INTRODUCTION
The increased expression of ICAM-1 on a wide range of cells and in the sera of patients with malignancies, chronic liver diseases and inflammation diseases has been described since the late 1980s[1-22]. Recently rapid progress in studies on expression of ICAM-1 in patients with hepatocellular carcinoma (HCC) have been achieved, including clinical and experimental researches[23-31]. It is well known now that ICAM-1 expressed in two ways in HCC: ① membrane-bounded ICAM-1 on the surface of HCC cells (mbICAM-1), which did not express in normal liver cells, and ② soluble ICAM-1 (sICAM-1) in sera of the patients, the concentration of which is well correlated with the progress and prognosis of the disease[32]. However, little is known about whether sICAM-1 is a diagnostic marker for early detecting HCC and monitoring its postoperative recurrence. It has been demonstrated that measurement of sICAM-1 might be of clinical values for early diagnosis and monitoring recurrence of HCC, particularly in patients with normal or low serum level of α-fetoprotein (AFP)[33-37]. Another controversy in this field is what is the main source of high levels of circulating sICAM-1 in HCC patients. It was reported that there were two forms of sICAM-1: HCC-specific circulating form of ICAM-1 shedding from HCC cells, and inflammation-associated ICAM-1 upregulated by several cytokines, of which interferon-gamma (INF-gamma) was the main cytokine trigger for ICAM-1 expression[38]. To solve the two problems mentioned above has become the key to the study. For this purpose, we have further confirmed the clinical values of sICAM-1 detection in HCC compared with benign liver diseases and normal control, analyzed the serum levels of AFP and sICAM-1 in HCC; observed mbICAM-1 expression in different regions of HCC tissues with the immunohistochemistry, and measured the expression of ICAM-1 mRNA in tissue samples by reverse transcriptase polymerase chain reaction (RT-PCR).
MATERIALS AND METHODS
Patients
Between January 1997 and July 2000, 151 patients with pathologically proven HCC either by surgical resection of liver tumors or by liver biopsies (131 men and 20 women; aged from 14 to 80 years, median 49) were treated in our department. Tumor was less than 5 cm in diameter in 21 patients,less than 10 cm in 43 and more than 10 cm or with extrahepatic metastasis in 87 cases. Liver cirrhosis was found in 137 patients. Hepatitis B surface antigen (HBsAg) was positive in 129 patients. Hepatitis C antibody was positive in 14 patients. The serum concentration of AFP was measured in all cases by radioimmunoassay (RIA) and its reference ranges were classified as follows: > 200 µg/L as positive in 93; 20 µg/L-200 µg/L as questionable positive in 33 and < 20 µg/L as negative in 25[35]. Treatment included surgical procedures (in 90 cases), interventioanl radiology (IR in 46) and percuteneous ethanol injection (PEI in 15). Among the surgically-treated patients, tumor resection was performed in 75, including radical resection in 42, nonradical in 33 due to intrahepatic vascular invasion on the resected margin pathologically or intrahepatic metastasis of tumor found intraoperatively. Laparotomy cathterization of the hepatic artery was undertaken in 15. The 46 patients underwent IR therapies including transcatheter arterial embolization (TAE) in 30 and transcatheter arterial infusion (TAI) in 16.
Follow-up of the patients undergoing hepatectomies
The patients undergoing hepatectomies were followed up monthly in the first year and once every two months in the second year postoperatively. During the follow-up, serum concentration of AFP and sICAM-1, liver function and image examinations including BUS, CT or selective hepatic angiography were undertaken. Tumor recurrence was confirmed when intrahepatic lesion or portal vein tumor thrombi were found by liver image, and pathological diagnosis was established by reoperation or biopsy of the tumor.
ELISA for sICAM-1
Concentrations of sICAM-1 were measured with an enzyme-linked immunosorbent assay kit (Biosource Europe, Fleurus, Belgium) as described previously[31-37]. In all HCC patients, sICAM-1 levels were compared with their levels of serum AFP. As controls, serum levels of sICAM-1 were measured in 62 patients with chronic hepatitis B (CH), 60 with liver cirrhosis (LC) and 50 healthy blood donors. Immunohistochemistry of liver tissues -Tissues from tumor and adjacent region were obtained from 52 patients with surgical resection. Histologically normal liver tissues were obtained from 3 patients with liver hemangioma. To demonstrate the presence of ICAM-1 in the resected liver tissues, each fresh specimen was cut at -20 °C with the cryostat (4 μm-thick), mounted on sialinized adhesion microscope slides, dried overnight at room temperature, fixed with cold acetone (-20 °C) for 10 min and chloroform for 20 min. Anti-human ICAM-1 mouse monoclonal antibody (Clone HA58, Pharmigen) was used. The slides were washed twice in TRIS/0.2% BSA and then incubated with sheep-anti-mouse-Ig (DAKO, Copenhagen, Denmark). And then the staining reaction was developed with a streptavidin-biotinylated-alkaline-phosphatase-complex (DAKO), slides were counterstained with hematoxylin, and nonreacting monoclonal antibody of IgG-1-isotype (DAKO) was used as negative control.
RNA extraction and DNA amplification
The total RNA was isolated from the fresh resected liver tissues by the acid guanidium thiocynate-phennol-chloroform method[39] (Gstract, Maxim Biotech, Inc., San Francisco, USA). The concentration of RNA was determined from absorption at 260 nm, and A 260: -80 ratios were > 1.7. RNA (10 μg)was subjected to electrophoresis in 1.5% agarose gels. The PCR primer for ICAM-1 and GAPDH were designed according to Vigano et al[40]. The following four primers presented by Dr. Shraven were used: ① (105)5’-TGATGACATCAAGAAGGTGGTGAAG-3’; ② (1047) 5’-TCCTTGAGGCCATGTGGGC-CAT-3’; ③ (825) 5’-GTCCCCTCAAAAGTCATCC-3’; ④ (1064) 5’-AACCCCATTCAGCGTCACCT-3’. The primer set was used to amplify an intron-spanning region of the human glyceraldeyde-3-phosphate dehydrogenase (GAPDH) gene. The latter gene provided a constitutively expressed internal control for complementary DNA contamination. The presence of ICAM-1 and GAPDH mRNAs was demonstrated by amplifying respective target sequences using PCR according to the instruction provided with the Technical Bulletin Kit (Promega). In brief, 3 μL (2.5 mM) RNA, and 50 pmol/L primers for ICAM-1 or GAPDH were added to each reaction mixture respectively, which included 0.4 mM dNTPs 2 μL, 3 μL (1.5 mM) MgSO4, AM V reverse transcriptase 1 μL (5 U), TfI DNA polymerase 1 μL (5 U), and AMV/TfI 5 × buffer 10 μL. The final reaction volume was 50 μL and was covered with 20 μL mineral oil. Then with PCR thermal cycle(Hema 480, China), RT-PCR reaction was run in the following procedures: ① 48 °C for 45 min, 1 circle; ② 94 °C for 2 min, 1 circle; ③ 94 °C for 30 s, 60 °C for 1 min, 38 °C for 2 min, 30 circles; and ④ 68 °C for 7 min, 1 circle. Five μL PCR product was placed on 1.5% agarose gel and observed by EB staining under UV light, the electrophoresis photo was transformed into computer, and ICAM-1 intensity was analyzed with MPIAS500 image system, while the GAPDH band intensity was subtracted as an internal standard.
Statistical analysis
Groups were compared by the Kruskal-Wallsi test and the t test.
RESULTS
sICAM-1 measurement
The concentrations of sICAM-1 measured in different groups are illustrated in Figure 1. The levels of sICAM-1 in the patients with CH (median -462 μg/L), LC (median -587 μg/L) and HCC (median -1120 μg/L) were significantly higher than that in the normal control (median -285 μg/L) (P < 0.01). The levels of sICAM-1 in HCC group was also significantly higher than those in CH and LC groups (P < 0.01).
Figure 1.

Serum concentration of sICAM-1 in normal controls (n = 50), in patients with chronic hepatitis (CH, n = 62), cirrhosis (LC, n = 60), and hepatocellular carcinoma (HCC, n = 151). aP < 0.05, bP < 0.01.
Comparative analysis of the serum values of sICAM-1 and AFP in HCC patients is listed in Table 1. There were 93 (62%) patients with positive serum AFP, and 58 (38%) with questionable and negative (33 and 25). However, the median values of sICAM-1 in these patients were 1597, 1456 and 1271 μg/L respectively. Statistical analysis showed no significant differences. In addition, analysis of ranges of sICAM-1 of HCC patients showed that 129 (85.4%) patients had a serum concentration exceeding 1000 μg/L, which was higher than the positive rate of serum AFP in the group of same patients.
Table 1.
Comparative analysis of serum levels of sICAM-1 and AFP in HCC patients
| Group | Number of patients | sICAM-1 (μg/L) | AFP (μg/L) |
| AFP < 20 μg/L | 25 | 1271 | 18 |
| AFP 20-200 μg/L | 33 | 1456 | 121 |
| AFP > 200 μg/L | 93 | 1597 | 26280 |
During the postoperative follow-up period of 6-61 months, tumor recurrence was confirmed in 41 patients. The median level of sICAM-1 of the patients was 1051 μg/L and 30 (73.2%) cases had a value higher than 1000 μg/L. On the other hand, there were 25 (60%) patients with serum AFP positive (> 200 μg/L). In 6 patients with negative AFP, tumor recurrence was not detected by liver image until their serum levels of sICAM-1 had exceeded 2-4 times higher than before for 1-4 months.
Immunohistochemical staining
In all HCC samples, cancerous regions showed positive membrane staining for ICAM-1 with a honeycomb pattern (Figure 2). Parts of plasma of HCC cells showed strong positive reactions. In contrast to the cancerous areas, in noncancerous adjacent areas (Figure 3), the expression of ICAM-1 was negative, except those hepatocytes in severe cirrhotic areas. Normal liver tissue showed negative or very weak staining of the vascular endothelial cells and hepatocyts for ICAM-1 (Figure 4).
Figure 2.

Immunohistochemical staining of ICAM-1 in hepatocellular carcinoma tissue is positive on the surface of tumor cells and in a honeycomb pattern.
Figure 3.
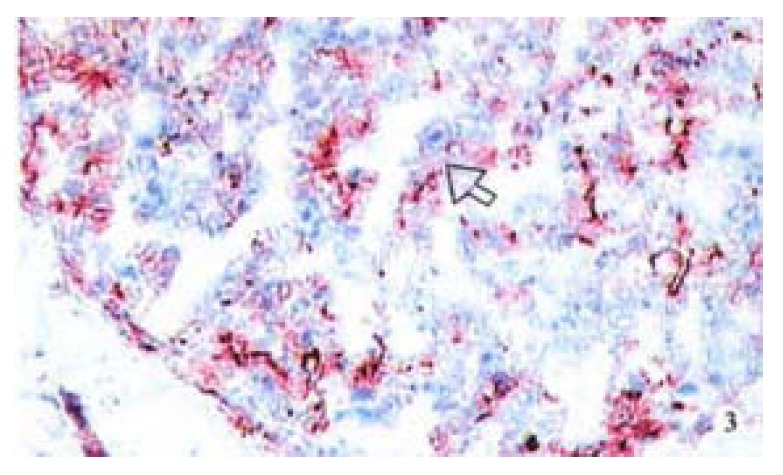
Increased expression of ICAM-1 in paracancerous tissue was shown with severe cirrhosis by immunohistochemical staining.
Figure 4.

ICAM-1 expression was negative in normal liver tissue by immunohistochemical staining (AEC method).
RT-PCR detection of ICAM-1
ICAM-1 mRNA in HCC tissues was detected by RT-PCR analysis (Figure 5). The result showed that freshly aspirated liver tissues expressed the gene coding for ICAM-1 because RT-PCR generated a DNA fragment corresponding to the predicted length, 943 bp, of the ICAM-1 amplification product. In each tissue sample, all GAPDH amplification products were of 240 bp length. The results revealed that the expression of ICAM-1 was stronger in the carcinomatous tissues of 28/43 cases (65.1%) than that in the paracacinomatous tissues of 13/43 (30.2%) cases. Thirty-two of 43 cases had the levels of sICAM-1 > 1000 μg/L.
Figure 5.

RT-PCR product gel electrophoresis. Three ìL RT-PCR products of ICAM-1 and GAPDH run on 1.5% agarose gel stained with EB. Lane 1 and Lane 4: the control for ICAM-1 and GAPDH. Lane 2 and 5: paracarcinomatous tissue for ICAM-1 and GAPDH. Lane and 6: HCC tissues for ICAM-1 and GAPDH.
The clinicopathological analysis of ICAM-1 mRNA and HCC is shown in Table 2. In the patients with serum levels of sICAM-1 above 1000 μg/L, the expression rates of ICAM-1 mRNA in HCC and adjacent tissues were 75.0% and 34.4%, respectively (P < 0.01), however, in group with sICAM-1 lower than 1000 μg/L, the expression rate in those tissues were 36.4% and 18.2%, respectively (P > 0.05). It is noticed that the expression rate of ICAM-1 mRNA was related to the severity of liver cirrhosis and intrahepatic metastasis of tumor. However, the expression rates of ICAM-1 mRNA were not correlated with the serum levels of AFP, differentiation of tumor and tumor sizes.
Table 2.
Clinicopathological analysis of ICAM-1 mRNA and HCC % (n)
| Clinical data | Cases | Positive tumor | Positive paratumor |
| ICAM-1 mRNA | ICAM-1 mRNA | ||
| Serum AFP > 400 μg/L | 25 | 68.0 (17/25) | 32.0 (8/25) |
| Serum AFP < 400 μg/L | 18 | 61.1 (11/18) | 27.8 (5/18) |
| sICAM-1 > 1000 μg/La | 32 | 75.0 (25/32) | 34.4 (11/32) |
| < 1000 μg/L | 11 | 36.4 (3/11) | 18.2 (2/11) |
| Severe cirrhosisa Yes | 30 | 80.0 (24/30) | 36.7 (11/30) |
| No | 13 | 30.8 (4/13) | 15.4 (2/13) |
| Differentiation High | 15 | 66.7 (10/15) | 33.3 (4/15) |
| Low | 28 | 64.3 (18/28) | 32.1 (9/28) |
| Tumor size > 5 cm | 31 | 66.7 (8/12) | 25.0 (3/12) |
| < 5 cm | 12 | 64.5 (20/31) | 32.3 (10/31) |
| Intrahepatic metastasisb Yes | 15 | 86.7 (13/15) | 40.0 (6/15) |
| No | 28 | 46.4 (13/28) | 25.0 (7/28) |
P < 0.01;
P < 0.05
DISCUSSION
HCC is one of the malignancies, which inflicts Chinese population severely. The prognosis of the disease is still dismal due to a delayed diagnosis, low resected rate and high recurrence rate of the tumor. Thus early diagnosis and effective postoperative monitoring are important to improve the surgical effectiveness for HCC[41]. The present study further confirmed our previous observations and other reports, in which elevated serum sICAM-1 was found in HCC, which was significantly higher than in benign liver diseases and the normal controls (Figure 1). As described by Shimizu et al[42], a sICAM-1 level above 1000 μg/L is a determinant for prognosis and progression of HCC. In our 151 patients with HCC, 129 (85.4%) cases had a high serum concentration of ICAM-1 above 1000 μg/L, which suggested that the positivity of sICAM-1 was higher than that of serum AFP. Although the serum levels of AFP in the HCC patients were different (Table 1), the sICAM-1 levels in the same group of patients showed no significant differences, particularly in cases with low levels of or negative AFP, indicating that measurement of sICAM-1 might be of diagnostic value for HCC.
Another interesting finding from our study is that in patients with AFP negative or questionable positive, sICAM-1 is a more sensitive serum diagnostic marker than AFP and other procedures, including BUS, CT, etc. In 41 patients with tumor recurrence detected during the postoperative follow-up, 73.2% patients had a high level of sICAM-1 above 1000 μg/L, however, the proportion of positive serum AFP in the same cases was only 60%. Moreover, in 6 of the 41 patients with negative AFP, tumor recurrence was diagnosed 1-4 months earlier by sICAM-1 than by liver image examination. We believe that sICAM-1 is not only a useful marker for predicting the progression and prognosis of the disease, but also a sensitive marker for diagnosing and monitoring HCC and its recurrence, especially for patients with low serum concentrations of AFP when the serum level of sICAM-1 was above 1000 μg/L[32-36].
As mentioned above, our clinical observations strongly supported that sICAM-1 might be of diagnostic value for HCC. However, it is unknown what is the main source of high level of sICAM-1 in HCC: HCC- specific ICAM-1 shedding from mbICAM-1 or inflammation-associated ICAM-1[38]. To distinguish the two forms of ICAM-1 is the ultimate goal of the study in this field[38]. Clinically, we have got the evidence that sICAM-1 is derived from HCC tumor cells, because we found in non-radical resected patients, the sICAM-1 concentrations maintained at a high level after the operation compared with those who underwent a radical resection of tumors, whose sICAM-1 levels would be decreased to the normal within 1-2 months postoperatively. This suggested that circulating sICAM-1 in HCC may originate mainly from tumor cell itself[36,37].
To verify our clinical findings that sICAM-1 is mainly derived from the HCC cells, we investigated the expression of ICAM-1 in HCC and its adjacent tissues with immunohistochemistry. The results showed that ICAM-1 expressed strongly in all specimens of HCC, but did not express in noncancerous regions, which reflected such a fact that high serum sICAM-1 levels of HCC patients might be attributable to tumor cells and a malignant transformation of hepatocytes. Our inference was supported by other authors[24,30,43,44]. Torri and Momosaky reported a high expression rate of ICAM-1 in HCC (80%-96%). Although three possible mechanisms for the expression of ICAM-1 were considered, Torri et al hold that malignant transformation of liver cells appeared to be the most important mechanism for the ICAM-1 expression in HCC. Thus they concluded that examination of ICAM-1 might yield significant information on the process of malignant transformation of hepatocytes[41,43]. In the nude mouse liver cancer metastasis model, Sun JJ et al demostrated that tissue ICAM-1 and sICAM-1 could indicate the stage of HCC, potential of hepatoma cells for invasion and metastasis[44]. In addition, in vitro study by Momosaky et al[43] showed that HCC cell itself markedly secreted soluble ICAM-1 into the culture supernantant in tumor cell lines. On the other hand, no soluble ICAM-1 was shed from normal mouse hepatocytes regardless of the presence or absence of cytokine stimuli[43]. According to the observations from the present and other studies mentioned above, we think that high levels of sICAM-1 in HCC patients might be released mostly from the tumor cells.
After the clinical and immunohistochemical studies, we have recently investigated the correlation between serum levels of sICAM-1 and expression of its mRNA in HCC tissues. The results (Table 2) suggested that hepatocytes transformation may be the essential cause for strong expression of ICAM-1 mRNA, as in carcinomatous tissues of the 43 patients, the positive rate of expression was 65.1% (28/43). However, that in non-carcinomatous tissues was only 30% (13/43), which was quite different from the HCC tissues (P < 0.01), and in normal liver tissues expression of ICAM-1 mRNA did not exist. Furthermore, the same correlation between the expression of ICAM-1 mRNA and the serum concentrations of sICAM-1 was observed. In patients with serum levels of sICAM-1 above 1000 μg/L, the expression rates of ICAM-1 mRNA in HCC and adjacent tissues were 75% and 34.4%, respectively, however, in group with sICAM-1 lower than 1000 μg/L, the expression rates were 36.4% and 18.2% respectively, which indicated that the expression of ICAM-1 protein was controlled by its correlative gene at the level of transcription regulation.
The expression rate of ICAM-1 mRNA was also related to the severity of liver cirrhosis and intrahepatic metastasis of tumor. Particularly in the later circumstances, the expression rate was much higher in metastatic patients (86.7%) than those without metastasis (53.6%), which suggested that the expression of ICAM-1 mRNA may play an important role in tumor intra and extrahepatic spread. These results were identical to our clinical observations, in which the proportion of sICAM-1 level > 1000 μg/L was higher than that of AFP (73.2% vs 60%) and sICAM-1 level was more sensitive than liver image examinations in indicating tumor recurrence.
Based on our studies on expressions of ICAM-1 and its mRNA in serum and tissues of HCC, we concluded that: ① Serum levels of sICAM-1 in HCC were significantly higher than that in benign liver diseases and normal controls, which indicated that it is useful to measure sICAM-1 to differentiate HCC from other benign lesions when the level of sICAM-1 is higher than 1000 μg/L. ② The high expression level of sICAM-1 might result from the strong expression of ICAM-1 in HCC tissue, which was controlled by its related gene. The source of sICAM-1 in HCC was originated mainly from HCC cells. ③ In HCC with intrahepatic metastasis, the expression of ICAM-1 mRNA was significantly high, which suggested that detecting sICAM-1 is of important value in predicting tumor recurrence after surgery. ④ With understanding of the mechanism of ICAM-1 expression and its origination, we believe that measurement of sICAM-1 may be of diagnostic value for HCC, particularly in patients with low levels of serum AFP.
ACKNOWLEDGEMENT
We gratefully acknowledge Prof. Meuer for his cooperation, Dr. Shraven for the primers of PCR; and Yong Ming Liu, and Si En Zen for their excellent works in this study.
Footnotes
Supported by the grant from the Guangxi Science and Technology Committee, No.9811003
Edited by Ma JY
References
- 1.Marlin SD, Springer TA. Purified intercellular adhesion molecule-1 (ICAM-1) is a ligand for lymphocyte function-associated antigen 1 (LFA-1) Cell. 1987;51:813–819. doi: 10.1016/0092-8674(87)90104-8. [DOI] [PubMed] [Google Scholar]
- 2.Wang YJ, Sun ZQ, Yu JJ, Xu XZ, Zhang X, Quan QZ. Biological effects of type I and III collagens in human hepatocellular carci-noma tissue. China Natl J New Gastroenterol. 1995;1:18–20. [Google Scholar]
- 3.Osborn L, Hession C, Tizard R, Vassallo C, Luhowskyj S, Chi-Rosso G, Lobb R. Direct expression cloning of vascular cell adhesion molecule 1, a cytokine-induced endothelial protein that binds to lymphocytes. Cell. 1989;59:1203–1211. doi: 10.1016/0092-8674(89)90775-7. [DOI] [PubMed] [Google Scholar]
- 4.Staunton DE, Merluzzi VJ, Rothlein R, Barton R, Marlin SD, Springer TA. A cell adhesion molecule, ICAM-1, is the major surface receptor for rhinoviruses. Cell. 1989;56:849–853. doi: 10.1016/0092-8674(89)90689-2. [DOI] [PubMed] [Google Scholar]
- 5.Adams DH, Hubscher SG, Shaw J, Rothlein R, Neuberger JM. Intercellular adhesion molecule 1 on liver allografts during rejection. Lancet. 1989;2:1122–1125. doi: 10.1016/s0140-6736(89)91489-x. [DOI] [PubMed] [Google Scholar]
- 6.Vogetseder W, Feichtinger H, Schulz TF, Schwaeble W, Tabaczewski P, Mitterer M, Böck G, Marth C, Dapunt O, Mikuz G. Expression of 7F7-antigen, a human adhesion molecule identical to intercellular adhesion molecule-1 (ICAM-1) in human carcinomas and their stromal fibroblasts. Int J Cancer. 1989;43:768–773. doi: 10.1002/ijc.2910430504. [DOI] [PubMed] [Google Scholar]
- 7.Adams DH, Hubscher SG, Shaw J, Johnson GD, Babbs C, Rothlein R, Neuberger JM. Increased expression of intercellular adhesion molecule 1 on bile ducts in primary biliary cirrhosis and primary sclerosing cholangitis. Hepatology. 1991;14:426–431. [PubMed] [Google Scholar]
- 8.Zöhrens G, Armbrust T, Pirzer U, Meyer zum Büschenfelde KH, Ramadori G. Intercellular adhesion molecule-1 concentration in sera of patients with acute and chronic liver disease: relationship to disease activity and cirrhosis. Hepatology. 1993;18:798–802. doi: 10.1002/hep.1840180408. [DOI] [PubMed] [Google Scholar]
- 9.Morita M, Watanabe Y, Akaike T. Inflammatory cytokines up-regulate intercellular adhesion molecule-1 expression on primary cultured mouse hepatocytes and T-lymphocyte adhesion. Hepatology. 1994;19:426–431. [PubMed] [Google Scholar]
- 10.Hutchins D, Steel CM. Regulation of ICAM-1 (CD54) expression in human breast cancer cell lines by interleukin 6 and fibroblast-derived factors. Int J Cancer. 1994;58:80–84. doi: 10.1002/ijc.2910580114. [DOI] [PubMed] [Google Scholar]
- 11.Zhang BH, Wu MC. Evaluation of serum AFP-reactive-lentil lec-tin determined by its mAb in the diagnosis of hepatocellular carcinoma. China Natl J New Gastroenterol. 1995;1:33–36. [Google Scholar]
- 12.Seth R, Raymond FD, Makgoba MW. Circulating ICAM-1 isoforms: diagnostic prospects for inflammatory and immune disorders. Lancet. 1991;338:83–84. doi: 10.1016/0140-6736(91)90077-3. [DOI] [PubMed] [Google Scholar]
- 13.Schwaeble W, Kerlin M, Meyer zum Büschenfelde KH, Dippold W. De novo expression of intercellular adhesion molecule 1 (ICAM-1, CD54) in pancreas cancer. Int J Cancer. 1993;53:328–333. doi: 10.1002/ijc.2910530226. [DOI] [PubMed] [Google Scholar]
- 14.Voraberger G, Schäfer R, Stratowa C. Cloning of the human gene for intercellular adhesion molecule 1 and analysis of its 5'-regulatory region. Induction by cytokines and phorbol ester. J Immunol. 1991;147:2777–2786. [PubMed] [Google Scholar]
- 15.Adams DH, Mainolfi E, Burra P, Neuberger JM, Ayres R, Elias E, Rothlein R. Detection of circulating intercellular adhesion molecule-1 in chronic liver diseases. Hepatology. 1992;16:810–814. doi: 10.1002/hep.1840160330. [DOI] [PubMed] [Google Scholar]
- 16.Chen J, Gong XY, Zhang YF. Clinical significance and immunogical measurement of cell adhesion molecules. Guowai Yixue Mianyixue Fence. 1993;6:310–313. [Google Scholar]
- 17.Tanaka Y, Hayashi M, Takagi S, Yoshie O. Differential transactivation of the intercellular adhesion molecule 1 gene promoter by Tax1 and Tax2 of human T-cell leukemia viruses. J Virol. 1996;70:8508–8517. doi: 10.1128/jvi.70.12.8508-8517.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang JF, Zhang B, Liu SF. Clinical significance of soluble inter-cellular adhesion molecule-1. Shanghai Mianyixue Zazhi. 1994;14:374–375. [Google Scholar]
- 19.Chen GY, Cao XT, Yu YZ, Zhang WP, Tao Q. Interleukin (IL)-2. Or IL-4 gene transfer in human melanoma cell, expression and function of intercellular adhesion molecule-1. Zhongguo Mianyixue Zazhi. 1996;12:20–22. [Google Scholar]
- 20.Muñoz C, Castellanos MC, Alfranca A, Vara A, Esteban MA, Redondo JM, de Landázuri MO. Transcriptional up-regulation of intracellular adhesion molecule-1 in human endothelial cells by the antioxidant pyrrolidine dithiocarbamate involves the activation of activating protein-1. J Immunol. 1996;157:3587–3597. [PubMed] [Google Scholar]
- 21.Dustin ML, Springer TA. Lymphocyte function-associated antigen-1 (LFA-1) interaction with intercellular adhesion molecule-1 (ICAM-1) is one of at least three mechanisms for lymphocyte adhesion to cultured endothelial cells. J Cell Biol. 1988;107:321–331. doi: 10.1083/jcb.107.1.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Budnik A, Grewe M, Gyufko K, Krutmann J. Analysis of the production of soluble ICAM-1 molecules by human cells. Exp Hematol. 1996;24:352–359. [PubMed] [Google Scholar]
- 23.Tsujisaki M, Imai K, Hirata H, Hanzawa Y, Masuya J, Nakano T, Sugiyama T, Matsui M, Hinoda Y, Yachi A. Detection of circulating intercellular adhesion molecule-1 antigen in malignant diseases. Clin Exp Immunol. 1991;85:3–8. doi: 10.1111/j.1365-2249.1991.tb05673.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Torii A, Harada A, Nakao A, Nonami T, Ito M, Takagi H. Expression of intercellular adhesion molecule-1 in hepatocellular carcinoma. J Surg Oncol. 1993;53:239–242. doi: 10.1002/jso.2930530410. [DOI] [PubMed] [Google Scholar]
- 25.Feng GS, Kramann B, Zheng CS, Zhou RM, Liang B, Zhang YF. Comparative study on the effects of hepatic arterial embolization with Bletilla Striata or gelfoam in the treatment of primary hepatic carcinoma. China Natl J New Gastroenterol. 1996;2:158–160. [Google Scholar]
- 26.Wang D, Shi JQ. Overexpression and mutations of tumor suppressor gene p53 in hepatocellular carcinoma. China Natl J New Gastroenterol. 1996;2:161–164. [Google Scholar]
- 27.Hu SX, Fang GY. Clinical use of hepatic carcinoma associated membrane protein antigen (HAg18-1) for detection of primary hepatocellular carcinoma. China Natl J New Gastroenterol. 1996;2:165–166. [Google Scholar]
- 28.Sun JJ, Zhou XD, Liu YK, Zhou G, Chen J, Tang ZY. Phasic expression of tissue intercellular adhesion molecule-1 in human liver cancer metastasis model in nude mice. Zhonghua Shiyan Waike Zazhi. 1999;16:155–156. [Google Scholar]
- 29.Sun JJ, Zhou XD, Zhou G, Liu YK. Expression of intercellular adhesive molecule-1 in liver cancer tissues andliver cancer metastasis. World J Gastroenterol. 1998;4:202–205. doi: 10.3748/wjg.v4.i3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sun JJ, Zhou XD, Liu YK, Zhou G. Phase tissue intercellular adhesion molecule-1 expression in nude mice human liver cancer metastasis model. World J Gastroenterol. 1998;4:314–316. doi: 10.3748/wjg.v4.i4.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu J, Mei MH, Dai ZB. Significance of detecting intercellular adhesion molecule-1 in hepatocellular carcinoma. Guowai Yixue Mianyixue Fence. 1998;21:86–89. [Google Scholar]
- 32.Mei MH, Xu J, Chen Q, Yang JH, Deng W, Shi QF, Tan LL. Measurement of serum and bile intercellular adhesion molecule-1 in patients with obstructive jaundice. Huazhong Yixue Zazhi. 2000;24:2–3. [Google Scholar]
- 33.Xu J, Mei MH, Shi QF. Clinical value of serum circulating intercel-lular adhesion molecule-1 in hepatocellular carcinoma. Zhonghua Shiyan Waike Zazhi. 1998;15:514–515. [Google Scholar]
- 34.Mei MH, Xu J, Shi QF, Chen Q, Qin LL. Measurement of serum circulating intercellular adhesion molecule-1 and its clinical significance in hepatocellular carcinoma. J Hepatobiliary Pancreat Surg. 1999;6:181–185. doi: 10.1007/s005340050103. [DOI] [PubMed] [Google Scholar]
- 35.Mei MH, Xu J, Shi QF, Yang JH, Chen Q, Qin LL. Clinical significance of serum intercellular adhesion molecule-1 detection in patients with hepatocellular carcinoma. World J Gastroenterol. 2000;6:408–410. doi: 10.3748/wjg.v6.i3.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu J, Mei MH, Shi QF. Combining with sevral marks for diagnosis of primary in hepatocellular carcinoma. Huazhong Yixue Zazhi. 2000;24:81–82. [Google Scholar]
- 37.Hyodo I, Jinno K, Tanimizu M, Doi T, Nishikawa Y, Hosokawa Y, Moriwaki S. Intercellular adhesion molecule-1 release from human hepatocellular carcinoma. Cancer Detect Prev. 1996;20:308–315. [PubMed] [Google Scholar]
- 38.Chomczynski P, Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem. 1987;162:156–159. doi: 10.1006/abio.1987.9999. [DOI] [PubMed] [Google Scholar]
- 39.Viganò P, Gaffuri B, Ragni G, Di Blasio AM, Vignali M. Intercellular adhesion molecule-1 is expressed on human granulosa cells and mediates their binding to lymphoid cells. J Clin Endocrinol Metab. 1997;82:101–105. doi: 10.1210/jcem.82.1.3646. [DOI] [PubMed] [Google Scholar]
- 40.Tang ZY. Clinical research of hepatocellular carcinoma in the 21st century. China Natl J New Gastroenterol. 1995;1:2–3. [Google Scholar]
- 41.Shimizu Y, Minemura M, Tsukishiro T, Kashii Y, Miyamoto M, Nishimori H, Higuchi K, Watanabe A. Serum concentration of intercellular adhesion molecule-1 in patients with hepatocellular carcinoma is a marker of the disease progression and prognosis. Hepatology. 1995;22:525–531. [PubMed] [Google Scholar]
- 42.Sun JJ, Zhou XD, Liu YK, Tang ZY, Feng JX, Zhou G, Xue Q, Chen J. Invasion and metastasis of liver cancer: expression of intercellular adhesion molecule 1. J Cancer Res Clin Oncol. 1999;125:28–34. doi: 10.1007/s004320050238. [DOI] [PubMed] [Google Scholar]
- 43.Momosaki S, Yano H, Ogasawara S, Higaki K, Hisaka T, Kojiro M. Expression of intercellular adhesion molecule 1 in human hepatocellular carcinoma. Hepatology. 1995;22:1708–1713. [PubMed] [Google Scholar]
- 44.Hyodo I, Jinno K, Tanimizu M, Hosokawa Y, Nishikawa Y, Akiyama M, Mandai K, Moriwaki S. Detection of circulating intercellular adhesion molecule-1 in hepatocellular carcinoma. Int J Cancer. 1993;55:775–779. doi: 10.1002/ijc.2910550514. [DOI] [PubMed] [Google Scholar]


