Abstract
AIM To discuss the effect of surgical procedures on the prognosis of patients of bile duct cancer and their indications.
METHODS A retrospective analysis was made for 52 cases of hepat oportal bile duct cancer treated from January 1991 to December 1996. All the cases were classified according to the modified Bismuth-Corlettle sys tem and received appropriate operation. Therapeutic effects were evaluated on the basis of their survival rates, jaundice elimination, comfort index, operative mortality and complications.
RESULTS Seventeen cases received surgical resection (32.7%). The survival rate was 71.4%, 35.7% and 10.4% for one, two and three years respectively, and was 30%, 16.8% and 0% for those with drainage (P < 0.05). The mortality rate was 6.0% for the drainage group and 5.9% for the resection group (P > 0.05). Of the 17 resected patients, 8 (47.1%) had curative resection and 9 (52.9%) noncurative resection. Their mean survival time was 21.1 months and 7.5 months respectively (P < 0.05).
CONCLUSION Proper surgical procedure should be used on the basis of the local and general conditions of the patients, and aggressive resection with or without liver resection is a valid procedure for the treatment of hepato portal bile duct cancer and can significantly improve the prognosis of patients.
Keywords: biliary tract neoplasms/surgery, prognosis hepatic portal
INTRODUCTION
Surgical resection is the only effective way for hepatoportal bile duct cancer. However, the treatment is very troublesome due to its low resectability and poor prognosis. The purpose of this paper is to discuss the effect of surgical procedures on its prognosis and indications.
PATIENTS AND METHODS
From January 1991 to December 1996, 52 patients with hepatoportal bile duct cancer (53.6% of extrahepatic bile duct cancer) were treated in our hospital. Of them, 39 were male and 13 female aged from 37 to 70 years, averaging 56.8. The patients aged from 50 to 70 years made up 65.4%. The diagnosis was confirmed by histological examination in 46 and by operation in 6. All the tumors were classified according to the modified Bismuth-Corlette system. Therapeutic effect was evaluated by their survival rate, jaundice elimination, comfort index, oper ative mortality and complications. The data collected during the follow-up were analysed with the help of American SAS software. The parameters were compared by Chi-square test and Student’s t test. Differences between the survival rates were analysed by Likelihood Ratio Test or Wilcoxon test, and significant difference (P < 0005) was found.
RESULTS
Pathological findings
Out of the 52 patients (88.5%), the diagnosis of bile duct cancer was confirmed by histological examination in 46 and by operation in 6. Adenocarcinoma was found in 97.8% and sclerotic cholangiocarcinoma in 52.9% of the 17 resected patients. Local or distant metastatic tumors were found in 7 patients, which wer e confirmed in the 6th, 55th, 45th, 15th, 14th, 25th and 15th month after operation respectively by fine needle aspiration biopsy (FNAB), CT, or B-US.
Based on macroscopic appearance, complete excision of the tumor was not achieved in six cases. Involvement of the stem of the portal vein was discovered in one case during dissection. Of the 17 resected patients, a macroscopic curative resection was achieved in 11 (11/52, 21.2%). Residual cancer cells were found at the surgical resection margins in 3 cases. Thus, curative resec tion was performed only in 8 patients (8/52, 15.4%).
Surgical findings
The types of operation for hepatoportal bile duct cancer are shown in Table 1.
Table 1.
Operative procedures for 52 hepatoportal bile duct cancer and their mortality
| Operative procedure | No. of patients | No. of death |
| Resection | 17 | 1 |
| Local resection (LR) | (3) | (0) |
| LR + Caudate segment resection | (1)a | (0) |
| LR + Median segment resection | (4)a | (1) |
| LR + Right/left hemihepatectomy | (9)b | (0) |
| Bypass | 33 | 2 |
| Segment III cholangiojejunostomy | (20) | (2) |
| Segment V cholangiojejunostomy | (9) | (0) |
| Choledochojejunostomy | (3) | (0) |
| Intubation | 1 | 0 |
| Exploration | 2 | 0 |
| Total | 53 | 3 |
Partial excision of portal vein and repair of its lateral wall;
Reconstruction of right hepatic artery in one case.
Operative survival rate and complications
The total operative mortality rate was 5.8% (3/52) and 5.9% (1/17) and 6.0% (2/33) respectively in resection group and drainage group with no stati stical significance (P = 0.5422). No death was found in 30 days after extensive excision. One patient died 27 days after palliative excision due to massive hemorrhage in the upper digestive tract caused by stress ulcer.
The total operative complication rate was 44.2% (23/52), 52.9% in the resect ion group and 42.4% in the drainage one with no statistical significance (P = 0.4797). The operative complication rate was 50.0% (4/8) in those who received curative resection, and was 55.6% in those who had palliative excision.
Survival rate
The average survival of the 52 patients was 9.1 months. The survival rate for 1, 2, 3, 4 and 5 years was 43.2%, 25.9%, 25.9%, 12.9% and 4.0%.
Types of operation and quality of life The average survival time was 6.4 months in the drainage group and was 15.6 months (P < 0.05) in the resection group. The quality of life after operation was evaluated according to the elimination of jaundice, and the comfort index. Complete elimination of jaundice means that serum bilirubin is returned to normal while partial elimination implies that serum bilirubin is dropped by 50% at least as compared with that before operation, and no reduction refers to its decrease of less than 50%. The duration of well-being is known as the period of time in which the patient is free of jaundice, pruritus, cholangitis and malaise after surgery. The comfort index is taken as the duration of well-being expressed in percentage of total survival time, which is close to 100% when the disease is completely relieved (Table 2).
Table 2.
Average survival time and comfort indices of the patients after resection and drainage
| Operative procedure | No. of patients | Mean survival time (mo) | Comfort index (%) |
| Resection | 17 | 15.62a | 91b |
| Drainage | 33 | 6.37a | 74b |
P < 0.005,
P < 0.05.
Math 1
Math 1.
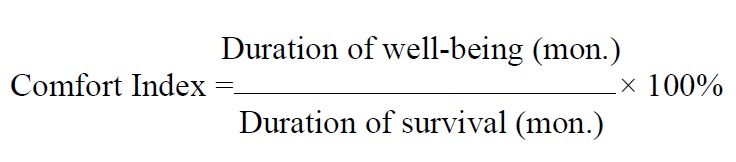
Math(A1).
Comparison of the survival rates between resection and drainage The survival rate was 71.4%, 35.7% and 10.4% for the patients who underwent resection, and 30.0%, 16.8% and 0% for the patients underwent drainage. There was a significant difference between them (P < 0.05).
DISCUSSION
The treatment of hepatoportal bile duct cancer is very troublesome. Untreated patients usually die of recurrent cholangitis and hepatic failure within 3 months when their diagnosis is confirmed[1]. Before 1970, many authors held that bile duct cancer should be treated vigorously. Therapeutic effect of excision for it has been gradually improved as a result of accurate diagnosis and better operative techniques.
It was reported that 15%-95% patients with hepatoportal bile duct cancer upon the spectrum of cases referred to any particular surgical unit and the cancer re ceived excision, which has exceeded 30%[2,3]. In our study 32.7% patients received excision. The excision rate and survival rate were much higher than those from 1986 to 1990 (P < 0.05)[4].
The data in our study provides strong support for other surgeons[2,3,5]. The survival rate for 1, 3 and 5 years after radical operation of hepatoportal bile duct cancer was 71.4%, 35.7% and 5.9% while the operative mortality and complications had no remarkable increase. The operative death rate due to hepatic failure and bile leakage at the anastomosis was 5.9% in our study, while it was from 0% to 27% in the literature.
It is controversial whether radical operation should be performed for hepatoportal bile duct cancer. Some authors held that it is not necessary to have partial hepatectomy because it can not improve the survival and will increase postoperative mortality and complications on the contrary[6,7]. The residual rate of cancer cell at its incisional margin was 28%-92% in the literature. Furthermore, the recurrent rate of tumor was high even after radical operation. Others advocate radical operation for cholangiocarcinoma with right or left hemihepatectomy, trisegmentectomy, vascular resection and its reconstruction and caudate lobe resection, even total hepatectomy and orthotopic liver transplanta tion[2,3,8] in order to remove more tumor tissues, prolong the survival and reduce its recurrence. In our study, out of the 17 resected patients, 14 (82.4%) had hepatectomy which was characterized by: (1) Hepatoportal parenchyma was excised if it was involved or in an effort to eliminate residu al cancer cells at its incisional margins; (2) Hepatolobectomy was a curative procedure for the patient when unilateral bile duct was involved; (3) Unilateral bile duct was involved beyond secondorder; (4) Unilateral portal vein or hepatic artery was involved. The average survival was 16.1 months. Of the 17 patients who underwent resection, curative excision was performed in 8, and non-curative excision in 9. Their average survival was 21.1 and 7.5 months respectively (P < 0.05). The 1 and 2-year survival of those with no residual cancer cells at their incisional margins was 87.5% and 44.5%, while it was 57.1% and 30.1% (P < 0.05) for those with residual cancer cells at their incisional margins. No significant difference was found in operative complication and death rate between the two groups. Therefore, hepatolectomy should be taken into consideration when the patient’s-local conditions and general conditions are good.
However, a considerable number of patients could not endure major operations due to their severe jaundice and poor liver function when they came to see a doctor . Major hepatectomy would undoubtedly lead to further damage of liver function and postoperative hepatic failure . Median hepatolectomy should be performed for such patients because it has the advantages of less hepatic injury and a higher cure rate[9]. In our study, 4 of the 17 resected patients received median hepatolectomy, 2 curative excision, and 2 palliative excision . One died of massive gastrointestinal bleeding due to stress ulcer on the 27th day after operation. The other 3 had significant improvement in their life Quality with an average survival of 14.7 months, and one is still alive 25 months after operation with no recurrence.
Cholangiocarcinoma is inclined to invade its peripheral tissues, such as portal vein, hepatic artery and parenchyma as well as the caudate lobe because there is no muscular layer of mucosa in the wall of bile duct. It was reported that better prognosis could be achieved by caudatolectomy[3,10]. One patient received this operation in our study. We advocate resection of the caudate lobe when considerable involvement of the caudate ducts or parenchyma is confirmed by preoperative or intraoperative assessment. Angiotectomy and reconstruction are advisable for selected patients when their blood vessels are involved[11]. In this study, wedge resection and reconstruction of portal vein were perfor med in one patient due to involvement of portal veins; and right hepatic artery reconstruction and left hemihepatectomy in another due to involvement of portal vein, left and right orteries. They recovered after operation. It is believed that residual cancer cells in the connective tissue around the hepatoduodenal ligament may play a major role in the tumor recurrence. Major hepatic resection, including excision of the whole hepatodudenal ligament, is experimen tally fe asible, and its clinical results are promising[12,13]. However, tumor cells were found in some patients even after such extensive excisions. So its indication should be taken into careful consideration in clinical practice.
Although, excision is the only way to cure hepatoportal bile duct cancer, a considerable number of patients are not suitable to receive it in spite of great advances having made in diagnostic techniques and surgical treatment. Palliative operation has advantages of less complications and better life quality over conservative treatment[14]. The curative effect of palliative operation is characterized by the level of jaundice elimination. In our study, complete elimination of jaundice was made in 85% of the 20 patients treated by segment III hepaticocholangiojejunostomy with a comfort index of 74%, and with a 10% operative mor tality. The curative effect of SV hepatocholangioj-ejunostomy in the other 9 patients was similar to that of segment III hepatocholang iojejunostomy. Drainage tube may be placed for those who can not receive excision and intrahepatic drai nage. Since long-standing external drainage of bile may lead to water and electrolyte imbalance, recurrence of jaundice, and cholangitis. Intrahepatic anastomosis to segment III or V hepatic duct, or both should be the first choice in palliative treatment.
From the above analysis, we believe that the following preoperative examinations must be made for cholangiocarcinoma, such as serological and bio-logical tests, liver and renal function test, blood co-agulation tests, B-US, PTC/ERCP, angio graphy, etc. Only when there are no contraindications and the patient’s general condition is good, should a tumor excision with or without liver resection be performed. Resection and reconstruction of hepatoportal vessels should be carr ied out for selected patients. If resection is not feasible, palliative biliary drainage is worthwhile. More extensive resection (like block resection) should be selected very carefully. It is not wise to lay undue stress on a more radical operation. What we advocate is the surgical procedure selected according to the extent, gross appearance and degree of infiltration of tumor to its adjacent tis sues or organs in order to achieve the most effective result and to relieve the patient’s-sufferings.
Footnotes
Edited by Xian-Lin Wang
References
- 1.DENBESTEN L, LIECHTY RD. CANCER OF THE BILIARY TREE. Am J Surg. 1965;109:587–589. doi: 10.1016/s0002-9610(65)80009-5. [DOI] [PubMed] [Google Scholar]
- 2.Baer HU, Stain SC, Dennison AR, Eggers B, Blumgart LH. Improvements in survival by aggressive resections of hilar cholangiocarcinoma. Ann Surg. 1993;217:20–27. doi: 10.1097/00000658-199301000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sugiura Y, Nakamura S, Iida S, Hosoda Y, Ikeuchi S, Mori S, Sugioka A, Tsuzuki T. Extensive resection of the bile ducts combined with liver resection for cancer of the main hepatic duct junction: a cooperative study of the Keio Bile Duct Cancer Study Group. Surgery. 1994;115:445–451. [PubMed] [Google Scholar]
- 4.Cao XH. A clinical analysis of 106 cases of extrahepatic bile duct cancer. Shiyong Waike Zazhi. 1992;12:578. [Google Scholar]
- 5.Huang JF, Li SP, Cao XH. A discussion on surgical option for proximal bile duct cancer. Fubu Waike. 1992;3:179. [Google Scholar]
- 6.Hadjis NS, Blenkharn JI, Alexander N, Benjamin IS, Blumgart LH. Outcome of radical surgery in hilar cholangiocarcinoma. Surgery. 1990;107:597–604. [PubMed] [Google Scholar]
- 7.Bengmark S, Ekberg H, Evander A, Klofver-Stahl B, Tranberg KG. Major liver resection for hilar cholangiocarcinoma. Ann Surg. 1988;207:120–125. doi: 10.1097/00000658-198802000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pichlmayr R, Weimann A, Ringe B. Indications for liver transplantation in hepatobiliary malignancy. Hepatology. 1994;20:33S–40S. doi: 10.1016/0270-9139(94)90271-2. [DOI] [PubMed] [Google Scholar]
- 9.White TT. Skeletization resection and central hepatic resection in the treatment of bile duct cancer. World J Surg. 1988;12:48–51. doi: 10.1007/BF01658485. [DOI] [PubMed] [Google Scholar]
- 10.Nimura Y, Hayakawa N, Kamiya J, Kondo S, Shionoya S. Hepatic segmentectomy with caudate lobe resection for bile duct carcinoma of the hepatic hilus. World J Surg. 1990;14:535–543; discussion 544. doi: 10.1007/BF01658686. [DOI] [PubMed] [Google Scholar]
- 11.Nimura Y, Hayakawa N, Kamiya J, Maeda S, Kondo S, Yasui A, Shionoya S. Combined portal vein and liver resection for carcinoma of the biliary tract. Br J Surg. 1991;78:727–731. doi: 10.1002/bjs.1800780629. [DOI] [PubMed] [Google Scholar]
- 12.Mimura H, Takakura N, Kim H, Hamazaki K, Tsuge H, Ochiai Y. Block resection of the hepatoduodenal ligament for carcinoma of the bile duct and gallbladder. Surgical technique and a report of 11 cases. Hepatogastroenterology. 1991;38:561–567. [PubMed] [Google Scholar]
- 13.Kumada K, Ozawa K, Shimahara Y, Morikawa S, Okamoto R, Moriyasu F. Truncoumbilical bypass of the portal vein in radical resection of biliary tract tumour involving the hepatic duct confluence. Br J Surg. 1990;77:749–751. doi: 10.1002/bjs.1800770711. [DOI] [PubMed] [Google Scholar]
- 14.Langer JC, Langer B, Taylor BR, Zeldin R, Cummings B. Carcinoma of the extrahepatic bile ducts: results of an aggressive surgical approach. Surgery. 1985;98:752–759. [PubMed] [Google Scholar]


