Abstract
A substantial minority of people dropout of cognitive behavioral therapies (CBT) for posttraumatic stress disorder (PTSD). There has been considerable research investigating who drops out of PTSD treatment, however, the question of dropout occurs has received far less attention. The purpose of the current study was to examine when individuals drop out of CBT for PTSD. Women participants (N = 321) were randomized to one of several PTSD treatment conditions. The conditions included Prolonged Exposure (PE), Cognitive Processing Therapy (CPT), CPT-cognitive only (CPT-C), and written accounts (WA). Survival analysis was used to examine temporal pattern of treatment dropout. Thirty-nine percent of participants dropped out of treatment, and those that dropped out tended to do so by mid treatment. Moreover, the pattern of treatment dropout was consistent across CBT conditions. Additional research is needed to examine if treatment dropout patterns are consistent across treatment modalities and settings.
Keywords: treatment dropout, posttraumatic stress disorder, cognitive behavioral therapy
Significant advances in the treatment of posttraumatic stress disorder (PTSD) have been made over the past 30 years. Several evidence-based treatments for PTSD have been identified (e.g., Institute of Medicine, 2007; VA/DOD, 2010), which includes Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT). Despite the effectiveness of these treatments, a substantial minority of individuals drop out of PTSD treatment (e.g., Hembree et al., 2003; Imel, Laska, Jakupcak, & Simpson, 2013). Even within the Department of Veterans Affairs (VA), the largest PTSD treatment provider, only one quarter of newly diagnosed veterans who initiate psychotherapy for PTSD complete eight or more sessions (Spoont, Murdoch, Hodges, & Nugent, 2010). PTSD treatment dropout is also a significant problem among military service personnel returning from combat missions (Hoge et al., 2014). Hoge and colleagues describe the PTSD treatment dropout problem as a “call to action” (p. 1002) to improve treatment engagement and retention.
Treatment dropout is a concern for all psychiatric conditions but it is a particular problem for PTSD. Although the average dropout rate for PTSD treatment is similar to anxiety and depression disorders (e.g., Aderka et al., 2011; Hans & Hiller, 2013; Hofmann & Suvak, 2006; Keijers, Kapman, Hoogduin, 2001), the average rate is misleading because there is significant variability of dropout rates across studies (Imel et al., 2013; Swift & Greenberg, 2012). Swift and Greenberg (2012) observed a significant difference in treatment dropout rate as a function of treatment approach only for PTSD and depression. The significant variability in dropout rates between treatment approaches was not observed for ten other psychiatric disorders. Moreover, a recent meta-analysis of PTSD treatment dropout conducted by Imel, Laska, Jakupcak, and Simpson (2013) indicated that trauma-focused treatment, such as PE and CPT, had substantially higher dropout rates (i.e., 36%) relative to non-trauma focused treatments (i.e., Present Centered Treatment, 18%). Thus, treatment dropout rates in evidence-based treatments for PTSD is notably higher than dropout rates observed for other treatment approaches as well as other psychiatric conditions. What is not known is why dropout rates are elevated in cognitive behavioral treatment (CBT) for PTSD. A number of studies have examined who drops out of treatment, although inconsistent findings have emerged. Some studies have found that younger age (Cloitre, Stovall-McClough, Miranda, & Chemtob, 2004), lower intelligence, less education (Rizvi, Vogt, & Resick, 2009), higher levels of anger at baseline (Foa, Riggs, Massie, Yarczower, 1995), and trauma event occurring in past year (Iverson et al., 2011) are risk factors for treatment dropout. Findings from other studies have not supported these risk factors (e.g., van Minnen, Arntz, Keijers, 2002).
To understand why people dropout of CBT for PTSD we must first know when the dropouts occur. Different factors may influence why people drop out early versus late in the course of treatment. For instance, individuals may drop out late in the course of treatment because they have achieved clinically significant improvement, and consequently do not feel the need to complete additional treatment sessions. This possibility was underscored by findings of van Minnen and Foa (2006) who found that participants receiving the 12 session PE protocol needed an average of 6.8 sessions in order to achieve a 50% reduction in PTSD symptoms from their pre-treatment PTSD symptom score. Alternatively, avoidance behavior may account for individuals dropping out early in the course of CBT for PTSD given the focus on confronting the trauma memory in these treatments. Better understanding the time course of PTSD treatment dropout is an important step in improving treatment engagement and retention rates.
The primary goal of the current study is to investigate when individuals drop out of CBT for PTSD. Treatment dropout is defined in psychotherapy research studies as dropping out after a participant has been randomized to a condition (Schnurr, 2007). This definition of treatment dropout provides the most unbiased estimate of a treatments’ benefit. However, other definitions have been used, such as attending a certain number of sessions for a given treatment protocol (e.g., 75%), and dropping out of treatment after the first session (Foa et al., 2005; Resick et al., 2002, 2008). Although there can be advantages to using different definitions, in this study we use the recommended definition (Schnurr, 2007) in order to best capture PTSD treatment dropouts.
To address investigate CBT for PTSD dropout we used two large randomized controlled trials conducted by Resick and her colleagues (2002, 2008). In the first study, participants were randomized to CPT, PE, or a minimal attention control condition (MA). In the second study participants were assigned to CPT, CPT-cognitive only condition (CPT-C), or written accounts (WA) condition, which is a component of CPT that involves writing about the trauma account, reading it to the therapist and reading it to oneself daily.1 Based on the limited information available on timing of treatment dropout (Wang et al., 2005), we expected that most participants who drop out of treatment would do so early in the course of treatment. We also anticipated that the time course of treatment dropout would be consistent across treatment conditions given that all treatments studied were a cognitive behavioral trauma-focused approach.
Method
Participants
Participants were 321 women who met study eligibility criteria for one of two PTSD randomized controlled trials (see Resick et al., 2002; Resick et al., 2008) and were part of the intention-to-treat (ITT) sample. Inclusion criteria for the treatment studies included being at least 18 years of age, female, and a diagnosis of PTSD related to an interpersonal violence event. Exclusion criteria included current psychosis, current suicidal intent, current substance use dependence diagnosis, illiteracy, a current abusive relationship, or a dangerous situation such as being stalked. Participants were recruited from the St. Louis, Missouri area. The combined sample had a mean age of 33.60 (SD = 11.28), a mean of 14.10 (SD = 2.57) years of education, and was diverse in terms of racial background (67% Caucasian, 29% African American, and 4% of other racial backgrounds). The mean baseline PTSD symptom severity, as measured by the Clinician Administered PTSD Scale (CAPS; Blake et al., 1995) for the women who completed treatment (72.76, SD = 18.75) and for women who did not complete treatment (73.00, SD = 19.31) did not significantly differ. The average time since the index trauma event occurred was 135.06 months. There were no significant differences between participants in the two studies in terms of demographic characteristics between treatment completers and non-completers, with treatment completion defined as attending every session of the treatment condition for which they were assigned. Additionally, there were no significant differences between women who presented to the first treatment session and those who did not.
Measures
Clinician-Administered PTSD Scale-DSM-IV (CAPS; Blake et al., 1995)
The CAPS is a gold standard 17-item clinician administered measure for PTSD that corresponds with the PTSD diagnostic criteria outline in the Diagnostic Statistical Manual of Mental Disorders-IV (DSM-IV, American Psychiatric Association, 1994). It has excellent psychometric properties (Blake et al., 1995; Weathers, Keane, & Davidson, 2001) and produces diagnosis and a total severity score, composed of both symptom frequency and intensity scores, which are separately rated on 0 (low) to 4 (high) scales. The CAPS was used in the current study to assess study eligibility and to provide a baseline measure of PTSD symptom severity.
Standardized Trauma Interview (Resick et al., 1988)
The standardized trauma interview is a clinician-administered measure that covers domains such as demographic information, information about the trauma, trauma history, social support, and treatment history. For this study, we used this interview to investigate participant characteristics of demographic information and information regarding time since the index trauma (in months).
Procedure
Both studies were conducted in accordance with approved procedures from the Institutional Review Board of the University of St. Louis, Missouri. Participants were recruited and participated in a brief telephone screen prior to being scheduled for an assessment. Written informed consent was obtained before starting the initial assessment interview. Following completion of the baseline assessment session, eligible participants were randomly assigned to one of the treatment conditions included in the respective study. As previously noted, consistent with the ITT approach (Schnurr, 2007), treatment drop out in this study was defined as dropping out after randomizing, which includes participants who dropped out prior to the first treatment session as well as participants who dropped out after the start of treatment. Substantial efforts were made to retain all randomized participants. If a participant did not attend a session, the therapist would call them at various times during the day and evening until they were reached. If a participant did not respond to telephone calls, a letter was sent to inquire about a desire to continue treatment and request the participant contact their therapist. When phones were disconnected, a letter was immediately sent and the therapist or research assistant would wait no longer than two weeks before attempting to re-contact the participant by phone.
In the Resick and colleagues study (2002) women were first randomly assigned to PE, CPT, or minimal attention (MA; Resick et al., 2002). CPT and PE were both conducted twice weekly for six weeks for a total of 13 hours of treatment.2 PE included a total of nine sessions with the first session consisting of 60 minutes and the remaining eight sessions requiring 90 minutes per session. CPT consisted of 12 sessions with each session requiring 60 minutes, except for sessions 4 and 5, which were 90 minutes in duration. Participants assigned to the MA condition were informed that treatment would be provided after a six week waiting period. A clinician contacted the MA participants every 2 weeks to ensure no emergency services were needed. The MA participants were then randomly assigned to either PE or CPT following the waiting period. These participants are included in the current study within the PE and CPT conditions.
The Resick et al. study (2008) was a dismantling study of CPT. That is, the full protocol of CPT was compared with its components, CPT-C or WA. Treatment consisted of a total of 12 hours of treatment for each condition. CPT and CPT-C were 12, twice weekly, 60-minute sessions. WA consisted of two, 60-minute sessions in the first week, followed by 2-hour weekly sessions for the remaining five sessions.
Data Analysis Plan
We used discrete-time survival analysis as described by Singer and Willett (2003) to examine temporal patterns of dropout. All analyses were conducted using SPSS, Version 22. For all analyses, randomization to treatment condition at the baseline assessment was used as the beginning of time and treatment session was used as the metric of time. Life tables were first constructed to quantify the number of individuals who dropped out of treatment at each treatment session as well the corresponding hazard and survival proportions at each treatment session. Life tables were constructed for each of the four treatment conditions (PE, CPT, CPT-C, WA) and for the entire sample collapsed across treatment conditions. Because reasons for dropping out before the first treatment session may differ from reasons for dropping during treatment, Chi-squared tests were used to evaluate whether there were differences among the four treatment conditions in the proportion of participants who presented for the first treatment session or the proportion of participants who completed a full course of treatment.
Results
Dropout across Treatment Conditions
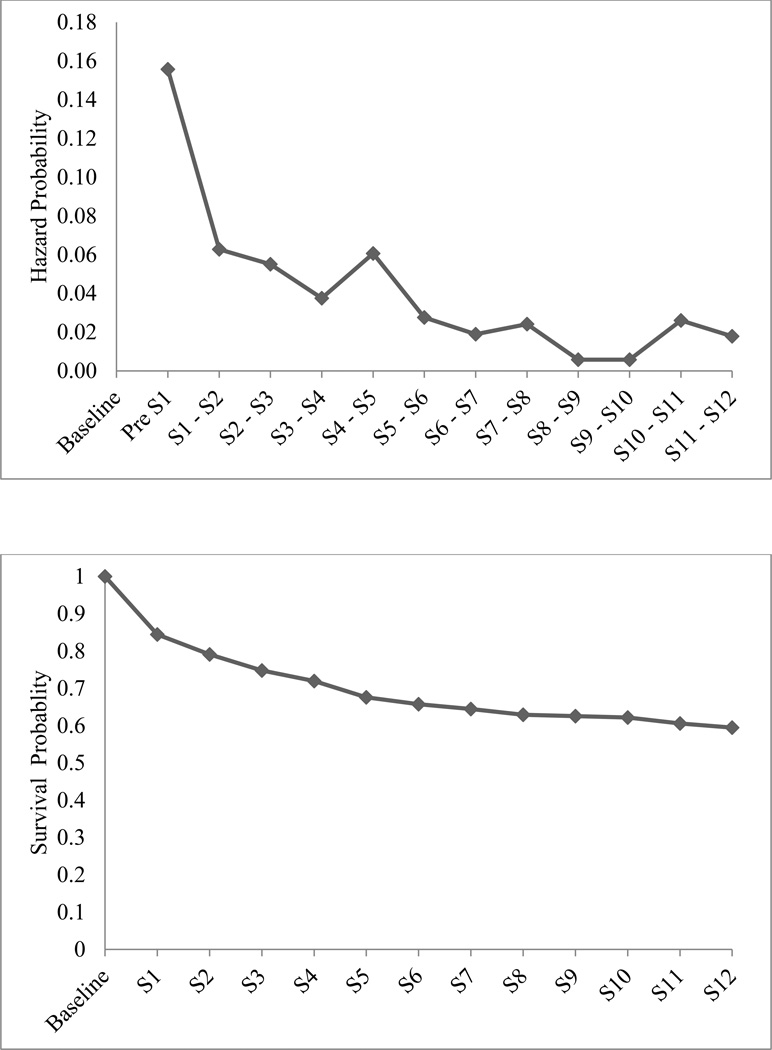
We began by constructing a life table to describe when individuals dropped out of treatment by collapsing across the four treatment conditions. Table 1 provides results at each session for the number of participants who dropped out, the hazard proportion, the survival proportion, the cumulative survival proportion, and the number of individuals who completed the full course of treatment. Plots of the hazard and survival proportions across time are presented in Figure 1. Results indicate that, across treatment conditions, the majority of participants (61%) completed the full course of treatment. Notably, the greatest risk of attrition across treatment conditions was prior to attending the first treatment session, with 16% of participants dropping out prior to the first treatment session. As expected, the majority of participants (83%) who dropped out did so within the first half of treatment (e.g., by session 5). However, there was no clear time point during which dropouts were most likely to occur after presenting for the first treatment session.
Table 1.
Life table indicating the number of individuals remaining in treatment, dropping out of treatment, completing treatment, hazard rates, survival rates, and cumulative survival rates across four treatment conditions
| Time | Interval | # In treatment |
# Dropped Out |
# Completed Treatment |
Proportion Dropped Out (Hazard) |
Proportion Remaining in Treatment (Survival) |
Cumulative Proportion Remaining in Treatment |
|---|---|---|---|---|---|---|---|
| 0 | Randomization | 321 | -- | -- | -- | 1.00 | 1.00 |
| 1 | Pre S1 | 321 | 50 | 0 | .16 | .84 | .84 |
| 2 | S1 – S2 | 271 | 17 | 0 | .06 | .94 | .79 |
| 3 | S2 – S3 | 254 | 14 | 0 | .06 | .94 | .75 |
| 4 | S3 – S4 | 240 | 9 | 0 | .04 | .96 | .72 |
| 5 | S4 – S5 | 231 | 14 | 0 | .06 | .94 | .68 |
| 6 | S5 – S6 | 217 | 6 | 0 | .03 | .97 | .66 |
| 7 | S6 – S7 | 211 | 4 | 0 | .02 | .98 | .64 |
| 8 | S7 – S8 | 207 | 5 | 30 | .02 | .98 | .63 |
| 9 | S8 – S9 | 172 | 1 | 0 | .01 | .99 | .63 |
| 10 | S9 – S10 | 171 | 1 | 55 | .01 | .99 | .62 |
| 11 | S10 – S11 | 115 | 3 | 0 | .03 | .97 | .61 |
| 12 | S11 – S12 | 112 | 2 | 110 | .02 | .98 | .59 |
Note: Thirty individuals completed a full course (seven sessions) of the WA treatment protocol, 55 individuals completed a full course (nine sessions) of the PE treatment protocol, 29 individuals completed a full course (twelve sessions) of the CPT-C treatment protocol, and 81 individuals completed a full course (twelve sessions) of the CPT/CPT-C treatment protocol.
CPT = Cognitive Processing Therapy, CPT-C = Cognitive Processing Therapy, Cognitive Only, PE = Prolonged Exposure, WA = Written Accounts
Figure 1.
Top graph: Hazard function indicating proportion of individuals who dropped out from treatment at different treatment intervals. Bottom graph: Survival function indicating the cumulative proportion of individuals who remained in treatment at different sessions. Both graphs include individuals from all four treatment conditions examined (CPT, CPT-C, PE, & WA).
Dropout within Treatment Conditions
A second life table was constructed to examine if patterns of dropout were different for the four treatment conditions (see Table 2). Results were consistent across treatment conditions. The median/modal survival times for the treatment conditions were 12 sessions (CPT and CPT-C), 9 sessions (PE), and 7 sessions (WA). These results indicate that the majority of participants in each of the four treatment conditions completed a full course of treatment, with the proportion of treatment completers varying from 60% in WA to 63% in PE. The greatest risk of dropout was prior to the first treatment session for all four treatment conditions, with 14–17% of individuals failing to return for their first treatment session. In addition, the majority of participants who dropped out did so within the first half of the treatment course. Importantly, findings revealed that there were no significant differences between the four treatment conditions in whether individuals returned for their first treatment session (χ2 (df = 3) = .39, p = .94) or whether individuals completed a full course of treatment (χ2 (df = 3) = .22, p = .97). Taken together, these findings suggest approximately one-third of individuals randomized to treatment dropout before completing the course of treatment. Importantly, the majority of dropouts occur in the first half of treatment, and a substantial proportion of individuals dropped out prior to the first treatment session across all treatment conditions.
Table 2.
Life table indicating the number of individuals remaining in treatment, dropping out of treatment, hazard rates, survival rates, and cumulative survival rates within each of the four treatment conditions (CPT, CPT-C, PE, WA)
| Treatment | Time | Interval | # In treatment |
# Dropped Out |
Proportion Dropped Out (Hazard) |
Proportion Remaining in Treatment (Survival) |
Cumulative Proportion Remaining in Treatment |
|---|---|---|---|---|---|---|---|
| CPT | 0 | Baseline | 136 | -- | -- | 1.00 | 1.00 |
| 1 | Pre S1 | 136 | 20 | 0.15 | 0.85 | 0.85 | |
| 2 | S1 – S2 | 116 | 7 | 0.06 | 0.94 | 0.80 | |
| 3 | S2 – S3 | 109 | 4 | 0.04 | 0.96 | 0.77 | |
| 4 | S3 – S4 | 105 | 4 | 0.04 | 0.96 | 0.74 | |
| 5 | S4 – S5 | 101 | 7 | 0.07 | 0.93 | 0.69 | |
| 6 | S5 – S6 | 94 | 2 | 0.02 | 0.98 | 0.68 | |
| 7 | S6 – S7 | 92 | 3 | 0.03 | 0.97 | 0.65 | |
| 8 | S7 – S8 | 89 | 4 | 0.04 | 0.96 | 0.63 | |
| 9 | S8 – S9 | 85 | 1 | 0.01 | 0.99 | 0.62 | |
| 10 | S9 – S10 | 84 | 1 | 0.01 | 0.99 | 0.61 | |
| 11 | S10 – S11 | 83 | 1 | 0.01 | 0.99 | 0.60 | |
| 12 | S11 – S12 | 82 | 1 | 0.01 | 0.99 | 0.60 | |
| CPT-C | 0 | Baseline | 47 | -- | -- | 1.00 | 1.00 |
| 1 | Pre S1 | 47 | 8 | 0.17 | 0.83 | 0.83 | |
| 2 | S1 – S2 | 39 | 4 | 0.10 | 0.90 | 0.74 | |
| 3 | S2 – S3 | 35 | 1 | 0.03 | 0.97 | 0.72 | |
| 4 | S3 – S4 | 34 | 1 | 0.03 | 0.97 | 0.70 | |
| 5 | S4 – S5 | 33 | 0 | 0.00 | 1.00 | 0.70 | |
| 6 | S5 – S6 | 33 | 1 | 0.03 | 0.97 | 0.68 | |
| 7 | S6 – S7 | 32 | 0 | 0.00 | 1.00 | 0.68 | |
| 8 | S7 – S8 | 32 | 0 | 0.00 | 1.00 | 0.68 | |
| 9 | S8 – S9 | 32 | 0 | 0.00 | 1.00 | 0.68 | |
| 10 | S9 – S10 | 32 | 0 | 0.00 | 1.00 | 0.68 | |
| 11 | S10 – S11 | 32 | 2 | 0.06 | 0.94 | 0.64 | |
| 12 | S11 – S12 | 30 | 1 | 0.03 | 0.97 | 0.62 | |
| PE | 0 | Baseline | 88 | -- | -- | 1.00 | 1.00 |
| 1 | Pre S1 | 88 | 15 | 0.17 | 0.83 | 0.83 | |
| 2 | S1 – S2 | 73 | 3 | 0.04 | 0.96 | 0.80 | |
| 3 | S2 – S3 | 70 | 5 | 0.07 | 0.93 | 0.74 | |
| 4 | S3 – S4 | 65 | 3 | 0.05 | 0.95 | 0.70 | |
| 5 | S4 – S5 | 62 | 4 | 0.06 | 0.94 | 0.66 | |
| 6 | S5 – S6 | 58 | 1 | 0.02 | 0.98 | 0.65 | |
| 7 | S6 – S7 | 57 | 1 | 0.02 | 0.98 | 0.64 | |
| 8 | S7 – S8 | 56 | 1 | 0.02 | 0.98 | 0.63 | |
| 9 | S8 – S9 | 55 | 0 | 0.00 | 1.00 | 0.63 | |
| WA | 0 | Baseline | 50 | -- | -- | 1.00 | 1.00 |
| 1 | Pre S1 | 50 | 7 | 0.14 | 0.86 | 0.86 | |
| 2 | S1 – S2 | 43 | 3 | 0.07 | 0.93 | 0.80 | |
| 3 | S2 – S3 | 40 | 4 | 0.10 | 0.90 | 0.72 | |
| 4 | S3 – S4 | 36 | 1 | 0.03 | 0.97 | 0.70 | |
| 5 | S4 – S5 | 35 | 3 | 0.09 | 0.91 | 0.64 | |
| 6 | S5 – S6 | 32 | 2 | 0.06 | 0.94 | 0.60 | |
| 7 | S6 – S7 | 30 | 0 | 0.00 | 1.00 | 0.60 | |
Note CPT = Cognitive Processing Therapy, CPT-C = Cognitive Processing Therapy-Cognitive Only, PE = Prolonged Exposure, WA = Written Accounts
Discussion
Findings from this study indicate that the majority of women who dropped out of treatment did so within the first half of the course of treatment. Notably, a large proportion of individuals (16%) dropped out prior to the first treatment session and, before receiving any treatment. This pattern of treatment attrition is consistent with the rate reported for trauma-focused treatments (e.g., Imel et al., 2013). It is also consistent with the observation that veterans and active duty military personnel seeking PTSD treatment drop out of treatment prior to receiving an adequate course of treatment (i.e., at least 6 sessions; Hoge et al., 2014; Wang et al., 2005).
The observation of a substantial percentage of individuals dropping out of treatment before the first treatment session is important as different factors may underlie not starting a treatment relative to starting treatment and then dropping out. This pattern is similar to routine care settings that have an initial intake assessment before being assigned a treatment provider and underscore the importance of investigating not only dropouts that occur after treatment has started but dropouts that occur between an initial intake appointment and the start of treatment. If the initial intake appointment was included in studies examining dropouts, the rates of dropout may be substantially greater than what has been reported.
Although most people who dropped out did so within the first half of the treatment course (by session 5), a smaller percentage of participants dropped out in the second half of treatment. It is possible that these individuals dropped out of treatment because they had a clinically significant reduction in PTSD symptoms and did not feel the need to attend additional sessions. Ideally, we would have tested this possibility by examining self-reported PTSD symptom severity completed during the treatment sessions. However, both studies had participants complete the PTSD measure at every other treatment session, starting with the second treatment session. Consequently, we were not able to examine PTSD symptom severity for participants who dropped out of treatment prior to the second session and for many of the other participants we did not have self-report data from the session immediately prior to dropout.
Overall, it is important for future studies to investigate reasons for dropout, including dropout that occurs between initial intake or assessment appointment and the first treatment session. There are likely to be multiple factors that influence dropout including time availability given other life demands (e.g., work, child care), transportation difficulties, and stigma associated with receiving mental health care services, and initial reactions to the clinic setting and providers. It is also important to acknowledge that treatment dropout rates may be lower in psychotherapy studies given the resources available in these studies to track and retain participants. Such resources are not typical in clinical care settings.
There are a number of strengths of the current study, including examination of different trauma-focused treatment conditions, a large sample of participants, and diagnostic interviews at the initial assessment session. There are limitations of the study that are important to consider. First, only women with PTSD related to interpersonal trauma were included so the findings may not generalize to other samples. In addition, the findings may not generalize to clinical practice because the motivation to present to a treatment study may differ from what is observed in clinical practice. Additionally, as previously described, assessments collected at every other treatment session prevented the analysis of end state functioning at the time of dropout. Lastly, due to insufficient power we were not able to investigate differences in individual characteristics between individuals who dropped out before treatment, by mid treatment, and those who completed treatment.
The findings of this study provide important information about the time course of drop out from trauma-focused treatment. It will be important to examine whether similar patterns of treatment dropout are observed with different trauma samples and samples of men, as well as other treatment approaches for PTSD, such as Present Centered Therapy. It will also be important to examine whether patterns for treatment dropout differ in clinical practice. Gaining a better understanding of when people drop out of PTSD treatment, through the use of qualitative and quantitative measures, is critical to improving PTSD treatment engagement and retention.
Acknowledgments
This work was supported by National Institute of Mental Health Grant NIH-1 R01-MH51509 and National Institute of Mental Health Grant NIH-2 R01-MH51509 awarded to Patricia A. Resick while at the University of Missouri–St. Louis. Drs. Gutner and Baker were supported by a National Institute of Mental Health grant (T32MH019836-15A2) awarded to Terence M. Keane. Dr. Gutner was also supported by a National Institute of mental Health Grant (1K23MH103396-01A1) awarded to Cassidy A. Gutner.
Footnotes
Although treatment dropout rate was reported in the primary papers (2002, 2008), the time course of treatment dropout was not reported. Moreover, individuals who dropped out after randomization but before the first treatment session were not included in the primary papers (2002, 2008).
References
- Aderka IM, Anholt GE, van Balkom AJ, Smits JH, Hermesh H, Hofmann SG, van Oppen P. Differences between early and late drop-outs from treatment for obsessive–compulsive disorder. Journal of Anxiety Disorders. 2011;25(7):918–923. doi: 10.1016/j.janxdis.2011.05.004. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, D.C.: Author; 1994. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stovall-McClough KC, Miranda R, Chemtob CM. Therapeutic alliance, negative mood regulation, and treatment outcome in child abuse-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2004;72:411–416. doi: 10.1037/0022-006X.72.3.411. [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Massie ED, Yarczower M. The impact of fear activation and anger on the efficacy of exposure treatment for post-traumatic stress disorder. Behavior Therapy. 1995;26:487–499. [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, Feeny NC, et al. Randomized trial of Prolonged Exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73:953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Hans E, Hiller W. Effectiveness of and dropout from outpatient cognitive behavioral therapy for adult unipolar depression: A meta-analysis of nonrandomized effectiveness studies. Journal of Consulting and Clinical Psychology. 2013;81(1):75–88. doi: 10.1037/a0031080. [DOI] [PubMed] [Google Scholar]
- Hembree EA, Foa EB, Dorfan NM, Street GP, Kowalski J, Tu X. Do patients drop out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress. 2003;16(6):555–562. doi: 10.1023/B:JOTS.0000004078.93012.7d. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Suvak M. Treatment attrition during group therapy for social phobia. Journal of Anxiety Disorders. 2006;20:961–972. doi: 10.1016/j.janxdis.2006.03.005. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Grossman SH, Aucherlonie JL, Riviere LA, Milliken CS, Wilk JE. PTSD treatment for soldiers after combat deployment: Low utilization of mental health care and reasons for dropout. Psychiatric Services. 2014;65:997–1004. doi: 10.1176/appi.ps.201300307. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Treatment of posttraumatic stress disorder: An assessment of the evidence. Washington (DC): National Academies Press; 2007. [Google Scholar]
- Iverson KM, Gradus JL, Resick PA, Suvak MK, Smith KF, Monson CM. Cognitive–behavioral therapy for PTSD and depression symptoms reduces risk for future intimate partner violence among interpersonal trauma survivors. Journal of consulting and clinical psychology. 2011;79(2):193–202. doi: 10.1037/a0022512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keijsers GP, Kampman M, Hoogduin CA. Dropout prediction in cognitive behavior therapy for panic disorder. Behavior Therapy. 2001;32(4):739–749. [Google Scholar]
- Resick PA, Galovski TE, Uhlmansiek MO, Scher CD, Clum G, Young-Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting & Clinical Psychology. 2008;76(2):243–258. doi: 10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Jordan CG, Girelli SA, Hutter CK, Marhoefer-Dvorak S. A comparative outcome study of group behavior therapy for sexual assault victims. Behavior Therapy. 1988;19:385–401. [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting & Clinical Psychology. 2002;70(4):867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, Vogt DS, Resick PA. Cognitive and affective predictors of treatment outcome in cognitive processing therapy and prolonged exposure for posttraumatic stress disorder. Behaviour Research and Therapy. 2009;47(9):737–743. doi: 10.1016/j.brat.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP. The rocks and hard places in psychotherapy outcome research. Journal of traumatic stress. 2007;20(5):779–792. doi: 10.1002/jts.20292. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. USA: Oxford University Press; 2003. [Google Scholar]
- Spoont M, Murdoch M, Hodges J, Nugent S. Treatment receipt by veterans after a PTSD diagnosis in PTSD, mental health, or general medical clinics. Psychiatric Services. 2010;61(1):58–63. doi: 10.1176/ps.2010.61.1.58. [DOI] [PubMed] [Google Scholar]
- Swift JK, Greenberg RP. Premature discontinuation in adult psychotherapy: A meta-analysis. Journal of Consulting and Clinical Psychology. 2012;80(4):547–559. doi: 10.1037/a0028226. [DOI] [PubMed] [Google Scholar]
- VA/DoD Management of Post-Traumatic Stress Working Group (Internet) Washington (DC): Department of Veterans Affairs, Department of Defense; 2010. VA/DOD clinical practice guideline for management of post-traumatic stress. Available from: http://www.healthquality.va.gov/ptsd/ptsd_full.pdf. [Google Scholar]
- Van Minnen A, Arntz A, Keijsers GPJ. Prolonged exposure in patients with chronic PTSD: predictors of treatment outcome and dropout. Behaviour Research and Therapy. 2002;40(4):439–457. doi: 10.1016/s0005-7967(01)00024-9. [DOI] [PubMed] [Google Scholar]
- Van Minnen A, Foa EB. The effect of imaginal exposure length on outcome of treatment for PTSD. Journal of Traumatic Stress. 2006;19(4):427–438. doi: 10.1002/jts.20146. [DOI] [PubMed] [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. JAMA Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13(3):132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]