Abstract
AIM: To compare the features of gastroesophageal reflux disease between elderly and younger patients.
METHODS: Twenty-four hour pH-monitoring and endoscopy were per formed for the 66 elderly patients with typical gastroesophageal reflux symptoms, and the results were compared with 112 symptomatic younger patients.
RESULTS: The results of 24-h pH-monitoring and endoscopy showe d that the elderly patients had pathological reflux and reflux esophagitis more frequently than the younger patients. Percentage time with pH < 4 in elderly patients with reflux esophagitis was 32.5% in 24 h, as compared with 12.9% in the younger patients with reflux esophagitis (P < 0.05). The elderly patients with reflux esophagitis have longer periods of acid reflux in both upright and supine positions than the younger patients. Endoscopy showed that 20.8% of elderly patients had grade III/IV esophagitis, whereas only 3.4% of younger patients had grade III/IV esophagitis (P < 0.002). Percentages of grades I/II esophagitis in the two groups were 12.5% and 26.5%, respectively (P < 0.002).
CONCLUSION: Elderly patients, as compared with younger patients, have more severe gastroesophageal reflux and esophageal lesions. The incompetence of lower esophageal sphincter and the presence of hiatal hernia may be important factors leading to the difference in incidence and severity of reflux esophagitis between elderly and younger patients.
Keywords: gastroesophageal reflux, esophagitis, hiatal hernia
INTRODUCTION
With the introduction of intraesophageal 24-h pH-monitoring in clinical practice, it is now possible to identify patterns of gastroesophageal reflux (GER) in the healthy people and patients and to assess the effect of H2 blockers and H+/K+ adenosine triphosphatase (ATPase) inhibitors on GER diseases[1-7]. It is increasingly recognized that symptomatic GER may occur in the patients of all ages. However, little information is available on symptomatic GER patterns in the elderly. Recently, Mold et al[8], investigated GER disease (GERD) in patients aged over 62 years in a primary care setting. However, the focus of this study was not on patterns of GER, but on prevalence of GER in the elderly. Therefore, the aim of the present study was to identify patterns and features of symptomatic GER in the elderly patients.
PATIENTS AND METHODS
Patients
One hundred and seventy-eight consecutive patients who had experienced heartburn, regurgitation and chest pain for at least 6 months were studied. These includ ed 66 elderly patients (36 men, 30 women) ranging in age from 65 to 76 years (mean age 67 years), and 112 younger patients (64 men, 48 women) aged from 21 to 64 years (mean age 41 years). None had undergone upper gastrointestinal surgery such as gastric resection and selective proximal vagotomy. None had taken H2-blockers or H+/K+-ATPase inhibitors in the 2-week period before 24-h pH-monitoring.
Endoscopy
All patients underwent upper gastrointestinal endoscopy. Esophagitis grade was assessed endoscopically by using the Savary & Miller Criteria[9], that is, from grade I to IV. Of these patients, very few presented with grades II and III esophagitis, and therefore grade I and II, and III and IV were grouped together.
Twenty-four hour intraesophageal pH-monitoring
Twenty-four hour intraesophageal pH-monitoring was carried out by a routine method used in our laboratory[10]. Patients were advised to take a standard 2200 kilocalories meal during 24-h intraesophageal pH-monitoring. A glass pH-electrode with an incorporated potassium chloride reference electrode (Ingol delectrode, No 440) was introduced via the naso-esophageal route and positioned with the tip 5 cm above the gastroesophageal junction identified by the pH-metry[11,12]. The output from the pH probe was recorded on a solid-state recorder (Autronicord CM 18), which could be carried on a belt by the patients. Data were analyzed on a computer by means of a dedicated computer program. The parameters recorded included the frequency and duration of GER in 24 h, upright and supine positions, and frequency of GER longer than 5 min. Pathological reflux was diagnosed if 1) the pH value in the regurgitated contents was < 4.0, and 2) the complete reflux duration was more than 7% in 24 h[10-12]. Reflux esophagitis was diagnosed if the patient with pathological GER had inflammatory esophageal lesions.
Statistical methods
Anamnestic data and endoscopic findings were analysed by means of the Chi-square test. The Mann-Whitney test and Fisher exact test were used to evaluate GER parameters.
RESULTS
Endoscopic findings showed that elderly patients had more severe esophageal lesions and a higher incidence of hiatal hernia than younger patients (Table 1) (P < 0.002).
Table 1.
Endoscopic findings in elderly and younger patients
| Non-esophagitis (%) |
Esophagitis |
Hiatal hernia (%) | ||
| I/II (%) | III/IV (%) | |||
| Elderly patients | 44 (66.7) | 8 (12.1)b | 14 (21.2)b | 16 (24.2)b |
| Younger patients | 78 (69.6) | 29 (25.8) | 4 (3.6) | 17 (15.1) |
P < 0.001, elderly patients vs younger patients.
On the basis of the results of the endoscopy and intraesophageal 24-h pH-monitoring, patients can be divided into three subgroups: physiologic reflux, pathologic reflux and reflux esophagitis. Table 2 lists the percentages of the three groups in elderly and younger patients. The incidence of pathologic reflux and reflux esophagitis in elderly patients was higher than that in younger patients (P < 0.05).
Table 2.
Percentages of physiological reflux (PhR), pathological reflux and reflux esophagitis (RE) in elderly and younger patients
| PhR (%) | PR (%) | RE (%) | |
| Elderly patients | 24 (36.4)a | 20 (30.3)a | 22 (33.3)a |
| Younger patients | 59 (52.7) | 19 (17.0) | 34 (30.3) |
P < 0.05, elderly patients vs younger patients; PhR = physiological reflux; PR = pathological reflux; RE = reflux esophagitis.
Figure 1 shows the percentage time of GER episodes in 24 h. In the reflux esophagitis group, percentage time of GER episodes in the elderly and younger patients during the entire 24-h period was 36.2% and 17.8%, respectively (P < 0.05). No statistically significant differences in the percentage time with GER episodes were found between the elderly and younger patients in either the physiologic or pathologic reflux subgroups.
Figure 1.
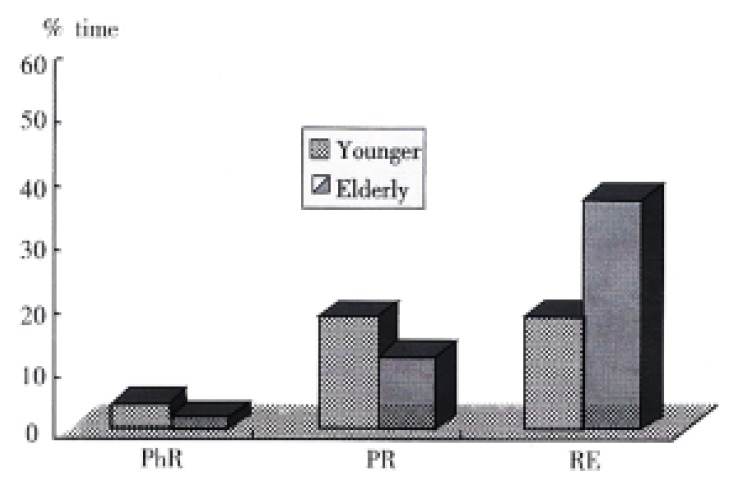
Percentige time of GER episodes in 24 h. PhR: physiological reflux; PR: pathological reflux; RE: reflux esophagitis.
Figure 2 and Figure 3 show the percentage time of GER episodes in upright and supine positions. Elderly patients with reflux esophagitis had significantly greater percentage time of GER episodes than younger patients with reflux esophagitis (upright position, 32.4% versus 13.6% supine position, 30.7% versus 11.7%; P < 0.05).
Figure 2.
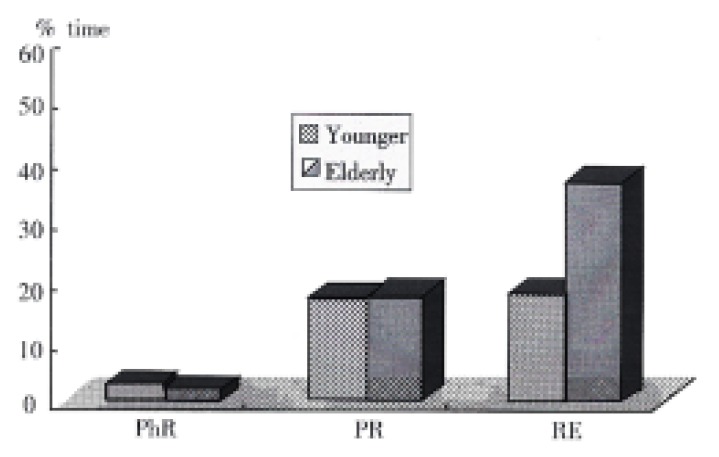
Percentage time of GER episodes in upright position.
Figure 3.
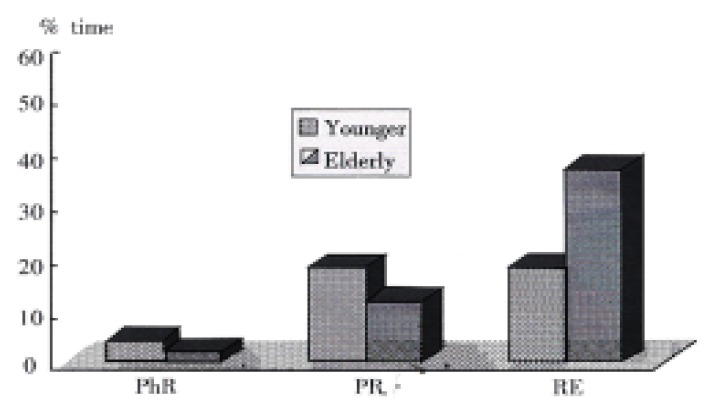
Percentage time of GER episodes in supine positions.
Elderly patients with reflux esophagitis had a higher frequency of GER episodes than younger patients with reflux esophagitis, the difference being statistically significant (Table 3). There was no significant difference between elderly and younger patients in frequency of GER episodes lasting more than 5 min (Table 4).
Table 3.
Frequency of GER episodes in elderly and younger patients (x- ± s)
| Elderly | Younger | patients | patients | |
| Upright position | ||||
| PhR | 1 0 | 10a | 24 | 20a |
| P R | 4 5 | 21b | 5 5 | 21b |
| RE | 8 5 | 64c | 5 3 | 32c |
| Supine position | ||||
| PhR | 3 | 4 | 3 | 9 |
| P R | 1 7 | 9d | 8 | 7d |
| RE | 1 8 | 3e | 7 | 7e |
P < 0.01, elderly vs younger;
P < 0.05, elderly vs younger;
P < 0.01, elderly vs younger;
P < 0.05, elderly vs younger.
Table 4.
Frequency of GER episodes lasting more than 5 min in eld erly and younger patients (x- ± s)
| Elderly | patients | Younger | patients | |
| Upright position | ||||
| P R | 3 | 2 | 5 | 3 |
| RE | 9 | 6 | 5 | 6 |
| Supine position | ||||
| P R | 3 | 2 | 5 | 3 |
| RE | 3 | 2 | 2 | 2 |
P > 0.05, elderly patients vs younger patients; PR = pathological reflux; RE = reflux esophagitis.
DISCUSSION
Although several studies of GER patterns have been carried out in healthy subjects and patients, the GER profile in the elderly has not been investigated. Many older people, as a result of physiological change or disease, have decreased salivary flow, gastric acid production, esophageal motility, gastric emptying, and/or lower esophageal sphincter tone. These changes may affect the features of symptomatic GER in the elderly patients.
The present study demonstrated that patterns of GER and esophageal lesions in elderly patients with GER symptoms showed different features from those presented by the younger patients. Firstly, the incidence of pathological reflux and reflux esophagitis in the elderly patients with GER symptoms was significantly higher than in the younger patients (66.7% vs 46.9%). Secondly, the elderly patients with GER symptoms have more severe esophageal lesions than younger patients. In the elderly patients, 20.8% of patients had grades III/IV esophagitis, as against only 3.4% of patients in the younger group. In addition, elderly patients had a higher incidence of hiatal hernia than their younger counterparts. Thirdly, 24-h intraesophageal pH-monitoring showed that elderly patients with reflux esophagitis had a more severe acid reflux than younger patients with reflux esophagitis. This is due to prolonged periods of acid reflux in both upright and supine positions. Similarly, in elderly patients with reflux esophagitis, the frequency of GER episodes in both upright and supine positions is higher than that in younger patients with reflux esophagitis. It is generally agreed that esophagitis may be the result of abnormal acid GER in most patients. Our results suggest that more severe patterns of GER in elderly patients leads to more severe esophageal lesions.
The present results showed that there was no statistically significant difference between the elderly and younger patients regarding frequency of GER episodes lasting more than 5 min (Table 4). This suggests that an impaired esophageal clearing function is not responsible for the difference in incidence and severity of reflux esophagitis observed between elderly and younger patients. Therefore, different pathogenetic mechanism such as the incompetence of lower esophageal sphincter and the presence of hiatal hernia may be important factors leading to the difference in incidence and severity of reflux esophagitis between elderly and younger patients.
Footnotes
Edited by Ma JY
References
- 1.Smout AJ, Breedijk M, van der Zouw C, Akkermans LM. Physiological gastroesophageal reflux and esophageal motor activity studied with a new system for 24-hour recording and automated analysis. Dig Dis Sci. 1989;34:372–378. doi: 10.1007/BF01536258. [DOI] [PubMed] [Google Scholar]
- 2.Duroux P, Emde C, Bauerfeind P, Francis C, Grisel A, Thybaud L, Arstrong D, Depeursinge C, Blum AL. The ion sensitive field effect transistor (ISFET) pH electrode: a new sensor for long term ambulatory pH monitoring. Gut. 1991;32:240–245. doi: 10.1136/gut.32.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Champion G, Richter JE, Vaezi MF, Singh S, Alexander R. Duodenogastroesophageal reflux: relationship to pH and importance in Barrett's esophagus. Gastroenterology. 1994;107:747–754. doi: 10.1016/0016-5085(94)90123-6. [DOI] [PubMed] [Google Scholar]
- 4.Breumelhof R, Smout AJ. The symptom sensitivity index: a valuable additional parameter in 24-hour esophageal pH recording. Am J Gastroenterol. 1991;86:160–164. [PubMed] [Google Scholar]
- 5.Hewson EG, Sinclair JW, Dalton CB, Richter JE. Twenty-four-hour esophageal pH monitoring: the most useful test for evaluating noncardiac chest pain. Am J Med. 1991;90:576–583. [PubMed] [Google Scholar]
- 6.Richter JE, Bradley LA, DeMeester TR, Wu WC. Normal 24-hr ambulatory esophageal pH values. Influence of study center, pH electrode, age, and gender. Dig Dis Sci. 1992;37:849–856. doi: 10.1007/BF01300382. [DOI] [PubMed] [Google Scholar]
- 7.Kahrilas PJ, Quigley EM. Clinical esophageal pH recording: a technical review for practice guideline development. Gastroenterology. 1996;110:1982–1996. doi: 10.1053/gast.1996.1101982. [DOI] [PubMed] [Google Scholar]
- 8.Mold JW, Reed LE, Davis AB, Allen ML, Decktor DL, Robinson M. Prevalence of gastroesophageal reflux in elderly patients in a primary care setting. Am J Gastroenterol. 1991;86:965–970. [PubMed] [Google Scholar]
- 9.Savary M, Miller G. The esophagus. Handbook and atlas of endoscopy. Switzerland: Gassmann. 1987:1–250. [Google Scholar]
- 10.Zhu HM, Bianchi Porro G, Sangaletti O, Pace F. Thresholds of gastroesophageal reflux in the diagnosis of esophageal reflux diseases. China Natl J New Gastroenterol. 1996;2:9–12. [Google Scholar]
- 11.Zhu HM. Study of influence of hiatus hernia on gastroesophageal reflux. China Natl J New Gastroenterol. 1997;3:27–30. doi: 10.3748/wjg.v3.i1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhu HM, Huang X, Deng CZ, Porro GP, Pace F, Sangaletti O. Pathogenetic factors affecting gastroesophageal reflux in patients with esophagitis and concomitant duodenal ulcer: a multivariate analysis. World J Gastroenterol. 1998;4:153–157. doi: 10.3748/wjg.v4.i2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]


