Abstract
Obstructive sleep apnea (OSA) is defined by quantifying apneas and hypopneas along with symptoms suggesting sleep disruption. Subtler forms of sleep-disordered breathing can be missed when this criteria is used. Newer technologies allow for non-invasive detection of flow limitation, however consensus classification is needed. Subjects with flow limitation demonstrate electroencephalogram changes and clinical symptoms indicating sleep fragmentation. Flow limitation may be increased in special populations and treatment with nasal continuous positive airway pressure (CPAP) has been shown to improve outcomes. Titrating CPAP to eliminate flow limitation may be associated with improved clinical outcomes compared to treating apneas and hypopneas.
Keywords: Inspiratory flow limitation, Obstructive sleep apnea, Upper airway resistance syndrome, Preeclampsia, Cyclic alternating pattern
1. Introduction
Severity of obstructive sleep apnea (OSA) has been defined by the quantity of apnea and hypopnea events (i.e. the apnea/hypopnea index, or AHI) occurring per hour of recorded sleep. Early detection of these events was accomplished via the use of oronasal thermistors. However, this technique cannot assess for respiratory effort; which has been identified to cause frequent arousals from sleep due to intrathoracic pressure swings that occur with little or no detectable change in thermistor signals [1], [2], [3]. Encephalography (EEG) arousals occurring in the absence of apneas and hypopneas with evidence of increased intrathoracic pressure swings can be included with AHI to an index known as the respiratory disturbance index (RDI). Elevation of RDI without significant increase in AHI is suggestive of upper airway flow limitation and clinically can be diagnosed as upper airway resistance syndrome (UARS). The International Classification of Sleep Disorders has placed UARS in the diagnostic category of OSA disorders [4]; however UARS may be more challenging to diagnosis. Diagnosis requires evidence of intrathoracic pressure changes culminating in arousals, defined as a respiratory effort related arousal (RERA), versus significant quantifiable reductions in air flow seen in OSA [5]. While there is strong evidence highlighting the cardiovascular risk of OSA [6], [7], it has been proposed that other forms of sleep disordered breathing (SDB) such as UARS can be correlated with excessive-daytime-sleepiness – EDS [8], [9], [10], long-term cardiovascular complications [11], [12] and significant costs to society [13], [14], [15].
The finding of RERAs has increased the sensitivity of diagnosing SDB, especially in individuals with a high clinical suspicion without polysomnogram (PSG) data supporting a clear diagnosis of OSA. The reference measurement for respiratory effort and intrathoracic pressure is esophageal pressure monitoring [16]. Chervin et al. showed a decreased esophageal pressure nadir and less sleep time with esophageal pressure more negative than 10 cm of water after adenotonsillectomy in children, suggestive of improved upper airway resistance after this procedure [17]. In clinical practice, the usage of respiratory inductance plethysmography (RIP) is accepted for measurement of respiratory effort in place of esophageal pressure monitoring by measuring thoraco-abdominal excursion during breathing versus direct measurement of intrathoracic pressure [18]. The principle of diagnosing SDB beyond quantitative airflow reductions remains important for recognition of the full spectrum pathology.
Inspiratory flow limitation (IFL) can be observed as flattening of the flow tracing on PSG. Physiologically, IFL indicates absence of an increase in flow despite an elevation in negative intrathoracic pressure indicating increasing effort [19]. Condos described this phenomenon during his study when titrating continuous positive airway pressure (CPAP) to where the inspiratory flow was rounded rather than plateaued. The flattening of the inspiratory flow is related to resistance of the airway which can occur even with application of positive airway pressure [20]. The presence of inspiratory flow limitation is vital to the understanding of UARS and subsequently as a diagnostic tool for this population.
This review on inspiratory flow limitation is intended to increase awareness of this entity, its diagnosis, and its clinical relevance. The current system using apneas and hypopneas does not capture all individuals who may be suffering from clinically significant respiratory disturbances during sleep. Often the most challenging cases faced by sleep medicine clinicians are patients with “normal” PSG findings despite presenting with symptoms consistent with OSA. With improved diagnostic measures and understanding of IFL, opportunities for successful treatment may follow.
2. Detection of IFL
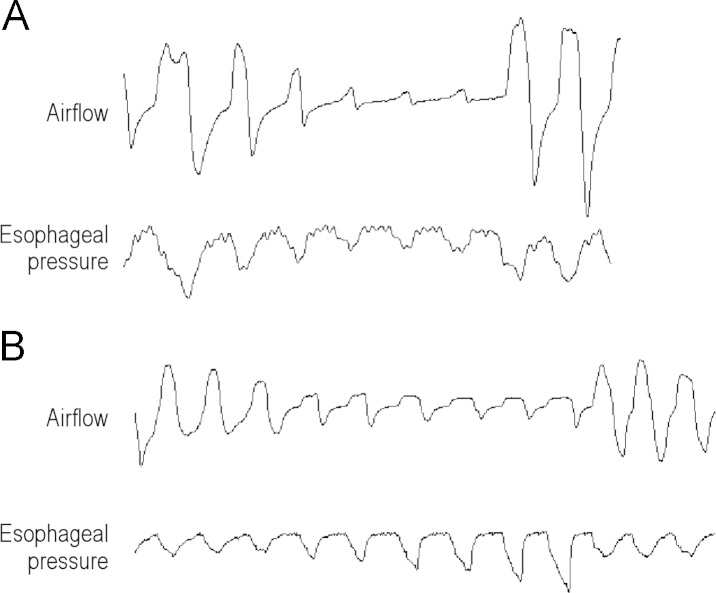
Assessing for inspiratory flow limitation requires recognition of both flow and intrathoracic pressure changes [21]. A decrease in flow normally is accompanied by a compensatory increase in intrathoracic pressure. This is illustrated in Fig. 1 in the setting of differentiating a central and obstructive event via airflow and esophageal pressure monitoring [18]. Inspiratory flow limitation, which does not meet criteria for an obstructive hypopnea is illustrated in Fig. 2. Esophageal pressure monitoring, by demonstrating intrathoracic pressure changes before EEG arousal, remains key in the clinical diagnosis of UARS [9]. As esophageal pressure monitoring may be uncomfortable and is not practical for routine monitoring, different methods ofidentification are needed. Conventional pneumotachography has demonstrated that plateaus on inspiratory flow waveforms correlate with elevated upper airway resistance [20], [21], [22]. Similar to esophageal pressure monitoring, routine application of pneumotachography is limited by discomfort with the monitoring equipment [22]. Respiratory-Inductance-Plethysmography – RIP-has also been shown to be effective for evaluation of upper airway resistance, however there is difficulty in ensuring an accurate tidal volume measurement when using this measure alone [23].
Fig. 1.
Airflow and esophageal pressure monitoring on PSG. (A) A central event with reduction in airflow without any change in esophageal pressure signal during the event. (B) A reduction in airflow with an increase in esophageal pressure for the duration of the event, indicative of an obstructive hypopnea. Flattening of the airflow signal can also be seen during the obstructive event suggestive of flow limitation.
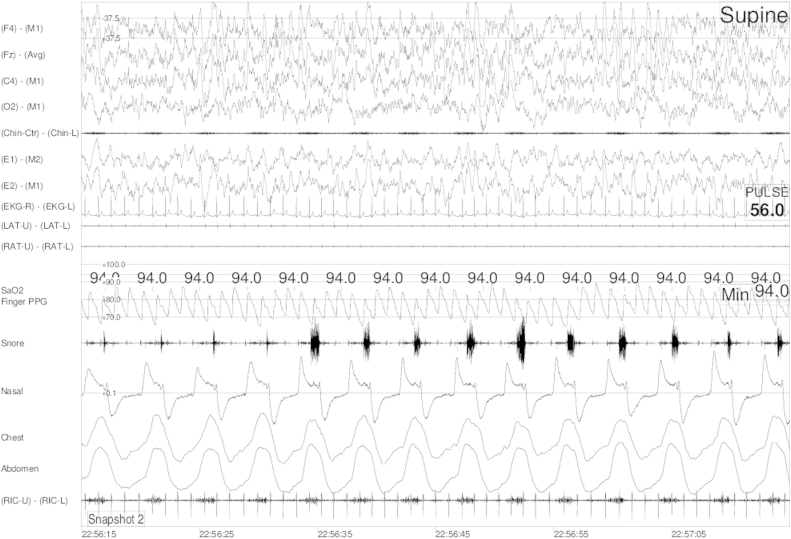
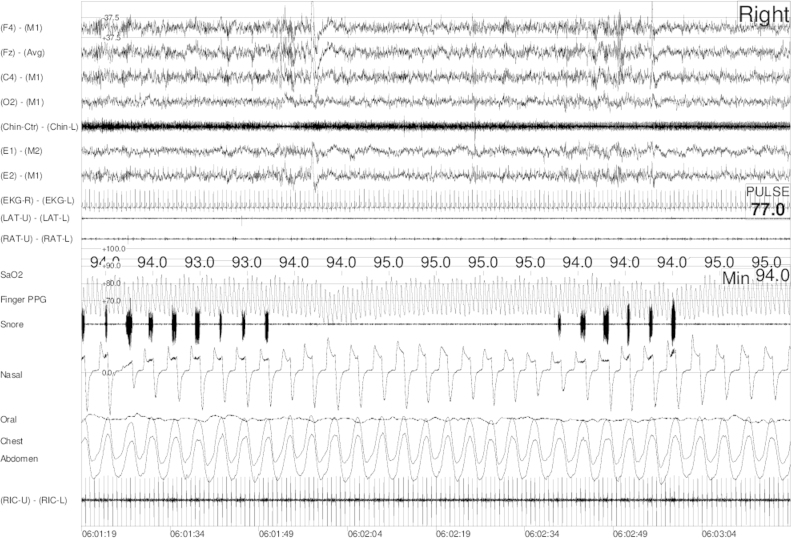
Fig. 2.
Polysomnographic recording of a subject with snoring and inspiratory flow limitation during slow-wave sleep. There is no fluctuation in oxygen saturation on pulse oximetry however flattening of the nasal waveform, coinciding with snoring, is present.
Many studies have been done assessing nasal cannula/pressure transducer system as a non-invasive assessment of IFL, in addition to its role in detection of hypopneas and apneas [2], [3], [21], [22], [24]. Ayappa et al. hypothesized that by assessing the contour of flow shape, rather than amplitude of signal, respiratory effort could be detected with similar accuracy to Pes. . Ayappa showed that assessment of RERAs via flattening of the waveform contour was nearly identical to the detection by Pes, with interclass correlation coefficient of 0.96 [24]. In addition, Hosselet showed that upper airway resistance is increased in flow limited breaths by as much as 387% [2].These results suggest that esophageal pressure monitoring may not be required in assessing for inspiratory effort, and that further evaluation of waveform contour via routinely applied nasal cannula/pressure transducer could reveal these very important events.
Comparison of different monitoring measures has been done since Ayappa׳s study showing promise of the nasal cannula/pressure transducer. Johnson et al. stimulated upper airway resistance in normal subjects with alcohol consumption and compared nasal cannula/pressure transducer with Pes, respiratory inductive plethysmography and a fourth method including a piezo-electrically treated stretch sensor adhered to the supraclavicular fossa. It was shown that nasal cannula/pressure transducer was superior to all tested modalities in detecting arousals secondary to increased upper airway resistance. Surprisingly, many events culminating in arousals were not associated initially with an increase in negative intraesophageal pressure detected by Pes; and over 90% of arousals were preceded initially by flow limitation seen via nasal pressure transducer [25].
It has been shown that additional metabolic factors exist for increasing respiratory effort during flow limited breathing. Rimpila et al. researched the relationship between transcutaneous carbon dioxide (tcCO2) level, flow limitation, and respiratory effort during sleep. It was found that flow limitation associated with increased respiratory effort correlated with tcCO2 above an individual׳s steady state during sleep. The authors noted that flow changes did exist below this tcCO2 threshold, however not with an increase in respiratory effort. It was concluded that carbon dioxide level can also be utilized to evaluate for flow limitation, and that flattening of flow contour exists without an increase in respiratory effort likely due to stabilization of breathing during sleep [26]. Abnormal flow limitation requires arousal and effort changes; therefore this type of flattening of the waveform without an increase in effort cannot be a scorable event. Carbon dioxide surrogate markers add to the understanding of flow limitation and respiratory effort, and raises questions regarding whether isolated flow limitation without RERAs or increase in arterial carbon dioxide is pathological.
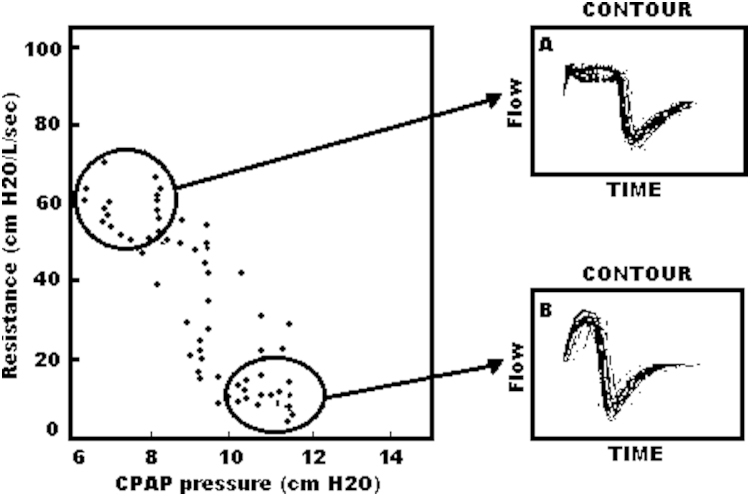
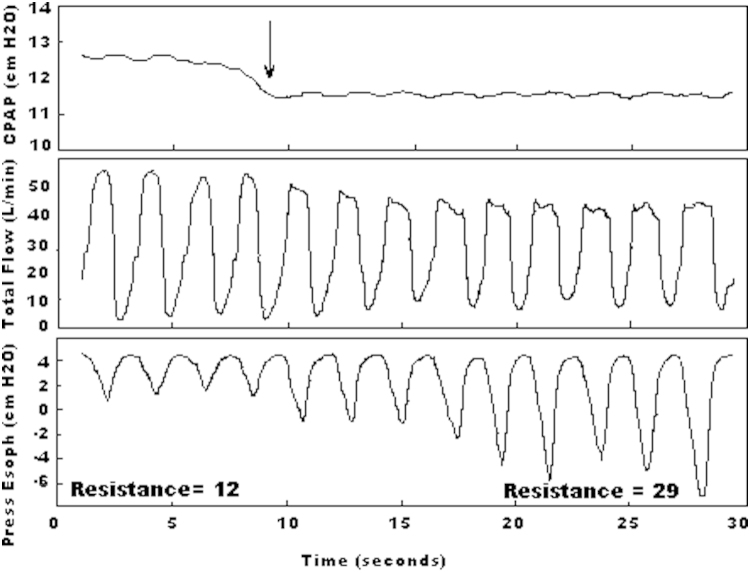
Attended CPAP titration and auto-titrating CPAP provides useful insights regarding the treatment and automated algorithms for detecting IFL, respectively. Condos has shown that rounded inspiratory flow contour with higher CPAP pressures correlates with a lower upper airway resistance. Lower CPAP pressures demonstrate higher upper airway resistance and a plateaued flow contour, illustrated in Fig. 3, Fig. 4. Flow limitation occurred when CPAP pressure when lowered concurrent with an increase in negative esophageal pressure, illustrated in Fig. 4 [20]. This work has been replicated by Montserrat et al. concluding that the rounded contour of inspiratory flow correlates with lowest esophageal pressure in CPAP titration [27]. With auto-titrating CPAP, a programmed algorithm is used to detect subtle airflow abnormalities; which differ by manufacturer of the device. This can include automated comparison of flow by the device with stored templates and corresponding actions, ongoing evaluation of flow contour with increase in pressure when flattening is detected, or small fluctuations in pressure delivery to determine the optimal pressure setting where no further improvement is flow shape identified. While cessation of apnea can be done with relative ease independent of algorithm used, each one detects IFL differently [28].
Fig. 3.
(with permission) from: Condos et al. (1994) [20]: Relationship between applied CPAP pressure and estimated resistance in data from a representative patient. Insets represent superimposed breaths from the areas circled on the left. Increase in PAP pressure improves nasal waveform and decrease in measured resistance.
Fig. 4.
(with permission) from: Condos et al. (1994) [20]: Continuous tracing of flow in one patient during transition to lower CPAP. At the arrow, CPAP was lowered by 1 cm H20. Note the increase in the esophageal pressure swings that occurs over five breaths and results in more than a twofold increase in estimated resistance. Simultaneously, the inspiratory flow contour loses its rounded shape and develops the characteristic plateau of flow limitation. )
Accurate visualization of the flow contour by nasal cannula/pressure transducer may be compromised with excessive filtering. Sampling rate should be at least 100 hZ to obtain accurate flow contour as has been described in the AASM scoring manual. Finally, the usage of PAP devices during PSG to assess for flow limitation may also be challenging depending on the PAP and PSG systems used.
Despite extensive literature supporting non-invasive techniques to assess for IFL as referenced above, this still requires manual visualization of breathing during PSG which can lead to differences in qualifying breaths as flow limited between physicians and technicians scoring events. A degree of uniformity regarding identification of flow limitation is needed; and a standardized approach to visual recognition of IFL will be vital. Objective quantification of flow limitation based on a mathematical formula using supraglottic pressure and flow data has been done, which aims to resolve the conflict of subjective differences [29]. Progress has been made to develop an automated system of calculating flow limitation using mathematical algorithms of pressure/flow relationship and waveform contour. As an example, Morgenstern et al. reports on development of a classifier to detect flow limitation non-invasively with sensitivity and specificity above manual scoring of events [30]. With a refined algorithm for detecting IFL using an upper airway pressure/flow relationship in addition to waveform contour, it is plausible that new auto-titrating CPAP algorithms can be programmed that treat IFL as effectively as obstructive apneas.
3. Characterization of IFL
A study in Turku, Finland demonstrated the spectrum of inspiratory flow signal shapes in patients with partial upper airway obstruction during sleep [31]. The upper airway is submitted to at least three forces during inspiration: phasic activity of the dilator muscles (activated at or prior to the onset of inspiration), negative airway pressure (maximal at mid-inspiration), and tracheal traction support (maximal at end-inspiration) [32], [33]. The investigators reasoned that the inspiratory flow shape could provide information on upper airway behavior throughout inspiration, similar to flow-volume loops in pulmonary function testing.
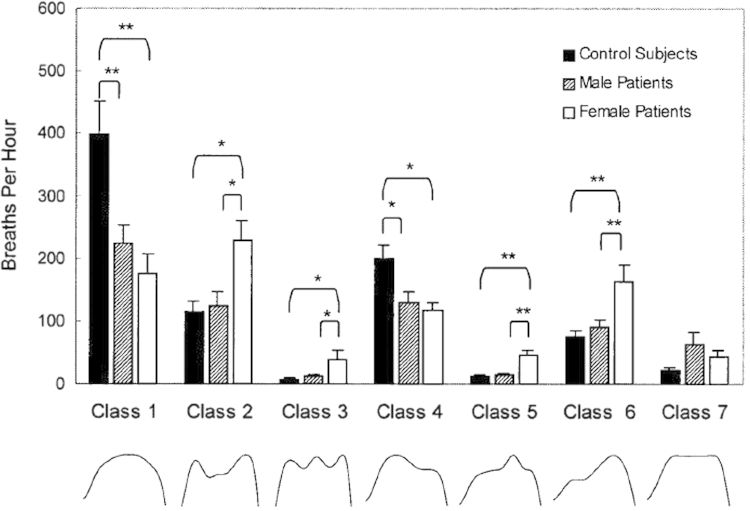
Postmenopausal women and male patients with established OSAS treated with uvulopalatopharyngoplasty were selected as patient groups. A control group was also selected. Inspiratory flow signals were evaluated on a breath-by-breath basis, and each inspiratory flow shape was extracted from an automated classifier. Recorded breaths were sorted into 7 classes of inspiratory flow shapes with their significance as it relates to anatomic flow abnormality (Table 1, Fig. 5). Based on the results seen, significant differences were seen in control subjects and patient group, but also between males and females [31].
Table 1.
Classes of inspiratory flow shapes.
| Class | Description | Interpretation | Flow limitation |
|---|---|---|---|
| 1 | Sinusoidal | Normal inspiration | No |
| 2 | Two peaks during inspiration | Upper airway reopening after initial collapse | Yes |
| 3 | Three or more (tiny) peaks | Soft-tissue vibration during inspiration | Yes |
| 4 | Peak during the initial phase followed by a plateau | Initial opening indicates effective phasic upper airway dilation | Yes/No |
| 5 | Peak at midinspiration with plateau on both sides | Significance uncertain; intensive phasic muscle activity at midinspiration (?) | Yes |
| 6 | Peak during late phase preceded by a plateau | Marked tracheal traction support during lung inflation | Yes |
| 7 | Plateau throughout inspiration | Collapse of noncompliant upper airway | Yes |
Fig. 5.
(with permission) from: Aittokallio et al. (2001) [30]: The distribution of flow shape classes in experimental and control subjects.
While this study attempts to classify flow data, correlate them with anatomical changes in the pharyngeal airway and whether it signifies flow limitation, the authors conclude that physiologic meanings cannot be reliably ascertained based on their findings alone. This work does provide a framework on which to characterize flow limitation and subsequently increase understanding of upper airway dynamics during sleep. Automated classification of inspiratory flow signals will need to be reinforced by similar manual classification in order to create a reproducible scoring system for characterizing flow limitation.
4. Epidemiology of IFL
A study using a representative population sample based on a census of Sao Paolo, Brazil evaluated the distribution of IFL in asymptomatic versus symptomatic subjects [34]. The goal was to define how much IFL exists in the general population and to determine a threshold beyond which IFL is considered pathologic.
The study took advantage of an existing epidemiologic cohort of 1,101 individuals who had undergone PSG to identify normal asymptomatic subjects. Subjects with moderate-to-severe OSA were excluded from the analysis, as IFL is unnecessary to support the diagnosis in these cases and tends to be absent in cases where apnea predominates. The scoring of IFL was performed manually by visual inspection. Periods of IFL were defined as at least four consecutive breaths showing inspiratory flattening of the airflow curve that did not meet criteria for hypopnea. Three scorers evaluated 20 studies and the inter-scorer agreement rate for percent rate of IFL was 0.950 (p<0.001). The normal group (n=163) was defined by the following criteria: (1) no known diagnosis of a sleep disorder or sleep complaints, (2) no OSA according to International Classification of Sleep Disorders (ICSD-2) criteria, and (3) no significant primary lung disease.
In the normal group, the 95th percentile for IFL was 31%. This percentage did not show a clear correlation with an increase in age, but it was significantly correlated with BMI. These results suggest that only IFL values greater than 30% should be used to support the diagnosis of SDB. Conversely, the IFL pattern cannot be used exclusively to determine abnormality, as roughly 5% of the normal population has IFL greater than 30% of the night. Despite these limitations, and lack of studies correlating IFL percentage with clinical symptoms, discussing IFL on PSG reports provides a metric that may be clinically relevant; especially in the absence of significant elevation of AHI.
5. IFL-related EEG changes during sleep
In prior studies, it has been demonstrated that UARS patients have an important disruption of sleep EEG with a continuous increase in fast range EEG frequencies, and that the sleep EEG is as disturbed with continuous IFL as it is with repetitive hypopneas [35], [36]. Black et al. showed that patients with SDB, predominantly IFL, did not re-open their airway only with presence of an alpha EEG burst; but often upper airway re-opening occurred in association with a burst of delta [37]. An alpha rhythm often followed the delta burst, but was commonly very short and did not respond to the definition of the EEG arousals from the AASM.
A large amount of work has been performed indicating that disturbance of sleep based on the sleep-EEG analysis did not respond to the definition of the EEG arousal [38]. Definitions of disturbance of sleep EEG based on specific patterns seen during non-rapid eye movement (NREM) sleep were tested and published under the label of “cyclic alternating pattern” or CAP. The CAP is a periodic EEG activity of NREM sleep characterized by sequences of transient electro-cortical events that are distinct from background EEG activity and recur at up to 1-min intervals as seen in Fig. 6 [39]. CAP activity may signify sleep stage instability, sleep disturbance, or both.
Fig. 6.
Polysomnographic recording demonstrating the cyclic alternating pattern in NREM sleep. Distinct change in EEG activity is seen in association with snoring and separated by a homogenous background activity without snoring.
A prospective, single-blinded study compared the CAP rate of subjects with UARS and controls [40]. Results of CAP analysis demonstrated a significant reduction in NREM sleep, an elevated CAP rate, and an increase in EEG arousals based on CAP rate analysis. There was a significant positive correlation between CAP rate and Epworth sleepiness scale (ESS) score.
Another study sought to define the relationship between chronic fatigue, unrefreshing sleep, and abnormal SWS involving symptomatic and asymptomatic (control) subjects by evaluating breathing using nasal cannula and Pes [36]. After performing conventional PSG scoring, Fast Fourier Transformation (FFT) was applied for investigation of the sleep EEG frequency bands. Symptomatic subjects presented an abnormal amount of IFL detected by nasal cannula monitoring and abnormal Pes recording providing evidence of increased inspiratory efforts. There was nocturnal sleep disturbances with reduction of SWS and sleep efficiency, increase in CAP rate, and FFT analysis showed an abnormal increase of the delta-1 (0.5–2 Hz) band with decrease in all other EEG bands compared to controls.
Guilleminault et al. also conducted a study involving OSA split into a hypopnea and apnea-hypopnea subgroup, UARS patients and an asymptomatic normal breathing control group matched for age and body-mass-index. The study compared the nocturnal sleep EEG after treatment using FFT to dissociate the different EEG band activity using a 4 min over-lapping time-window [40]. All SDB groups had a significantly different sleep EEG than controls, but the UARS patients were also significantly different than both OSA patients groups: There was a significant increase in both delta and alpha bandwidth powers in UARS compared to OSA, and a much higher alpha power with less delta power than controls. The conclusion of the authors was that the UARS patient demonstrated less sleep disturbance when considering the bands other than alpha, but had a much more “alert type” of EEG during the total sleep time with much higher alpha relative power leading to a maintenance of air exchange at the cost of continuous near-awakening.
These studies suggest that IFL is associated with EEG abnormalities that are likely clinically significant, however are not currently recognized as scorable events. Recognition of IFL on a qualifiable level in conjunction with associated EEG changes provides a deeper understanding of more subtle forms of SDB. This spectrum of airflow and EEG changes taken together allow for increasing sensitivity in diagnosing SDB beyond apneas.
6. IFL is associated with clinical symptoms
The bulk of research identifying comorbidities with SDB has focused on apnea and hypoxia. However, there is evidence that IFL and sleep fragmentation also may lead to problems. Patients with UARS, defined by the presence of IFL associated with EEG arousal [5], suffer from sleep disruption and poorer quality of life [41]. SDB also has been linked to insomnia, daytime fatigue and unrefreshing sleep [42]. Prior studies have demonstrated that in mild SDB with diagnosed insomnia, treatment of SDB in addition to targeted cognitive behavioral therapy leads to superior outcomes than cognitive behavioral therapy alone [43], [44].
It is important to note that thermistors were used in many studies identifying the pathologic associations of IFL. Many events characterized by thermistors as IFL today may be classified as hypopneas. While clear association between isolated IFL and clinical symptoms have not been reported, there is extensive literature outlining both positive and negative effects of arousal from sleep; which can be seen as a consequence of IFL. Eckert and Younes outlined these effects summarizing that overall the effects of arousal during sleep associated with obstructed breathing are negative. While restoration of airflow associated with arousal treats hypoxemia associated with obstruction, the frequency of arousals disrupt sleep and prevent natural progression to deeper stages of sleep [45]. In the population presenting with insomnia and fatigue, frequent arousals during sleep associated with IFL can explain symptoms often attributed to etiologies not related to sleep.
7. IFL in special populations
Further work has been done delineating an association between functional somatic syndrome, anxiety disorders and SDB. Gold has hypothesized an increase in hypothalamic–pituitary axis activity related to the effects of SDB creating a final common pathway of functional somatic syndrome and anxiety disorders; including but not limited to chronic fatigue syndrome, fibromyalgia, chronic migraine/tension headache and irritable bowel syndrome [46]. Gold has previously shown that patients with UARS complain of symptoms consistent with functional somatic syndrome more than patients with OSA [47]. This further reinforces the importance of comprehensive sleep monitoring in patients that may not present with classic symptoms of an obstructed airway. Research has shown that treatment of upper airway resistance has led to improved subjective measures of pain and fatigue in patients with chronic sinusitis [48], [49]
Snoring is common in pregnant women [50], [51]. Pre-eclampsia is a syndrome that is potentially fatal for both fetus and mother. It is related to an anomaly of insertion on placenta and associated with elevated BP that is apparent during second half of pregnancy. Edwards et al. showed that inspiratory flow limitation is common in patients at time of preeclampsia, and that short-term nasal CPAP is associated with a reduction in nocturnal blood pressure [52].
Connolly et al. conducted a prospective case control study involving normal non-pregnant women, normal pregnant women from each trimester and women with preeclampsia [53]. None of the preeclampsia patients had hypertension prior to pregnancy. All subjects underwent overnight PSG and in addition to differentiating apneas and hypopneas, a flow limitation index (“flattening index”) was calculated [54]. Each subject also had overnight intermittent blood pressure monitoring. Patients with preeclampsia spent almost one-third of the sleep period with evidence of IFL, compared to 15% in normal third-trimester women, 4.6% in normal second-trimester woman, 3.7% in normal first-trimester woman, and 1.6% in normal controls. Poyares et al. performed a randomized prospective study placing 50% of women with hypertension early during pregnancy considered “at risk for pre-eclampsia” on nasal CPAP. All women received alpha-methyl-dopa for their hypertension. Women with nasal CPAP had progressive decrease in usage of hypertensive medication, normal pregnancy, delivery and normal infants at one month of age; women in the non-treatment group had presence of IFL and/or some hypopnea during sleep, worsened blood pressure control, infants smaller than predicted based on gestational age and more medical visits during first month [55]. Further study is needed to definitively associate IFL with pathophysiologic mechanisms in preeclampsia, especially due to the multi-factorial nature of this condition.
8. Evidence supports the use of flow limitation in diagnostic criteria for sleep-disordered—breathing-SDB
While there is ample evidence that excessive flow limitation is abnormal and leads to pathologic changes in sleep and wakefulness, it is currently unclear whether including this in the diagnostic criteria for OSA would have any value. There are many available metrics to qualify SDB; including apneas, hypopneas, oxygen desaturation and arousals. Studies in children and adults have been conducted to demonstrate that the current criterion most commonly used to score abnormal breathing during sleep is inappropriate. These studies were based on several investigations in patients treated for only some of the abnormal breathing patterns during sleep; supporting the role of flow limitation as a breathing pattern important to recognize and treat for optimal clinical outcomes [31], [45], [56], [57], [58], [59].
As previously stated, investigation of the general population regarding the presence and quantity of flow limitation and study of health complaints in this sample has been a second approach done by Palombini et al. [34]. In addition, Meurice et al. conducted an experiment in which two groups of patients diagnosed with OSA were treated with different CPAP pressures. The first group was treated with CPAP pressures targeted to eliminate flow limitation and the second group treated with CPAP pressures targeted to treat apneas, hypopneas and snores. The pressure requirements for the first group were higher than for the second group; however the first group had an increase in sleep time and more consistent improvement in maintenance of wakefulness testing [59]. These results are suggestive that titration to eliminate flow limitation would lead to improved clinical outcomes.
The findings by Palombini and Meurice are further reinforced by work done by Hosselet and illustrate the need for classification systems including abnormal flow limitation. Hosselet et al. looked at different indices based on different definitions of abnormal breathing patterns in conjunction with complaints of EDS and subjects without complaints of EDS [56]. A receiver operator curve (ROC) was constructed for each defined index, and cut points were chosen to optimize the separation between EDS and non-EDS groups. The optimal cutoff for separating subjects with and without EDS was then chosen based upon calculated sensitivity and specificity. The authors had an index where all abnormal breathing patterns (apnea–hypopnea, flow limitation) were included, referred to as the RDITotal; the study demonstrated that RDITotal provided a better sensitivity and specificity than the other studied index, the most commonly used AHI.
9. Conclusion
Categorizing SDB using measures related only to reduction in airflow does not encompass the range of upper airway abnormalities, and further categorization of the full spectrum of abnormalities is needed. While many tools are available for determining respiratory effort and airflow, measurement of nasal flow by a nasal cannula pressure transducer permits recording of the respiratory flow curve. The flow tracing generated has a consistent relationship with upper airway resistance; and therefore can help assess for pathological IFL when used in conjunction with other variables, such as EEG tracing and tcCO2, in patients with mild SDB.
Analysis of multiple indices for quantifying recorded SDB has shown that scoring flow limitation events in addition to apneas and hypopneas has a better sensitivity and specificity of correlating symptoms with their respiratory causes than currently used strategies. In particular, it is necessary to detect more subtle forms of SDB such as IFL in certain patient populations that do not present with frank apneas. Standardized IFL scoring should lead to better detection and characterization of IFL. A reasonable threshold to define abnormal IFL would be greater than 30% of sleep, however other quantifiable techniques should be considered. While there is data that IFL may be linked to clinical consequences in certain circumstances, more research is needed to establish guidelines in reproducible scoring of IFL. In addition, further evidence of its negative health associations are warranted before routinely incorporating into PSG interpretation.
Conflict of interest
None.
Footnotes
Peer review under responsibility of Brazilian Association of Sleep.
References
- 1.Guilleminault C., Stoohs R., Clerk A., Simmons J., Labanowski M. A cause of excessive daytime sleepiness: the upper airway resistance syndrome. Chest. 1993;104:781–787. doi: 10.1378/chest.104.3.781. [DOI] [PubMed] [Google Scholar]
- 2.Hosselet J.J., Norman R.G., Ayappa I., Rapoport D.M. Detection of flow limitation with a nasal cannula/pressure transducer system. Am J Respir Crit Care Med. 1998;157:1461–1467. doi: 10.1164/ajrccm.157.5.9708008. [DOI] [PubMed] [Google Scholar]
- 3.Norman R.G., Ahmed M.M., Walsleben J.A., Rapoport D.M. Detection of respiratory events during NPSG: nasal cannula/pressure sensor versus thermistor. Sleep. 1997;20:1175–1184. [PubMed] [Google Scholar]
- 4.3rd ed. American Academy of Sleep Medicine; Darien, IL: 2014. International classification of sleep disorders. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pepin J.L., Guillot M., Tamisier R., Levy P. The upper airway resistance syndrome. Respiration. 2012;83:559–566. doi: 10.1159/000335839. [DOI] [PubMed] [Google Scholar]
- 6.Chung S., Yoon I.Y., Lee C.H., Kim J.W. The association of nocturnal hypoxemia with arterial stiffness and endothelial dysfunction in male patients with obstructive sleep apnea syndrome. Respiration. 2010;79:363–369. doi: 10.1159/000228905. [DOI] [PubMed] [Google Scholar]
- 7.Caples S.M., Garcia A.T., Somers V.K. Sleep-disordered breathing and cardiovascular risk. Sleep. 2007;30:291–303. doi: 10.1093/sleep/30.3.291. [DOI] [PubMed] [Google Scholar]
- 8.Fleetham J.A. A wake up call for sleep disordered breathing. Br Med J. 1997;314:839–840. doi: 10.1136/bmj.314.7084.839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guilleminault C., Stoohs R., Clerk A., Cetel M., Maistros P. A cause of excessive daytime sleepiness: the upper airway resistance syndrome. Chest. 1993;104:781–787. doi: 10.1378/chest.104.3.781. [DOI] [PubMed] [Google Scholar]
- 10.Phillipson E.A. Sleep apnea—a major public health problem. N Engl J Med. 1993;328:1271–1273. doi: 10.1056/NEJM199304293281712. [DOI] [PubMed] [Google Scholar]
- 11.Guilleminault C., Stoohs R., Shiomi T., Kushida C., Schnittger I. Upper airway resistance syndrome, nocturnal blood pressure monitoring, and borderline hypertension. Chest. 1996;109:901–908. doi: 10.1378/chest.109.4.901. [DOI] [PubMed] [Google Scholar]
- 12.Silverberg D.S., Oksenberg A. Essential hypertension and abnormal upper airway resistance during sleep. Sleep. 1997;20:794–806. [PubMed] [Google Scholar]
- 13.American Thoracic Society Sleep apnea, sleepiness, and driving risk. Am J Respir Crit Care Med. 1994;150:1463–1473. doi: 10.1164/ajrccm.150.5.7952578. [DOI] [PubMed] [Google Scholar]
- 14.Dement W.C. The perils of drowsy driving. N Engl J Med. 1997;337:783–784. doi: 10.1056/NEJM199709113371111. [DOI] [PubMed] [Google Scholar]
- 15.Mitler M.M., Miller J.C., Lipsitz J.J., Walsh J.K., Wylie C.D. The sleep of long-haul truck drivers. N Engl J Med. 1997;337:755–761. doi: 10.1056/NEJM199709113371106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Academy of Sleep Medicine Task Force Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22:667–689. [PubMed] [Google Scholar]
- 17.Chervin R.D., Ruzicka D.L., Hoban T.F., Fetterolf J.L., Garetz S.L., Guire K.E. Esophageal pressures, polysomnography, and neurobehavioral outcomes of adenotonsillectomy in children. Chest. 2012;142:101–110. doi: 10.1378/chest.11-2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berry R.B., Budhiraja R.B., Gottlieb D.J., Gozal D., Iber C., Kapur V.K. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. J Clin Sleep Med. 2012;8(5):597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sabil A., Eberhard P., Baconnier P., Benchetrit G. A physical model of inspiratory flow limitation in awake healthy subjects. Adv. Exp. Med. Biol. 2005;551:211–216. doi: 10.1007/0-387-27023-x_32. [DOI] [PubMed] [Google Scholar]
- 20.Condos R., Norman R.G., Krishnasamy I., Peduzzi N., Goldring R.M., Rapoport D.M. Flow limitation as a noninvasive assessment of residual upper-airway resistance during continuous positive airway pressure therapy of obstructive sleep apnea. Am J Respir Crit Care Med. 1994;150(2):475–480. doi: 10.1164/ajrccm.150.2.8049832. [DOI] [PubMed] [Google Scholar]
- 21.Clark S.A., Wilson C.R., Satoh M., Pegelow D., Dempsey J.A. Assessment of inspiratory flow limitation invasively and noninvasively during sleep. Am J Respir Crit Care Med. 1998;158(3):713–722. doi: 10.1164/ajrccm.158.3.9708056. [DOI] [PubMed] [Google Scholar]
- 22.Heitman S.J., Atkar R.S., Hajduk E.A., Wanner R.A., Flemons W.W. Validation of nasal pressure for the identification of apneas/hypopneas during sleep. Am J Respir Crit Care Med. 2002;166(3):386–391. doi: 10.1164/rccm.2105085. [DOI] [PubMed] [Google Scholar]
- 23.Loube D.I., Andrada T., Howard R.S. Accuracy of respiratory inductive plethysmography for the diagnosis of upper airway resistance syndrome. Chest. 1999;115:1333–1337. doi: 10.1378/chest.115.5.1333. [DOI] [PubMed] [Google Scholar]
- 24.Ayappa I., Norman R.G., Krieger A.C., Rosen A., O’Malley R.L., Rapoport D.M. Non-invasive detection of respiratory effort-related arousals (RERAs) by a nasal cannula/pressure transducer system. Sleep. 2000;23(6):763–771. doi: 10.1093/sleep/23.6.763. [DOI] [PubMed] [Google Scholar]
- 25.Johnson P., Edwards N., Burgess K., Sullivan C. Detection of increased upper airway resistance during overnight polysomnography. Sleep. 2005;28(1):85–90. doi: 10.1093/sleep/28.1.85. [DOI] [PubMed] [Google Scholar]
- 26.Rimpila V., Saaresrabta T., Huhtala H., Virkki A., Salminen A., Polo O. Transcutaneous CO2 plateau as set-point for respiratory drive during upper airway flow-limitation. Respir Physiol Neurobiol. 2013;191:44–51. doi: 10.1016/j.resp.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 27.Montserrat J., Ballester M.E., Olivi H., Reolid A., Lloberes P., Morello A. Time-course of stepwise CPAP titration: behavior of respiratory and neurological variables. Am J Respir Crit Care Med. 1995;152:1854–1859. doi: 10.1164/ajrccm.152.6.8520746. [DOI] [PubMed] [Google Scholar]
- 28.Nolan G.M., Ryan S., O’Connor T.M., McNicholas W.T. Comparison of three auto-adjusting positive pressure devices in patients with sleep apnoea. Eur Respir J. 2006;28(1):159–164. doi: 10.1183/09031936.06.00127205. [DOI] [PubMed] [Google Scholar]
- 29.Mansour K.F., Rowley J.A., Meshenish A.A., Shkoukani M.A., Badr M.S. A mathematical model to detect flow limitation during sleep. J Appl Phys. 2002;93(3):1084–1092. doi: 10.1152/japplphysiol.01140.2001. [DOI] [PubMed] [Google Scholar]
- 30.Morgenstern C., Jane R., Schwaibold M., Randerath W. Characterization of inspiratory flow limitation during sleep with an exponential model. Conf Proc IEEE Eng Med Biol Soc. 2008:2439–2442. doi: 10.1109/IEMBS.2008.4649692. [DOI] [PubMed] [Google Scholar]
- 31.Aittokallio T., Saaresranta T., Polo-Kantola P., Nevalainen O., Polo O. Analysis of inspiratory flow shapes in patients with partial upper-airway obstruction during sleep. Chest. 2001;119(1):37–44. doi: 10.1378/chest.119.1.37. [DOI] [PubMed] [Google Scholar]
- 32.Hoffstein V., Zamel N., Phillipson E.A. Lung volume dependence of pharyngeal cross-sectional area in patients with obstructive sleep apnea. Am Rev Respir Dis. 1984;130:175–178. doi: 10.1164/arrd.1984.130.2.175. (abstract) [DOI] [PubMed] [Google Scholar]
- 33.Van-de-Graff W.B. Thoracic influence on upper airway patency. J Appl Physiol. 1988;65:2124–2131. doi: 10.1152/jappl.1988.65.5.2124. (abstract) [DOI] [PubMed] [Google Scholar]
- 34.Palombini L., Tufik S., Rapoport D., Ayappa I., Guilleminault C., de Godoy L. Inspiratory flow limitation in a normal population of adults in Sao Paolo, Brazil. Sleep. 2013;36:1663–1668. doi: 10.5665/sleep.3122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guilleminault C., Kim Y.D., Chawdhuri S., Horita M., Ohayon M.M., Kushida C. Sleep and daytime sleepiness in upper airway resistance syndrome compared to obstructive sleep apnea syndrome. Eur Respir J. 2001;17:1–10. doi: 10.1183/09031936.01.17508380. [DOI] [PubMed] [Google Scholar]
- 36.Guilleminault C., Poyares D., da Rosa A., Kirisoglu C., Almeida T., Lopes M.C. Chronic fatigue, unrefreshing sleep and nocturnal polysomnography. Sleep Med. 2006;7:513–520. doi: 10.1016/j.sleep.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 37.Black J.E., Guilleminault C., Colrain I.M., Carillo O. Upper airway resistance syndrome: central EEG power and changes in breathing effort. Am J Respir Crit Care Med. 2000;162:406–411. doi: 10.1164/ajrccm.162.2.9901026. [DOI] [PubMed] [Google Scholar]
- 38.Atlas Task Force ASDA report EEG arousals: scoring rules and examples: a preliminary report from the sleep disorders atlas task force of the American Sleep Disorders Association. Sleep 2000; 15: 173-184 1992 [PubMed]
- 39.Terzano M.G., Parrino L., Sherieri A., Chervin R., Chokroverty S., Guilleminault C. Atlas, rules, and recording techniques for the scoring of cyclic alternating pattern (CAP) in human sleep. Sleep Med. 2001;6:537–553. doi: 10.1016/s1389-9457(01)00149-6. [DOI] [PubMed] [Google Scholar]
- 40.Guilleminault C., Lopes M.C., Hagen C.C., da Rosa A. The cyclic alternating pattern demonstrates increased sleep instability and correlates with fatigue and sleepiness in adults with upper airway resistance syndrome. Sleep. 2007;5:641–647. doi: 10.1093/sleep/30.5.641. [DOI] [PubMed] [Google Scholar]
- 41.Tantrakul V., Park C.S., Guilleminault C. Sleep-disordered breathing in premenopausal women: differences between younger (less than 30 years old) and older women. Sleep. 2012;13:656–662. doi: 10.1016/j.sleep.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 42.Guilleminault C., Davis K., Huynh N.T. Prospective randomized study of patients with insomnia and mild sleep disordered breathing. Sleep. 2008;31:1527–1533. doi: 10.1093/sleep/31.11.1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guilleminault C., Palombini L., Poyares D., Chowdhuri S. Part 2 comparison of nondrug treatment trials in normal breathing and UARS postmenopausal women complaining of chronic insomnia. J Psychosom Res. 2002;53:617–623. doi: 10.1016/s0022-3999(02)00463-4. [DOI] [PubMed] [Google Scholar]
- 44.Krakow B., Melendrez D., Lee S.A., Warner T.D., Clark J.O., Sklar D. Refractory insomnia and sleep-disordered breathing: a pilot study. Sleep Breat. 2004;8:15–29. doi: 10.1007/s11325-004-0015-5. [DOI] [PubMed] [Google Scholar]
- 45.Eckert D.J., Younes M.K. Arousal from Sleep: implications for obstructive sleep apnea pathogenesis and treatment. J Appl Phys. 2014;116:302–313. doi: 10.1152/japplphysiol.00649.2013. [DOI] [PubMed] [Google Scholar]
- 46.Gold A.R. Functional somatic syndromes, anxiety disorders and the upper airway: a matter of paradigms. Sleep Med Rev. 2011;15(6):389–401. doi: 10.1016/j.smrv.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 47.Gold A.R., Dipalo F., Gold M.S., O’Hearn D. The symptoms and signs of upper airway resistance syndrome: a link to the functional somatic syndromes. Chest. 2003;123(1):87–95. doi: 10.1378/chest.123.1.87. [DOI] [PubMed] [Google Scholar]
- 48.The effects of endoscopic sinus surgery on level of fatigue in patients with chronic rhinosinusitis. Am J Rhinol 2008; 22(4): 420–6. [DOI] [PubMed]
- 49.Chester A.C. Symptom outcomes following endoscopic sinus surgery. Curr Opin Otolaryngol Head Neck Surg. 2009;17(1):50–58. doi: 10.1097/MOO.0b013e32831b9e2a. [DOI] [PubMed] [Google Scholar]
- 50.Franklin K.A., Holmgren P.A., Jonsson F., Poromaa N., Stenlund H., Svanborg E. Snoring, pregnancy-induced hypertension, and growth retardation of the fetus. Chest. 2000;117:137–141. doi: 10.1378/chest.117.1.137. [DOI] [PubMed] [Google Scholar]
- 51.Loube M.D.I., Poceta J.S., Morales M.C., Peacock M.D., Littner M.M. Self-reported snoring in pregnancy: association with fetal outcome. Chest. 1996;109:885–889. doi: 10.1378/chest.109.4.885. [DOI] [PubMed] [Google Scholar]
- 52.Edwards N., Blyton D.M., Kirjavainen T., Kesby G.J., Sullivan C.E. Nasal continuous positive airway pressure reduces sleep-induced blood pressure increments in preeclampsia. Am J Respir Crit Care Med. 2000;162:252–257. doi: 10.1164/ajrccm.162.1.9905006. [DOI] [PubMed] [Google Scholar]
- 53.Connolly G., Razak A.R., Hayanga A., Russell A., McKenna P., McNicholas W.T. Inspiratory flow limitation during sleep in pre-eclampsia: comparison with normal pregnant and nonpregnant women. Eur Respir J. 2001;18(4):672–676. doi: 10.1183/09031936.01.00053501. [DOI] [PubMed] [Google Scholar]
- 54.Teschler H., Berthon-Jones M., Thompson A., Henkel A., Henry J., Konietzko N. Automated continuous positive airway pressure titration for obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 1996;154:734–740. doi: 10.1164/ajrccm.154.3.8810613. [DOI] [PubMed] [Google Scholar]
- 55.Poyares D., Guilleminault C., Hachul H., Fujita L., Takaoka S., Tufik S. Pre-eclampsia and nasal CPAP (part 2) hypertension during pregnancy, chronic snoring and early nasal CPAP intervention. Sleep Med. 2007;9:15–21. doi: 10.1016/j.sleep.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 56.Hosselet J.J., Ayappa I., Norman R., Krieger A., Rapoport D. Classification of Sleep-disordered breathing. Am J Respir Crit Care Med. 2001;163(2):398–405. doi: 10.1164/ajrccm.163.2.9808132. [DOI] [PubMed] [Google Scholar]
- 57.Guilleminault C., Li K.K., Khramtsov A., Pelayo R., Martinez S. Sleep disordered breathing: surgical outcome in prebutertal children. Laryngoscope. 2004;114:132–137. doi: 10.1097/00005537-200401000-00024. [DOI] [PubMed] [Google Scholar]
- 58.Tantrakul V., Guilleminault C. Chronic sleep complaints in premenopausal women and their association with sleep-disordered breathing. Lung. 2009;187:82–92. doi: 10.1007/s00408-009-9137-7. [DOI] [PubMed] [Google Scholar]
- 59.Meurice J.C., Paquereau J., Denjean A., Patte F., Series F. Influence of correction of flow limitation on continuous positive airway pressure efficiency in sleep apnoea/hypopneoa syndrome. Eur Resp J. 1998;11:1121–1127. doi: 10.1183/09031936.98.11051121. [DOI] [PubMed] [Google Scholar]