Abstract
Objective
The purpose of this study was to evaluate the feasibility of the methods proposed to conduct a full randomized clinical trial to assess the effectiveness of mobilization with movement on shoulder functionality in older adults with shoulder dysfunction.
Methods
A pilot, randomized, single-blinded clinical trial was carried out with 44 older adults (83.9±8.2 years) with shoulder dysfunction in 3 nursing homes in Toledo, Spain. Participants were recruited through information sessions and were randomly allocated into 2 groups. The control group (n = 22) intervention consisted of a physical therapy standard protocol proposed by the Spanish Rheumatology Society. Techniques based on Mulligan’s concepts of mobilization with movement were added to the standard protocol for the experimental group (n = 22) intervention. Interventions took place 3 times a week for 2 consecutive weeks and were performed by 2 experienced therapists. Main outcomes were recruitment rates, participation and adherence to interventions, assessment procedures, and the implementation of mobilization with movement. Clinical outcomes were shoulder functionality, active glenohumeral range of motion, and pain intensity. Data were collected at baseline, after each group intervention, and at 1 and 3 months after finishing interventions.
Results
All the participants accepted to be randomized. Participation rates were 97.7% for the experimental group and 95.5% for the control group. The analysis of variance did not show any statistically significant difference between treatment groups for any of the variables (all P values for the group effect were greater than .36) or a change of the difference between groups over time (all P values for the time-treatment interactions were greater than .3).
Conclusion
The research methods tested in this pilot study offer a suitable foundation to conduct a full clinical trial.
Key indexing terms: Shoulder, Disability evaluation, Physical therapy modalities, Frail elderly
Introduction
Shoulder dysfunction is a common problem in older adults with a described prevalence of 21%.1 Shoulder symptoms, such as pain and reduction in active range of motion (AROM) and functionality, might be associated to chronic pain, disability, and a decrease in physical performance over time.1, 2 Upper limbs and shoulder joint proper functionality leads to an adequate independence in activities of daily living (ADLs) and functional performance. Therefore, maintaining independence in ADL and the functional well-being in older adults should be a priority target for health care.3 A successful therapeutic approach depends on understanding that the aging process is responsible for major changes in muscles and joints and may cause muscle disorders and joint stiffness.4
Physical therapy interventions are often recommended as the first choice for a conservative treatment in the most common approaches to treat patients with shoulder dysfunction.5, 6, 7 Regarding physical therapy interventions, there are evidence about the effectiveness of therapeutic exercise,8, 9 and the benefit of manual therapy10, 11 so as to increase shoulder mobility, and a trend in improving pain measures. Enhancements in function and quality of life are still questionable.6, 7
Mobilization with movement (MWM) is a manual therapy technique based on the analysis and correction of any minor positional faults in a joint. According to Mulligan, positional faults are due to various soft tissue and/or bone lesions in/around the joint. The relevance of a correct joint position was argued in a kinematic study in healthy shoulders.12 This technique aims to realign the joints positional faults by performing a manually specific oriented glide to a painful joint, and assessing and adjusting force intensity. Meanwhile, the patient performs an active joint movement so that patient's symptoms are immediately relieved and the maneuvers improve pain and movement.13 Therefore, when a correct mobilization is sustained, pain-free movement is restored. The patient must repeat the movement several times to get an improvement that lasts over time.14, 15 The initial effects of MWM in adults were assessed by Teys et al16 who proved its effectiveness in increasing shoulder AROM and decreasing positional faults. Therefore, it may be an effective technique in the physical therapy treatment for shoulder dysfunction, as this addresses passive and active shoulder structures.17 However, no studies about its effectiveness for shoulder dysfunction in older adults have been found.
Considering the differences between the treatment for shoulder dysfunction in adults and older people, and the little evidence about the treatment in the aged population, it may be useful to carry out a pilot study using the Mulligan MWM technique to assess the possibility of conducting a full randomized controlled trial (RCT).
The purpose of this pilot study was to evaluate the feasibility of the methods proposed to conduct a full RCT to assess the effectiveness of Mulligan concept MWM on shoulder functionality in older adults with shoulder dysfunction. The primary objective was to evaluate the process of recruitment rates, willingness of participants to be randomized, participant attendance and adherence to interventions, assessment procedures, and implementation of MWM. The secondary aim was to undertake a preliminary comparison of patient-reported outcomes and to estimate the variability of these outcomes in older adults with shoulder dysfunction.
Methods
Study Design
This study was a feasibility study of a randomized clinical trial with concealed randomization and blinded assessment that was carried out between January 2012 and March 2013. This study was approved by Complejo Hospitalario de Toledo Human Research Ethics Committee. It was registered at the ClinicalTrials.gov register (Trial Registration: NCT2217540 https://register.clinicaltrials.gov/).
Setting
The location of this study was in 3 nursing homes in Toledo, Spain.
Recruitment Process
Study brochures were distributed to all residents of 3 different nursing homes. Announcements were posted at preferred locations to inform potential participants to attend informational sessions about the study for participants’ recruitment.
Participants
To be included in this study, participants were required to be older than 65 years, diagnosed with shoulder dysfunction18 (shoulder pain and/or limited AROM in the last 4 weeks) by their physician, dependent on at least 1 ADL, with a limited glenohumeral AROM of 25% to 75%, and a resident in the nursing homes where the study took place. According to medical records, subjects with moderate or severe cognitive impairment, specific rheumatic diseases, osteoarthritis of the glenohumeral joint or cervical spine, neoplasms, shoulder joint instability, circulatory disorders (hemophilia, clotting problems), skin problems aggravated by contact with the skin, traumas in the past month, and bilateral shoulder disorders were excluded.
Randomization
Two-hundred subjects were screened for study eligibility, and 44 met the inclusion criteria and provided their written informed consent. Participants were randomly allocated by a research assistant (MJVM) into the experimental group (EG) (n = 22) or the control group (CG) (n = 22) by selecting consecutively opaque envelopes with the name EG or CG, only unsealed by the research assistant after baseline assessment. Participant’s study identification number was then written on the envelope before opening it. The assessor (GBP) and the statistics analyst (DPM) were the 2 blinded members of the research team.
Interventions
Physical therapy interventions for the EG and CG were performed by 2 physical therapists (CLR and YCM) who have more than 5 years of experience with older adults and MWM. Before the study began, both physical therapists participated in training and consensus sessions, so the interventions were the same for both groups in the 3 nursing homes. They were the only research group members who were aware of the allocation of participants. The interventions took place 3 times a week for 2 consecutive weeks in the nursing home where each participant lived.
The intervention in the CG consisted of the physical therapy treatment standard protocol proposed by the Spanish Rheumatology Society for shoulder dysfunction, which is performed in most nursing homes in Spain.19 It consists of 30-minute sessions, with postural advices about positions to adopt while sleeping and picking up heavy objects and how to avoid worsening symptoms. Participants performed 20 repetitions of exercises in active shoulder flexion, extension, and rotation movements with 2 minutes of rest every 5 repetitions. Participants had assistance for performing movements, if necessary.
The intervention in the EG consisted of the same physical therapy standard protocol as the CG and active accessory mobilizations of the humeral head using MWM. For this technique, participants were seated on a stretcher, and the physical therapist was standing opposite to the upper extremity that was going to be treated. The internal hand of the physical therapist stabilized participants’ shoulder girdle and, with the thenar eminence of the other hand, the physical therapist performed a posterior-lateral glide of the humeral head (this direction is the most suitable for treating such shoulder limitations).13, 20 Participants were asked to flex the affected shoulder until pain started while the physical therapist sustained the gliding force to the humeral head. The physical therapist tried to maintain the glide at right angles to the plane of movement throughout the entire range while participants were requested to perform an active elevation. Participants were instructed that MWM, including shoulder movement, must be pain free and should be immediately stopped if any pain was experienced during the treatment. The MWM technique lasted around 20 minutes, in 3 sequences of 10 repetitions with a rest interval of 30 seconds between each sequence.13 Therefore, the EG intervention lasted around 50 minutes.
Both groups continued receiving the standard protocol 3 times a week during the 3-month follow-up period.
Data Collection and Outcome Assessment
Primary outcomes were feasibility of recruitment, randomization, retention, assessment procedures, and implementation of MWM.
Measurement of Recruitment and Randomization
Throughout the recruitment process, the researchers recorded the reasons for participant’s exclusions from the study or if a subject declined either to participate in the study or to be randomized to the proposed interventions groups.
Measurement of Participation
According to the current trial protocol, participants from both groups were required to enroll in each group physical therapy intervention and attend all the assessments. Information regarding participation in physical therapy sessions was collected by the physical therapist who was delivering the intervention throughout the intervention and follow-up phases. Information about subject’s participation in physical therapy assessments was collected by the blinded assessor. If a participant did not attend a session or an assessment, the reason for nonparticipation was recorded. The number of physical therapy sessions and assessment sessions each participant attended was registered.
Measurement of Adherence
According to the current trial protocol, each participant in the EG and the CG was required to perform 20 repetitions of exercises in active shoulder flexion, extension, and rotation movements, with 2 minutes of rest every 5 repetitions, 3 times a week during the 3-month follow-up. The research group considered that it would not be ethical not to treat the patients who remained symptomatic during this period. Throughout the intervention period, information regarding adherence to the intervention was recorded by the physical therapists who performed the protocol. The number of sessions wherein the participant completed the protocol and the reasons for not completing it were registered. Any problems with the performance of MWM or an adverse effect in an EG participant were also recorded.
Measurement of Clinical Outcomes
The primary outcome treatment effect measure was shoulder functionality measured with the validated Spanish version of Shoulder Disability Questionnaire (S-SDQ).21 This questionnaire is mostly used in research and clinical practice in several countries, and its scores can range from 0 to 100, where 0 = no functional limitation and 100 = affirmative to all items; so the higher the scores, the higher the disability.22, 23
Other effect treatment outcomes were glenohumeral AROM (flexion, abduction, and external and internal rotations) measured with a universal goniometer (Enraf Nonius ibérica, Madrid, Spain) and pain intensity measured with the 11-point Verbal Numeric Rating Scale for its good reliability, validity, and usefulness in older adults.24
For data collection, 4 physical therapy assessments were performed: at baseline (A0), immediately after group interventions (A1), after 1 month (A2), and after 3 months postintervention (A3). The assessor (GBP) was blinded to group assignments and carried out all the assessment measurements and prestudy training sessions with the assessment tools to maximize intrarater reliability.
Sample Size Calculation
The primary aim of this study was to pilot the methods proposed and to estimate the variability of the participant-reported outcomes to conduct a full RCT. In this context, a total of 44 participants were considered to be adequate for this purpose, as stated in some publications that concern the implementation of pilot studies.25, 26, 27
Statistical Analysis
Recruitment, participation, adherence rates, and percentage of participants randomized were presented descriptively. Descriptive statistics were also calculated to describe baseline data. The Shapiro-Wilk test was used to assess normal or not distribution, whereas the nonparametric χ2 test and the Mann-Whitney U test or parametric t test were conducted to determine whether the 2 groups differed on demographic variables and day 0 (preintervention) characteristics. The effect of the intervention in each individual was calculated taking into account the difference between baseline status and each observation period status (D1 = A1 − A0, D2 = A2 − A0 and D3 = A3 − A0). Subsequently, the effect was compared in the 3 observation periods (D1, D2, D3) between the 2 treatment groups (control and experimental ones) through a 2 × 3 analysis of variance (ANOVA) with repeated measures in individuals over different observation periods. Interaction coefficients between observation period and treatment were included to test if the differences between treatment groups changed over time. If the interaction coefficient was not significant, the ANOVA was run again only with the main effects. Distribution of residuals was checked using the Shapiro-Wilk test and normal quantile plots. Group effects with a nonparametric Kruskal-Wallis test for ranks were double checked if a significant group difference and a strong departure from normality in the residuals of the ANOVA were found. For variable pain, the differences between each postintervention assessment and preintervention pain were recorded into “reduction of pain” binary variables, with values 0 = more pain or the same pain and 1 = less pain. Then, the rate of participants who reduced their pain in both groups was compared. The risk ratio (RR) and the χ2 tests were conducted. Differences were considered statistically significant when P < .05. STATA/SE (version 12.0; StataCorp, College Station, TX, 2010) software was used for the statistical analysis.
Results
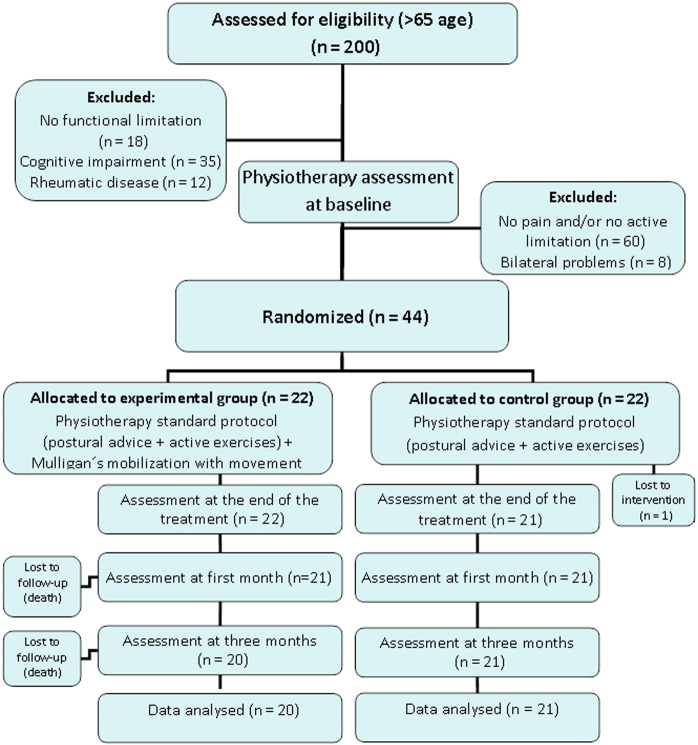
Flow of participants of this study is shown in Figure 1. Two hundred older adults were screened for eligibility, and 112 (56%) of them were potentially eligible for the study. After excluding 68 (34%) subjects, 44 (22%) participants were randomly assigned to the EG (physical therapy standard protocol + MWM) or the CG (physical therapy standard protocol). Overall, 41 participants completed all assessments: 20 in the EG and 21 in the CG. Participants in the EG received a mean amount of 6 sessions, and subjects in the CG received a mean of 5.5. Participation rates were 97.7% in the EG and 95.5% in the CG. The most common reason for nonparticipation was illness following a medical visit. No reason was given by 1 CG participant. Adherence to the protocol was 96.8% in the EG and 93.2% in the CG. The most common reason for nonadherence was illness. Non–statistically significant differences were found for participation and adherence between the 2 groups. All participants, from both groups, understood and completed the S-SDQ, and the assessor did not have any instrumental problems in assessing the shoulder AROM and pain. No adverse events related to the intervention were reported during the study period.
Fig 1.
Flow and progression of participants throughout the study. (Color version of figure appears online.)
Baseline demographics and descriptive statistics (pretreatment frequencies and pretreatment mean values [standard deviation]) for outcome variables of each group are described in Table 1. Groups showed homogeneity at baseline suggesting that randomization was adequate.
Table 1.
Comparison Between Randomized Groups at Baseline
| Demographic Variables | EG (n = 22) | CG (n = 22) | P Valuea | Total Sample Value n = 44 |
|---|---|---|---|---|
| Sex, n women (%) | 11 (50) | 11 (50) | – | 22 (50) |
| Affected limb, n right (%) | 10 (45.5) | 11 (50) | .8 | 21 (47.7) |
| Complaints > 6 mo pretreatment, n yes (%) | 22 (100) | 22 (100) | – | 44 (100) |
| Pretreatment, n yes (%) | 21 (95.5) | 22 (100) | – | 43 (97.8) |
| P Valueb | ||||
| Age (years old), mean (SD) | 84.7 (8.7) | 83.1 (7.8) | .5 | 83.9 (8.2) |
| Demographic Variables | EG (n = 22) | CG (n = 22) | P Valuea | Total Sample Value n = 44 |
| Shoulder functionality S-SDQd (points) | 58.3 (23.4) | 55.1 (29.4) | .2 | 56.7 (26.3) |
| Glenohumeral range of motion | ||||
| Flexion (°) | 101.3 (19.5) | 99.1 (22.5) | .62 | 100.2 (20.9) |
| Abduction (°) | 90.9 (19.6) | 88.2 (20) | .82 | 89.6 (19.1) |
| Internal rotation (°) | 42.3 (19.8) | 48.3 (19.6) | .88 | 47.8 (19.4) |
| External rotation (°) | 56.6 (20.1) | 60.1 (20.6) | .94 | 58.3 (20.1) |
| P Valuec | ||||
| Pain | 0.5 (3.3) | 0.2 (4.3) | .98 | 0 (3.8) |
CG, control group; EG, experimental group; S-SDQ, Shoulder Disability Questionnaire; SD, standard deviation.
Mean (standard deviation) except in the pain case that is nonparametric and wherein median (interquartile range) was used.
P value obtained by t test.
P value obtained by χ2 test.
P value Mann-Whitney U test.
From minimum [0] (no functional limitation) to maximum [100] (affirmative answer to all applicable items).
Clinical Outcomes
Mean and standard deviations of change from baseline (D1, D2, and D3) in S-SDQ and glenohumeral AROM in each group are shown in Table 2. The ANOVA did not show any statistically significant difference between treatment groups for any of the variables (all P values for the group effect were greater than .36) or a change of the difference between groups over time (all P values for the time-treatment interactions were greater than .3). Only flexion AROM showed a significant change over time (P value < .006). Fig 2 shows a box plot of the S-SDQ at each measurement point, whereas Fig 3 shows a box plot of the changes (differences) in the S-SDQ from baseline to the measurement point. In Fig 3, the boxes seem to be predominantly below 0, indicating a reduction in the S-SDQ after the intervention, but there was no clear change over time of these differences.
Table 2.
Mean (Standard Deviation) in S-SDQ and Glenohumeral AROM in Each Group
| EG |
CG |
|||||
|---|---|---|---|---|---|---|
| Measurements | D1 = Postintervention Minus Baseline (A1 − A0) | D2 = 1 mo Minus Baseline (A2 − A0) | D3 = 3 mo Minus Baseline (A3 − A0) | D1 = Postintervention Minus Baseline (A1 − A0) | D2 = 1 mo Minus Baseline (A2 − A0) | D3 = 3 mo Minus Baseline (A3 − A0) |
| Functionality S-SDQ (points) | − 14.4 (15.5) | − 16.9 (17.9) | − 13.1 (15.9) | − 8 (17.5) | − 8 (22.5) | − 11 (25) |
| Flexion range of motion (°) | 7.7 (6.8) | 8.5 (7.8) | 7 (7.2) | 6.3 (8.6) | 9.5 (11.2) | 6.3 (11) |
| Abduction range of motion (°) | 11.4 (11.3) | 11.6 (12.9) | 10.9 (12.9) | 7.8 (12.8) | 12.2 (15.8) | 9 (14.4) |
| Internal rotation range of motion (°) | 12.6 (11.8) | 11.9 (17.5) | 11 (15.1) | 6.6 (9.9) | 11.2 (13.6) | 14.4 (18.6) |
| External rotation range of motion (°) | 8.9 (9.9) | 11.8 (13.7) | 12.7 (11.9) | 7.3 (10.2) | 8.4 (13.5) | 7.6 (13.6) |
CG, control group; EG, experimental group; S-SDQ, Shoulder Disability Questionnaire; SD, standard deviation.
Fig 2.
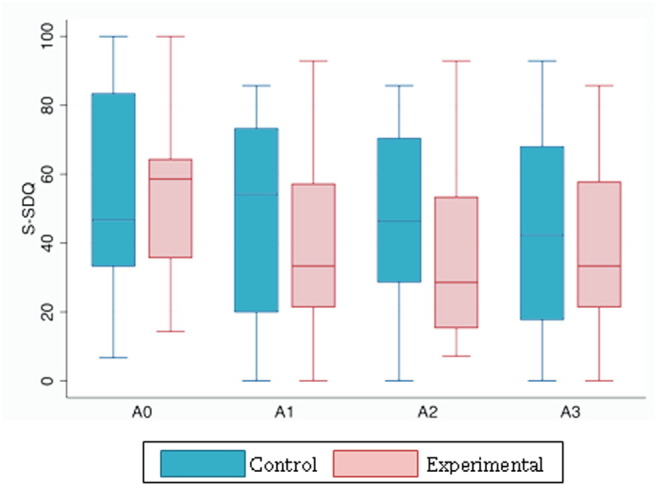
Box plot graph showing related sample of functionality (S-SDQ) at each measurement. S-SDQ, Shoulder Disability Questionnaire. (Color version of figure appears online.)
Fig 3.
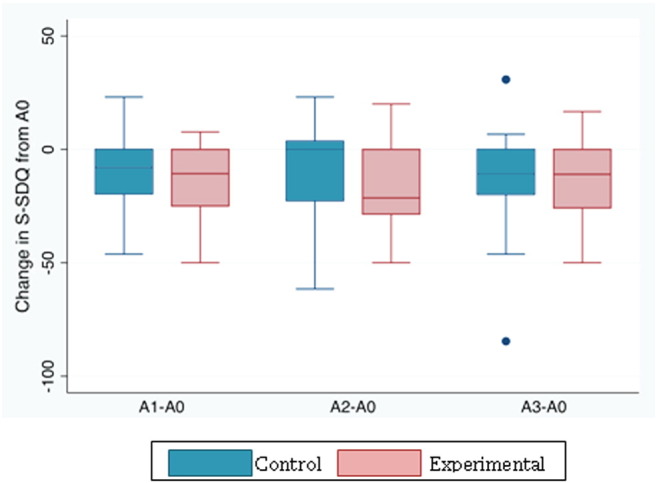
Box plot graph showing changes in S-SDQ from baseline. S-SDQ, Shoulder Disability Questionnaire. (Color version of figure appears online.)
For shoulder pain, the RR as the proportion of participants that reduced their level of pain in the EG over the proportion in the CG was calculated. At each assessment, the results were as follows: A1: RR = .32/.15 = 2.12 (P value = .20), A2: RR = .38/.25 = 1.5 (P value = .37), and A3: RR = .35/.35 = 1 (P value = 1). In the sample, participants in the EG have a higher chance of pain reduction than in the CG right after intervention, but over time, both groups began to show more similarities. However, these results are not statistically significant.
Discussion
To the best of authors’ knowledge, this is the first pilot RCT on the effect of MWM as part of a physical therapy intervention for older adults with shoulder dysfunction. Although few pilot studies about feasibility of physical therapy in older adult have been found, the current literature shows the importance of this type of studies because they can contribute to avoid mistakes in the implementation of a RCT, especially when dealing with older adults.27, 28
With reference to the specific objectives of the pilot study, recruitment for the small sample in this pilot was achieved within the time frame. A larger trial would be necessary to recruit participants from other nursing homes to obtain a larger sample. Retention rates were excellent, as all participants accepted to be randomized. Interventions and follow-up participation as well as adherence to treatment were high, and assessment procedures were adequate. High levels of participation and adherence might be related to the fact that participants’ interventions were provided in the nursing home where each participant lived, so the participation in physical therapy sessions was encouraged. Besides, during the follow-up period, physical therapists were involved in applying the intervention protocol, encouraging each participant in the attempt to maintain adherence to the intervention protocol.
Regarding clinical outcomes, the outcome measures used were acceptable in terms of completion at 3 months. Preliminary statistical analysis indicated an improvement in outcomes in both groups, although the EG showed greater functionality improvement than the CG.
Concerning MWM, a potential source of bias could be the difficulty of achieving proper alignment of the joint in the positional faults in older adults’ shoulders. Besides, the difference in endogenous analgesic systems of this population might hinder pain relief. Mulligan postulated the positional fault model about changes in the shape of joint surfaces, cartilage thickness, orientation of ligament fibers and capsules, or muscle and tendon directions and pull, which is the basis to explain the benefits of MWM on shoulder functionality.13, 29 This fact may improve functionality which can be observed in many studies about MWM on shoulder dysfunction. Patil,29 Mathew and Afsaneh,30 and Kachingwe et al31 in their studies show that a correct positional fault entails a functional improvement. Their results were similar to the ones found in this pilot study, although none of them are on older adults. Besides, the effects of sclerosing and grinding processes of the acromioclavicular joint facets and the presence of subchondral cysts and osteophytes in the glenohumeral joint, among other degenerative processes, can lead to deformations of joint structures. Therefore, these structures lose their normal alignment, leading to a misalignment of the joint which leads to a normal movement alteration.32 All these facts can disrupt the correction of the positional faults and may partially explain the results of the present study. Therefore, further investigation is needed about the degenerative effect in relation to the application of manual therapy.
According to the Mulligan concept, an appropriate joint alignment is needed to get better results in AROM. As a result, it is difficult to be sure whether the alignment is correctly performed because of the lack of stability that degenerative changes may cause in older adults.13, 32 In the present study, a non–statistically significant trend was found in AROM, except for a trend toward an increase of AROM glenohumeral flexion in the EG. Although an improvement in shoulder functionality was found, the results are not similar to other studies about Mulligan technique which state that shoulder functionality is correlated to glenohumeral AROM.31
Teys et al16 showed the effectiveness of the Mulligan technique on pain in adults younger than 60 years. Although the study had a small sample size (n = 24), statistically significant results were found concerning immediate effects after 1 MWM treatment session. Even if the neurophysiologic mechanism of MWM for pain-relief effects is not very clear, it seems that passive mobilization treatment of peripheral joints produces hypoalgesia and concurrent excitation in the motor system and the sympathetic nervous system.33 There are age-related differences in endogenous pain modulation systems; therefore, the magnitude of analgesic response is found to be significantly lower in older people.34 This might be the reason why, in the present study, no clinically significant changes in pain intensity were found.
The lack of significant difference in the clinical outcomes may also be due to small sample size. For this reason, this small-scale pilot has been carried out in order to test the feasibility of MWM for shoulder dysfunction in older adults and to provide the data to enable a power calculation to be conducted for a definitive study. A post hoc power calculation using the statistical program GRANMO (version 7.11; Barcelona, Spain, 2011) indicated that 52 participants per group would have a power of 80% to detect a difference in shoulder function between groups of 10 points on the S-SDQ, assuming a standard deviation of 17.5 points on the S-SDQ (according to findings in this pilot study), a significance level of .05, and a 7% dropout rate.
Limitations
This pilot study has some limitations. Participants were only from 3 nursing homes. If the population was larger, such as older adults living at nursing homes in the entire region, participants could have been selected in a probabilistic way, thus reducing potential selection bias.
Another limitation was that participants were not blinded to intervention. In this population, it is difficult for participants not to speak to each other to find out which treatment each participant received, although they were expressly informed not to.
Consideration for a Future Randomized Controlled Trial
This study showed that shoulder functionality improved in both groups. Therefore, perhaps EG intervention should last longer, for example, 1 month, to have better results. It seems that the 3-month postintervention period with continuing exercise may result in the groups being more equal at the end.
Although it is difficult to find a specific diagnosis for older adults with functional loss in the upper limb, the diagnosis of “shoulder dysfunction,” despite being quoted in other studies,6, 18, 35 was not the most adequate as an inclusion criterion because of the lack of specificity in symptoms. The MWM technique tries to regain mobility working very specifically on the altered structures, so it would be appropriate to use a more accurate diagnosis.
Although, in this pilot study, none of these differences were statistically significant, the consistency of the effect direction in all outcomes is encouraging and should be regarded as a stimulus to conduct a full RCT based upon the methods used and the considerations proposed in this pilot study. Notwithstanding, even if statistically significant differences were found in an adequately powered RCT, their potential clinical relevance should be further analyzed.
Conclusions
The research methods tested in this pilot RCT were suitable to conduct a full RCT. Regarding clinical changes, although non–statistically significant results were found, S-SDQ score showed better results in the EG than the CG. Moreover, the consistency of the effect direction in all outcomes may encourage researchers to conduct a full RCT to evaluate the clinical effectiveness of MWM plus the standard treatment vs the usual standard treatment for shoulder dysfunction in older adults. It would be useful to consider recruitment from multiple nursing homes, the inclusion of participants with a more accurate diagnosis, as well as increasing the number of sessions of MWM technique.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Acknowledgments
The authors are grateful to the management of the nursing home for older adults “Mercedes Patiño” in Villarrubia de Santiago, “San Juan de Dios” in Lillo, and “Rio Riansares” in Corral de Almaguer for their consent and for providing optimal conditions and the place to conduct the trial.
The authors also acknowledge the award given to this research study (the VI Physical Therapy Research Award) from Castilla-La Mancha Board of Physical Therapists.
References
- 1.Chard M.D., Hazleman R., Hazleman B.L., King R.H., Reiss B.B. Shoulder disorders in the elderly: a community survey. Arthritis Rheum. 1991;34(6):766–769. doi: 10.1002/art.1780340619. [DOI] [PubMed] [Google Scholar]
- 2.Eggermont L.H., Leveille S.G., Shi L. Pain characteristics associated with the onset of disability in older adults: the maintenance of balance, independent living, intellect, and zest in the Elderly Boston Study. J Am Geriatr Soc. 2014;62(6):1007–1016. doi: 10.1111/jgs.12848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vermeulen J., Neyens J.C., van Rossum E., Spreeuwenberg M.D., de Witte L.P. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr. 2011;11:33. doi: 10.1186/1471-2318-11-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koh E.S., Jae-Young L. The management of shoulder pain in the elderly: focusing on clinical characteristics and conservative treatment. J Korean Geriatr Soc. 2013;17(1):1–6. [Google Scholar]
- 5.Chester R., Shepstone L., Lewis J.S., Jerosch-Herold C. Predicting response to physiotherapy treatment for musculoskeletal shoulder pain: protocol for a longitudinal cohort study. BMC Musculoskelet Disord. 2013;14(1):192. doi: 10.1186/1471-2474-14-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brudvig T.J., Kulkarni H., Shah S. The effect of therapeutic exercise and mobilization on patients with shoulder dysfunction: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2011;41(10):734–748. doi: 10.2519/jospt.2011.3440. [DOI] [PubMed] [Google Scholar]
- 7.Camarinos J., Marinko L. Effectiveness of manual physical therapy for painful shoulder conditions: a systematic review. J Man Manip Ther. 2009;17(4):206–215. doi: 10.1179/106698109791352076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chou C.H., Hwang C.L., Wu Y.T. Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: a meta-analysis. Arch Phys Med Rehabil. 2012;93(2):237–244. doi: 10.1016/j.apmr.2011.08.042. [DOI] [PubMed] [Google Scholar]
- 9.de Vries N.M., van Ravensberg C.D., Hobbelen J.S., Olde Rikkert M.G., Staal J.B., Nijhuis-van der Sanden M.W. Effects of physical exercise therapy on mobility, physical functioning, physical activity and quality of life in community-dwelling older adults with impaired mobility, physical disability and/or multi-morbidity: a meta-analysis. Ageing Res Rev. 2012;11(1):136–149. doi: 10.1016/j.arr.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Knebl J.A., Shores J.H., Gamber R.G., Gray W.T., Herron K.M. Improving functional ability in the elderly via the Spencer technique, an osteopathic manipulative treatment: a randomized, controlled trial. J Am Osteopath Assoc. 2002;102(7):387–396. [PubMed] [Google Scholar]
- 11.van den Dolder P.A., Roberts D.L. A trial into the effectiveness of soft tissue massage in the treatment of shoulder pain. Aust J Physiother. 2003;49(3):183–188. doi: 10.1016/s0004-9514(14)60238-5. [DOI] [PubMed] [Google Scholar]
- 12.Graichen H., Stammberger T., Bonel H., Karl-Hans E., Reiser M., Eckstein F. Glenohumeral translation during active and passive elevation of the shoulder—a 3D open-MRI study. J Biomech. 2000;33(5):609–613. doi: 10.1016/s0021-9290(99)00209-2. [DOI] [PubMed] [Google Scholar]
- 13.Mulligan B.R. 6 ed. Orthopedic Physical Therapy Products; Wellington: 2010. Manual therapy 'NAGS', 'SNAGS', 'MWMS' etc. [Google Scholar]
- 14.Solanki D. KLE University; Belgaum, Karnataka: 2012. Effectiveness of medial Mulligan glide versus internal rotation Mulligan glide in knee osteoarthritis—randomized clinical trial. [Google Scholar]
- 15.Vicenzino B., Paungmali A., Teys P. Mulligan's mobilization-with-movement, positional faults and pain relief: current concepts from a critical review of literature. Man Ther. 2007;12(2):98–108. doi: 10.1016/j.math.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 16.Teys P., Bisset L., Vicenzino B. The initial effects of a Mulligan's mobilization with movement technique on range of movement and pressure pain threshold in pain-limited shoulders. Man Ther. 2008;13(1):37–42. doi: 10.1016/j.math.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 17.Ho C.Y., Sole G., Munn J. The effectiveness of manual therapy in the management of musculoskeletal disorders of the shoulder: a systematic review. Man Ther. 2009;14(5):463–474. doi: 10.1016/j.math.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 18.Lin J.J., Hanten W.P., Olson S.L. Shoulder dysfunction assessment: self-report and impaired scapular movements. Phys Ther. 2006;86(8):1065–1074. [PubMed] [Google Scholar]
- 19.Hombro doloroso In: Sociedad Española de Reumatología. http://www.seres/wiki/indexphp/Folleto_de_la_SER:El_Hombro_doloroso [Accessed July10th, 2014]
- 20.Smith H., Wido D.M., Kasser R.J., Rose J., DiAngelo D.J. Glenohumeral biomechanics of physical therapy mobilization techniques. In: IEEE, editor. Biomedical Engineering Conference (SBEC). 29th Southern; 2013. Biomedical Engineering Conference; 2013. pp. 69–70. [Google Scholar]
- 21.Alvarez-Nemegyei J., Puerto-Ceballos I., Guzman-Hau W., Bassol-Perea A., Nuno-Gutierrez B.L. Development of a Spanish-language version of the Shoulder Disability Questionnaire. J Clin Rheumatol. 2005;11(4):185–187. doi: 10.1097/01.rhu.0000173229.50674.31. [DOI] [PubMed] [Google Scholar]
- 22.Angst F., Schwyzer H.K., Aeschlimann A., Simmen B.R., Goldhahn J. Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society standardized shoulder assessment form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI) Arthritis Care Res (Hoboken) 2011;63(Suppl. 11):S174–S188. doi: 10.1002/acr.20630. [DOI] [PubMed] [Google Scholar]
- 23.Doner G., Guven Z., Atalay A., Celiker R. Evaluation of Mulligan's technique for adhesive capsulitis of the shoulder. J Rehabil Med. 2013;45(1):87–91. doi: 10.2340/16501977-1064. [DOI] [PubMed] [Google Scholar]
- 24.Jones K.R., Fink R., Hutt E. Measuring pain intensity in nursing home residents. J Pain Symptom Manage. 2005;30(6):519–527. doi: 10.1016/j.jpainsymman.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 25.Argimón J.M. Elsevier España; Barcelona: 2013. Métodos de investigación clínica y epidemiológica. [Google Scholar]
- 26.Leon A.C., Davis L.L., Kraemer H.C. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thabane L., Ma J., Chu R., Cheng J., Ismaila A., Rios L.P. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10(1):1–10. doi: 10.1186/1471-2288-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nyrop K.A., Muss H.B., Hackney B., Cleveland R., Altpeter M., Callahan L.F. Feasibility and promise of a 6-week program to encourage physical activity and reduce joint symptoms among elderly breast cancer survivors on aromatase inhibitor therapy. J Geriatr Oncol. 2014;5(2):148–155. doi: 10.1016/j.jgo.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 29.Patil K.K. KLE University; Belgaum, Karnataka: 2010. A comparative study between Kaltenborn mobilization and Mulligan’s mobilization with movement in treatment of frozen shoulder: randomised clinical trial. [Google Scholar]
- 30.Mathew A., Afsaneh A. A combination approach using manual therapy and exercise in the treatment of shoulder impingement syndrome. Indian J Physiother Occup Ther. 2013;7(1):87–89. [Google Scholar]
- 31.Kachingwe A.F., Phillips B., Sletten E., Plunkett S.W. Comparison of manual therapy techniques with therapeutic exercise in the treatment of shoulder impingement: a randomized controlled pilot clinical trial. J Man Manip Ther. 2008;16(4):238–247. doi: 10.1179/106698108790818314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prescher A. Anatomical basics, variations, and degenerative changes of the shoulder joint and shoulder girdle. Eur J Radiol. 2000;35(2):88–102. doi: 10.1016/s0720-048x(00)00225-4. [DOI] [PubMed] [Google Scholar]
- 33.Farrell M.J. Age-related changes in the structure and function of brain regions involved in pain processing. Pain Med. 2012;13(Suppl. 2):S37–S43. doi: 10.1111/j.1526-4637.2011.01287.x. [DOI] [PubMed] [Google Scholar]
- 34.Joshi K.C., Kumar S.P. Role of sympathetic nervous system in pain: mechanism-based examination and treatment using physical therapy: a focused review. Int J Neurol Neurosurg. 2012;4(2):53–61. [Google Scholar]
- 35.Odom C.J., Taylor A.B., Hurd C.E., Denegar C.R. Measurement of scapular asymmetry and assessment of shoulder dysfunction using the lateral scapular slide test: a reliability and validity study. Phys Ther. 2001;81(2):799–809. doi: 10.1093/ptj/81.2.799. [DOI] [PubMed] [Google Scholar]