Abstract
Objective
The purpose of this in vitro study was to evaluate and compare the fracture resistance and fracture mode of extensive indirect inlay and onlay composite resin restorations performed for endodontically treated premolars.
Materials and methods
A total of 55 extracted maxillary premolars were randomly divided into four groups. The first group (n = 15) remained untreated to serve as a positive control; the second group (n = 15) was endodontically treated with inlay cavities prepared and restored with indirect composite inlay restorations; the third group (n = 15) was also endodontically treated with onlay cavities prepared and restored with indirect composite onlay restorations; and the fourth group (n = 10) was endodontically treated with mesio-occlusodistal (MOD) cavities prepared and left unrestored to serve as negative controls. Dual cure indirect composite resin was used to fabricate the inlay and onlay restorations performed for the second and third groups, respectively. All teeth were subjected to compressive axial loading test using a metal ball (6 mm in diameter) in a universal testing machine (Instron 1195) with a cross-head speed of 0.5 mm/min until a fracture occurred. Statistical analysis of fracture resistance and fracture mode were performed with analysis of variance (ANOVA) (α = 0.05) and Kruskal–Wallis (α = 0.05) tests, respectively.
Results
For the four treatment groups, the mean fracture resistance values were 1326.9 N, 1500.1 N, 1006.1 N, and 702.7 N, respectively. Statistical analyses showed no significant differences between the mean fracture resistance of the intact tooth group and the inlay restoration group (p > 0.05), while significant differences were observed between the mean fracture resistance of all the other groups (p < 0.05). The Kruskal–Wallis test showed statistically significant differences between the fracture modes of the four groups.
Conclusion
Within the limitations of this study, endodontically treated teeth were successfully restored with indirect composite inlay and onlay restorations. However, the fractures that accompanied the inlay restorations were more severe and were unable to be restored.
Keywords: Fracture resistance, Composite, Inlay restoration, Onlay restoration, Endondontics
1. Introduction
Endodontic treatment is generally associated with reductions in the resilience and fracture resistance of the treated teeth (Reeh et al., 1989, Hansen et al., 1990). The primary factors for loss of tooth structure include dental caries, cavity preparation, endodontic access, and root canal preparation (Huang et al., 1992, Papa et al., 1994). Moreover, the depth and design for cavity preparations are critical factors for fracture resistance. When a cavity preparation involves a greater depth, this typically generates stress in the enamel (Hansen and Asmussen, 1990, Lin et al., 2001). One of the most important factors for maintaining the stability of dentin is the remaining axial thickness (Hansen and Asmussen, 1990). Preparation of an endodontic access cavity compromises the strength of a tooth, resulting in an increased susceptibility to fractures (Yamada et al., 2003, Plotino et al., 2008). Consequently, loss of dentin, as well as anatomic structures such as cusps, ridges, and an arched roof of the pulp chamber, may result in the fracture of tooth tissue after the final restoration (Trope et al., 1986, Reeh et al., 1989). Randow and Glantz (1986) previously reported that teeth have a protective feedback mechanism that is lost when pulp is removed, and this may also contribute to occurrence of tooth fractures. Mesio-occlusodistal (MOD) intracoronal preparations commonly result in the creation of elongated cusps (González-López et al., 2006), and these may reduce the original strength of tooth structures (Hannig et al., 2005, Habekost et al., 2007).
After a root canal treatment (RCT), a reinforcing ferrule design for the restoration is commonly recommended to reduce fracture susceptibility (Steele and Johnson, 1999). Partial-veneer crowns that cover all cusps or laboratory-fabricated complete crowns are usually included in the restoration of the endodontically treated teeth. Recently, composite resin restorations or adhesive ceramic inlays that provide internal reinforcement of teeth without occlusal coverage have been advocated (Van Dijken, 2000, St-Georges et al., 2003, Hannig et al., 2005). However, these techniques do not guarantee a full restoration of the fracture toughness of a sound tooth (Costa et al., 1997). Studies have also shown that after endodontic treatment, teeth that are restored with bonded restorations are more resistant to fracture compared with those that are restored with silver amalgam (Oliveira et al., 1987, Wendt et al., 1987); yet, both bonded silver amalgam and bonded cast metal inlays have been recommended for the reinforcement of prepared teeth (Zidan and Abdel-Keriem, 2003).
Clinicians often prefer composite resin due to its excellent esthetic and mechanical properties, its ease of handling, and its reported ability to reinforce weakened dental structures (Bremer and Geurtsen, 2001). Although hybrid composite resins are mostly preferred for restoration of small- and medium-sized occlusal cavities, direct composite resin restorations are highly technique sensitive, presenting disadvantages related to polymerization shrinkage, postoperative sensitivity, and wear resistance (Ritter and Baratieri, 1999). Recent generation of indirect composite encourage using this material for a large cavity as an inlay or onlay restoration. However, the disadvantages associated with hybrid composite resins include postoperative sensitivity, polymerization shrinkage, and wear resistance (Ritter and Baratieri, 1999). Indirect composites have recently been generated and these have been recommended for inlays or onlay restorations of large cavities.
The purpose of this in vitro study was to evaluate and compare the fracture resistance and type of fractures that occur in endodontically treated premolars that receive extensive indirect inlays versus onlay composite resin restorations.
2. Materials and methods
A total of 55 intact human, caries-free, and recently extracted maxillary premolars that met orthodontic treatment requirements were obtained. All the teeth had two canals and the bucco-palatal dimension of the crowns ranged from 9 to 9.5 mm. The teeth were properly cleaned using sodium hypochlorite and any cracks were observed under magnification (×30) with a stereomicroscope (Stemi SV6; Carl Zeiss SpA, Arese, Italy). The teeth were stored in a 0.5% chloramine T solution until being randomly distributed into four different groups. For Group 1 (n = 15), the teeth received no cavity preparation or RCT in order to serve as positive controls. For Group 2 (n = 15), the teeth underwent RCT followed by inlay preparation and indirect composite inlay restoration. For Group 3 (n = 15), the teeth underwent RCT, onlay preparation, and indirect composite onlay restoration. For Group 4 (n = 10), the teeth underwent RCT and inlay preparation with no restoration to serve as negative controls. A single operator performed all the RCTs, the inlay and onlay preparations, and the restorations.
2.1. RCT
An access cavity was prepared for each tooth using a water-cooled, high-speed handpiece tool with a 2.3 mm round bur and 1.4 fissure bur (Komet, GEBR, Brasseler, Germany). Each canal orifice was enlarged with a Gates Glidden size III (JS Dental, Switzerland) and the canals were prepared with NiTi rotary instruments (ProTaper; Dentsply Maillefer, Ballaigues, Switzerland) until size 25 was reached. A root canal conditioner, Glyde (Dentsply Maillefer), was used to facilitate the canal preparations, and 6% sodium hypochlorite (Henry Schein, NY, USA) was used for canal irrigation. Finally, each canal was dried with paper points (Dentsply Maillefer) and were obturated with lateral condensed gutta-percha (Dentsply Maillefer) and Zinc Oxide Eugenol sealer (Dentsply Maillefer). Gutta-percha cones were cut to the level of the canal orifice and the access cavity were restored with temporal fillings.
After 24 h, each temporary filling was removed using a 1.4 fissure bur. Part of the gutta-percha was also removed (to the depth of 9 mm from the tip of the corresponding cusp) using Pesso-reamers (Dentsply Maillefer). Cavities were properly cleaned, were etched with 37% phosphoric acid for 15 s (Total etch, Ivoclar Vivadent, Liechtenstein), and then were irrigated with water for 10 s and dried gently. Bond (Excite, Ivoclar Vivadent) was applied for 20 s and was cured for 15 s. Dual-cure composite material (MultiCore, Ivoclar Vivadent) was applied to fill both canal orifices and cavities and was cured for 40 s.
3.2. Cavity preparations
Using square-shape metal containers (40 × 20 × 20 mm3), the root of the specimens were embedded perpendicularly up to 2 mm below the cement-enamel junction (CEJ) using a self-curing acrylic resin (Unifast II, GC). For the MOD cavities that were to receive inlay restorations, these teeth were prepared for RCT with a water-cooled hand-piece and a bur kit (Komet, GEBR) that was replaced after every five preparations. To determine the width of the cavities to be treated, the distance between the two cusp tips of each tooth were measured using a digital caliper (Mitutoyo, Corp, Kawasaki, Japan). Each cavity was subsequently prepared with an equal distance between the two cusps. Cavity dimensions are shown in Fig. 1.
Figure 1.
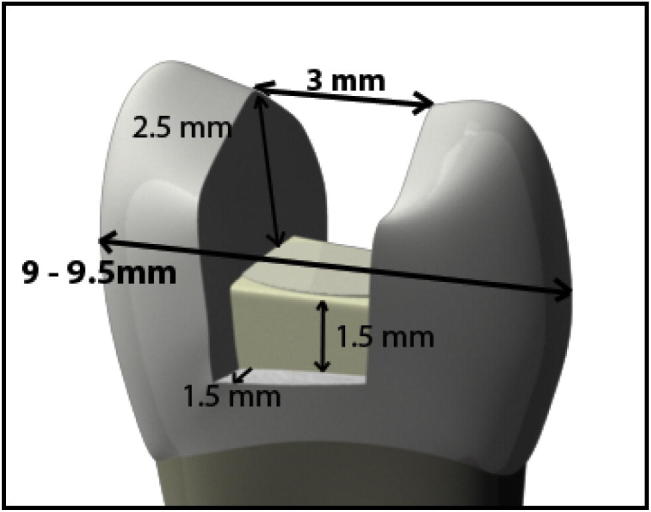
Dimensions of inlay cavity preparation.
After all teeth were prepared, 15 teeth were randomly selected to be prepared for onlay restorations (Group 3). Buccal and palatal inclinations of the palatal cusps were reduced evenly by 1.5 mm using a 1.4 fissure bur. For the buccal cusps, a 1 mm reduction was performed following cusp inclinations (Fig. 2). To control the reduction, putty index (SwissTEC, Coltène/Whaledent Inc., Switzerland) was fabricated for each tooth and three grooves were prepared at the beginning of each cusp reduction.
Figure 2.
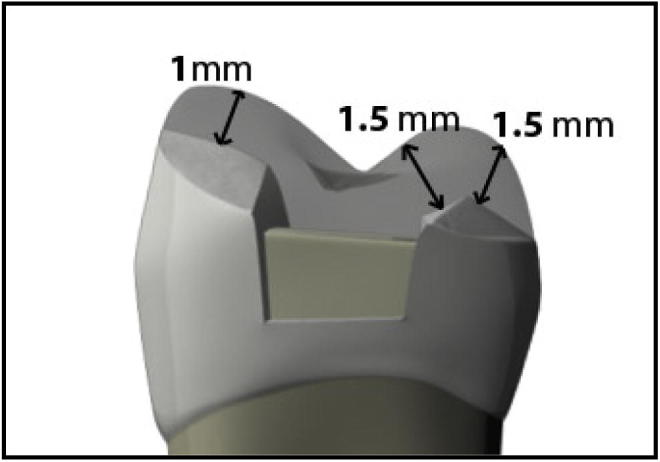
Dimensions of cusps reduction for onlay preparation.
3.3. Impression and restoration methods
Impressions were obtained with polyvinyl silicon light body and putty (SwissTEC) for each preparation using custom-made impression trays. The impressions were then poured with a vacuum-mixed die stone (SHERA Werkstoff-Technologie GmbH, Lemförde, Germany). After the die stones were completely set, the dies were carefully separated and evaluated to ensure that they were free of air bubbles and deformities. A die spacer (Sculpture plus die spacer, Jeneric/Pentron Inc., Wallingford, CT, USA) was applied to each cavity. Inlay and onlay restorations were built incrementally using indirect light-cured composite materials (Adoro SR, Ivoclar Vivadent, Liechtenstein). According to the manufacturer’s instructions, Light cure (FLASH lite 1401, LED Discus Dental, USA) was applied every 2 mm until complete build-up of the restoration was achieved. A glaze was applied on top of each restoration. To complete the curing process, the restorations were placed in a light cure furnace (Cure-lite plus, Jeneric/Pentron Inc.) for 2 min. The restorations were further polymerized in a heat polymerization oven (Sculpture FiberKor Curing Unit, Jeneric/Pentron Inc.) at 110 °C for 20 min.
The cementation procedure was completed by using dual-cured resin cement (Multilink, Ivoclar Vivadent, Liechtenstein) according to the manufacturer’s instructions. The fitting surface of each restoration was treated with a primer (Monobond S, Ivoclar Vivadent) for 60 s. Each cavity was then treated with 37% phosphoric acid for 30 s on the enamel, and for 15 s on the dentine, followed by application of a bonding agent (Excite, Ivoclar Vivadent) onto the cavity for 15 s. Finally, resin cement (Multilink, Ivoclar Vivadent) was mixed and applied on the fitting surface of each restoration before the restorations were placed in the cavities. Excess cement was removed with a brush and was cured for 60 s.
3.4. Fracture test
After each restoration, the specimens were stored in distilled water at 37 °C for 24 h prior to fracture testing. For fracture testing, each specimen was positioned to maintain the occlusal surface perpendicular to the loading axis. All specimens were submitted to axial compression in an Instron universal testing machine (Instron 1195, Instron Ltd. High Wycombe, UK) using an 6 mm diameter steel ball at a continuous loading speed of 0.5 mm per minute until a fracture occurred. The steel ball contacted the buccal and lingual inclined cuspal planes of the teeth in Groups 1 and 4. However, for the teeth in Groups 2 and 3, the steel ball connected to the three surfaces; buccal inclined cuspal plane, lingual inclined cuspal plane, and the restoration surface.
To evaluate the mode of fracture, a classification system proposed by Burke et al. (1993) was modified and applied as follows: Type I fractures were restricted to the restoration; Type II fractures were restricted to the crowns and did not extend to the root; Type III fractures of the crown extended to the root, yet they were less than 1 mm below the acrylic line and were restorable; and Type IV fractures occurred in the crown and the root and extended more than 1 mm below the acrylic line and were not restorable.
The force necessary to cause each fracture was recorded in kilograms. These values were subsequently converted transferred to Newton (N) values. Data for the fracture resistance tests were subjected to a one-way analysis of variance (ANOVA). The fracture patterns were evaluated using a nonparametric Kruskal–Wallis test to identify significant differences among the groups. When the Kruskal–Wallis test indicated a significant difference, multiple comparisons were performed using the Mann–Whitney test to determine which group differed from the others.
3. Results
The mean fracture resistance values obtained for each group are listed in Table 1 and statistically significant differences between the four groups were observed. When the Least Significant Difference (LSD) test was applied to compare individual groups, the mean fracture resistance value for the intact teeth (Group 1) was significantly higher than the values for the teeth that received onlay restorations (Group 3) and non-restored inlay cavities (Group 4) (p < 0.05). The teeth that received inlay restorations (Group 2) also showed a significant increase in fracture resistance compared with the teeth that received onlay restorations (Group 3) and the non-restored inlay cavities (Group 4) (p < 0.05). Furthermore, the fracture resistance of the teeth that received onlay restorations (Group 3) was significantly higher than that of the non-restored inlay cavities (Group 4) (p < 0.05). In contrast, there were no significant differences between the intact teeth (Group 1) and the teeth that received inlay restorations (Group 2) (p > 0.05) (Table 2).
Table 1.
The mean fracture resistance and standard deviation for each group.
| Group | n | Cavity | Restoration | Mean of the FR (N), ±SD |
|---|---|---|---|---|
| Group 1 | 15 | Intact | No restoration | 1326.92 ± 428.06 |
| Group 2 | 15 | Inlay | Inlay restoration | 1500.05 ± 307.78 |
| Group 3 | 15 | Onlay | Onlay restoration | 1006.13 ± 329.92 |
| Group 4 | 10 | Inlay | No restoration | 673.88 ± 243.97 |
Table 2.
Comparison of the results using LSD for the means of fracture resistances between all tested groups.
| (I) group | (J) group | Mean difference (I–J) | Std. error | Sig. | Lower bound | Upper bound | 95% Confidence interval |
|---|---|---|---|---|---|---|---|
| 1.00 | 2.00 | −173.13333 | 126.26712 | .176 | −519.7469 | 173.4802 | Not significant |
| 3.00 | 320.78667 | 126.26712 | .014 | −25.8269 | 667.4002 | Significant | |
| 4.00 | 624.26000⁎ | 141.17093 | .000 | 236.7343 | 1011.7857 | Significant | |
| 2.00 | 3.00 | 493.92000⁎ | 126.26712 | .000 | 147.3065 | 840.5335 | Significant |
| 4.00 | 797.39333⁎ | 141.17093 | .000 | 409.8676 | 1184.9191 | Significant | |
| 3.00 | 4.00 | 303.47333 | 141.17093 | .036 | −84.0524 | 690.9991 | Significant |
The mean difference is significant at the 0.05 level.
The Kruskal–Wallis test showed that the fracture modes of the four groups also significantly differed. When the Mann–Whitney test was applied, significant differences in the fracture modes were observed between the intact teeth (Group 1) and the teeth that received inlay and onlay restorations (Groups 2 and 3, respectively) (p < 0.05) (Table 3). Significant differences in the fracture modes between the teeth that received inlay restorations (Group 2) and the teeth that received onlay restorations and the non-restored teeth (Groups 3 and 4) were also observed, as well as between the onlay group (Group 3) and the non-restored group (Group 4). In contrast, there was no significant difference in the fracture mode between the untreated teeth of Group 1 and the non-restored teeth of Group 4.
Table 3.
Distribution of fracture mode for each tested group.
| Group | n | Fracture mode |
|||
|---|---|---|---|---|---|
| Type I | Type II (%) | Type III (%) | Type IV (%) | ||
| Group 1 | 15 | – | 12 (80%) | 1 (6.67 5) | 2 (13.33%) |
| Group 2 | 15 | – | – | 3 (20%) | 12 (80%) |
| Group 3 | 15 | 11 (73.33%) | – | 1 (6.67 5) | 3 (20%) |
| Group 4 | 10 | – | 9 (90%) | 1 (10%) | – |
| Total | 55 | 11 (20%) | 21 (38.18%) | 6 (10.91%) | 17 (30.91%) |
4. Discussion
In the present study, differences in fracture resistance and mode of failure were observed between intact teeth and teeth that underwent RCT and then were restored with inlay or onlay indirect composite restorations. Maxillary premolars were selected for this study due to their increased susceptibility to fracture following RCT compared to molar teeth (Hansen and Asmussen, 1990, Tamse et al., 1999, Testori et al., 1993, Lustig et al., 2000). Previously, numerous studies have been conducted to compare fracture resistance between intact teeth and teeth that have received RCT. Endodontic treatment has been reported to weaken tooth structure and increase tooth susceptibility to fracture (Khera et al., 1990, Burke, 1992, Schwartz and Robbins, 2004). Similarly, other studies (Mondelli et al., 1980, Pantvisai and Messer, 1995, Fokkinga et al., 2003) have demonstrated that tooth weakening occurs following restorative procedures which negatively affect tooth structure. However, both inlay and onlay restorations have been shown to improve fracture resistance when extensive loss of tooth structure has occurred (Van Dijken, 2000, Hannig et al., 2005, Morimoto et al., 2009). In the present study, the fracture resistances of inlay and onlay indirect restorations were compared with positive and negative control endodontically-treated upper premolars.
A compression force was applied to the specimens in the present study until breakage occurred. The advantage of this method is that it determines the maximum loads that lead to fracture. A steel ball of 6 mm diameter was used in these assays based on its ability to contact the buccal cusp, the palatal cusp, and the restorations with equal distance. Moreover, the same size ball has been used in previous studies (Soares et al., 2008a, Soares et al., 2008b). The load applied in the present study was also applied to the direction of the long axis of each tooth, and numerous studies have used the same direction to test compressive loads (Steele and Johnson, 1999, St-Georges et al., 2003, Habekost et al., 2007, Soares et al., 2008a, Soares et al., 2008b). In particular, the application of a load at an angle of 30° (Yamada et al., 2003) or 35° (Plotino et al., 2008) has been applied to the long axis of teeth to simulate lateral movements of the jaw. All these methods are commonly applied in laboratory experiments to simulate clinical situations. The average fracture resistance observed in the present study was 1326.9 N, and this value is consistent with those reported in previous studies: Soares et al. (2008a) (1124.6 N), Mondelli et al. (1998) (1698.3 N), Habekost et al. (2006) (1303.4 N), Habekost et al. (2007) (1577.8 N), and Morimoto et al. (2009) (1170 N). It is hypothesized that the variations in these values are related to differences in the speed and angle of the load that was applied.
The results of the present study demonstrate that fracture resistance decreased following the onlay restorations and the preparation of MOD cavities. These results are in agreement with those of previous studies (Yamada et al., 2003, Habekost et al., 2006, Plotino et al., 2008), where intact teeth exhibited increased fracture resistance following direct or indirect onlay restorations. In other studies (Salis et al., 1987, Burke et al., 1993, Brunton et al., 1999), onlay restorations that were fabricated with an indirect composite, porcelain, or casted gold were found to enhance fracture resistance to levels similar to the resistance levels observed for intact teeth; although these studies were conducted on vital teeth where a greater amount of tooth structure was preserved. In the present study, the onlay restoration of teeth with MOD cavities that underwent RCT resulted in an improvement of fracture resistance by 43%. However, these restorations did not provide fracture resistance that was comparable to that of the untreated teeth, and a significant difference in fracture resistance was observed between the two groups.
There were no significant differences in the fracture resistance detected between the intact teeth (Group 1) and the teeth that received inlay restorations (Group 2). These results are in accordance with those of a previous study by Hannig et al. (2005) where no significant difference between intact teeth and teeth restored with Computer-Aided Design and Computer-Aided Manufacturing (CAD/CAM) inlay restorations was observed. Two previous studies by Habekost et al. (2007) and Morimoto et al. (2009) reported similar results with vital teeth, while inlay restorations with resin cement exhibited a higher fracture resistance compared with intact teeth in other studies (Hofmann et al., 1998, Lustig et al., 2000, Yamada et al., 2003, Soares et al., 2008a). On the other hand, Allara et al. (2004) reported significantly higher fracture resistance for intact teeth compared with teeth that underwent MOD restorations with a direct composite technique. The fracture resistance of the teeth that underwent onlay restorations was also less than that of the teeth that were restored with inlay restorations, and this difference was statistically significant. However, the fractures that occurred in the onlay group most often occurred in the restorations themselves, which allowed the fractures to be repaired. These results are consistent with the relatively low resistance to breakage leading to fracture which has been experimentally characterized for composite resin restorations upon application of a load. This characteristic provides the ability to absorb a load and protect the tooth from being fractured.
The Group 4 teeth (e.g., those with non-restored MOD cavities that underwent RCT) served as negative controls in the present study, and in comparison with the teeth in Group 1 (intact teeth), a marked decrease in fracture resistance was observed for the MOD cavities. Based on these results and those of previous studies (Dalpino et al., 2002, Soares et al., 2008a, Soares et al., 2008b), decreased fracture resistance appears to not only be related to tooth vitality and the remaining tooth structure, but more importantly, is related to the bucco-lingual width of a MOD cavity. In the present study, fracture resistance decreased by 47% for teeth with a 3 mm bucco-lingual width. In previous studies by Dalpino et al. (2002), the fracture resistance for premolar teeth with unrestored MOD cavities decreased by approximately 50% when the bucco-lingual width was equal to half the distance between cusp tips (3–3.5 mm). In another study by Soares et al., 2008a, Soares et al., 2008b, the fracture resistance for upper premolar teeth with a 4.5 mm bucco-palatal width that underwent RCT decreased by 81%.
Of the fractures that occurred in the present study, 80% were non-restorable fractures (Type IV) that affected the inlay restorations, while 20% were Type III (e.g., could be restored with periodontal surgery). Moreover, compared to the intact teeth, 80% of the fractures were Type II (where the fracture was restricted to the crown and did not extend to the root) and 20% of the fractures were Type III or Type IV. These results are consistent with those of Soares et al. (2008a) where 90% of the fractures occurred in the inlay restorations, and the fractures were non-restorable. In addition, Type II fractures were observed in the intact teeth. In a study by Yamada et al. (2003), 90% of all the upper premolars that underwent RCT and inlay restoration had restorable fractures. However, it is important to note that different loading angles were used in latter study (30°) versus the present study (90°).
Regarding the onlay restorations performed in the present study, 73% of the fractures that occurred for these teeth were Type I (which only affected the restorations), and this number of fractures significantly differed from the number that occurred in the other groups. The fractures also occurred in areas with a thickness of 1 mm, and this type of early fracture protects the underlying tooth structure from unfavorable stress. These results are consistent with those of Yamada et al. (2003) where 60% of the fractures that occurred involved upper premolars that had undergone onlay restorations, and the fractures were restorable. The fractures also occurred within the small thickness area of the restorations.
It is important to point out that the present study was carried out under in vitro conditions and the fracture tests were performed 24 h after the restorations were performed. The application of thermal, chemical, and physical stresses over a longer period of time may further clarify the results obtained. In addition, the method of applying a continually increasing load to teeth, as performed in the present study, is not typical of the type of loading that occurs clinically. Ideally, more relevant test methods should be developed so that the results of in vitro tests more closely mimic the failure mechanisms of teeth and restorations that are observed clinically. Accordingly, clinical investigations are recommended to verify in vitro results and to compare fracture type and resistance according to the types of restorations performed.
5. Conclusions
Within the limits of the current study, it can be concluded that:
-
1.
Cavity preparations significantly reduced the fracture resistance of the RCT-treated maxillary premolars examined.
-
2.
MOD cavities in maxillary premolars that received RCT with indirect composite inlays or onlay restorations exhibited increased fracture resistance to withstand loads that represent those applied during mastication.
-
3.
Fractures that occurred following inlay restorations were generally more severe and were not able to be restored compared to the fractures that occurred following onlay restorations. Moreover, in the former, the fractures usually occurred within the restoration itself.
Ethical statement
This study was performed only with extracted teeth and did not include humans or animals. Therefore, ethical approval was not required.
Conflict of interest
The authors have no conflict of interest to declare.
Footnotes
Peer review under responsibility of King Saud University.
References
- Allara F.W., Jr., Diefenderfer K.E., Molinaro J.D. Effect of three direct restorative materials on molar cuspal fracture resistance. Am. J. Dent. 2004;17(4):228–232. [PubMed] [Google Scholar]
- Bremer B.D., Geurtsen W. Molar fracture resistance after adhesive restoration with ceramic inlays or resin-based composites. Am. J. Dent. 2001;14(4):216–220. [PubMed] [Google Scholar]
- Brunton P.A., Cattell P., Burke F.J., Wilson N.H.F. Fracture resistance of teeth restored with onlays of three contemporary tooth-colored resin-bonded restorative materials. J. Prosthet. Dent. 1999;82(2):167–171. doi: 10.1016/s0022-3913(99)70151-4. [DOI] [PubMed] [Google Scholar]
- Burke F.J.T. Tooth fracture in vivo and in vitro. J. Dent. 1992;20(3):131–139. doi: 10.1016/0300-5712(92)90124-u. [DOI] [PubMed] [Google Scholar]
- Burke F.J.T., Wilson N.H.F., Watts D.C. The effect of cuspal coverage on the fracture resistance of teeth restored with indirect composite resin restorations. Quintessence Int. Ed. 1993;24:875–880. [PubMed] [Google Scholar]
- Costa L.C.S., Pegoraro L.F., Bonfante G. Influence of different metal restorations bonded with resin on fracture resistance of endodontically treated maxillary premolars. J. Prosthet. Dent. 1997;77(4):365–369. doi: 10.1016/s0022-3913(97)70160-4. [DOI] [PubMed] [Google Scholar]
- Dalpino P.H., Francischone C.E., Ishikiriama A., Franco E.B. Fracture resistance of teeth directly and indirectly restored with composite resin and indirectly restored with ceramic materials. Am. J. Dent. 2002;15(6):389–394. [PubMed] [Google Scholar]
- Fokkinga W.A., Kreulen C.M., Vallittu P.K., Creugers N.H. A structured analysis of in vitro failure loads and failure modes of fiber, metal, and ceramic post-and-core systems. Int. J. Prosthodont. 2003;17(4):476–482. [PubMed] [Google Scholar]
- González-López S., De Haro-Gasquet F., Vilchez-Diaz M.A., Ceballos L., Bravo M. Effect of restorative procedures and occlusal loading on cuspal deflection. Oper. Dent. 2006;31(1):33–38. doi: 10.2341/04-165. [DOI] [PubMed] [Google Scholar]
- Habekost L., De V., Camacho G.B., Pinto M.B., Demarco F.F. Fracture resistance of premolars restored with partial ceramic restorations and submitted to two different loading stresses. Oper. Dent. 2006;31(2):204–211. doi: 10.2341/05-11. [DOI] [PubMed] [Google Scholar]
- Habekost L., De V., Camacho G.B., Azevedo E.C., Demarco F.F. Fracture resistance of thermal cycled and endodontically treated premolars with adhesive restorations. J. Prosthet. Dent. 2007;98(3):186–192. doi: 10.1016/S0022-3913(07)60054-7. [DOI] [PubMed] [Google Scholar]
- Hannig C., Westphal C., Becker K., Attin T. Fracture resistance of endodontically treated maxillary premolars restored with CAD/CAM ceramic inlays. J. Prosthet. Dent. 2005;94(4):342–349. doi: 10.1016/j.prosdent.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Hansen E.K., Asmussen E. In vivo fractures of endodontically treated posterior teeth restored with enamel-bonded resin. Dent. Traumatol. 1990;6(5):218–225. doi: 10.1111/j.1600-9657.1990.tb00422.x. [DOI] [PubMed] [Google Scholar]
- Hansen E.K., Asmussen E., Christiansen N.C. In vivo fractures of endodontically treated posterior teeth restored with amalgam. Dent. Traumatol. 1990;6(2):49–55. doi: 10.1111/j.1600-9657.1990.tb00389.x. [DOI] [PubMed] [Google Scholar]
- Hofmann N., Just N., Haller B., Hugo B., Klaiber B. The effect of glass ionomer cement or composite resin bases on restoration of cuspal stiffness of endodontically treated premolars in vitro. Clin. Oral Invest. 1998;2(2):77–83. doi: 10.1007/s007840050049. [DOI] [PubMed] [Google Scholar]
- Huang T-.J.G., Schilder H., Nathanson D. Effects of moisture content and endodontic treatment on some mechanical properties of human dentin. J. Endod. 1992;18(5):209–215. doi: 10.1016/S0099-2399(06)81262-8. [DOI] [PubMed] [Google Scholar]
- Khera S.C., Askarieh Z., Jakobsen J. Adaptability of two amalgams to finished cavity walls in class II cavity preparations. Dent. Mater. 1990;6(1):5–9. doi: 10.1016/0109-5641(90)90035-d. [DOI] [PubMed] [Google Scholar]
- Lin C., Chang C., Ko C. Multifactorial analysis of an MOD restored human premolar using auto-mesh finite element approach. J. Oral Rehabil. 2001;28(6):576–585. doi: 10.1046/j.1365-2842.2001.00721.x. [DOI] [PubMed] [Google Scholar]
- Lustig J.P., Tamse A., Fuss Z. Pattern of bone resorption in vertically fractured, endodontically treated teeth. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000;90(2):224–227. doi: 10.1067/moe.2000.107445. [DOI] [PubMed] [Google Scholar]
- Mondelli J., Steagall L., Ishikiriama A., de Lima Navarro M.F., Soares F.B. Fracture strength of human teeth with cavity preparations. J. Prosthet. Dent. 1980;43(4):419–422. doi: 10.1016/0022-3913(80)90213-9. [DOI] [PubMed] [Google Scholar]
- Mondelli R.F., Barbosa W.F., Mondelli J., Franco E.B., Carvalho R.M. Fracture strength of weakened human premolars restored with amalgam with and without cusp coverage. Am. J. Dent. 1998;11(4):181–184. [PubMed] [Google Scholar]
- Morimoto S., Vieira G.F., Agra C.M., Sesma N., Gil C. Fracture strength of teeth restored with ceramic inlays and overlays. Braz. Dent. J. 2009;20(2):143–148. doi: 10.1590/s0103-64402009000200010. [DOI] [PubMed] [Google Scholar]
- Oliveira F.C., Denehy G.E., Boyer D.B. Fracture resistance of endodontically prepared teeth using various restorative materials. J. Am. Dent. Assoc. 1987;115(1):57–60. doi: 10.14219/jada.archive.1987.0212. [DOI] [PubMed] [Google Scholar]
- Pantvisai P., Messer H.H. Cuspal deflection in molars in relation to endodontic and restorative procedures. J. Endod. 1995;21(2):57–61. doi: 10.1016/s0099-2399(06)81095-2. [DOI] [PubMed] [Google Scholar]
- Papa J., Cain C., Messer H.H. Moisture content of vital vs endodontically treated teeth. Dent. Traumatol. 1994;10(2):91–93. doi: 10.1111/j.1600-9657.1994.tb00067.x. [DOI] [PubMed] [Google Scholar]
- Plotino G., Buono L., Grande N.M., Lamorgese V., Somma F. Fracture resistance of endodontically treated molars restored with extensive composite resin restorations. J. Prosthet. Dent. 2008 Mar;99(3):225–232. doi: 10.1016/S0022-3913(08)60047-5. [DOI] [PubMed] [Google Scholar]
- Randow K., Glantz P.-O. On cantilever loading of vital and non-vital teeth an experimental clinical study. Acta Odontol. 1986;44(5):271–277. doi: 10.3109/00016358609004733. [DOI] [PubMed] [Google Scholar]
- Reeh E.S., Messer H.H., Douglas W.H. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J. Endod. 1989;15(11):512–516. doi: 10.1016/S0099-2399(89)80191-8. [DOI] [PubMed] [Google Scholar]
- Ritter A.V., Baratieri L.N. Ceramic restorations for posterior teeth: guidelines for the clinician. J. Esthet. Restor. Dent. 1999;11(2):72–86. doi: 10.1111/j.1708-8240.1999.tb00381.x. [DOI] [PubMed] [Google Scholar]
- Salis S.G., Hood J.A.A., Kirk E.E.J., Stokes A.N.S. Impact-fracture energy of human premolar teeth. J. Prosthet. Dent. 1987;58(1):43–48. doi: 10.1016/s0022-3913(87)80140-3. [DOI] [PubMed] [Google Scholar]
- Schwartz R.S., Robbins J.W. Post placement and restoration of endodontically treated teeth: a literature review. J. Endod. 2004;30(5):289–301. doi: 10.1097/00004770-200405000-00001. [DOI] [PubMed] [Google Scholar]
- Soares P.V., Santos-Filho P.C.F., Martins L.R.M., Soares C.J. Influence of restorative technique on the biomechanical behavior of endodontically treated maxillary premolars. Part I: fracture resistance and fracture mode. J. Prosthet. Dent. 2008;99(1):30–37. doi: 10.1016/S0022-3913(08)60006-2. [DOI] [PubMed] [Google Scholar]
- Soares P.V., Santos-Filho P.C., Gomide H.A., Araujo C.A., Martins L.R., Soares C.J. Influence of restorative technique on the biomechanical behavior of endodontically treated maxillary premolars. Part II: strain measurement and stress distribution. J. Prosthet. Dent. 2008 Feb;99(2):114–122. doi: 10.1016/S0022-3913(08)60027-X. [DOI] [PubMed] [Google Scholar]
- Steele A., Johnson B.R. In vitro fracture strength of endodontically treated premolars. J. Endod. 1999;25(1):6–8. doi: 10.1016/S0099-2399(99)80389-6. [DOI] [PubMed] [Google Scholar]
- St-Georges A.J., Sturdevant J.R., Swift E.J., Jr., Thompson J.Y. Fracture resistance of prepared teeth restored with bonded inlay restorations. J. Prosthet. Dent. 2003;89(6):551–557. doi: 10.1016/s0022-3913(03)00173-2. [DOI] [PubMed] [Google Scholar]
- Tamse A., Fuss Z., Lustig J., Kaplavi J. An evaluation of endodontically treated vertically fractured teeth. J. Endod. 1999;25(7):506–508. doi: 10.1016/S0099-2399(99)80292-1. [DOI] [PubMed] [Google Scholar]
- Testori T., Badino M., Castagnola M. Vertical root fractures in endodontically treated teeth: a clinical survey of 36 cases. J. Endod. 1993;19(2):87–90. doi: 10.1016/S0099-2399(06)81202-1. [DOI] [PubMed] [Google Scholar]
- Trope M., Langer I., Maltz D., Tronstad L. Resistance to fracture of restored endodontically treated premolars. Dent. Traumatol. 1986;2(1):35–38. doi: 10.1111/j.1600-9657.1986.tb00120.x. [DOI] [PubMed] [Google Scholar]
- Van Dijken J.W. Direct resin composite inlays/onlays: an 11 year follow-up. J. Dent. 2000;28(5):299–306. doi: 10.1016/s0300-5712(00)00010-5. [DOI] [PubMed] [Google Scholar]
- Wendt S.L., Jr., Harris B.M., Hunt T.E. Resistance to cusp fracture in endodontically treated teeth. Dent. Mater. 1987;3(5):232–235. doi: 10.1016/S0109-5641(87)80078-7. [DOI] [PubMed] [Google Scholar]
- Yamada Y., Tsubota Y., Fukushima S. Effect of restoration method on fracture resistance of endodontically treated maxillary premolars. Int. J. Prosthodont. 2003;17(1):94–98. [PubMed] [Google Scholar]
- Zidan O., Abdel-Keriem U. The effect of amalgam bonding on the stiffness of teeth weakened by cavity preparation. Dent. Mater. 2003;19(7):680–685. doi: 10.1016/s0109-5641(03)00013-7. [DOI] [PubMed] [Google Scholar]


