Abstract
Central vein stenosis is common because of the placement of venous access and cardiac intravascular devices and compromises vascular access for dialysis. Endovascular intervention with angioplasty and/or stent placement is the preferred approach, but the results are suboptimal and limited. Primary patency after angioplasty alone is poor, but secondary patency can be maintained with repeated angioplasty. Stent placement is recommended for quick recurrence or elastic recoil of stenosis. Primary patency of stents is also poor, though covered stents have recently shown better patency than bare metal stents. Secondary patency requires repeated intervention. Recanalization of occluded central veins is tedious and not always successful. Placement of hybrid graft-catheter with a combined endovascular surgical approach can maintain patency in many cases. In the presence of debilitating symptoms, palliative approach with endovascular banding or occlusion of the access may be necessary. Prevention of central vein stenosis is the most desirable strategy.
Keywords: Angioplasty, Central vein stenosis, Hybrid graft–catheter device, Stent placement, Vascular access for hemodialysis
Introduction
Central veins are commonly injured as a result of placement of intravascular devices and vascular access for a critical illness and for performance of hemodialysis (HD). Nearly 80% of patients with end-stage renal disease in the United States initiate dialysis using a catheter, and consequently, central vein injury and subsequent restorative response leading to central vein stenosis (CVS) are extremely common. Central veins are generally obscured by the bony skeleton and are difficult to approach surgically. Hence, endovascular intervention with angioplasty and/or stent placement becomes a logistically more amenable approach for treatment of CVS. However, anatomically and functionally, central veins have several important characteristics including the size, elasticity, curvature, and amount of blood flow that make treatment and maintenance of their patency after intervention difficult. This article will describe approaches to endovascular intervention in different clinical scenarios, which should be planned carefully.
Preintervention planning for CVS
There are several important considerations before formulating a management plan for CVS.
Asymptomatic versus symptomatic CVS
This is a crucial consideration before planning an intervention because central veins are more elastic and prone to recoil. An intravascular ultrasound study showed immediate recoil in >50% of central lesions [1]. Because of the elasticity of such lesions, stent placement is more likely to be required after angioplasty. At present, the natural history of angioplasty and stent placement are compromised by frequent and rapid recurrence. It is also possible that an asymptomatic lesion can become symptomatic after the intervention. Indeed, stenosis has been shown to progress faster after intervention [2]. Thirty-five asymptomatic HD patients with arteriovenous (AV) graft and >50% CVS underwent 86 venograms. Of the 28% of patients not undergoing intervention, no one progressed to symptoms, stent placement, or additional CVS. However, of the 72% of the patients undergoing percutaneous angioplasty (PTA), 8% experienced acceleration of CVS requiring further interventions. At the same time, a rather high residual stenosis (40%) in the intervention group was potentially indicative of worse prognosis to begin with, making it difficult to compare the 2 groups. Certainly, it is possible that angioplasty can aggravate the venous response and accelerate the stenotic process. The mechanism of angioplasty itself involves cracking and fissuring of the vessel intima which can incite accelerated neointimal hyperplasia, and recurrent lesions after angioplasty have been shown to have more aggressive neointimal hyperplasia with higher proliferative index than the primary lesion [3]. Thus, higher elasticity and potential for worse recurrent neointimal hyperplasia should deter intervention in asymptomatic or mildly symptomatic CVS. These patients require careful follow-up as worsening symptoms would require intervention.
Availability of other access options
It is important to plan for a backup option in case the CVS interventions were to fail. All available options should be considered including reduction of access flow, placement of hybrid catheter graft, or surgical bypass if another potential site for access placement is unavailable. Consideration of alternate method of renal replacement therapy should always be a part of the discussion.
Availability of local expertise and logistics for managing CVS
Complexity of CVS requires a multidisciplinary approach—ranging from percutaneous to open intervention. Availability of expertise will obviously define the final approach. Formation of a multidisciplinary team for discussion of challenging vascular access cases will facilitate interaction of all practitioners involved in the care of the patient. As newer technologies become available, it will be important to conduct clinical trials that use standard criteria to define severity and outcome.
Endovascular intervention for CVS
Endovascular approaches to correction of CVS remain limited, suboptimal, and possibly even detrimental in certain cases. As mentioned earlier, more aggressive neointimal hyperplasia and proliferative lesions were found in restenotic areas after angioplasty than in the original stenotic lesions [3]. Consequently, endovascular intervention for CVS requires careful planning while using restraint when clinically feasible and acceptable.
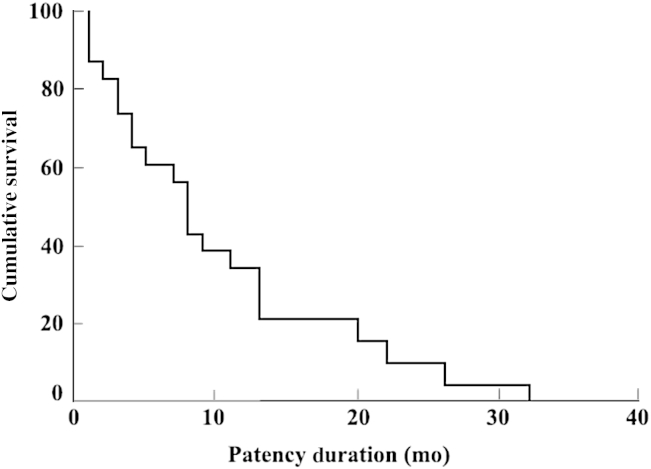
Percutaneous angioplasty
PTA with or without stent placement has been the recommended preferred approach to CVS. The guideline 20 of Kidney Disease Outcomes Quality Initiative (K/DOQI) suggests that the percutaneous intervention with transluminal angioplasty is the preferred treatment for CVS [4]. PTA has a very high initial technical success rates, ranging from 70% to 90% [5], [6], [7], [8], [9], [10], [11]. The unassisted patency rates reported after PTA have varied from 23% to 63% at 6 months and cumulative patency rates from 29% to 100%. At 12 months, the unassisted patency rate after PTA has ranged from 12% to 50% and cumulative patency rate from 13% to 100%. A more recent study using high-pressure balloons noted better results with PTA alone, with unassisted patency rate of 60% at 6 months and 30% at 12 months (Fig. 1) [12]. It is to be noted that the published studies in CVS used criteria that are not uniform in reporting the description of lesion, severity, or outcome and have been conducted in variable demographics using variable technique and equipment with resultant wide variation among the results of these studies. Better results from a second more recent study [10] also suggest presence of changing variables. It is to be noted that the secondary patency can be significantly better with repeated angioplasty, even without the use of stent. It is also difficult to compare PTA or stent placement because of the reporting issues previously discussed.
Figure 1.
Kaplan–Meier curve of post-PTA primary patency duration after angioplasty for CVS.
CVS, central vein stenosis; PTA, percutaneous angioplasty.
Note. From “Endovascular treatment of central venous stenoses in patients with dialysis shunts”, by E. Buriánková, M. Köcher, P. Bachleda, P. Utíkal, Z. Kojecký, M. Cerná, M. Herman, 2003, Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub, 147, p. 203–206. Doi: 10.5507/bp.2003.030. Copyright 2003, Biomedical Papers. Reprinted with permission.
There remain drawbacks of angioplasty approach to CVS management. As mentioned, intravascular ultrasound study after angioplasty of central veins has shown that central veins are much more likely to recoil than the peripheral veins [1]. Thus, the success of PTA often depends on the elastic or nonelastic nature of the lesion, which may have different structural characteristics of the stenosis. In addition, accelerated neointimal hyperplasia and faster progression of asymptomatic lesions after angioplasty should curb the enthusiasm to intervene in such lesions without significant rationale [2], [3].
Stents
Treatment of CVS is challenging, and stents for CVS were used because of poor long-lasting results of PTA alone [13]. Guidelines for CVS recommend placement of a stent for elastic recoil of the vein that leads to significant residual stenosis after PTA or for lesions recurring within 3 months after angioplasty [4], [14]. Self-expandable stents can be placed with a high degree of technical success, and use of self-expanding metallic stents for elastic lesions has been associated with better outcomes than angioplasty alone.
Stents can be used in 2 scenarios:
-
1
Primary stent placement after PTA without waiting for recurrence
Primary angioplasty (PTA) with primary stent placement (PTS) has been considered in an attempt to improve short- and long-term results. The outcomes of primary PTA and PTS were compared at a tertiary referral academic medical center via a retrospective analysis of database of consecutive HD patients from 1995 to 2003 [11]. After primary high-pressure balloon angioplasty, stenting (PTS) was used for failed or suboptimal angioplasty in 26 patients with 26 CVS. PTA was done in 47 patients with 49 CVS. The stent group underwent 71 percutaneous interventions per stenosis (average, 2.7 ± 2.4 interventions), and the PTA group underwent 98 interventions per stenosis (average, 2.0 ± 1.6 interventions). Primary patency was equivalent between groups by Kaplan–Meier analysis, with 30-day rates of 76% for both groups and 12-month rates of 29% for PTA and 21% for PTS (P = 0.48). Assisted primary patency was also equivalent (P = 0.08), with a 30-day patency rate of 81% and 12-month rate of 73% for the PTA group versus PTS assisted patency rates of 84% at 30 days and 46% at 12 months. Ipsilateral HD access survival was equivalent between groups. The authors concluded that PTA or PTS for CVS was safe, with low rates of technical failure, required multiple additional interventions, and neither modality offered durable outcomes. Furthermore, PTS did not improve on the patency rates more than PTA and did not add to the longevity of ipsilateral HD access sites. However, the study displays the inherent dilemma of comparing patients who responded to PTA and those who did not and underwent stent placement for that reason. Inherent severity and nature of resistant lesions make the comparison of these populations difficult and unfair. It is likely that the lesions undergoing primary stenting would have suffered early occlusion without stenting because of suboptimal results, and the study could not provide a true comparison of primary angioplasty with primary stenting of lesions that actually were successfully treated with PTA alone.
-
2
Stent placement after failure or recurrence of CVS
Stents are commonly used for difficult or failed lesions with angioplasty alone, and primary stenting is not common. The technical success rates for stents are usually quite good. However, the primary and secondary patency of stents is limited, probably because of the difficult and more severe or recurrent nature of the lesions requiring stent placement. Some initial studies showed promisingly good results with the use of stainless steel stents [15]. However, other studies showed only marginal results of such stents [16], [17]. A recent retrospective analysis of the nitinol shape memory alloy stents showed a significantly higher primary patency in central and peripheral veins though a systematic study of such stents has not been performed [18]. It is difficult to compare results of studies done over a period because stainless steel stents were used in earlier studies and more advanced stents were used in the later study, which may be responsible for better results. Irrespective of the primary technical success, repeated interventions can provide a significantly longer assisted patency. This may be appropriate in many clinical circumstances with end-stage vascular access.
In more recent literature, use of covered stents (also known as stent grafts or endografts) has shown promise [19], [20]. The technical success rate is high, and primary and assisted patency rates are significantly better than the bare metal stents. The graft material provides a relatively inert and stable matrix for endothelialization, thereby reducing restenosis. The results in salvaging occluded veins remain worse than the results of stent placement in stenosed veins. Even though stents have limitations (migration, fracture, intrastent neointimal hyperplasia, and appearance of unrelated stenosis in the access circuit leading to access failure), stent placement can provide an immediate therapy for access salvage in difficult cases.
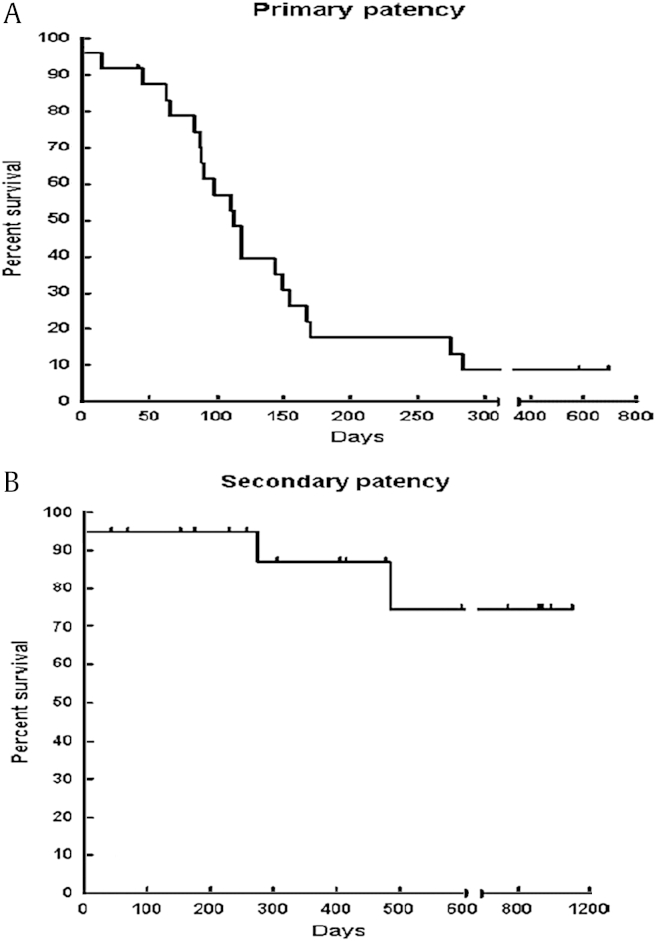
The CVS related to the placement of cardiac rhythm devices can be managed similar to CVS from other causes. Techniques involve angioplasty, stent placement, or as a last resort, ligation of access to reduce symptoms. Angioplasty has been shown to be safe and provides poor primary but acceptable secondary patency rates at 1 year (Figs. 2A and B) [21]. When treating a device-related CVS, placing stent to cover the lead wire is not recommended to avoid trapping the wire. Angioplasty over the wire is considered safe, but if stenting is needed, the device should be removed and replaced after angioplasty and stent placement. Epicardial leads represent an emerging alternative for patients with advanced chronic kidney disease to preserve central veins.
Figure 2.
Primary (A) and secondary (B) patency after angioplasty of central vein stenosis associated with cardiac rhythm devices[21].
Note. From “Patency rates for angioplasty in the treatment of pacemakerinduced central venous stenosis in hemodialysis patients: results of a multi-center study,” by A. Asif, L. Salman, R.G. Carrillo, J.D. Garisto, G. Lopera, U. Barakat, O. Lenz, A. Yevzlin, A. Agarwal, F. Gadalean, B. Sachdeva, T.J. Vachharajani, S. Wu, I.D. Maya, K. Abreo, 2009, Semin Dial, 22, p. 671–676. Copyright 2009. Wiley. Reprinted with permission.
Recanalization for occluded central veins
Central vein occlusion represents a catastrophic event, precluding use of that extremity for any type of access. It is not uncommon to find patients with severe stenosis or occlusion of veins due to repeated and prolonged catheter placement while attempting to create a functioning AV fistula. In young patients with central venous occlusion, it is worthwhile attempting to recanalize the vein if an ipsilateral access is already in development or is being considered for various reasons. A classic hydrophilic wire approach may be successful at times, though sharp recanalization with a needle that can be snared out from the other side of the occlusion is often required. A radiofrequency wire to recanalize occluded veins is another option. As can be imagined, all such approaches of recanalization would require stent placement to maintain the patency. Failure to recanalize and recurrence of the lesion are common. Frequent and multiple interventions to maintain patency are generally required. Because of the complex nature of such occlusions, the procedure can often result in complications and should be performed with great caution.
Hybrid endovascular/surgical approach
In case of a refractory and recurrent stenosis, it is now possible to maintain the patency of the central vein with a hybrid graft–catheter device [22]. The graft portion of the device is anastomosed to the artery in the arm and connected to the outflow provided by the catheter component that crosses the treated stenosed portion of the central vein. This type of access usually performs like an AV graft. The advantage of such an access is primarily due to avoidance of an exteriorized catheter thereby reducing rates of infection.
Endovascular intervention as a palliative approach
A high-flow access can be especially detrimental in the presence of inflow–outflow mismatch because of CVS. Such accesses can often continue to work without having to abandon the access if the flow can be reduced with consequent decrease in intravascular pressure and related symptoms. Balloon-assisted banding with a goal of about 50% reduction of access flow has been used to reduce such symptoms [23].
When CVS remains refractory and symptomatic, sometimes one has to resort to symptomatic and palliative approach to reduce discomfort. For breast edema due to CVS, coil embolization of the long thoracic vein can be useful [24]. When the access is no longer desirable, percutaneous ligation of access can be done. Occlusion of access with a saline-filled balloon can be attempted before resorting to surgical occlusion (Personal communication. Gerald Beathard, MD).
Challenges in endovascular intervention of CVS
It is important to consider limitations of our current knowledge in endovascular intervention for CVS. Better understanding and development of equipment and angioplasty technique to reduce endovascular injury and postoperative methods of modulating endovascular response will transform this area of unmet need. Despite advances, the primary approach to CVS should be prevention of CVS by avoiding endovascular injury.
Conflicts of interest
The author has no conflicts of interest to declare.
References
- 1.Davidson C.J., Newman G.E., Sheikh K.H., Kisslo K., Stack R.S., Schwab S.J. Mechanisms of angioplasty in hemodialysis fistula stenosis evaluated by intravascular ultrasound. Kidney Int. 1991;40:91–95. doi: 10.1038/ki.1991.185. [DOI] [PubMed] [Google Scholar]
- 2.Levit R.D., Cohen R.M., Kwak A., Shlansky-Goldberg R.D., Clark T.W., Patel A.A., Stavropoulos S.W., Mondschein J.I., Solomon J.A., Tuite C.M., Trerotola S.O. Asymptomatic central venous stenosis in hemodialysis patients. Radiology. 2006;238:1051–1056. doi: 10.1148/radiol.2383050119. [DOI] [PubMed] [Google Scholar]
- 3.Chang C.J., Ko P.J., Hsu L.A., Ko Y.S., Ko Y.L., Chen C.F., Huang C.C., Hsu T.S., Lee Y.S., Pang J.H. Highly increased cell proliferation activity in the restenotic hemodialysis vascular access after percutaneous transluminal angioplasty: implication in prevention of restenosis. Am J Kidney Dis. 2004;43:74–84. doi: 10.1053/j.ajkd.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 4.National Kidney Foundation Guideline 20. K/DOQI Clinical Practice Guidelines for Vascular Access, 2000. Am J Kidney Dis. 2001;37(Suppl 1):S137–S181. doi: 10.1016/s0272-6386(01)70007-8. [DOI] [PubMed] [Google Scholar]
- 5.Glanz S., Gordon D.H., Lipkowitz G.S., Butt K.M., Hong J., Sclafani S.J. Axillary and subclavian vein stenosis: percutaneous angioplasty. Radiology. 1988;168:371–373. doi: 10.1148/radiology.168.2.2969117. [DOI] [PubMed] [Google Scholar]
- 6.Beathard G.A. Percutaneous transvenous angioplasty in the treatment of vascular access stenosis. Kidney Int. 1992;42:1390–1397. doi: 10.1038/ki.1992.431. [DOI] [PubMed] [Google Scholar]
- 7.Kovalik E.C., Newman G.E., Suhocki P., Knelson M., Schwab S.J. Correction of central venous stenoses: use of angioplasty and vascular Wallstents. Kidney Int. 1994;45:1177–1181. doi: 10.1038/ki.1994.156. [DOI] [PubMed] [Google Scholar]
- 8.Quinn S.F., Schuman E.S., Demlow T.A., Standage B.A., Ragsdale J.W., Green G.S., Sheley R.C. Percutaneous transluminal angioplasty versus endovascular stent placement in the treatment of venous stenosis in patients undergoing hemodialysis: intermediate results. J Vasc Interv Radiol. 1995;6:851–855. doi: 10.1016/s1051-0443(95)71200-3. [DOI] [PubMed] [Google Scholar]
- 9.Dammers R., de Haan M.W., Planken N.R., van der Sande F.M., Tordoir J.H. Central vein obstruction in hemodialysis patients: results of radiological and surgical intervention. Eur J Vasc Endovasc Surg. 2003;26:317–321. doi: 10.1053/ejvs.2002.1943. [DOI] [PubMed] [Google Scholar]
- 10.Surowiec S.M., Fegley A.J., Tanski W.J., Sivamurthy N., Illig K.A., Lee D.E., Waldman D.L., Green R.M., Davies M.G. Endovascular management of central venous stenoses in the hemodialysis patient: results of percutaneous therapy. Vasc Endovasc Surg. 2004;38:349–354. doi: 10.1177/153857440403800407. [DOI] [PubMed] [Google Scholar]
- 11.Bakken A.M., Protack C.D., Saad W.E., Lee D.E., Waldman D.L., Davies M.G. Long-term outcomes of primary angioplasty and primary stenting of central venous stenosis in hemodialysis patients. J Vasc Surg. 2007;45:776–783. doi: 10.1016/j.jvs.2006.12.046. [DOI] [PubMed] [Google Scholar]
- 12.Buriankova E., Kocher M., Bachleda P., Utíkal P., Kojecký Z., Cerná M., Herman M. Endovascular treatment of central venous stenoses in patients with dialysis shunts. Biomed Papers. 2003;147:203–206. doi: 10.5507/bp.2003.030. [DOI] [PubMed] [Google Scholar]
- 13.Gunther R.W., Vorwerk D., Bohndorf K., Klose K.C., Kistler D., Mann H., Sieberth H.G., el-Din A. Venous stenoses in dialysis shunts: treatment with self-expanding metallic stents. Radiology. 1989;170:401–405. doi: 10.1148/radiology.170.2.2521397. [DOI] [PubMed] [Google Scholar]
- 14.Aruny J.E., Lewis C.A., Cardella J.F., Cole P.E., Davis A., Drooz A.T., Grassi C.J., Gray R.J., Husted J.W., Jones M.T., McCowan T.C., Meranze S.G., Van Moore A., Neithamer C.D., Oglevie S.B., Omary R.A., Patel N.H., Rholl K.S., Roberts A.C., Sacks D., Sanchez O., Silverstein M.I., Singh H., Swan T.L., Towbin R.B., Trerotola S.O., Bakal C.W. Society of Interventional Radiology Standards of Practice Committee: quality improvement guidelines for percutaneous management of the thrombosed or dysfunctional dialysis access. Standards of Practice Committee of the Society of Cardiovascular & Interventional Radiology. J Vasc Interv Radiol. 2003;14:S247–S253. [PubMed] [Google Scholar]
- 15.Haage P., Vorwerk D., Piroth W., Schuermann K., Guenther R.W. Treatment of hemodialysis-related central venous stenosis or occlusion: results of primary Wallstent placement and follow-up in 50 patients. Radiology. 1999;212:175–180. doi: 10.1148/radiology.212.1.r99jl21175. [DOI] [PubMed] [Google Scholar]
- 16.Gray R.J., Horton K.M., Dolmatch B.L., Rundback J.H., Anaise D., Aquino A.O., Currier C.B., Light J.A., Sasaki T.M. Use of Wallstents for hemodialysis access-related venous stenoses and occlusions untreatable with balloon angioplasty. Radiology. 1995;195:479–484. doi: 10.1148/radiology.195.2.7724770. [DOI] [PubMed] [Google Scholar]
- 17.Maya I.D., Saddekhi S., Allon M. Treatment of refractory central vein stenosis in hemodialysis patients with stents. Semin Dial. 2007;20:78–82. doi: 10.1111/j.1525-139X.2007.00246.x. [DOI] [PubMed] [Google Scholar]
- 18.Vogel P.M., Parise C. SMART stent for salvage of hemodialysis access grafts. J Vasc Interv Radiol. 2004;15:1051–1060. doi: 10.1097/01.RVI.0000129915.48500.DC. [DOI] [PubMed] [Google Scholar]
- 19.Jones R.G., Willis A.P., Jones C., McCafferty I.J., Riley P.L. Long-term results of stent-graft placement to treat central venous stenosis and occlusion in hemodialysis patients with arteriovenous fistulas. J Vasc Interv Radiol. 2011;22:1240–1245. doi: 10.1016/j.jvir.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Sapoval M.R., Turmel-Rodrigues L.A., Raynaud A.C., Bourquelot P., Rodrigue H., Gaux J.C. Cragg covered stents in hemodialysis access: initial and midterm results. J Vasc Interv Radiol. 1996;7:335–342. doi: 10.1016/s1051-0443(96)72863-4. [DOI] [PubMed] [Google Scholar]
- 21.Asif A., Salman L., Carrillo R.G., Garisto J.D., Lopera G., Barakat U., Lenz O., Yevzlin A., Agarwal A., Gadalean F., Sachdeva B., Vachharajani T.J., Wu S., Maya I.D., Abreo K. Patency rates for angioplasty in the treatment of pacemaker-induced central venous stenosis in hemodialysis patients: results of a multicenter study. Semin Dial. 2009;22:671–676. doi: 10.1111/j.1525-139X.2009.00636.x. [DOI] [PubMed] [Google Scholar]
- 22.Katzman H.E., McLafferty R.B., Ross J.R., Glickman M.H., Peden E.K., Lawson J.H. Initial experience and outcome of a new hemodialysis access device for catheter-dependent patients. J Vasc Surg. 2009;50:600–607. doi: 10.1016/j.jvs.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 23.Jennings W.C., Miller G.A., Coburn M.Z., Howard C.A., Lawless M.A. Vascular access flow reduction for arteriovenous fistula salvage in symptomatic patients with central venous occlusion. J Vasc Access. 2012;13:157–162. doi: 10.5301/jva.5000020. [DOI] [PubMed] [Google Scholar]
- 24.Miller G.A., Friedman A., Khariton A., Jotwani M.C., Savransky Y. Long thoracic vein embolization for the treatment of breast edema associated with central venous occlusion and venous hypertension. J Vasc Access. 2010;11:115–121. doi: 10.1177/112972981001100206. [DOI] [PubMed] [Google Scholar]