Highlights
-
•
Leiomyosarcoma in the vagina is rare.
-
•
Atypical fibroids recurring as leiomyosarcoma
-
•
Leiomyomas should be classified based on recurrence risk.
Keywords: Leiomyosarcoma, Atypical, Leiomyoma, Vaginal
1. Introduction
Recurrent, atypical leiomyoma following hysterectomy is rare. Furthermore, recurrence in the form of leiomyosarcoma is even less common. Treatment recommendations as well as prognosis are based on expert-opinion and case reports.
2. Case report
Our patient presented as a 53 year-old gravida 0 with a history of enlarging fibroids, menorrhagia and an abnormal Pap smear, AS-CUS cannot rule out ASC-H. A colposcopy revealed HGSIL and an ECC showed LGSIL. Her medical history is significant for colitis and hypothyroidism. She had an ultrasound that revealed an enlarged uterus including a new fibroid compared to an ultrasound one year prior. The uterus measured 17.9 × 10.7 × 13.7 cm. She desired definitive treatment. An endometrial biopsy was benign. She underwent a robotically-assisted total laparoscopic hysterectomy with bilateral salpingo-oophorectomy with a mini-laparotomy for specimen retrieval. The specimen was not morcellated either in bag or intra-abdominally. A Rumi-KOH uterine manipulator was utilized during surgery. The final pathologic diagnosis was atypical leiomyoma with cytologic atypia of the symplastic type (Fig. 1). The histopathologic diagnosis was confirmed by external review of an independent pathologist. The patient did well following surgery and was discharged. Twenty-two months later, she presented to the office with complaint of a vaginal mass that had been growing over a few months. A 5-6 cm submucosal, well-demarcated, spherical, mobile, non-tender mass was appreciated arising from the posterior aspect of the vagina at the level of the hymenal ring. She underwent resection of the mass. The specimen was removed via posterior colporrhaphy. The specimen was noted to be cystic and soft with apparent degenerative necrosis. The entire mass was removed; however it was removed in a piecemeal fashion due to the soft and friable nature of the tumor. The final pathologic diagnosis was a low to intermediate grade leiomyosarcoma with margins favored to be positive (Supplemental S1). The same external pathologist was consulted as in the patient's first surgery and there was again agreement upon this histopathologic diagnosis. The original specimen slides were available and were re-reviewed and the tumors were felt to be different histologically such that the leiomyosarcoma arising in the vagina represented a recurrence of the original disease via transformation of a symplastic atypical leiomyoma into a leiomyosarcoma. The patient underwent a PET/CT, which was negative for metastatic disease. Whole pelvic and vaginal brachytherapy was recommended but patient declined. The treating physician and patient agreed upon chemotherapy. She completed four cycles of a chemotherapy regimen consisting of gemcitabine 750 mg/m2 on days 1 and 8 as well as docetaxel 75 mg/m2 on day 8 every 21 days.
Fig. 1.
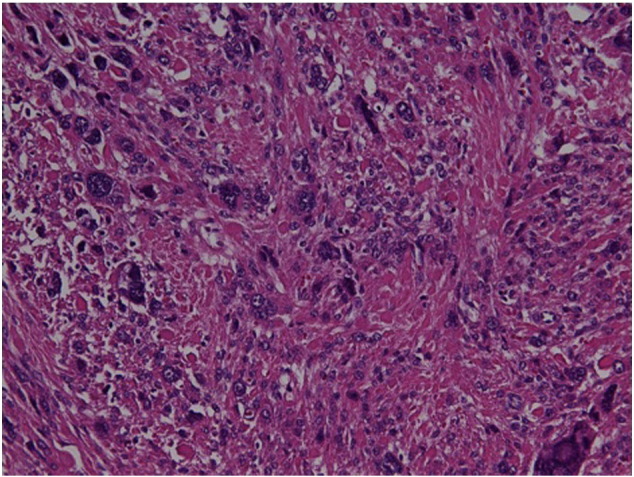
This image at 200 × magnification shows an atypical leiomyoma due to diffuse cytologic atypia of the symplastic type/bizarre atypia. There is no evidence of coagulative necrosis and no increased mitotic activity and this did not meet the criteria for leiomyosarcoma.
S1.
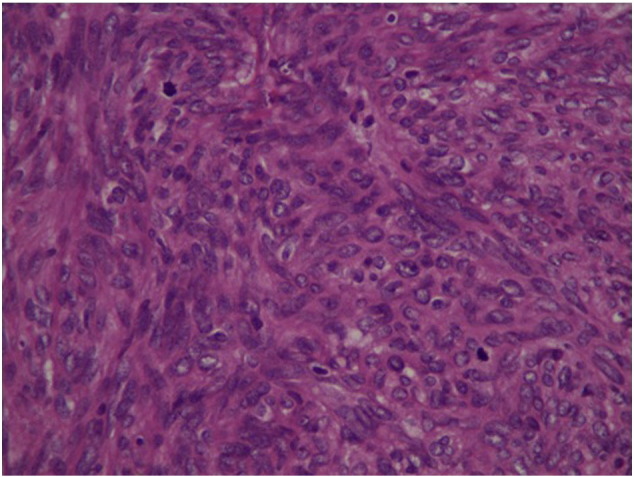
This image at 400 × magnification depicts numerous mitotic figures at a rate of 7–12/high power fields, moderate cytologic atypia and some atypical mitotic figures. This is diagnostic of vaginal leiomyosarcoma of low to intermediate nuclear grade. The vaginal material shows greater hypercellularity compared to the prior and a high mitotic rate but no coagulative necrosis.
3. Discussion
Leiomyosarcoma in the vagina presenting as a recurrence from atypical uterine leiomyomas, as far as we are aware, has not been previously reported. The diagnosis of primary vaginal leiomyosarcoma is rare and represents 2–3% of vaginal cancers (Curtin et al., 1995). The original pathologic specimen showed areas of smooth muscle neoplasm interspersed with foci of bizzare, atypical cells. No mitotic figures or coagulative necrosis was present. Based on the World Health Organization revised criteria this patient's original tumor met criteria for the smooth muscle tumor of uncertain malignant potential (STUMP) subgroup of ‘atypical leiomyoma with limited experience’ due to lack of tumor cell necrosis and less than 10 mitotic figures per high powered field (Ip et al., 2010). The vaginal lesion was hypercellular with a high mitotic count among moderate cytologic atypia and no coagulative necrosis thus favoring diagnosis of leiomyosarcoma based on the WHO classification system.
Due to its uncommon occurrence, the presenting symptoms of a leiomyosarcoma arising from or metastatic to the vaginal submucosa are not well described. Our patient's complaint was related to mass effect due to the size and location of her lesion. She did not complain of pain, discharge or abnormal bleeding. Malignant tumors that develop in the vagina have a predilection for the posterior wall (Curtin et al., 1995).
Recurrence risk for atypical leiomyoma including STUMP has been assessed in retrospective studies. A case-study of 51 atypical leiomyomas identified 1 case treated with hysterectomy that recurred with retroperitoneal atypical leiomyoma following an average of 42 months follow-up (Ly et al., 2013). A review by Ip and colleagues (Ip et al., 2010) included bizarre or symplastic leiomyoma under the heading ‘little or no recurrent and/or metastatic potential’ and based diagnosis on that of the Stanford criteria. They site a Stanford study examining 46 cases of atypical leiomyomas of which 4 recurred. Various mitotic counts were observed in the recurrent cases indicating it may not be a reliable predictor of recurrence risk in atypical leiomyomas (Ip et al., 2010). A review of 24 cases of bizarre leiomyoma did not identify any recurrences in all cases with a mean follow-up of 11.2 years (Downes & Hart, 1997). A retrospective evaluation of 67 cases of leiomyosarcoma identified 20 cases that did not meet current diagnostic criteria for leiomyosarcoma and were reclassified as atypical or benign leiomyoma. Of the 18 atypical leiomyoma cases, 3 had recurrence resulting in death. Recurrences occurred between 6 and 11 years following initial diagnosis (Giuntoli et al., 2007). None of these studies identified leiomyosarcoma at the time of recurrence of atypical leiomyoma. It is unclear what produced the recurrence in our patient as her specimen was removed through an abdominal mini-laparotomy and the leiomyoma was not entered during the hysterectomy. The possibility exists that the Rumi-KOH may have seeded the vagina as it was removed following the hysterectomy.
Treatment of leiomyosarcoma arising in the vagina is currently based on expert opinion and should be guided by staging and histologic grading. Vaginal sarcomas should be clinically staged based on FIGO recommendations for vaginal cancers. However, our patient was classified as recurrence of leiomyoma and was treated as such. Treatment of leiomyosarcoma in the vagina should include primary surgical resection with a wide margin followed by radiation plus or minus chemotherapy (Curtin et al., 1995). Studies examining the use of gemcitabine with docetaxel have shown objective response in patients with metastatic leiomyosarcoma as first-line therapy (Hensley et al., 2008). After a multi-disciplinary team met to discuss treatment options our patient was offered chemotherapy with radiation. She declined radiation. Her recommended follow-up was every 3 months to include history and physical exam with symptom-based imaging. A review on soft-tissue sarcomas noted a 70% survival at 5-years and found a favorable outcome when a low-grade sarcoma was diagnosed compared to high-grade. This review included various histologic subtypes and thus may not be applicable to leiomyosarcomas specifically. Additionally, they noted a trend towards high-grade sarcomas recurring as distant metastases as opposed to locally (Curtin et al., 1995).
The recurrence risk of atypical leiomyomas is still poorly understood. We have presented a case here in which bizarre, atypical leiomyomas recurred as leiomyosarcoma in the vagina. Our patient has remained disease free in the 11 months since surgery.
The following is the supplementary data related to this article.
Conflict of interest
The authors acknowledge no conflicts of interest, financial or otherwise, that may have impacted this manuscript.
Footnotes
Disclosures: The authors report no conflict of interest.
Financial support: This study was not supported by any financial contributions or grants.
References
- Curtin J.P., Sorgo P., Slusher B. Soft tissue sarcoma of the vagina and vulva: a clino-pathologic study. Obstet. Gynecol. 1995;86:269–272. doi: 10.1016/0029-7844(95)00160-s. [DOI] [PubMed] [Google Scholar]
- Ip P., Tse K., Tam K. Uterine smooth muscle tumors other than the ordinary leiomyomas and leiomyosarcomas: a review of selected variants with emphasis on recent advances and unusual morphology that may case concern for malignancy. Adv. Anat. Pathol. 2010;17:91–112. doi: 10.1097/PAP.0b013e3181cfb901. [DOI] [PubMed] [Google Scholar]
- Ly A., Mills A.M., McKenney J.K. Atypical leiomyomas of the uterus: clinicopathologic study of 51 cases. Am. J. Surg. Pathol. 2013;37:643–649. doi: 10.1097/PAS.0b013e3182893f36. [DOI] [PubMed] [Google Scholar]
- Downes K.A., Hart W.R. Bizarre leiomyomas of the uterus: a comprehensive pathologic study of 24 cases with long-term follow-up. Am. J. Surg. Pathol. 1997;21:1261–1270. doi: 10.1097/00000478-199711000-00001. [DOI] [PubMed] [Google Scholar]
- Giuntoli R.L., Gostout B.S., DiMarco C.S. Diagnostic criteria for uterine smooth muscle tumors: leiomyoma variants associated with malignant behavior. J. Reprod. Med. 2007;52:1001–1010. [PubMed] [Google Scholar]
- Hensley M.L., Blessing J.A., Mannel R., Rose P.G. Fixed-dose rate gemcitabine plus docetaxel as first-line therapy for metastatic uterine leiomyosarcoma: a gynecologic oncology group phase II trial. Gynecol. Oncol. 2008;109:329–334. doi: 10.1016/j.ygyno.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]


