Abstract
Background and Aims
Stepped care approaches for mandated college students provide individual Brief Motivational Interventions (BMI) only for individuals who do not respond to an initial, low-intensity level of treatment such as Brief Advice (BA). However, how BMIs facilitate change in this higher-risk group of mandated students remains unclear. Perceived descriptive norms and alcohol-related expectancies are the most commonly examined mediators of BMI efficacy, but have yet to be examined in the context of stepped care.
Methods
Participants were mandated college students (N = 598) participating in a stepped care trial in which mandated students first received BA. Those who reported continued risky drinking 6 weeks following a BA session were randomized to either a single-session BMI (N=163) or an Assessment-only comparison condition (AO; N = 165). BMI participants reduced alcohol-related problems at the 9 month follow up significantly more than AO participants. Multiple mediation analyses using bootstrapping techniques examined whether perceived descriptive norms and alcohol-related expectancies mediated the observed outcomes.
Results
Reductions in perceptions of average student drinking (B = -.24; CI = -.61 to -.04) and negative expectancies (B = -.13; CI = -.38 to -.01) mediated the BMI effects. Furthermore, perceived average student norms were reduced after the BMI to levels approximating those of students who had exhibited lower risk drinking following the BA session.
Conclusions
Findings highlight the utility of addressing perceived norms and expectancies in BMIs, especially for students who have not responded to less intensive prevention efforts.
Keywords: Mediation, perceived descriptive norms, alcohol expectancies, alcohol, motivational interventions
Approximately half of the young adult population in the US currently attends college, and 60.3% of these students are current drinkers, with 40.1% engaging in heavy episodic drinking (HED, defined as 5 or more drinks in one occasion for males and 4 or more for females; SAMHSA, 2012; Snyder & Dillow, 2012). These students are at risk of experiencing a variety of alcohol-related problems (NIAAA, 2002), including campus alcohol policy violations (Wechsler et al., 2002). Many students who violate these policies are required to complete either public service or receive an alcohol intervention (Wechsler et al., 2002). However, a significant subset of these individuals do not require intensive intervention (Barnett et al., 2008; Barnett & Read, 2005) and may be more appropriate for a stepped care approach (Borsari et al., 2012; McKellar, Austin, & Moos, 2012; Sobell & Sobell, 2000). In stepped care, individuals who do not respond to an initial, low-intensity level of treatment are provided a more intensive treatment. One such treatment that has been demonstrated to reduce alcohol use and problems in mandated college students is individual Brief Motivational Interventions (BMIs: Borsari & Carey, 2005; Carey, Henson, Carey, & Maisto, 2009; Doumas, Workman, Smith, & Navarro, 2011; White, 2006).
To enhance existing BMIs and stepped care approaches, it is important to determine which components of BMIs facilitate reductions in alcohol use and problems. BMIs often include personalized feedback that can address several topics including personal rates of drinking, engagement in high risk behaviors, consequences from alcohol use, tips to reduce drinking, and other didactic information (Walters & Neighbors, 2005). Additionally, BMIs often provide feedback regarding two types of alcohol-related cognitions: perceived descriptive norms and alcohol-related expectancies. In a recent review of 43 studies providing personalized feedback to college students, perceived norms (42 of 43 studies; 98%) and alcohol-related expectancies (13 of 43; 30%) were the most commonly addressed drinking-related cognitions (Miller et al., 2013).
Perceived descriptive norms refer to students' perceptions of how much and how often other individuals consume alcohol (Perkins, 2003) are commonly assessed by asking students to estimate the drinking of other students (e.g., close friend, the average college student). Norms have consistently been associated with college student drinking (Borsari & Carey, 2001, 2003; Larimer et al., 2011; Lewis & Neighbors, 2004), with students who overestimate the amount and frequency of alcohol consumption of others reporting higher drinking themselves (Borsari & Carey, 2001). Normative data are typically incorporated into interventions to correct the misperception that other student's drink heavily, in hope that drinking will decrease (Lewis & Neighbors, 2006; Miller et al., 2012). Prior research has demonstrated that a lowered perception of other students drinking mediates treatment and alcohol-related outcomes (Borsari & Carey, 2000; Carey, Henson, Carey, & Maisto, 2010; Turrisi et al., 2009; Walters, Vader, Harris, Field, & Jouriles, 2009; Wood, Capone, Laforge, Erickson, & Brand, 2007).
Alcohol expectancies, or the beliefs about the effects/consequences of alcohol, are also predictive of alcohol consumption and problems (Fromme & D'Amico, 2000; Greenfield, Harford, & Tam, 2009; Pabst, Kraus, Piontek, Mueller, & Demmel, 2014). Approaches that challenge and modify these expectancies have been shown to reduce alcohol use in the short-term (Lau-Barraco & Dunn, 2008; NIAAA, 2002; Scott-Sheldon, Terry, Carey, Garey, & Carey, 2012). These interventions differ in content and delivery with some expectancy challenges implementing an in-vivo approach designed to reduce alcohol expectancies through experiential learning typically in a bar-like setting (Labbe & Maisto, 2011; Scott-Sheldon et al., 2012), and others, like BMIs, take a more didactic approach (Scott-Sheldon et al., 2012). Hence, one way BMIs may reduce drinking and associated problems is through changes in negative (“I would feel guilty”) and positive (“I would be outgoing”) alcohol expectancies. With respect to BMIs, there have been mixed findings for alcohol expectancies mediating the relationship between treatment and alcohol-related outcomes, with some studies demonstrating that changes in alcohol beliefs mediate the relationship for consumption and problems (Black et al., 2012; Turrisi et al., 2009), whereas others have not found expectancies to be an influential mediator of either outcome (Borsari & Carey, 2000; Kulesza, McVay, Larimer, & Copeland, 2013). One reason for this discrepancy may be the population examined, which ranged from heavy drinking, but not mandated students, socially anxious college students and former athletes. The current study would add to the expectancy literature by examining mandated college students within a stepped care approach.
In sum, perceived norms and expectancies are widely addressed in BMIs (Butler, Silvestri, & Correia, 2014; Miller & Leffingwell, 2013) and can mediate BMI effects (Black et al., 2012; Borsari & Carey, 2000; Carey et al., 2010; Turrisi et al., 2009; Walters et al., 2009; Wood et al., 2007). It is possible that the highly personalized nature of feedback for both norms and expectancies in the context of BMIs play a role in their utility. A recent meta-analytic review has highlighted the link between BMI efficacy and the degree to which BMI content has been personalized (Ray et al., 2014). Specifically, BMI's that contain information based on the individual's own behaviors and cognitions (depth) were more effective than BMIs that delivered a wide range of topics (breadth). Despite these compelling findings, it is important to consider that this research evaluated “stand alone” interventions. Therefore, it is necessary to replicate and extend this research in the context of stepped care approaches, in which BMI recipients have continued to exhibit risky drinking despite receiving a lower-intensity intervention. Perhaps more personalized topics presented to this particularly risky sample will be more likely to facilitate change.
To examine whether norms and expectancies mediate BMIs delivered to higher-risk mandated students, we conducted a secondary analysis of data from a randomized clinical trial implementing stepped care with mandated college students (Borsari et al., 2012). In the parent study, participants who violated a campus alcohol policy at a four-year, private liberal arts university in the Northeast, agreed to participate in the research study and provided informed consent. All students received a manualized, 10-15 minute Brief Advice (BA) session that was administered by a peer counselor (fellow college student). Six weeks after the BA session, participants completed an online assessment and higher risk (i.e., those who reported 5 or more alcohol-related consequences and four or more HED occasions) were eligible to receive the next step of care and were randomly assigned to BMI or Assessment Only conditions (AO). Perceived descriptive norms and alcohol-related expectancies were discussed in the BMI, but not in the initial BA session that everyone received. Participants completed assessments 3, 6 and 9 months following the assignment to condition. Lower risk drinkers (4 or fewer alcohol-related consequences and 3 or fewer HED episodes) were not provided additional intervention, but completed follow-up assessments. Higher risk participants who received a BMI significantly reduced their alcohol-related problems (but not alcohol use) at the 9-month follow-up compared to participants in the AO condition. Furthermore, lower risk students reported stable levels of low-risk drinking throughout the entire 9 month follow-up period.
We examined three hypotheses to evaluate whether perceived descriptive norms and alcohol-related expectancies mediated the observed reductions in alcohol-related problems reported 9 months after receiving a BMI. First, because descriptive norms were addressed in the BMI session, we hypothesized that the BMI would be associated with lower perceived descriptive norms, which would be related to fewer alcohol-related problems. Second, with both positive and negative expectancies discussed within the BMI session, we hypothesized that BMI would lead to decreases in positive expectancies and increases in negative expectancies, which would be related to fewer alcohol-related problems. Then, in order to put these mediation analyses in the context of the larger stepped care trial, we examined changes in the proposed mediators across time in higher risk drinkers in comparison to the lower risk drinkers. We hypothesized that participants receiving the BMI would report lower perceived descriptive norms, fewer positive expectancies and more negative expectancies at levels similar to the lower risk drinkers. These analyses provide a stringent test of whether perceived descriptive norms and alcohol-related expectancies mediate BMI efficacy in the context of stepped care with mandated college students.
Method
Participants
Prospective participants were undergraduate students age 18 years and older, who violated campus alcohol policy at a four-year, private liberal arts university in the Northeast (Borsari et al., 2012). Students (N = 982) were referred to the student health office for mandatory counseling following adjudication by campus judicial affairs staff. Of these students, 61% (n=598; 69.1% male; 95.8% Caucasian) agreed to participate in the study and provided informed consent. Students who declined to participate (n = 384) received treatment as usual, consisting of a 15-30 minute individual discussion of their referral incident and alcohol use. Of the 598 students, 97% (n = 582) completed an online assessment 6 weeks after the BA session; lower risk drinkers (n = 102) were not randomized to stepped care and were not provided additional intervention, but completed follow-up assessments. Those identified as higher risk were randomly assigned to BMI (n = 211) or AO (n = 194) conditions. Because mediation focuses on the product of two path coefficients and to minimize the effect of missing data, analyses for the current study were conducted only with participants who completed all three follow-up assessments (n = 418; 64.6% male; 96.2% Caucasian; Chen, Aryee, & Lee, 2005; Preacher & Hayes, 2004), resulting in a total of 90 lower risk drinkers and 328 higher risk drinkers (BMI: n = 163; AO: n = 165)1. All procedures were approved by the university Institutional Review Board.
Interventions
Step 1: Brief Advice (BA)
The manualized BA was administered by a peer counselor employed at the Office of Health and Wellness on campus. The counselor provided a 12-page booklet containing educational information (Cunningham, Wild, Bondy, & Lin, 2001). The BA session was mostly didactic, but the counselors did solicit personal information from participants using open-ended questions and gave participants the opportunity to ask questions or discuss their personal alcohol use. The average time of the BA session was 14.07 minutes (SD = 4.59).
Step 2: Brief Motivational Intervention (BMI)
This manualized BMI was adapted from previous interventions with college students (Dimeff, Baer, Kivlahan, & Marlatt, 1999). Participants were given a personalized report that provided feedback from individual responses to the baseline and six-week follow-up assessments, including information about perceived and actual campus drinking norms and positive and negative alcohol expectancies. Throughout the BMI, interventionists followed the four principles of Motivational Interviewing (MI): express empathy, develop discrepancy, roll with resistance, and support self-efficacy for change (see Miller & Rollnick, 2002) to facilitate intrinsic motivation to reduce alcohol use and consequences. The average length of the BMIs was 52.54 minutes (SD = 12.12). All interventionist received thorough training in motivational interviewing that consisted of didactics, role plays, and supervision to ensure competency. Feedback from supervision included advice on BMI proficiency and adherence to the protocol. Intervention fidelity was measured by coding sessions with the Motivational Interviewing Skills Code (MISC 2.1; (Miller, Moyers, Ernst, & Amrhein, 2008). Results indicated high fidelity and that clinicians consistently administered the intervention components and adhered to an MI style when indicated (Borsari et al., in press).
Outcome Measure
Alcohol-related problems
Alcohol-related consequences were assessed using the Brief-Young Adult Alcohol Consequences Questionnaire (B-YAACQ; Kahler, Strong, & Read, 2005), a 24-item subset of the 48-item Young Adult Alcohol Consequences Questionnaire (YAACQ: Read, Kahler, Strong, & Colder, 2006). Dichotomous items (yes/no) are summed for a total number of consequences experienced in the past month. The B-YAACQ is reliable yet sensitive to changes in alcohol use over time (Kahler, Hustad, Barnett, Strong, & Borsari, 2008) and has demonstrated high internal consistency in research with college students (Kahler et al., 2005). In this study, the B-YYACQ demonstrated good internal consistency at baseline and the three follow-up assessments (Cronbach alphas ranged from .85 - .89).
Mediator Variables
Perceived drinking norms
Perceived drinking norms were assessed at baseline and all follow-up appointments via the Drinking Norms Rating Form (DNRF; Baer, Stacy, & Larimer, 1991). The DNRF assessed participants' estimates of their own weekly alcohol consumption in the past month as well as their perceptions of the weekly drinking of their close friends and the average student at their university. The DNRF has been used extensively with mandated college students (Borsari, Boyle, et al., 2007; Borsari & Carey, 2005; Carey, Borsari, Carey, & Maisto, 2006). The current study utilized the reported perceived number of drinks per week of a close friend and the average student in analyses.
Alcohol expectancies
Expectancies were measured using the Brief Comprehensive Effects of Alcohol Scale (Ham, Stewart, Norton, & Hope, 2005) at baseline and all follow-up assessments. This 15-item measure assesses positive (e.g., “I would act sociable”) and negative (e.g., “I would feel dizzy”) expectancies about the effects of alcohol use. Students reported their level of agreement with each expectancy statement using a 4-point scale (1 = Disagree to 4 = Agree). Scores are computed by summing across all items among the individual factors and divided by the total number of items in each factor. Higher values are indicative of more alcohol expectancies. Internal consistency was good for the baseline and all follow-up assessments (Cronbach alphas at ranged from .77 to 87).
Analysis Plan
In the current study, we were interested in the indirect effect of BMI on alcohol related problems through norms and expectancies.2 The stepped care approach necessitates some unique decisions regarding data selection. Specifically, all participants received a BA session in the interim between the baseline and 6-week assessment. Therefore, data collected at the 6-week assessment (and not baseline) was the closest assessment of covariates before randomization to BMI or AO (Borsari et al., 2014). Furthermore, the two mediators were assessed 3 months post-BMI.
After controlling for gender and pre-randomization alcohol-related problems, multiple mediation of 3 month mediator variables was tested to the 9-month outcome variable. Simultaneous multiple mediation was conducted using the INDIRECT SPSS macro that utilized bootstrapping techniques for indirect effects based on 5000 bootstrap samples (Preacher & Hayes, 2008). The bootstrapping technique makes no distributional assumptions, nor does it require a significant relationship between the independent and dependent variables (MacKinnon et al., 2000; Preacher & Hayes, 2008). If zero lies within the 95% confidence intervals of the bootstrapping method, results are interpreted as non-significant. Finally, to examine the mediation analyses in the context of the larger stepped care trial, we examined differences between lower risk drinkers and higher risk drinkers on the proposed mediators using separate one-way ANOVAs at each time point.
Results
Preliminary Analyses
Baseline descriptive characteristics of the overall sample were examined, including demographic information and the means and standard deviations for the outcome variable (alcohol-related problems) and mediator variables (perceived drinking norms and alcohol expectancies). Comparison between those who completed all follow-up assessments (n = 418) and those who did not (n = 180) revealed no significant differences on demographic or baseline drinking and mediator variables (all ps > .05).
Mediation Analyses
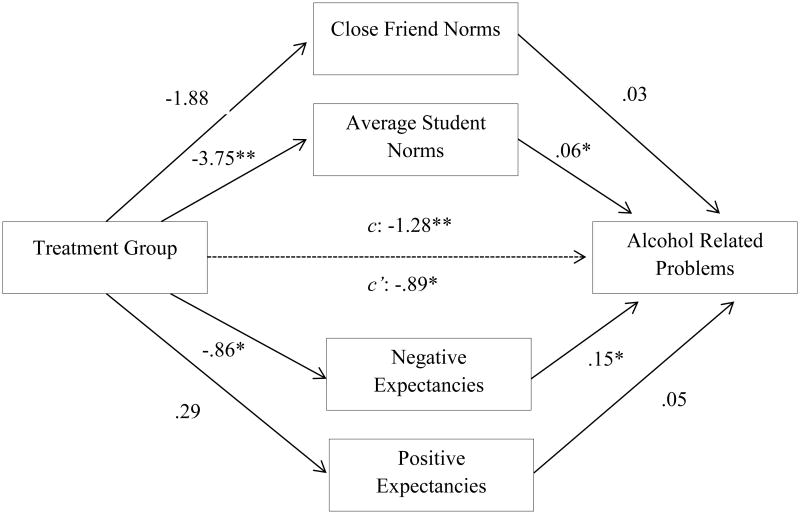
The significance tests for the total and the direct effects, which allow for the interpretation of the direction of the various paths of the individual putative mediators at the 9-month follow-up, are presented in Table 1 and Figure 1. The a path (treatment group to mediator variables) indicated that treatment group is significantly related to average student drinking norms (p = .008) and negative expectancies (p = .04). The b path (mediator variables to alcohol-related problems) demonstrated that perceived drinking of the average student and negative expectanices were significantly related to alcohol-related problems at the 9-month follow-up (p = .002; p = .03, respectively).
Table 1. Significance tests for the total and direct effects (Path a and Path b) of the individual putative meditators and alcohol related problems at the 9 month follow-up.
| Treatment Group on Mediators (a path) | Mediators on Dependent Variable (b path) | |
|---|---|---|
| β(se) | β(se) | |
|
|
|
|
| Descriptive Norms | ||
| Close friend | -1.884 (1.60) | 0.025 (.02) |
| Average student | -3.746 (1.40)** | 0.063 (.02)** |
| Expectancies regarding alcohol use | ||
| Negative Expectancies | -0.856 (.41)* | 0.151 (.07)* |
| Positive Expectancies | 0.290 (.45) | 0.053 (.06) |
Note.
p ≤. 05;
p ≤ .01
Figure 1.
Multiple Mediator model with unstandardized regression coefficients predicting 9 month alcohol related problems, controlling for baseline alcohol related problems and gender. * p <.05; **p <.01
Table 2 contains the overall significance of the individual mediators (point estimates and confidence intervals). Interpretation of the mediation analysis does not require significance of the a and b paths, but instead focuses on the direction and size of the indirect effects (Preacher & Hayes, 2008). Results indicate that taken as a set, perceived drinking norms and alcohol expectancies significantly mediate BMI effects on alcohol related problems (B = -.40; CI = -.80 to -.07). An examination of the specific indirect effects however, reveal that only estimates of the average student norm and negative expectancies at 3 months mediated the effect of the BMI on alcohol-related problems by the 9 month follow-up. The BMI condition was associated with lower perceived norms at 3 months, and these reductions were related to fewer problems at 9 months (B = -.24; CI = -.61 to -.04). Contrary to hypotheses, students in the BMI condition endorsed lower negative expectations than those in AO at 3 months, and these reductions were associated with fewer problems at the 9 month assessment (B = -.13; CI = -.38 to -.01). Neither estimates of close friend norms or positive expectancies contributed to the above indirect effect above and beyond perceived average student norms and negative expectancies.
Table 2. Mediation of alcohol-related problems by descriptive norms and alcohol expectancies of drinking at the 9 month follow-up.
| Alcohol related problems | |||
|---|---|---|---|
|
| |||
| Point Estimate | BCa 95% CI | ||
|
| |||
| Lower | Upper | ||
| Descriptive Norms | |||
| Close friend | -.0476 | -.2419 | .0221 |
| Average student | -.2365 | -.6132 | -.0404* |
| Alcohol-related Expectancies | |||
| Negative Expectancies | -.1294 | -.3792 | -.0080* |
| Positive Expectancies | .0150 | -.0296 | .1596 |
| Total | -.3985 | -.7963 | -.0728* |
Note: BCa = Bias Corrected and Accelerated.
Confidence intervals not containing zero are interpreted as significant
Comparisons between lower and higher risk drinkers on mediation variables
Separate one way ANOVA's and post-hoc analyses were conducted to compare the proposed mediator variables in lower risk (BA group) and higher risk (BMI vs. AO groups) drinkers at four assessment time points (Table 3). At all follow-ups, the lower risk group reported lower levels of norms and expectancies than the higher risk group (all ps < .002). Higher risk drinkers who completed a BMI reported reduced average student norms at the 3 and 9 month follow-ups (consistent with lower risk drinkers). In contrast, those in the AO condition continued to report significantly higher average student norms. Finally, higher risk drinkers who completed a BMI reported significantly fewer negative expectancies compared to drinkers in the AO condition at the 3 month follow-up (p < .001).
Table 3. Means and standard deviations on outcome and mediator variables of lower and higher risk groups at each assessment.
| Baseline | 6 Week | 3 Month | 9 Month | |
|---|---|---|---|---|
|
| ||||
| Variables | M(SD) | M(SD) | M(SD) | M(SD) |
| Alcohol Problems | ||||
| Lower Risk | 2.81(.307)a | 1.30(1.70)a | 1.96(2.78)a | 2.56(3.55)a |
| Higher Risk - BMI | 6.63(4.42)b | 6.66(4.70)b | 5.26(4.44)b | 4.76(4.49)b |
| Higher Risk - AO | 7.27(4.47)b | 7.56(5.04)b | 6.68(5.38)c | 6.61(5.42)c |
| Descriptive Norms | ||||
| Close Friend Norms | ||||
| Lower Risk | 16.97(12.63)a | 15.67(13.06)a | 15.01(11.55)a | 16.49(12.83)a |
| Higher Risk - BMI | 27.10(15.95)b | 26.78(15.24)b | 23.21(14.49)b | 23.06(13.76)b |
| Higher Risk - AO | 27.61(15.57)b | 27.91(14.59)b | 26.45(16.25)b | 26.06(16.22)b |
| Average Student Norms | ||||
| Lower Risk | 21.96(9.67)a | 20.32(12.04)a | 20.83(12.62)a | 21.51(11.86)a |
| Higher Risk - BMI | 28.94(14.15)b | 27.77(14.07)b | 22.35(11.87)a | 21.32(10.76)a |
| Higher Risk - AO | 29.57(13.50)b | 27.24(11.94)b | 27.24(14.48)b | 26.21(12.26)b |
| Alcohol Expectancies | ||||
| Negative Expectancies | ||||
| Lower Risk | 15.28(4.43)a | 15.13(3.90)a | 15.08(3.85)a | 15.42(4.34)a |
| Higher Risk - BMI | 17.13(4.30)b | 16.82(3.98)b | 16.46(3.92)b | 16.71(4.01)b |
| Higher Risk - AO | 17.47(4.14)b | 17.19(4.11)b | 17.53(3.83)c | 17.22(3.44)b |
| Positive Expectancies | ||||
| Lower Risk | 19.49(5.37)a | 19.08(5.01)a | 19.46(4.98)a | 19.76(5.41)a |
| Higher Risk - BMI | 21.51(4.71)b | 21.55(4.45)b | 21.55(4.16)b | 21.77(4.55)b |
| Higher Risk - AO | 21.86(4.65)b | 21.45(4.28)b | 21.58(4.29)b | 21.54(3.91)b |
Note. All participants received a brief advice session that at baseline. Those who continued to drink to risky levels and experienced alcohol related problems (higher risk drinkers) were randomized to either the BMI or AO condition following the 6 week assessment. BMI assessments occurred between 6 week and 3 month assessments. All participants (lower and higher risk drinkers) completed the 3 and 9 month follow-ups. Means that do not share subscripts differ at p < .05.
Discussion
To our knowledge, this is the first study to examine whether drinking norms and alcohol expectancies mediate the effects of a BMI delivered in the context of stepped care. Results indicated that changes in norms and expectancies mediated BMI effects on alcohol related problems. These findings are consistent with prior research showing that BMIs reduce perceptions of descriptive norms, which in turn reduces alcohol-related consequences (Borsari & Carey, 2001; Carey et al., 2010; Wood et al., 2007). They also support the presence of a bidirectional relationship between perceived norms and alcohol-related problems (Lee, Geisner, Patrick, & Neighbors, 2010) and that changes in norms precedes reductions in problems (Neighbors, Dillard, Lewis, Bergstrom, & Neil, 2006).
Although descriptive norms are cognitions representing actual drinking behaviors, in this sample, norms were a mediator of the effects of the BMI on alcohol related problems, not consumption. The experience of alcohol related problems by college students cannot be solely explained by alcohol consumption (Larimer et al., 2001; Turner, Larimer, & Sarason, 2000), hence descriptive norms may in part, contribute to this relationship. For example, corrected drinking norms following the BMI may have led to increased pressure to conform to socially appropriate drinking practices. Because alcohol consumption is often done in a public setting, consequences experienced while drinking are likely to be observed or noticed by others and indicative of heavy drinking. Participants may have figured out a way to reduce their experience of alcohol related problems while maintaining similar drinking rates. For example, students may have increased their protective behavioral strategies following the BMI that allowed them to reduce the harm associated with their drinking (Murphy et al., 2012). Although we did not assess protective behavioral strategies in this paper, following the BMI, participants may have spread out their drinks throughout the night, alternated alcoholic beverages with non-alcoholic beverages, and/or decreased pre-gaming behaviors. Therefore, despite quantity of drinks remaining constant, participant's experience of alcohol-related problems may have been reduced.
The lack of mediation by close friend perceived descriptive norms may be because it was not specifically corrected in the BMI: actual drinking of friends was not presented, which supports research demonstrating normative perceptions are stable and unlikely to change without corrective information (Neighbors et al., 2006). Although examining alcohol consumption, the stability of norms is also consistent with research indicating that mandated students who had higher close friend norms were less likely to reduce their drinking regardless of alcohol sanctions than students who perceived lower close friend norms (Merrill, Carey, Reid, & Carey, 2014).
Contrary to hypotheses and prior research (Black et al., 2012), positive expectancies did not mediate reductions in problems. Although counterintuitive, BMI was associated with reductions in negative expectancies, which were then linked to reductions in alcohol-related problems. Although both positive and negative expectancies were addressed in the BMI, perhaps mandated students receiving intensive interventions are more sensitive to reductions in negative expectancies than reductions in positive expectancies. They may be more likely to expect negative consequences and accept them as a natural result of drinking or alternatively, may not actually evaluate them as negative (Mallett, Bachrach, & Turrisi, 2008). A recent integrative data analysis study found that when brief alcohol intervention content is personalized, interventions that include more content are generally more efficacious (Ray et al., 2014), so perhaps our discussion of alcohol expectancies were not personalized enough to facilitate change. Future work should consider incorporating more personal accounts of alcohol expectancies. There may be temporal confound at work as well during the 3 month assessment point, with negative expectancies being suppressed by the simultaneous reduction in alcohol-related problems. A meta-analysis on expectancy challenges indicated that interventions appeared to only increase negative expectancies in older college students (Scott-Sheldon et al., 2012). Our sample was relatively young (M = 18.77) and perhaps these students did not have enough experience with alcohol to encounter negative alcohol consequences and therefore could not summon negative expectancies during the BMI session.
Furthermore, the stepped care design of the parent trial provided a unique context in which to examine BMIs effect on alcohol-related problems and on potential mediators. Specifically, lower risk drinkers reported lower perceptions of average students drinking compared to higher risk drinkers, and the higher risk drinkers randomized to the BMI condition reduced their perceptions of the average students' drinking at the remainder of the follow-ups. This reduction was not observed in the higher-risk students in AO condition. It is also telling that neither intervention (BA or BMI) appeared to have altered the higher risk drinkers' perceptions of close friends' drinking behaviors. In contrast, lower risk drinkers reported significantly lower close friend norms in comparison to higher risk drinkers' at four time points. Although lower risk drinkers reported fewer positive and negative expectancies compared to higher risk drinkers at all assessment time points, higher risk drinkers who received a BMI reported fewer negative expectancies (consistent with lower risk drinkers) than those in the AO condition who continued to report elevated negative expectancies. Future research may want to continue investigating lower risk drinkers to inform BMIs and potential mediators to target.
Clinically, the observed reduction in typical student norms following the BMI provides further support for explicitly addressing perceived norms in interventions designed to reduce alcohol-related problems. If not addressed, norms appear to be stable and resistant to change and there is little evidence to suggest that providing normative data information for lower risk drinkers will result in an increase in normative perception or personal drinking (Prince, Reid, Carey, & Neighbors, 2014). The verdict on the utility of expectancies is somewhat less definitive. Our results suggest that BMI led to fewer alcohol related problems through reductions in negative expectancies, and lower risk drinkers report fewer negative alcohol expectancies. Therefore, our findings do not support decreasing positive expectancies and clinicians may want to focus on discussions about negative alcohol expectancies when working with mandated students. The lack of the expected mediation effects of positive expectancies, suggests that these cognitions may be more resistant to change in a mandated students. Perhaps a more intensive expectancy challenge intervention (experiential) is required to facilitate mediation of positive expectancies in this particularly risky sample.
The results of this study should be interpreted within the context of its limitations. First, the decision rules identifying lower and higher risk students in this trial were based on pilot research (Borsari, O'Leary Tevyaw, Barnett, Kahler, & Monti, 2007), thus limiting the generalizability of the present findings to future applications of stepped care with mandated students using more (or less) stringent decision rules for assignment to the next step of intervention. Second, we acknowledge that the measurement of mediators at the 6-week and 3-month assessments, with an intervening BMI, is not ideal. It is possible that more acute change in the mediators facilitated by the BMI may have been missed, or that other personal or environmental factors may have influenced the observed changes in perceived descriptive norms and expectancies (e.g., changes in social group). Third, lack of a control condition such as an alcohol education session (Borsari & Carey, 2005) makes it impossible to rule out other nonspecific factors as contributing to the observed effects (e.g., attending another session with an interventionist). Fourth, data were collected via self-report and did not include corroborating measures. Previous research with collateral informants (Borsari & Muellerleile, 2009) revealed that mandated students may slightly under-report their alcohol use, and perhaps this occurred during this trial.
Despite these limitations, our findings add to the existing literature on mediators of BMIs. Namely, changes in perceived average student descriptive norms and negative expectancies appear to play a significant role in the reductions of alcohol-related problems following a BMI, even in students who are not responsive to less intense intervention. Therefore, we recommend the continued inclusion of perceived descriptive norms in BMIs for mandated students, whereas further research on the utility of including expectancies in BMIs is warranted. Additionally, any innovations that make this feedback personal and compelling to its recipients is encouraged.
Acknowledgments
Ali Yurasek's contribution to the manuscript was supported by NIDA grant T32 DA016184. Brian Borsari's contribution was supported by National Institute on Alcohol Abuse and Alcoholism Grants R01-AA015518, R01-AA017874, and VISN1 Career Development Award V1CDA2012-18. Molly Magill's contribution was supported by NIAAA grant K23 AA018126. Nadine Mastroleo's contribution to this manuscript was supported by NIAAA grant T32 AA07459. John Hustad's contribution was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through grant UL1RR033184 and KL2RR033180. Peter Monti's contribution was supported by NIAAA grant K05AA019681.
Footnotes
Due to the importance of temporal assessment and concerns that missing values at 6 weeks before the BMI and 3 months following the intervention would not provide a clear picture of the mediation effects, authors decided to use complete sample data. However, multiple mediation analyses were also conducted with the full sample, regardless of follow-up completion, and results indicated a similar pattern of findings.
Because some researchers argue that a significant total effect of X on Y is not necessary for mediation to occur (MacKinnon, Krull, & Lockwood, 2000), multiple mediation was also conducted with the proposed mediators to the primary alcohol consumption outcome variables at the 9-month follow-up. Results indicated that changes in perceived norms and expectancies were not significant mediators on the effects of a BMI on alcohol consumption delivered in the context of stepped care.
Contributor Information
Ali M. Yurasek, Center for Alcohol and Addiction Studies, Public Health Department, Brown University
Brian Borsari, Center for Alcohol and Addiction Studies, Public Health Department, Brown University.
Molly Magill, Center for Alcohol and Addiction Studies, Public Health Department, Brown University.
Nadine R. Mastroleo, Center for Alcohol and Addiction Studies, Public Health Department, Brown University
John T.P. Hustad, Department of Medicine, Pennsylvania State College of Medicine
Tracy O'Leary Tevyaw, Mental Health and Behavioral Sciences Service, Department of Veterans Affairs Medical Center.
Nancy P. Barnett, Center for Alcohol and Addiction Studies, Public Health Department, Brown University
Christopher W. Kahler, Center for Alcohol and Addiction Studies, Public Health Department, Brown University
Peter M. Monti, Center for Alcohol and Addiction Studies, Public Health Department, Brown University
References
- Baer JS, Stacy A, Larimer ME. Biases in the perception of drinking norms among college students. Journal of Studies on Alcohol. 1991;52(6):580–586. doi: 10.15288/jsa.1991.52.580. [DOI] [PubMed] [Google Scholar]
- Barnett NP, Borsari B, Hustad JTP, Tevyaw TO, Colby SM, Kahler CW, Monti PM. Profiles of college students mandated to alcohol intervention. Journal of Studies on Alcohol and Drugs. 2008;69(5):684–694. doi: 10.15288/jsad.2008.69.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett NP, Read JP. Mandatory alcohol intervention for alcohol-abusing college students: A systematic review. Journal of Substance Abuse Treatment. 2005;29(2):147. doi: 10.1016/j.jsat.2005.05.007. [DOI] [PubMed] [Google Scholar]
- Black JJ, Tran GQ, Goldsmith AA, Thompson RD, Smith JP, Welge JA. Alcohol expectancies and social self-efficacy as mediators of differential intervention outcomes for college hazardous drinkeres with social anxiety. Addictive Behaviors. 2012;37:248–255. doi: 10.1016/j.addbeh.2011.10.004. [DOI] [PubMed] [Google Scholar]
- Borsari B, Boyle KE, Hustad JTP, Barnett NP, O'Leary Tevyaw T, Kahler CW. Drinking before drinking: Pregaming and drinking games in mandated students. Addictive Behaviors. 2007;32(11):2694–2705. doi: 10.1016/j.addbeh.2007.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. Journal of Consulting and Clinical Psychology. 2000;68(4):728–733. doi: 10.1037//0022-006X.68.4.728. [DOI] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Peer influences on college drinking: A review of the research. Journal of Substance Abuse. 2001;13(4):391–424. doi: 10.1016/S0899-3289(01)00098-0. [DOI] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Descriptive and injunctive norms in college drinking: a meta-analytic integration. Journal of Studies on Alcohol. 2003;64(3):331–341. doi: 10.15288/jsa.2003.64.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Two brief alcohol interventions for mandated college students. Psychology of Addictive Behaviors. 2005;19(3):296–302. doi: 10.1037/0893-164X.19.3.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Hustad JTP, Mastroleo NR, Tevyaw TO, Barnett NP, Kahler CW, et al. Monti PM. Addressing alcohol use and problems in mandated college students: A randomized clinical trial using stepped care. Journal of Consulting & Clinical Psychology. 2012;80(6):1062–1074. doi: 10.1037/A0029902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Muellerleile P. Collateral reports in the college setting: A meta-analytic integration. Alcoholism: Clinical & Experimental Research. 2009;33(5):826–838. doi: 10.1111/j.1530-0277.2009.00902.x.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, O'Leary Tevyaw T, Barnett NP, Kahler CW, Monti PM. Stepped care for mandated college students: a pilot study. American Journal on Addictions. 2007;16(2):131–137. doi: 10.1080/10550490601184498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Short EE, Mastroleo NR, Hustad JT, Tevyaw TO, Barnett NP, et al. Monti PM. Phone-delivered brief motivational interventions for mandated college students delivered during the summer months. Journal of Substance Abuse Treatment. 2014;46(5):592–596. doi: 10.1016/j.jsat.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler LH, Silvestri MM, Correia CJ. Student perceptions of specific components within a personalized feedback intervention. Psychol Addict Behav. 2014;28(2):614–618. doi: 10.1037/a0036485. [DOI] [PubMed] [Google Scholar]
- Carey KB, Borsari B, Carey MP, Maisto SA. Patterns and importance of self-other differences in college drinking norms. Psychology of Addictive Behaviors. 2006;20(4):385–393. doi: 10.1037/0893-164X.20.4.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Henson JM, Carey MP, Maisto SA. Computer versus in-person intervention for students violating campus alcohol policy. Journal of Consulting and Clinical Psychology. 2009;77(1):74–87. doi: 10.1037/a0014281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Henson JM, Carey MP, Maisto SA. Perceived Norms Mediate Effects of a Brief Motivational Intervention for Sanctioned College Drinkers. Clinical Psychology-Science and Practice. 2010;17(1):58–71. doi: 10.1111/j.1468-2850.2009.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JA, Wild TC, Bondy SJ, Lin E. Impact of normative feedback on problem drinkers: A small-area population study. Journal of Studies on Alcohol. 2001;62(2):228–233. doi: 10.15288/jsa.2001.62.228. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief Alcohol Screening and Intervention for College Students (BASICS): A harm reduction approach. New York: Guilford Press; 1999. [Google Scholar]
- Doumas DM, Workman C, Smith D, Navarro A. Reducing high-risk drinking in mandated college students: evaluation of two personalized normative feedback interventions. Journal of Substance Abuse. 2011;40(4):376–385. doi: 10.1016/j.jsat.2010.12.006. [DOI] [PubMed] [Google Scholar]
- Fromme K, D'Amico EJ. Measuring adolescent alcohol outcome expectancies. Psychology of Addictive Behaviors. 2000;14(2):206–212. doi: 10.1037//0893-164x.14.2.206. [DOI] [PubMed] [Google Scholar]
- Greenfield AL, Harford TC, Tam TW. Modeling cognitive influences on drinking and alcohol problems. Journal of Studies on Alcohol and Drugs. 2009;70:78–86. doi: 10.15288/jsad.2009.70.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ham LS, Stewart S, Norton P, Hope DA. Psychometric Assessment of the Comprehensive Effects of Alcohol Questionnaire: Comparing a Brief Version to the Original Full Scale. Journal of Psychopathology and Behavioral Assessment. 2005;27(3):141–158. [Google Scholar]
- Kahler CW, Hustad JTP, Barnett NP, Strong DR, Borsari B. Validation of the 30-Day version of the Brief Young Adult Alcohol Consequences Questionnaire for use in longitudinal studies. Journal of Studies on Alcohol and Drugs. 2008;69(4):611–615. doi: 10.15288/jsad.2008.69.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Read JP. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: the brief young adult alcohol consequences questionnaire. Alcoholism: Clinical & Experimental Research. 2005;29(7):1180–1189. doi: 10.1097/01.ALC.0000171940.95813.A5. [DOI] [PubMed] [Google Scholar]
- Kulesza M, McVay MA, Larimer ME, Copeland AL. A randomized clinical trial comparing the efficacy of two active conditions of a brief intervention for heavy college drinkers. Addictive Behaviors. 2013;38(4):2094–2101. doi: 10.1016/j.addbeh.2013.01.008. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Neighbors C, LaBrie JW, Atkins DC, Lewis MA, Lee CM, et al. Walter T. Descriptive drinking norms: for whom does reference group matter? J Stud Alcohol Drugs. 2011;72(5):833–843. doi: 10.15288/jsad.2011.72.833. Research Support, N.I.H., Extramural. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Turner AP, Anderson BK, Fader JS, Kilmer JR, Palmer RS, Cronce JM. Evaluating a brief alcohol intervention with fraternities. Journal of Studies on Alcohol. 2001;62(3):370. doi: 10.15288/jsa.2001.62.370. [DOI] [PubMed] [Google Scholar]
- Lau-Barraco C, Dunn ME. Evaluation of a single-session expectancy challenge intervention to reduce alcohol use among college students. Psychology of Addictive Behaviors. 2008;22(2):168–175. doi: 10.1037/0893-164x.22.2.168. [DOI] [PubMed] [Google Scholar]
- Lee CM, Geisner IM, Patrick ME, Neighbors C. The social norms of alcohol-related negative consequences. Psychology of Addictive Behaviors. 2010;24(2):342–348. doi: 10.1037/a0018020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C. Gender-Specific Misperceptions of College Student Drinking Norms. Psychology of Addictive Behaviors. 2004;18(4):334. doi: 10.1037/0893-164X.18.4.334. [DOI] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C. Social Norms Approaches Using Descriptive Drinking Norms Education: A Review of the Research on Personalized Normative Feedback. Journal of American College Health. 2006;54(4):213–218. doi: 10.3200/jach.54.4.213-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon D, Krull JL, Lockwood CM. Eqivalence of the mediation, confounding and suppression effect. Prevention Science. 2000;1(4):173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallett KA, Bachrach RL, Turrisi R. Are all negative consequences truly negative? Assessing variations among college students' perceptions of alcohol related consequences. Addictive Behaviors. 2008;33(10):1375–1381. doi: 10.10106/j.addbeh.2008.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKellar J, Austin J, Moos R. Building the first step: a review of low-intensity interventions for stepped care. Addiction Science & Clinical Practice. 2012;7(1):26. doi: 10.1186/1940-0640-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill JE, Carey KB, Reid AE, Carey MP. Drinking reductions following alcohol-related sanctions are associated with social norms among college students. Psychology of Addictive Behaviors. 2014;28(2):553–558. doi: 10.1037/a0034743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MB, Leffingwell T, Claborn K, Meier E, Walters S, Neighbors C. Personalized feedback interventions for college misuse: an update of Walters & Neighbors. Psychology of Addictive Behaviors. 2013;27(4):909–920. doi: 10.1037/a0031174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MB, Leffingwell TR. What do college student drinkers want to know? Student perceptions of alcohol-related feedback. Psychology of Addictive Behaviors. 2013;27(1):214–222. doi: 10.1037/a0031380. [DOI] [PubMed] [Google Scholar]
- Miller MB, Leffingwell TR, Claborn K, Meier E, Walters S, Neighbors C. Personalized Feedback Interventions for College Alcohol Misuse: An Update of Walters & Neighbors (2005) Psychology of Addictive Behaviors. 2012 doi: 10.1037/a0031174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Moyers TB, Ernst D, Amrhein P. Manual for the motivational interviewing skills code (MISC) Version 2.1. Unpublished Manual 2008 [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd. Guilford Press; 2002. [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari B, Barnett NP, Colby SM, Martens MP. A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. Journal of Consulting & Clinical Psychology. 2012;80(5):876–886. doi: 10.1037/a0028763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Dillard AJ, Lewis MA, Bergstrom RL, Neil TA. Normative Misperceptions and Temporal Precedence of Perceived Norms and Drinking. Journal of Studies on Alcohol. 2006;67(2):290–299. doi: 10.15288/jsa.2006.67.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIAAA. National Institute on Alcohol Abuse and Alcoholism: A call to action: Changing the culture of drinking at U S colleges. Washington D.C.: National Institute of Health; 2002. [Google Scholar]
- Pabst A, Kraus L, Piontek D, Mueller S, Demmel R. Direct and indirect effects of alcohol expectancies on alcohol-related problems. Psychology of Addictive Behaviors. 2014;28(1):20–30. doi: 10.1037/a0031984. [DOI] [PubMed] [Google Scholar]
- Perkins HW, editor. The Social Norms Approach to Preventing School and College Age Substance Abuse. San Francisco: Jossey-Bass; 2003. [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Prince MA, Reid A, Carey KB, Neighbors C. Effects of normative feedback for drinkers who consume less than the norm: Dodging the boomerang. Psychol Addict Behav. 2014;28(2):538–544. doi: 10.1037/a0036402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray AE, Kim SY, White HR, Larimer ME, Mun EY, Clarke N, et al. Huh D. When Less Is More and More Is Less in Brief Motivational Interventions: Characteristics of Intervention Content and Their Associations With Drinking Outcomes. Psychology of Addictive Behaviors. 2014;28:1026–1040. doi: 10.1037/a0036593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Kahler CW, Strong DR, Colder CR. Development and preliminary validation of the young adult alcohol consequences questionnaire. Journal of Studies on Alcohol. 2006;67(1):169–177. doi: 10.15288/jsa.2006.67.169. [DOI] [PubMed] [Google Scholar]
- SAMHSA, S. A. a. M. H. S. A. Results from the 2012 national survey on drug use and health 2012 [Google Scholar]
- Scott-Sheldon LA, Terry DL, Carey KB, Garey L, Carey MP. Efficacy of expectancy challenge interventions to reduce college student drinking: A meta-analytic Review. Psychology of Addictive Behaviors. 2012 doi: 10.1037/a0027565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder TD, Dillow SA. Digest of Education Statistics. National Center for Education Statistics; 2012. [Google Scholar]
- Sobell MB, Sobell LC. Stepped care as a heuristic approach to the treatment of alcohol problems. Journal of Consulting & Clinical Psychology. 2000;68(4):573–579. doi: 10.1037/0022-006X.68.4.573. [DOI] [PubMed] [Google Scholar]
- Turner AP, Larimer ME, Sarason IG. Family risk factors for alcohol-related consequences and poor adjustment in fraternity and sorority members: exploring the role of parent-child conflict. J Stud Alcohol. 2000;61(6):818–826. doi: 10.15288/jsa.2000.61.818. [DOI] [PubMed] [Google Scholar]
- Turrisi R, Larimer ME, Mallett KA, Kilmer JR, Ray AE, Mastroleo NR, et al. Montoya H. A randomized clinical trial evaluating a combined alcohol intervention for high-risk college students. J Stud Alcohol Drugs. 2009;70(4):555–567. doi: 10.15288/jsad.2009.70.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Neighbors C. Feedback interventions for college alcohol misuse: what, why and for whom? Addictive Behaviors. 2005;30(6):1168–1182. doi: 10.1016/j.addbeh.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR, Field CA, Jouriles EN. Dismantling motivational interviewing and feedback for college drinkers: a randomized clinical trial. Journal of Consulting & Clinical Psychology. 2009;77(1):64–73. doi: 10.1037/a0014472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993-2001. Journal of American College Health. 2002;50:203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- White HR. Reduction of alcohol-related harm on United States college campuses: The use of personal feedback interventions. International Journal of Drug Policy. 2006;17(4):310–319. doi: 10.1016/j.drugpo.2006.02.006. [DOI] [Google Scholar]
- Wood MD, Capone C, Laforge R, Erickson DJ, Brand NH. Breif motivational intervention and alcohol expectancy challenge with heavy drinking college students: A randomized factorial study. Addictive Behaviors. 2007;32(11) doi: 10.1016/j.addbeh.2007.06.018. [DOI] [PubMed] [Google Scholar]