Abstract
AIM: To recognize the characteristic findings of micro-liver cancer (MLC) and to evaluate the effect of CT arterial portography (CTAP) and CT hepatic arteriography (CTHA) in diagnosis of MLC.
METHODS: Between April 1996 to December 1998, CTAP and CTHA were performed in 12 patients with MLC, which were not detected by conventional CT examinations. After CTHA, 3 mL-5 mL mixture of lipiodol, doxorubicin and mitoycin C were injected into hepatic artery through the catheter, and the followed up by CT three or four weeks later (Lipiodol CT Lp-CT).
RESULTS: A total of 22 micro-tumors (0.2 cm-0.6 cm in diameter) were detected in 12 patients, which manifested as small perfusion defects in CTAP and small round enhancement in CTHA. The rate of detectability of CTAP and CTHA was 68.2% (15/22) and 77.3% (17/22) respectively, and the rate of the simultaneous use of both procedures reached 86.4% (19/22). All micro-tumors were demonstrated as punctate lipiodol deposit foci in Lp-CT. After Lp-CT, the elevated serum level of α-fetoprotein (AFP) dropped to the normal level in all patients.
CONCLUSION: The CTAP and CTHA are the most sensitive imaging methods for detecting micro-liver cancer. Confirmed by the change of the elevated serum AFP level and lipiodol deposit foci in Lp-CT, small perfusion defects in CTAP and puntuate enhancement in CTHA may suggest micro-liver cancer.
Keywords: liver neoplasms/diagnosis, CT arterial portography, CT hepatic arteriography
INTRODUCTION
With combined the findings of diagnostic imaging and elevated serum AFP level, more and more small liver cancer were detected earlier, and the therapeutic effect was significantly improved[1,2]. Except for other causes, such as hepatitis and teratoma, the elevated serum AFP level (higher than 400 μg/L) strongly suggests the occurrence of primary hepatocellular carcinoma. However, sometimes no tumors could be found on conventional CT scanning (contrast material administered by intra-venous injection). These patients were further examined with were CTAP and CTHA. From April 1996 to December 1998, 12 patients with micro-cancer were examined with CTAP and CTHA in our hospital.
MATERIALS AND METHODS
Materials
From April 1996 to December 1998, 12 patients (10 men, 2 women) suspected to hav e liver cancer were examined with CTAP and CTHA. They ranged in age from 23 to 54 years (mean age, 36.4 years). The serum level of AFP was elevated in all the patients with a range of 201 μg/L to 1405 μg/L (including 8 cases > 400 μg/L, 4 cases < 400 μg/L). Cirrhosis occurred in 7 cases. The tumors were 0.2 cm-0.6 cm in size with a mean of 0.46 cm. Multiple nodules were found in 7 cases.
Methods
CTAP examinations were performed with incremental scanning of the liver in cranial-to-caudal direction with 2.7 mm to 8 mm collimation on bi-spiral-Elscint Twin Flash scanner (Elscint-Corp.). CT images were obtained 25 sec-35 sec after the initiation of transcatheter (5-F) superior mesenteric artery injection of 30 mL-40 mL of non-ionic contrast medium at a rate of 2.5 mL/sec-3.0 mL/sec with an automatic power injector (Medrad, Pittsburgh). During the catheterization, contrast medium administered before CT scanning was limited to 5 mL-10 mL inject ed by hand to visualize any aberrant vessels and to facilitate proper catheter placement.
CTHA examinations were done by injecting contrast medium into proper hepatic artery or common hepatic artery. Twenty mL to 30 mL of contrast medium was injected at a rate of 3.0 mL/sec-3.5 mL/sec. Consecutive scanning of the liver was started 6sec-8sec after the initiation of injection of the contrast m edium. After CTHA examinations, 3 mL-5 mL mixture of lipiodol, doxorubicin (10 mg-15 mg), and mitoycin C (2 mg-4 mg) were injected into hepatic artery, and the follow-up CT was performed three or four weeks later (Lp-CT). The serum AFP level was detected in all the patients two or three weeks later, and all returned to normal within 1-6 months.
RESULTS
Detectable rate of micro-tumors
A total of 22 micro-tumors were found in our group. The tumors measured 0.2 cm-0.6 cm with a mean of 0.46 cm. CTAP and CTHA images were carefully interpreted by two experienced radiologists. Fifteen tumors were demonstrated as fleckly perfusion defects on CTAP images with a detectable rate of 68.2%, and 17 manifested as punctate enhancement foci on CTHA with a detectable rate of 77.3%. Nineteen were found by simultaneous use of both procedures with a detectable rate of 84.4%. But 3 tumors were not detected by CTAP and CTHA in 2 patients. All 22 micro-tumors manifested as punctate lipiodol deposit foci in Lp-CT, which was performed two or three weeks later. Because the tumors in our series were extremely small, no pathologic dia gnosis was acquired in all patients.
Follow-up of patients
The serum AFP level was examined two or three weeks after Lp-CT. The AFP level dropped to the normal level in all the patients. Within 1-6 months. All survived without any signs of recurrence in our group, and the survival period ranged f rom 3 to 33 months (mean, 15.2 months).
DISCUSSION
In some of our patients found with elevated serum level by AFP, no tumors were d etected by conventional CT scanning. For those patients, CTAP and CTHA examinations were recommended. Fleckly perfusion defects were found on CTAP (Figure 1) and punctate enhancement foci on CTHA (Figure 2). After CTHA examination, 3 mL-5 mL mixture of lipiodol and anticancer drug was tentatively injected in to hepatic artery for Lp-CT diagnosis, which was repeated three or four weeks later. Micro-foci of lipiodol deposit was found with elevated serum AFP level, which dropped continuous to normal. The prognosis of these patients was very good. Since April 1996, 12 patients with such findings have been examined in our hospital. All patients were surviving without any signs of recurrence, and the longest survival being 33 months. Due to its special clinical significance, we sugge sted the definition of micro-cancer in liver (0.2 cm-0.6 cm in diameter) which includes: (1) elevated serum AFP level (AFP ≥ 400 μg/L, or rising continuouslly); (2) no micro-tumors were detected by conventional imaging methods, but by CTAP and CTHA; (3) Punctate lipiodol deposit foci were demonstrated on Lp-CT; and (4) after Lp-CT, serum AFP level lowered continous or turned to normal level. CTAP and CTHA are considered as the most sensitive imaging methods for detecting small hepatocellular carcinoma[3]. The development of spiral CT technique greatly facilitated procedures and improved the quality of CT images[4]. Detectability of CTAP and CTHA for very small tumors (as small as 0.2 cm in diameter, Figure 3) was high, being 68.2% and 77.3% respectively, and that of simultaneous use of both procedures was 84.4%. But there were still some cases of micro-tumors which could not be detected by CTAP and CTHA. In a 28-year-old female patient with elevated AFP level of 860 μg/L, no tumors were found eit her on conventional CT scanning or on CTAP and CTHA images. Three weeks later, Lp-CT detected a punctate lipiodol deposit focus of 0.2 cm in diameter in her left lobe with AFP continous dropping to normal level (Figure 4). This patient had survived for 33 months without any signs of recurrence. With the widespread use of CTAP and CTHA, ther e have been more reports on non- pathologic perfusion defects detected with CTAP and non-pathologic enhancement detected with CTHA. Due to aberration of blood supply for some parts of the liver, such as arterio-portal shunt[5], cirrhotic nodule, focal nodular hyperplasia, and focal fatty infiltration, the normal tissue could manifest as perfusion defects in CTAP, especially in the medial segment of the left lobe[6]. Peterson et al[7] reported that perfusion defects on CTAP were sometimes nonspecific, and peripheral flat or wedge-shaped perfusion defects indicated benignity. In our study, the occurrence rate of non-pathologic perfusion defects detected with CTAP was 15.1%, and peripheral wedge-shaped perfusion defects were most common[8]. Similar to findings of CTAP, pseudo-lesion enhancement of normal liver tissue also occurred in CTHA. Kanematsu et al[9] supposed that local non-pathologic enhancement detected with CTHA might result from the cystic venous drainage or peripheral arterio-portal shunts. In our study, the occurrence rate of non-pathologic enhance ment detected with CTHA was 22.0%, and small round peripheral enhancement was s een most commonly[8] (Figure 5). Thus, we do not recommend to use CTAP or CTHA alone to interpret small hepatocellular carcinomas. The combined use of both procedures can help distinguish micro-cancer from the false-positive findings on CTAP and CTHA, and increase the accuracy of diagnosis for small hepatocellular carcinoma[10]. Besides the findings on CTAP and CTHA images, combination of lipiodol deposit foci on Lp-CT and dropping of elevated serum AFP level are also helpful for the establishment of diagnosis for liver micro-cancer.
Figure 1.

CTAP image obtained in a 40-year-old man with liver micro-cancer shows a punctuate perfusion defect in right lobe.
Figure 2.
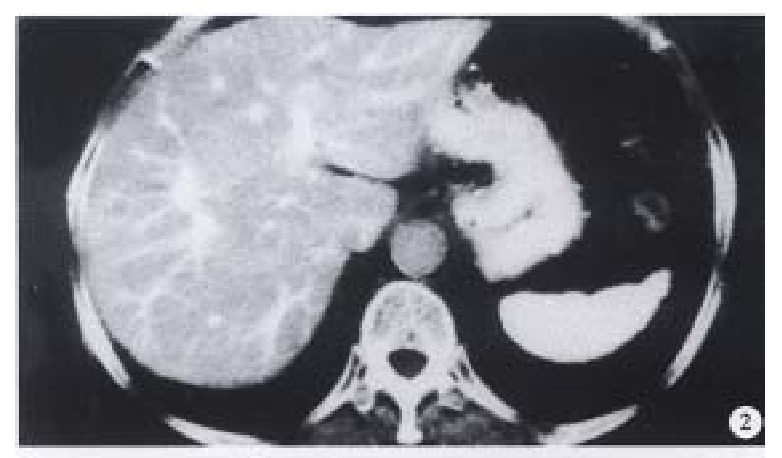
CTHA image obtained on the same slice to Figure 1, the micro-tumor manifested as an small round enhancement nodule.
Figure 3.

CTHA in a 45-year-old man shows a micro-cancer with a diameter of 0.3 cm.
Figure 4.
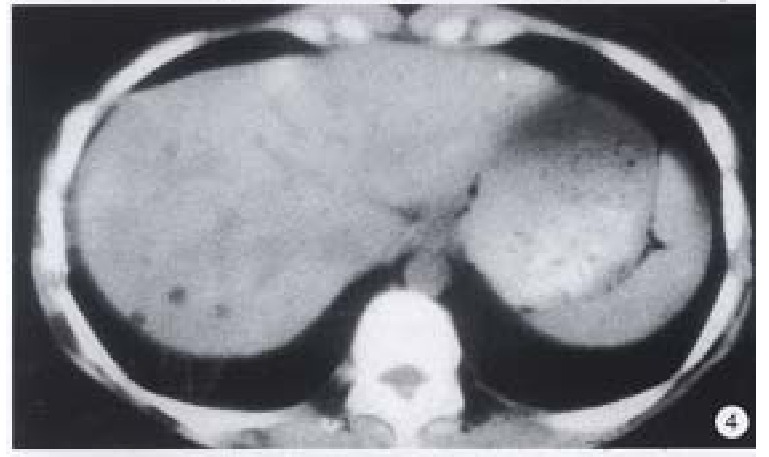
A punctuate lipiodol deposit focus with 0.2 cm in diameter is shownon Lp-CT in a 28-year-old woman with elevate d serum AFP level of 860 μg/L detects which was not detected by CTAP and CTHA.
Figure 5.

CTHA in a 35-year-old man shows two punct uate non-pathologic enhancement foci on the edge of right lobe.
Footnotes
Supported by “9·5” National Major Project of National Committee of Sciences and Technology, No. 96-907-03-02.
Edited by Jing-Yun Ma
References
- 1.Wu MC. Clinical research advances in primary liver cancer. World J Gastroenterol. 1998;4:471–474. doi: 10.3748/wjg.v4.i6.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tang ZY. Advances in clinical research of hepatocellular carci-noma in China. WCJD. 1998;6:1013–1016. [Google Scholar]
- 3.Hori M, Murakami T, Oi H, Kim T, Takahashi S, Matsushita M, Tomoda K, Narumi Y, Kadowaki K, Nakamura H. Sensitivity in detection of hypervascular hepatocellular carcinoma by helical CT with intra-arterial injection of contrast medium, and by helical CT and MR imaging with intravenous injection of contrast medium. Acta Radiol. 1998;39:144–151. doi: 10.1080/02841859809172168. [DOI] [PubMed] [Google Scholar]
- 4.Murakami T, Oi H, Hori M, Kim T, Takahashi S, Tomoda K, Narumi Y, Nakamura H. Helical CT during arterial portography and hepatic arteriography for detecting hypervascular hepatocellular carcinoma. AJR Am J Roentgenol. 1997;169:131–135. doi: 10.2214/ajr.169.1.9207512. [DOI] [PubMed] [Google Scholar]
- 5.Tamura S, Kihara Y, Yuki Y, Sugimura H, Shimizu T, Adjei ON, Watanabe K. Pseudo lesions on CTAP secondary to arterio-portal shunts. Clin Imaging. 1997;21:359–365. doi: 10.1016/s0899-7071(96)00088-5. [DOI] [PubMed] [Google Scholar]
- 6.Matsui O, Kadoya M, Yoshikawa J, Gabata T, Kawamori Y, Ueda K, Nobata K, Takashima T. Posterior aspect of hepatic segment IV: patterns of portal venule branching at helical CT during arterial portography. Radiology. 1997;205:159–162. doi: 10.1148/radiology.205.1.9314978. [DOI] [PubMed] [Google Scholar]
- 7.Peterson MS, Baron RL, Dodd GD, Zajko AJ, Oliver JH, Miller WJ, Carr BI, Bron KM, Campbell WL, Sammon JK. Hepatic parenchymal perfusion defects detected with CTAP: imaging-pathologic correlation. Radiology. 1992;185:149–155. doi: 10.1148/radiology.185.1.1326119. [DOI] [PubMed] [Google Scholar]
- 8.Li L, Wu PH, Lin HG, Li JQ, Mo YX, Zheng L, Lu LX, Ruan CM, Chen L. Findings of non-pathologic perfusion defects by CT arterial portography and non-pathologic enhancement of CT hepatic arteriography. World J Gastroenterol. 1998;4:513–515. doi: 10.3748/wjg.v4.i6.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kanematsu M, Hoshi H, Imaeda T, Yamawaki Y, Mizuno S, Manabe T, Enya M, Yokoyama R. Nonpathological focal enhancements on spiral CT hepatic angiography. Abdom Imaging. 1997;22:55–59. doi: 10.1007/s002619900140. [DOI] [PubMed] [Google Scholar]
- 10.Irie T, Takeshita K, Wada Y, Kusano S, Terahata S, Tamai S, Hatsuse K, Aoki H, Sugiura Y. CT evaluation of hepatic tumors: comparison of CT with arterial portography, CT with infusion hepatic arteriography, and simultaneous use of both techniques. AJR Am J Roentgenol. 1995;164:1407–1412. doi: 10.2214/ajr.164.6.7754883. [DOI] [PubMed] [Google Scholar]


