gynecol. 2011;118:323–33. doi: 10.1097/AOG.0b013e3182255999. 2 Pt 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Parikh LI, Reddy UM, Männistö T, Mendola P, Sjaarda L, Hinkle S, et al. Neonatal outcomes in early term birth. Am J Obstet Gynecol. 2014;211(3):265.e1–11. doi: 10.1016/j.ajog.2014.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Laughon SK, Reddy UM, Sun L, Zhang J. Precursors for late preterm birth in singleton gestations. Obstet Gynecol. 2010;116(5):1047–55. doi: 10.1097/AOG.0b013e3181f73f97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kelly R, Zatzick D, Anders T. The detection and treatment of psychiatric disorders and substance abuse among pregnant women cared for in obstetrics. Am J Psychiatry. 2001;158(2):213–9. doi: 10.1176/appi.ajp.158.2.213. [DOI] [PubMed] [Google Scholar]
- [37].Know your terms initiative [Internet] National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development. Bethesda, MD: [updated 2014 Feb 7; cited 2015 May 24]. Available from: http:/www.nichd.nih.gov/ncmhep/terms/Pages/index.aspx. [Google Scholar]
- [38].Rallis S, Skouteris H, McCabe M, Milgrom J. A prospective examination of depression, anxiety and stress throughout pregnancy. Women Birth. 2014;27(4):e36–42. doi: 10.1016/j.wombi.2014.08.002. [DOI] [PubMed] [Google Scholar]
- [39].Shapiro GD, Fraser WD, Frasch MG, Seguin JR. Psychosocial stress in pregnancy and preterm birth: Associations and mechanisms. J Perinat Med. 2013;41(6):631–45. doi: 10.1515/jpm-2012-0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].American College of Obstetricians and Gynecologists (ACOG) ACOG Committee Opinion No. 453. Screening for depression during and after pregnancy. Obstet Gynecol. 2010;115:394–5. doi: 10.1097/AOG.0b013e3181d035aa. 2 Pt 1. [DOI] [PubMed] [Google Scholar]
- [41].Ding XX, Wu YL, Xu SJ, Zhu RP, Jia RP, Zhang SF, et al. Maternal anxiety during pregnancy and adverse birth outcomes: A systematic review and meta-analysis of prospective cohort studies. J Affect Dis. 2014;159:103–10. doi: 10.1016/j.jad.2014.02.027. [DOI] [PubMed] [Google Scholar]
- [42].Alder J, Fink N, Bitzer J, Hösli I, Holzgreve W. Depression and anxiety during pregnancy: A risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med. 2007;20(3):189–209. doi: 10.1080/14767050701209560. [DOI] [PubMed] [Google Scholar]
- [43].Verkerk PH. The impact of alcohol misclassification on the relationship between alcohol and pregnancy outcome. Int J Epidemiol. 1992;21(Suppl 1):S33–37. doi: 10.1093/ije/21.supplement_1.s33. [DOI] [PubMed] [Google Scholar]
- [44].Huybrechts KF, Sanghani RS, Avorn J, Urato AC. Preterm birth and antidepressant medication use during pregnancy: A systematic review and meta-analysis. PLoS One. 2014;9(3):e92778. doi: 10.1371/journal.pone.0092778. [DOI] [PMC free article] [PubMed] [Google Scholar]