Abstract
Chronic Fatigue Syndrome (CFS) is a multisystem illness, which may be associated with imbalances in gut microbiota. This study builds on recent evidence that sleep may be influenced by gut microbiota, by assessing whether changes to microbiota in a clinical population known to have both poor sleep and high rates of colonization with gram-positive faecal Streptococcus, can improve sleep. Twenty-one CFS participants completed a 22- day open label trial. Faecal microbiota analysis was performed at baseline and at the end of the trial. Participants were administered erythromycin 400 mg b.d. for 6 days. Actigraphy and questionnaires were used to monitor sleep, symptoms and mood. Changes in patients who showed a clinically significant change in faecal Streptococcus after treatment (responders; defined as post-therapy distribution<6%) were compared to participants who did not respond to treatment. In the seven responders, there was a significant increase in actigraphic total sleep time (p=0.028) from baseline to follow up, compared with non-responders. Improved vigour scores were associated with a lower Streptococcus count (ρ=−0.90, p=0.037). For both the responders and the whole group, poorer mood was associated with higher Lactobacillus. Short term antibiotic treatment appears to be insufficient to effect sustainable changes in the gut ecosystem in most CFS participants. Some improvement in objective sleep parameters and mood were found in participants with reduced levels of gram-positive gut microbiota after antibiotic treatment, which is encouraging. Further study of possible links between gut microorganisms and sleep and mood disturbances is warranted.
Abbreviations: CFS, Chronic Fatigue Syndrome; CNS, central nervous system; FMA, faecal microbiota analysis; HPA, hypothalamic-pituitary adrenal; POMS, Profile of Mood States; SFI, sleep fragmentation index; SOL, sleep onset latency; TST, total sleep time; WASO, wake after sleep onset; MALDI-TOF MS, matrix assisted laser desorption ionization – time of flight mass spectrometry.
Keywords: Chronic Fatigue Syndrome, Sleep, Actigraphy, Intestinal dysbiosis, Mood
1. Introduction
Chronic Fatigue Syndrome (CFS) is a multisystem illness, associated with disabling fatigue, cognitive dysfunction and sleeping disturbances. In 1992 the WHO approved the term “Chronic Fatigue Syndrome” and recognized this disorder as a neurological disease (WHO ICD-10 G93.3). CFS is characterized by persistent and relapsing fatigue, post exertional malaise (both physical and mental), cognitive and mood changes, and gastrointestinal disturbance and food intolerances. In addition, sleep disturbances and unrefreshing sleep are commonly reported by these patients [1]. While there are now internationally recognized criteria for diagnosing this disorder, the cause (or causes) remains elusive [2].
Recent developments support the model of CFS as a multisystem illness with symptoms that are due to gastrointestinal and neurotoxic features, on a background of immunological dysfunction. Importantly, discoveries in recent years reinforce the idea that CFS is associated with imbalances in intestinal microbiota (dysbiosis) [3]. Sheedy and colleagues have reported higher levels of gram-positive bacteria, particularly Enterococcus and Streptococcus spp., in CFS patients compared to controls, in whom the levels were 5.0×106 and 8.9×104 cfu/L respectively [4]. Streptococcus spp. are gram-positive, facultative anaerobic organisms and are classified as homofermenative, producing predominantly lactic acid from glucose catabolism and generally regarded as potent D- and L-lactic acid producers [4]. Increased proportions of lactic acid in the intestine may result in a change in the distribution of both the facultative anaerobic and anaerobic microbiome (the collective genomes of the microorganisms in the gut), thus giving rise to a vicious cycle. Increased distribution of lactic acid bacteria (Streptococcus, Enterococcus sp.) may lower the colonic pH [5], modify faecal microbiota metabolism, and alter intestinal epithelial barrier function, increasing passive intestinal permeability [6]. Accumulation of D-lactate in the intestine can also push absorption into the blood. Circulating D-lactate can cross the blood-brain barrier, resulting in neurological symptoms, including delirium, ataxia and slurred speech. This has been termed the D-lactate hypothesis [7]. D-lactic acid accumulation is typically found in patients with short bowel syndrome, and has been linked to cognitive and mood changes in animals [8], [9] and humans [4].
We have previously proposed a link between intestinal colonization of gram-positive bacteria and expression of CFS symptoms in a subgroup of patients [10]. Recent evidence supports a decade-old contention that intestinal dysbiosis can profoundly affect multiple aspects of sleep, mood and cognitive function [11]. The gastrointestinal system is an important organ for the equilibrium of health, and has been found to have a bidirectional relationship with the central nervous system (CNS) [12]; referred to as the “gut-brain axis”. Intestinal bacteria can communicate with the CNS through vagal sensory nerve fibres and the peripheral immune system. In patients with functional bowel disease (e.g. some CFS), increased colonization of faecal gram-positive bacteria is associated with neurologic dysfunctions (inability to concentrate, excessive irritability, confusion, impaired motor coordination [13]). Further research into the bidirectional relationship between intestinal dysbiosis and symptom expression including sleep problems [1] in patients with CFS is needed.
If altered intestinal microbiota contributes to the pathogenesis of CFS, then therapeutics that rebalance or modify intestinal microbiota may have the potential to reduce symptoms [14]. Only two studies to date have examined the effect of probiotic treatment on mood symptoms in individuals with CFS [15], [16]. In an uncontrolled study by Sullivan and colleagues, 15 CFS patients completed four weeks of probiotic therapy (Lactobacillus acidophilus and Bifidobacterium lactis). While no change in intestinal microbiota was observed, six of 15 patients reported improvements in fatigue and mood following treatment, with an overall improvement in neurocognitive function. These findings were partially replicated by Rao and colleagues [15], who reported significant decreases in anxiety symptoms in 39 CFS patients after ingesting Lactobacillus casei strain Shirtota for two months compared to placebo.
While these studies lend support to the notion that alterations in gut microbiota can change subjective symptom expression, as outlined above, it is likely that many CFS patients experience intestinal dysbiosis, warranting the use of antibiotic treatment to the return of a balanced microbial ecology. Only one pilot study has reported on symptoms in four CFS patients after three months of antibiotic treatment for Coxiella burnetti infection [17]. After treatment, patients were reported to be negative for infection, but their CFS symptoms remained unchanged. There has been no systematic study to explore real world improvements in sleep quality and daytime symptoms, following antibiotic treatment for intestinal dysbiosis in people who suffer CFS, and this area requires further research.
This study aims to determine if participants with CFS who, at baseline, are predominantly colonized with gram-positive faecal Streptococcus (determined by stool analysis and suggestive of abnormal gut functioning) will demonstrate significant improvements in sleep (measured by objective actigraphy and subjective self-reporting diary), fatigue, mood and self-reported CFS symptoms after a six-day antibiotic treatment of erythromycin. Changes in these measures with treatment will be considered separately for those who were found to (i) respond to the antibiotic treatment, by a reduction in the Streptococcus distribution, compared to those who did not respond with such reduced distribution, and (ii) the whole sample.
2. Methods
2.1. Participants
The final sample who completed the trial consisted of 22 CFS patients (5 males), aged between 23 and 66 (mean age 41.8±12.2). The inclusion criteria at entry to the study were: meet CFS criteria according to the Canadian consensus document [18]; be aged over 18 years; not currently on antibiotics and not been on antibiotics for four weeks prior to Baseline phase; not been on any non-prescription probiotics for at least two weeks prior to Baseline; not currently taking any prescription hypnotics (this does not include melatonin); no evidence of a sleep disorder (apart from insomnia); have an Epworth Sleepiness Scale score <15; agree to maintain their current intake of any over-the-counter supplements and/or permitted prescription tablets over the entire 22 day period (if relevant). If any changes were made to their current medication, they were asked to notify the researchers at the time of the change. Those who met the initial inclusion criteria were then asked to complete a Bioscreen FMA test to confirm they met the threshold gram-positive count (Streptococcus>3×105 cfu/g). Details of participant numbers meeting different screening criteria are presented in the Results. This study was approved by the institution׳s Human Research Ethics Committee, and written informed consent was obtained from all participants. The trial was registered with the Australian and New Zealand Clinical Trial Registry (ACTRN12615000457549).
2.2. Measures
Epworth Sleepiness Scale is a widely used 8-item scale for determining whether a person has excessive daytime sleepiness [19]. A score >15 indicates significant sleepiness difficulties and would be inconsistent with a CFS diagnosis without further investigation by a sleep specialist, and therefore this was used as the cut-off exclusion criteria.
The Multivariable Apnea Prediction Index is a 13 item validated measure uses an individual׳s body mass index, age, gender and scores on three questions related to sleep apnea (snorting and gasping, loud snoring, and breathing stops) to calculate the probability of sleep apnea [20]. Scores >0.5 were used as the cut-off for study exclusion.
Day & Sleep Diary A day and sleep diary was completed each morning (sleep) and night (day) for 22 days, and the data was used to assist in the interpretation of the wrist actigraphy output (e.g. time of lights out). The day diary asked participants, prior to bed, to assess various physical symptoms and selected mood and cognitive variables during the day, including 11 items from the Chalder Fatigue Scale [21], a pain rating scale (1=poor, 10=excellent), and experience of CFS symptoms (1= better than usual, 4=much worse than usual). The sleep diary asked participants to note their time of getting into bed, lights out, number of awakenings during the night, and the time they woke and got out of bed, each morning of the study. In addition, it provided subjective assessments of sleep quality, on a 10 point scale (1=poor, 10=excellent).
The Profile of Mood States Short Form (POMS; [22]) consists of 37 adjectives that are rated by subjects on a 5-point scale, over a 7 day time period. Six factors have been derived from this: tension-anxiety, depression-dejection, anger-hostility, fatigue-inertia, vigor-activity, and confusion-bewilderment.
The Symptom Severity and Severity Hierarchy Profile consists of a list of 21 common symptoms of CFS, that are rated on a four point scale (0=absent – 3=severe), and rank in order of severity [23].
An Actiwatch monitor (Respironics Actiwear 2) was used to objectively assess sleep via actigraphy, which has been used previously in this population [24]. The wrist Actiwatch was worn on the non-dominant wrist of participants for the duration of the study, and measured 24-h activity levels in 60 second epochs. An algorithm yields approximate values for sleep efficiency, sleep onset latency (SOL), wake after sleep onset (WASO), rest time (time in bed), number of wake bouts, total sleep time (TST) and sleep fragmentation index (SFI). Daytime activity and light exposure levels were also recorded (but not analyzed in this study). In order to remove any wash-in or wash-out effect of the treatment, the middle four days of actigraphy for the baseline and treatment periods was used in the analysis. The post treatment period was further divided into two four-day periods (post treatment 1 and post treatment 2).
2.3. Procedure
This study involved an open label trial over 22 days. Potential participants were recruited from the CFS Discovery Centre and cared for by one investigator (DL). They were provided information about the study from the clinic staff. Interested patients were asked to contact the researchers directly, who then mailed sleep and health screening questionnaires to the potential participants. Consent was obtained from participants who met the sleep and general health criteria. A faecal microbiota analysis (FMA) test kit was sent to each participant for analysis. Four lactic acid producing organisms (Streptococcus, Enterococcus, Lactobacillus and Bifidobacterium) from each of the submitted faecal samples were investigated by Bioscreen Pty Ltd. Participants were included in the study if the FMA test showed increased colonization of Streptococcus sp. (defined as >3×105 cfu/g of faecal sample). The prevalence of the remaining three lactic acid producing organisms, Enterococcus, Lactobacillus and Bifidobacterium, were also assessed. Faecal organisms were identified by MALDI-TOF MS (Matrix Assisted Laser Desorption Ionization- Time of Flight Mass Spectrometry). All participants included in the study were treated with erythromycin 400 mg b.d, at Day 8 for 6 days. Each participant included in the study also received an Actiwatch and completed a sleep diary each morning and evening.
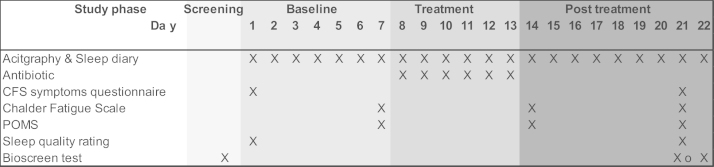
All participants followed a baseline, treatment and follow up protocol, across a total of 22 days (Fig. 1). This protocol was chosen in order to collect sufficient baseline and follow up actigraphy of 7 days (including at least 5 week days), and to allow for 6 days of antibiotic treatment.
Fig. 1.
Study protocol.
The Actiwatch was worn continuously day and night and sleep diaries completed in the morning and evening every day throughout the study. During week 1, baseline measures of sleep, symptoms and mood were recorded. On Day 8 participants started their 6- day antibiotic treatment (erythromycin). Six days of antibiotics was used as this is the standard single course of treatment used in the clinic. A reminder note was placed in the sleep diary, and participants were asked to note any discrepancies in their treatment starting day or any missed doses during the week. After the 6 days of treatment, monitoring continued for a further 7 days to assess post-intervention variables, including sleep. CFS symptoms were assessed with the Symptoms Severity Profile on Day 1 and Day 21, and mood and fatigue was assessed at day 7, 15, and 22. A second FMA was performed at the end of the trial, either on Day 22 or 23. A wash out period of 7 days between the final antibiotic dose and the follow-up FMA was chosen in order to examine the immediate impact of the treatment once the antibiotics were eliminated from the system.
2.4. Statistical analysis
Data analysis was conducted in two ways. Firstly, changes in outcome measures in patients (termed here as “responders”) who showed a significant change in Streptococcus after antibiotic treatment (defined as post-therapy percentage distribution<6%) were compared to participants who did not show such a drop in Streptococcus percentage distribution (non-responders). Secondly, whole group analyses were conducted for each outcome measure.
2.4.1. FMA
All data was checked for normality, and logarithmic transformations were conducted when this assumption was violated. The FMA data, both before and after log transformation, did not meet the normality assumption. Therefore, non-parametric Wilcoxon tests were conducted to assess differences in FMA measures from baseline to follow-up.
2.4.2. Actigraphy
Due to technical problems with the devices, actigraphy did not record for four of the participants, leaving 18 participants for the actigraphy analysis. Of these, 13 had complete data across the 28 days, and the other five had partial data for some of the protocol. All actigraphy measures were logarithmically transformed prior to analysis if they were not normally distributed. There was two outliers in the sleep efficiency and one for the total sleep time data (>3 standard deviations below the mean); these subjects were removed from these analyses. For each actigraphic variable, analyses were first conducted within each group (responders and non-responders) across baseline versus post-treatment week 2. Difference scores between baseline and post-treatment 2 for actigraphic variables were then compared between responders and non-responders. Due to small participant numbers in the responders versus non-responder groups, non-parametric Wilcoxon tests were used for both sets of analyses. Secondly, changes across the study (baseline; treatment, post treatment 1, post treatment 2) were analyzed for all the participants using repeated measures ANOVAs.
2.4.3. Subjective measures
Two participants in the responders group had only partial sleep diary data, leaving six cases in the final analysis of some of the subjective measures. For the whole sample analyses, paired samples t-test were conducted to assess differences in CFS symptoms ratings, differences in mood (POMS total score and subscales), Chalder Fatigue Scale and subjective sleep quality at baseline (Day 7), after the antibiotic phase (post treatment 1, Day 14) and at the end of the trial (post treatment 2, Day 22).
Correlation analyses (Spearman׳s tests) were conducted within the responders group and across the whole sample to examine associations between all the subjective measures, including the POMS subscales, and the three FMA results of Streptococcus, Lactobacillus and Bifidobacterium counts and percentage distribution at baseline and at the end of the trial (post treatment 2).
3. Results
3.1. Participant characteristics
A total of 70 patients were recruited in the study. Of these, eight patients reported excessive daytime sleepiness or were at risk of obstructive sleep apnea, one did not have any significant sleep issues, two were currently using sleeping medication, three were currently on antibiotic or other treatment, and one was not able to be contacted; these participants did not continue any further with the study. The remaining 55 participants completed a FMA test, and of these 30 did not have streptococcal gut dysbiosis by the study criteria, and were excluded. Twenty five participants had elevated levels of Streptococcus and/or Enterococcus spp. in the faecal samples by the FMA test. Of these 25, two discontinued prior to the trial commencing and one withdrew from the study as the patient became unwell, leaving 22 participants who completed the trial.
3.2. Faecal microbiota analysis (FMA)
Table 1 presents the data from the FMA at baseline and at the end of the trial. The percentage distribution of Streptococcus in relation to the total facultative anaerobic counts decreased significantly after antibiotic treatment (Wilcoxon=−2.17, p=0.030). While there was a reduction in Streptococcus counts this did not reach statistical significance. Thirteen of the patients showed a reduction in Streptococcus counts after treatment, whereas four patients showed an increase level of Streptococcus and four patients had no change at the end of the trial (as indicated by the exponent). Both the count and percentage distribution of Bifidobacterium declined after treatment (Wilcoxon=−2.76, p=0.006, Wilcoxon=−2.92, p=0.004 respectively). Lactobacillus count also decreased after treatment, although not significantly (p=0.060).
Table 1.
Intestinal microbial viable counts and percentage distribution of microorganisms from the FMA in CFS patients at the start and end of the trial.
| Baseline (N=22) | End of trial (N=21) | |
| Median (IQR) |
Median (IQR) |
|
| Streptococcus count | 9.83+E06 (2.3+E06–3.1+E07) | 6.87E+06 (2.6E+05–4.7E+07) |
| Enterococcus count | 0.00 (0.00–2.3E+06) | 0.00 (0.00–7.7E+04) |
| Lactobacillus count | 7.05E+05 (0.00–3.33E+08) | 5.00E+05 (0.00–7.0E+05) |
| Bifidobacterium count⁎ | 5.5E+07 (5.0E+05–1.7E+09) | 5.00E+05 (0.00–5.0E+07) |
| Streptococcus %⁎ | 72.36 (44.8–93.59) | 39.54 (1.77–96.78) |
| Enterococcus % | 0.00 (0.00–13.03) | 0.00 (0.00–0.19) |
| Lactobacillus % | 0.00 (0.00–0.22) | 0.00 (0.00–0.01) |
| Bifidobacterium %⁎ | 0.24 (0.00–10.19) | 0.00 (0.00–0.00) |
Wilcoxon test results p<0.05.
While 13 participants showed a reduction in Streptococcus only 7 of these had a significant change as defined by a percentage distribution post-therapy of less than 6% of Streptococcus after antibiotic treatment (termed here as “responders”). The remaining 14 tested at follow up did not show such a drop in Streptococcus percentage distribution (non-responders). In the 7 responders, both Streptococcus viable count (1.34E+07 to 2.20E+06; p=0.028) and percentage distribution (45.5% to 3.57%; p=0.018) significantly decreased after treatment. There was no significant difference in age (46.7±12.6, 37.5±10.5 years) between the responders and non-responders (p=0.70).
3.3. Actigraphy
Means and standard deviations of the four day averages for the actigraphy measures for responders and non-responders are shown in Table 2 for two time points. It can be seen that statistical power was reduced by the low number of responders with actigraphy data, especially at the post-treatment week 2 time point. These findings consistently suggested more improvement in actigraphic sleep with treatment in responders compared to non-responders from baseline to post-treatment 2.
Table 2.
Mean and standard deviations of actigraphy variables for responders and non-responders, and p levels for analyses of difference scores from baseline to post treatment week 2.
| Responders |
Non responders |
p# |
|||||
| N | Mean | SD | N | Mean | SD | ||
| Baseline rest time (min) | 6 | 551.41 | 71.14 | 12 | 540.98 | 49.77 | |
| Post 2 rest time | 4 | 566.31 | 46.04 | 9 | 494.20 | 71.58 | >.10 |
| Baseline sleep efficiency (%) | 6 | 68.05 | 27.65 | 11 | 77.91 | 11.19 | |
| Post treatment 2 sleep efficiency (%) | 4 | 78.42 | 9.26 | 9 | 81.70 | 9.62 | .07 |
| Baseline WASO (min) | 6 | 73.82 | 26.60 | 11 | 76.97 | 60.35 | |
| Post treatment 2 WASO (min) | 4 | 90.94 | 32.91 | 9 | 60.99 | 44.92 | >.10 |
| Baseline TST (min) | 6 | 397.14 | 159.86 | 11 | 427.16 | 63.24 | |
| Post treatment 2 TST (min) | 4 | 441.88 | 21.15 | 9 | 412.73 | 58.96 | .03 |
| Baseline SOL (min) | 6 | 42.07 | 63.57 | 11 | 20.75 | 18.88 | |
| Post treatment 2 SOL (min) | 4 | 17.75 | 19.03 | 9 | 22.55 | 22.83 | .08 |
| Baseline number of wake bouts | 6 | 32.38 | 12.33 | 12 | 25.13 | 11.17 | |
| Post 2 number of wake bouts | 4 | 37.31 | 6.85 | 9 | 24.72 | 9.43 | >.10 |
| Baseline SFI | 6 | 41.56 | 14.38 | 11 | 44.44 | 34.61 | |
| Post treatment 2 SFI | 4 | 40.85 | 10.18 | 9 | 34.66 | 19.12 | >.10 |
WASO=wake after sleep onset; TST=total sleep time; SOL=sleep onset latency; SFI = sleep fragmentation index.
Wilcoxeon test p levels, comparing the difference in responders to the difference in non-responders (from baseline to post-treatment week 2 for each group).
Total sleep time (TST) increased by 44 min from baseline to the end of the study in responders, while non-responders slept an average of 15 min less from baseline to post-treatment 2. Comparison of the difference scores in actigraphy measures from baseline to post treatment 2 between groups revealed that the mean change (improvement) scores in TST were significantly greater in the responders group compared to non-responders (Wilcoxon=−2.21, p=0.028).
For the measure of sleep efficiency (SE), baseline levels were below the “normal” threshold of 85% [25]. SE showed some improvement for the responders from baseline to post treatment week 2 compared to non-responders (Table 2). At baseline responders had about 10% less SE than non-responders and they gained this 10% by the post treatment 2 data point. In contrast, non-responders gained less than 4% improvement in SE. SE change scores tended to be greater in the responders than non-responders (p=0.07).
Sleep onset latency (SOL) tended to improve from baseline to post treatment week 2 for the responders (42.1–17.75 min; p=0.11), while no positive change was evident for non-responders (Table 2). The difference scores for responders compared to the non-responders was not significant (p=0.08). As SOL >30 min is considered abnormal, this change indicates that treatment improved the responder group mean SOL from an abnormal to normal duration [25].
Means and standard deviations of the four day averages for the actigraphy measures for the whole group and the repeated measures ANOVA results are shown in Table 3. The analyses revealed that sleep fragmentation index and time in bed showed improvements (reduction in both parameters) across the study, however these changes did not reach statistical significance. Sleep efficiency, sleep onset latency, WASO, total sleep time and the number of wake bouts did not change across the study.
Table 3.
Mean and standard deviations of actigraphy variables, averaged across each week for each study period (baseline, treatment, post treatment 1, post treatment 2). Repeated measures ANOVA results also shown.
| N | Mean | Std. deviation | |
| Baseline rest time (min) | 18 | 544.46 | 55.83 |
| Treatment week rest time (min) | 17 | 542.26 | 84.11 |
| Post 1 rest time (min) | 15 | 520.37 | 59.47 |
| Post 2 rest time (min) | 13 | 516.38 | 71.73 |
| (F2.33, 27,91=2.23, p=0.12; partial η2=0.16) | |||
| Baseline sleep efficiency (%) | 16 | 78.31 | 9.51 |
| Treatment sleep efficiency (%) | 16 | 79.96 | 7.94 |
| Post 1 sleep efficiency (%) | 14 | 82.66 | 6.26 |
| Post 2 sleep efficiency (%) | 11 | 84.15 | 3.33 |
| (F2.54, 25.38=0.90, p=0.44; partial η2=0.08) | |||
| Baseline WASO | 17 | 75.86 | 50.00 |
| Treatment WASO | 17 | 73.56 | 33.56 |
| Post 1 WASO | 15 | 60.55 | 25.90 |
| Post 2 WASO | 13 | 70.21 | 42.70 |
| (F2.19, 24.03=0.47, p=0.65; partial η2=0.04) | |||
| Baseline TST (min) | 16 | 442.64 | 56.59 |
| Treatment TST (min) | 17 | 430.63 | 66.10 |
| Post 1 TST (min) | 15 | 421.12 | 51.46 |
| Post 2 TST (min) | 13 | 416.30 | 55.20 |
| (F1.98, 19.79=1.10, p=0.35; partial η2=0.10) | |||
| Baseline SOL (min) | 18 | 27.86 | 39.07 |
| Treatment SOL (min) | 17 | 21.40 | 18.02 |
| Post 1 SOL (min) | 15 | 23.72 | 28.43 |
| Post 2 SOL (min) | 13 | 21.07 | 21.06 |
| (F2.18, 23.94=0.74, p=0.50; partial η2=0.06) | |||
| Baseline # wake bouts | 18 | 27.54 | 11.74 |
| Treatment # wake bouts | 17 | 29.47 | 9.44 |
| Post 1 # wake bouts | 15 | 27.70 | 8.91 |
| Post 2 # wake bouts | 13 | 28.60 | 10.37 |
| (F1.81, 21.67=0.52, p=0.59; partial η2=0.04) | |||
| Baseline SFI | 17 | 43.42 | 28.55 |
| Treatment SFI | 17 | 44.70 | 22.42 |
| Post 1 SFI | 15 | 33.14 | 9.86 |
| Post 2 SFI | 13 | 36.56 | 16.69 |
| (F2.41, 26.50=1.75, p=0.19; partial η2=0.14) | |||
WASO=wake after sleep onset; TST=total sleep time; SOL=sleep onset latency; SFI=sleep fragmentation index.
3.4. Subjective measures
Means and standard deviations of the subjective sleep, fatigue and mood scales rated by patients who demonstrated the required alteration of bacterial viable counts following treatment (responders) and those who did not respond to treatment are shown in Table 4. No significant change in any of the subjective measures was observed between baseline and the two follow-up points for responders versus non-responders.
Table 4.
Mean and standard deviations (SD) of CFS symptoms, sleep, fatigue and mood across the study for the responders and non-responders.
| Day 7 |
Day 15 |
Day 22 |
||||
| Responders Mean (SD) | Non responders Mean (SD) | Responders Mean (SD) | Non responders Mean (SD) | Responders Mean (SD) | Non responders Mean (SD) | |
| CFS symptoms | 30.50 (13.98) | 29.08 (13.28) | – | – | 31.00 (14.42) | 27.23 (13.36) |
| Sleep quality | 4.63 (0.86) | 4.77 (1.55) | 4.82 (1.79) | 4.88 (1.54) | 5.63 (1.15) | 5.33 (1.65) |
| Chandler Fatigue Scale | 13.01 (3.65) | 14.90 (4.13) | 15.78 (5.12) | 13.89 (2.83) | 14.64 (3.74) | 14.08 (4.92) |
| POMS total score | 44.86 (23.43) | 33.36 (24.43) | 50.30 (19.26) | 34.43 (23.33) | 40.00 (26.55) | 34.86 (23.72) |
| POMS tension | 6.29 (5.28) | 6.79 (4.42) | 9.29 (5.91) | 5.71 (5.41) | 9.00 (5.73) | 6.29 (4.86) |
| POMS confusion | 7.57 (4.86) | 6.64 (4.34) | 10.00 (4.08) | 7.00 (4.24) | 7.67 (4.72) | 6.07 (3.83) |
| POMS fatigue | 16.14 (3.98) | 12.14 (5.49) | 15.43 (5.09) | 11.86 (5.46) | 15.50 (6.16) | 12.64 (5.94) |
| POMS vigor | 4.00 (2.45) | 5.29 (3.29) | 3.57 (2.76) | 4.36 (3.61) | 6.00 (3.41) | 3.93 (3.52) |
| POMS depression | 11.57 (10.01) | 7.64 (8.16) | 13.29 (8.24) | 7.50 (6.12) | 8.33 (7.15) | 6.64 (5.88) |
| POMS anger |
|
5.86 (5.68) | 6.00 (4.93) | 6.34 (5.17) | 5.50 (3.73) | 6.93 (7.77) |
CFS symptoms=Chronic Fatigue Syndrome symptoms checklist; POMS=Profile of Mood States.
Note: for the POMS vigor subscale and sleep quality, higher scores indicate better symptoms. For all other scales, higher scores indicate worse symptoms.
Table 5 shows the scores of the CFS symptoms, subjective sleep quality, Chalder Fatigue Scale and POMS questionnaire scores for the whole group across the study. Average weekly ratings of sleep quality improved significantly across the 3 weeks. There was a significant improvement in subjective sleep quality from Day 7 to Day 22 (t(21)=−2.52, p=0.020) and from Day 15 to Day 22 (t(21)=−2.99, p=0.007). There was no significant difference in CFS symptoms total ratings score between baseline and after the end of the trial (t(18)=1.12, p=0.280). Similarly, there were no difference in any POMS subscales or Chalder Fatigue Scale scores between Day 7 and Day 14 (immediately following antibiotic treatment), or between Day 7 and Day 22 (end of the trial) (all p′s>0.05).
Table 5.
Mean and standard deviations of subjective CFS symptoms, sleep, fatigue and mood across the study.
| Day 7 (N=22) Mean (SD) | Day 15 (N=22) Mean (SD) | Day 22 (N=21) Mean (SD) | |
| CFS symptoms ratings | 29.35 (12.80) | – | 28.15 (13.11) |
| Subjective sleep quality⁎ | 4.78 (1.32) | 4.81 (1.56) | 5.38 (1.46) |
| Chandler Fatigue Scale | 14.32 (3.90) | 14.60 (3.66) | 14.30 (4.37) |
| POMS total score | 39.18 (25.38) | 38.41 (23.24) | 36.29 (23.40) |
| POMS tension | 7.05 (4.91) | 7.18 (5.71) | 7.14 (5.01) |
| POMS confusion | 7.14 (4.40) | 8.09 (4.25) | 6.47 (3.97) |
| POMS fatigue | 13.55 (5.18) | 13.05 (5.36) | 13.57 (5.85) |
| POMS vigor | 4.73 (3.03) | 4.09 (3.22) | 4.57 (3.44) |
| POMS depression | 9.59 (8.07) | 9.91 (7.43) | 7.19 (5.99) |
| POMS anger | 6.86 (5.68) | 6.77 (5.46) |
|
CFS symptoms=Chronic Fatigue Syndrome symptoms checklist; POMS=Profile of Mood States. Note: for the POMS vigor subscale and sleep quality, higher scores indicate better symptoms. For all other scales, higher scores indicate worse symptoms.
Significant difference between Day 7 and Day 15, and Day 7 and Day 22 (p<0.05).
3.5. Correlational analyses for mood
Although the sample size of responders was small (n=7), a significant, and large, negative correlation between Streptococcus viable count and POMS vigor subscale (ρ=−0.90, p=0.037) was found at post treatment 2, indicating improved mood with a lower Streptococcus count. At this time point there were strong positive correlations between Lactobacillus percentage distribution and POMS total score (ρ=0.83, p=0.042), and the confusion (ρ=0.84, p=0.036), anger (ρ=0.84, p=0.036) and depression (ρ=0.84, p=0.036) POMS subscales, and a negative correlation with POMS vigor subscale (ρ=−0.83, p=0.042). These indicate poorer mood with higher Lactobacillus in the responders at the end of the trial.
Spearman׳s correlations across the whole group similarly revealed that Lactobacillus viable counts at the end of the trial (n=21) were significantly and positively correlated with POMS total score (ρ=0.70, p=0.001), POMS confusion subscale (ρ=0.60, p=0.005), POMS tension subscale (ρ=0.47, p=0.038), POMS anger subscale (ρ=0.67, p=0.001) and POMS depression subscale (ρ=0.65, p=0.002), indicating poorer mood with higher Lactobacillus counts for all these scales. Similar results were found between POMS scores and Lactobacillus percentage distributions.
4. Discussion
This open-label trial is the first study to our knowledge to report on changes in objective and subjective sleep and self-reported symptoms in CFS patients after antibiotic treatment. The primary finding from the study was evidence of an improvement in several objective sleep parameters in participants in whom the increased colonization of lactic acid producing organisms was resolved after antibiotic treatment. A second key finding of this study was that, across the whole sample, there was an improvement in sleep quality ratings over the course of the trial. This was not, however, associated with objective improvements in sleep as measured by actigraphy. CFS symptoms and mood did not change significantly across the course of the study. Confirmation of these findings in a larger, placebo-controlled study is required.
It was anticipated in the current study that sleep (both objectively and subjectively measured) would improve after antibiotic treatment, as a result of a decreased colonization of lactic acid producing organisms. When examining those participants who showed a clinically significant improvement in faecal Streptococcus after treatment, some promising results emerged, with a significant increase of 44 min of total sleep time. There is an important body of literature supporting the link between immune dysfunction and alterations in sleep-wake behaviour in healthy populations [26], [27]. One mechanism that may mediate the sleep response to infection is an increase the expression of cytokines (including TFN-α, nitric oxide and prolactin) [28], many of which are intimately involved with sleep regulation [29]. Some researchers have suggested that it is the effect of cytokines on various organs, such as the brain, which could be an important mechanism in producing the symptoms of CFS [30], particularly in relation to sleep. Thus a potential mechanism for improvements in sleep may a reduction in circulating proinflammatory cytokines as a result of improved gut health.
Importantly, however, only a subset of 7 of the 21 participants showed a clinically significant reduction in both Streptococcus count and percentage distribution after 6 days of erythromycin treatment, and therefore this finding warrants further investigation. Four participants showed an increase in streptococcal levels at the end of the trial. It is possible that these patients were non-responsive to the antibiotics, or may be a result of an inadequate dosage or treatment duration of the antibiotic. In general, the principle of microbial suppression of anti-microbial agents is depended firstly on the achievable concentration of the anti-microbial agent in relation to the organism susceptibility profile, and secondly on the level of interference substance present at the site with the index organism(s). As the lumen of the bowel is grossly mixed, masking and/or interfering the activities of the antimicrobial agent will occur, resulting in a diminished anti-microbial effect against the organism(s), effecting a partial suppression of the index organism. The understanding of antimicrobial activities in the large bowel is at its infancy. This study highlights the importance in understanding the intestinal ecology and its management with antibiotics.
Erythromycin, a macrolide, was selected as the antibiotic of choice for the study. The antibiotic, once absorbed, is excreted into the intestine via the bile, and attains a high concentration in the colon [31]. The bacteriostatic activity of erythromycin against lactic acid producing organisms Streptococcus, Lactobacillus and Bifidobacterium is well documented [31]; but with different activities against Enterococcus. The serum achievable concentration for erythromycin is typically not adequate nor high to provide a bactericidal effect for Enterococcus-related infections. Pharmacokinetically, however, erythromycin can provide a positive suppressive effect against specific intestinal organisms in the large bowel. With the minimum inhibitory concentration (MIC) of erythromycin for the organism Enterococcus is generally between 25–50 mg/L, an oral dose of 400 mg b.d. should result a change in the organism viable count, as shown in the study. Differential responses to the erythromycin antibiotic treatment may be explained by the dosage of the antibiotic, frequency of administration, duration of treatment and/or the antibiotic appropriateness targeting multi-strains of organisms. Examining different doses of erythromycin will help to determine whether some patients require higher levels of antibiotics before treatment responses are observed. Treatment periods of 6 days of antibiotics are typically used in these patients by the clinician involved in this trial, however longer treatment periods may also be required. Probiotic use may also be beneficial in restoring gut flora as may be needed after antibiotic treatment [15]. This combined therapy may be required to observe clinical improvements in symptoms. Given the potential for events that are known to exacerbate CFS symptoms occurring that were outside of the researchers׳ control (e.g. stress, over-activity), changes in symptoms may have made any changes resulting from antibiotics difficult to detect. Assessing a larger sample of patients in longitudinal studies would help to overcome this variability in symptom expression. While erythromycin treatment reduced Streptococcus levels in some patients, it also significantly diminished levels of Lactobacillus and Bifidobacteria in these patients. Alterations in Bifidobacteria, and anaerobes in general, have been shown to amplify the domination of cytokines in the system in patients with ulcerative colitis [32]. Treatments typically incorporate both antibiotic and probiotic treatments to balance and restore microflora. Thus this single treatment alone may not have been sufficient to improve symptoms, as the system needs a balance of microbiota for optimal health. Research examining treatment outcomes of longer and more targeted therapeutic protocols with different dosages of antibiotics is needed.
Study inclusion for the current trial required self-reported unrefreshed or disturbed sleep. Although sleep disturbances are a hallmark feature of CFS [1], only a proportion of the participants had poor sleep over the baseline week of the study, as measured by actigraphy. There are a few possible explanations for this. Firstly, symptoms often fluctuate in these patients, and while generally the participants in the study had poor sleep, some participants may have had better sleep during the baseline week. Secondly, while CFS patients often report the symptom of unrefreshed sleep [1], this poorly understood sleep complaint [33] may not be accurately measured by actigraphic variables. In fact, although not presented in the results, we did not find any association between the objective actigraphy variables and subjective sleep ratings at baseline, consistent with the well-documented dissociation between objective and subjective sleep measurements [34], [35]. This raises the issue of how sleep is best assessed in CFS patients (for further discussion see [1]).
Results from the correlation analysis for both responders and the whole group revealed that higher Lactobacillus viable counts were significantly associated with poorer overall mood, including higher levels of confusion, depression and anger. In responders, lower Streptococcus viable count at the end of the trial was associated with better subjective sleep quality and vigor ratings. These findings highlight that commensal intestinal organisms, if disturbed, have the ability to influence emotional responses and behavior [36]. While the Lactobacillus finding is not in line with previous studies reporting a reduction in depressive and anxiety symptoms after probiotic treatment in both healthy [37] and CFS populations [15], the current findings do support the D-lactate hypothesis. Possible explanations for the discrepancy between this and previous studies may be differences in the specific strain of Lactobacillus, which may have more protective or pathogenic qualities [38], or an adverse interaction between increased Lactobacillus levels and other organisms in the large intestine. Most lactobacilli produce both L- and D- lactic acids. It is possible that the association shown between Lactobacillus and mood in our study may be influenced by interactions with other microbes, for example the combination of high levels of Lactobacillus and Streptococcus may be more detrimental to the host. Further to this, Rao et al. (2009) showed that supplementation with Lactobacillus also increased Bifidobacterium levels at post-testing, and this was associated with decreased anxiety in CFS patients. Thus, it is difficult to determine the direct influence of a specific microbe, given the complex and interactive nature of the gut ecosystem.
The current pilot study was conducted as an open label trial, without a placebo group. Instead, with the study design including different phases (baseline, treatment and follow up), each patient essentially became their own control. The benefit of such a design is that it reduces the between-group variability in symptom severity that is commonly found between patients with CFS. However, this design is limited by individual fluctuations in CFS patients׳ symptoms, as well as changes or differences in diet and exercise within and between participants, which may independently alter the outcome measures. There is also the possibility of placebo effects on our subjective measures. Interestingly, placebo effects in the CFS population are low with psychological interventions, but can be higher with immune-based interventions [39]. Thus, while placebo effects would also be expected to be minimized by the use of objective sleep monitoring, it could be argued that patient expectations of improved sleep may in fact lead them to become more relaxed during sleep which would be expressed through actigraphy. As discussed above, actigraphic measures may not be able to detect differences between non-restorative and restorative sleep, and thus further studies using more sensitive measures of sleep disturbance, such as polysomnography, are needed.
5. Conclusion
Key contributions of this study are the suggestion that one week of antibiotic treatment is insufficient to effect important changes in the gut ecosystem in most CFS participants, that reducing the levels of gram-positive gut microbiota is associated with some improvement in objective sleep parameters and self-reported vigor in CFS patients, and that high levels of Lactobacilli may be detrimental to mood. In sum, this pilot study provides preliminary evidence that changes to microbiota in a clinical population (CFS) may alter sleep. However, changes to the antibiotic regime, adding a placebo control group, using a larger sample size and measuring sleep polysomnographically are needed to clarify and extend these findings.
Conflict of interest
Dr. Butt is the Director of Bioscreen (Aust) Pty Ltd. who provided the analyses free of charge for the study. Dr. Lewis is the Director of CFS Discovery. Centre. Neither Dr Butt or Dr Lewis received any financial compensation from their participation in the study. None of the other authors have any actual or potential conflicts of interest to disclose.
Acknowledgements
This study was supported by Bioscreen (Aust) Pty Ltd. MJ was supported by a National Health and Medical Research Council of Australia Early Career Fellowship (APP#1036292) and a postdoctoral fellowship from Victoria University. The authors wish to thank Amy Wallis for her assistance with the interpretation of the study findings.
Footnotes
This work was conducted at Victoria University, Melbourne, Australia.
Peer review under responsibility of Brazilian Association of Sleep.
References
- 1.Jackson M., Bruck D. Sleep abnormalities in chronic fatigue syndrome/myalgic encephalomyelitis: a review. J Clin Sleep Med. 2012;8:719–728. doi: 10.5664/jcsm.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hornig M., Montoya J.G., Klimas N.G., Levine S., Felsenstein D., Bateman L. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. Sci Adv. 2015;1:e1400121. doi: 10.1126/sciadv.1400121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frémont M., Coomans D., Massart S., De Meirleir K. High-throughput 16S rRNA gene sequencing reveals alterations of intestinal microbiota in myalgic encephalomyelitis/chronic fatigue syndrome patients. Anaerobe. 2013;22:50–56. doi: 10.1016/j.anaerobe.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Sheedy J.R., Wettenhall R.E.H., Scanlon D., Gooley P.R., Lewis D.P., McGregor N. Increased D-lactic acid intestinal bacteria in patients with chronic fatigue syndrome. In Vivo. 2009;23:621–628. [PubMed] [Google Scholar]
- 5.van der Wiel-Korstanje J.A., Winkler K. The faecal flora in ulcerative colitis. J Med Microbiol. 1975;8:491–501. doi: 10.1099/00222615-8-4-491. [DOI] [PubMed] [Google Scholar]
- 6.Maes M., Mihaylova I., Leunis J.C. Increased serum IgA and IgM against LPS of enterobacteria in chronic fatigue syndrome (CFS): indication for the involvement of gram-negative enterobacteria in the etiology of CFS and for the presence of an increased gut–intestinal permeability. J Affect Disord. 2007;99:237–240. doi: 10.1016/j.jad.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 7.Bested A.C., Logan A.C., Selhub E.M. Intestinal microbiota, probiotics and mental health: from Metchnikoff to modern advances: Part II-contemporary contextual research. Gut Pathog. 2013;5:1–14. doi: 10.1186/1757-4749-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hanstock T., Clayton E., Li K., Mallet P. Anxiety and aggression associated with the fermentation of carbohydrates in the hindgut of rats. Physiol Behav. 2004;82:357–368. doi: 10.1016/j.physbeh.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Hanstock T., Mallet P., Clayton E. Increased plasma d-lactic acid associated with impaired memory in rats. Physiol Behav. 2010;101:653–659. doi: 10.1016/j.physbeh.2010.09.018. [DOI] [PubMed] [Google Scholar]
- 10.Butt HL, Dunstan RH, McGregor NR, Roberts TK. Bacterial colonosis in patients with persistent fatigue. In: Proceedings of the AHMF international clinical and scientific conference. Sydney, Australia; 2001.
- 11.Opp M.R., Toth L.A. Neural-immune interactions in the regulation of sleep. Front Biosci. 2003;8:768–779. doi: 10.2741/1061. [DOI] [PubMed] [Google Scholar]
- 12.Cryan J.F., O’Mahony S. The microbiome‐gut‐brain axis: from bowel to behavior. Neurogastroenterol. Motil. 2011;23:187–192. doi: 10.1111/j.1365-2982.2010.01664.x. [DOI] [PubMed] [Google Scholar]
- 13.Uribarri J., Oh M.S., Carroll H.J. D-lactic acidosis: a review of clinical presentation, biochemical features, and pathophysiologic mechanisms. Medicine. 1998;77:73–82. doi: 10.1097/00005792-199803000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Logan A.C., Venket Rao A., Irani D. Chronic fatigue syndrome: lactic acid bacteria may be of therapeutic value. Med. Hypotheses. 2003;60:915–923. doi: 10.1016/s0306-9877(03)00096-3. [DOI] [PubMed] [Google Scholar]
- 15.Rao A.V., Bested A.C., Beaulne T.M., Katzman M.A., Iorio C., Berardi J.M. A randomized, double-blind, placebo-controlled pilot study of a probiotic in emotional symptoms of chronic fatigue syndrome. Gut Pathogens. 2009;1:1–6. doi: 10.1186/1757-4749-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sullivan A., Nord C.E., Evengård B. Effect of supplement with lactic-acid producing bacteria on fatigue and physical activity in patients with chronic fatigue syndrome. Nutr J. 2009:8. doi: 10.1186/1475-2891-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iwakami E., Arashima Y., Kato K., Komiya T., Matsukawa Y., Ikeda T. Treatment of chronic fatigue syndrome with antibiotics: pilot study assessing the involvement of Coxiella burnetii infection. Intern Med. 2005;44:1258–1263. doi: 10.2169/internalmedicine.44.1258. [DOI] [PubMed] [Google Scholar]
- 18.Carruthers B.M., van de Sande M.I., De Meirleir K.L., Klimas N.G., Broderick G., Mitchell T. Myalgic encephalomyelitis: International Consensus Criteria. J. Intern. Med. 2011;270:327–338. doi: 10.1111/j.1365-2796.2011.02428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johns M. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 20.Maislin G., Pack A.I., Kribbs N.B., Smith P.L., Schwartz A.R., Kline LR. A survey screen for prediction of apnea. Sleep. 1995;18:158–166. doi: 10.1093/sleep/18.3.158. [DOI] [PubMed] [Google Scholar]
- 21.Chalder T., Berelowitz G., Pawlikowska T., Watts L., Wessely S., Wright D. Development of a fatigue scale. J Psychosom Res. 1993;37:147–153. doi: 10.1016/0022-3999(93)90081-p. [DOI] [PubMed] [Google Scholar]
- 22.Curran S.L., Andrykowski M.A., Studts J.L. Short form of the profile of mood states (POMS-SF): psychometric information. Psychol Assess. 1995;7:80. [Google Scholar]
- 23.Carruthers BM, Van de Sande MI. Myalgic encephalomyelitis/chronic fatigue syndrome: a clinical case definition and guidelines for medical practitioners: an overview of the canadian consensus document BM Carruthers; 2005.
- 24.Tajima S., Kuratsune H., Yamaguti K., Takahashi A., Takashima S., Watanabe Y. Estimation of fatigue state in patient with CFS using actigraph and R-R interval power spectrum analysis. Jpn J Clin Med. 2007;65:1057–1064. [PubMed] [Google Scholar]
- 25.Edinger J.D., Bonnet M.H., Bootzin R.R., Doghramji K., Dorsey C.M., Espie C.A. Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27:1567–1596. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- 26.Majde J.A., Krueger J.M. Neuroimmunology of sleep. In: D’haenen H., editor. editor. Textbook of biological psychiatry. John Wiley & Sons, Ltd; London: 2002. pp. 1247–1257. [Google Scholar]
- 27.Mullington J.M., Hinze‐Selch D., Pollmächer T. Mediators of inflammation and their interaction with sleep: relevance for chronic fatigue syndrome and related conditions. Ann N Y Acad Sci. 2001;933:201–210. doi: 10.1111/j.1749-6632.2001.tb05825.x. [DOI] [PubMed] [Google Scholar]
- 28.Krueger J.M., Majde J.A., Obál F. Sleep in host defense. Brain Behav Immun. 2003;17:41–47. doi: 10.1016/s0889-1591(02)00065-x. [DOI] [PubMed] [Google Scholar]
- 29.Kushikata T., Yoshida H., Yasuda T. Cytokines and sleep: neuro-immune interactions and regulations. In: Pandi-Perumal S., Cardinali D., Chrousos G., editors. editors. Neuroimmunology of sleep. Spinger; USA: 2007. pp. 155–166. [Google Scholar]
- 30.Maes M. Inflammatory and oxidative and nitrosative stress pathways underpinning chronic fatigue, somatization and psychosomatic symptoms. Curr Opin Psychiatr. 2009;22:75–83. doi: 10.1097/yco.0b013e32831a4728. [DOI] [PubMed] [Google Scholar]
- 31.Chelvan P., Hamilton‐Miller J., Brumfitt W. Biliary excretion of erythromycin after parenteral administration. Br J Clin Pharmacol. 1979;8:233–235. doi: 10.1111/j.1365-2125.1979.tb01007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Groeger D., O’Mahony L., Murphy E.F., Bourke J.F., Dinan T.G., Kiely B. Bifidobacterium infantis 35624 modulates host inflammatory processes beyond the gut. Gut Microbes. 2013;4:325–339. doi: 10.4161/gmic.25487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stone K.C., Taylor D.J., McCrae C.S., Kalsekar A., Lichstein K.L. Nonrestorative sleep. Sleep Med Rev. 2008;12:275–288. doi: 10.1016/j.smrv.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 34.Baker F.C., Maloney S., Driver H.S. A comparison of subjective estimates of sleep with objective polysomnographic data in healthy men and women. J Psychosom Res. 1999;47:335–341. doi: 10.1016/s0022-3999(99)00017-3. [DOI] [PubMed] [Google Scholar]
- 35.Vitiello M.V., Larsen L.H., Moe K.E. Age-related sleep change: gender and estrogen effects on the subjective–objective sleep quality relationships of healthy, noncomplaining older men and women. J Psychosom Res. 2004;56:503–510. doi: 10.1016/S0022-3999(04)00023-6. [DOI] [PubMed] [Google Scholar]
- 36.Foster J.A., Neufeld K.-A.M. Gut–brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36:305–312. doi: 10.1016/j.tins.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 37.Benton D., Williams C., Brown A. Impact of consuming a milk drink containing a probiotic on mood and cognition. Eur J Clin Nutr. 2007;61:355–361. doi: 10.1038/sj.ejcn.1602546. [DOI] [PubMed] [Google Scholar]
- 38.Harty D., Oakey H., Patrikakis M., Hume E.B.H., Knox K.W. Pathogenic potenial of lactobacilli. Int J Food Microbiol. 1994;24:179–189. doi: 10.1016/0168-1605(94)90117-1. [DOI] [PubMed] [Google Scholar]
- 39.Cho H.J., Hotopf M., Wessely S. The placebo response in the treatment of chronic fatigue syndrome: a systematic review and meta-analysis. Psychosom Med. 2005;67:301–313. doi: 10.1097/01.psy.0000156969.76986.e0. [DOI] [PubMed] [Google Scholar]