Abstract
Study question Can treatment of the symptoms of uncomplicated urinary tract infection (UTI) with ibuprofen reduce the rate of antibiotic prescriptions without a significant increase in symptoms, recurrences, or complications?
Methods Women aged 18-65 with typical symptoms of UTI and without risk factors or complications were recruited in 42 German general practices and randomly assigned to treatment with a single dose of fosfomycin 3 g (n=246; 243 analysed) or ibuprofen 3×400 mg (n=248; 241 analysed) for three days (and the respective placebo dummies in both groups). In both groups additional antibiotic treatment was subsequently prescribed as necessary for persistent, worsening, or recurrent symptoms. The primary endpoints were the number of all courses of antibiotic treatment on days 0-28 (for UTI or other conditions) and burden of symptoms on days 0-7. The symptom score included dysuria, frequency/urgency, and low abdominal pain.
Study answer and limitations The 248 women in the ibuprofen group received significantly fewer course of antibiotics, had a significantly higher total burden of symptoms, and more had pyelonephritis. Four serious adverse events occurred that lead to hospital referrals; one of these was potentially related to the trial drug. Results have to be interpreted carefully as they might apply to women with mild to moderate symptoms rather than to all those with an uncomplicated UTI.
What this paper adds Two thirds of women with uncomplicated UTI treated symptomatically with ibuprofen recovered without any antibiotics. Initial symptomatic treatment is a possible approach to be discussed with women willing to avoid immediate antibiotics and to accept a somewhat higher burden of symptoms.
Funding, competing interests, data sharing German Federal Ministry of Education and Research (BMBF) No 01KG1105. Patient level data are available from the corresponding author. Patient consent was not obtained but the data are anonymised and risk of identification is low.
Trial registration No ClinicalTrialGov Identifier NCT01488955.
Introduction
Uncomplicated urinary tract infections are common in many clinical settings but especially in general practice, where they account for 25% of antibiotic prescriptions.1 2 Prescription of antibiotics when many cases are self limiting contributes to increased resistance rates, posing a serious health threat.3 4 Disease burden and treatment costs have to be considered as well.5Escherichia coli, the main causative agent, is increasingly resistant to current antibiotics,6 and the number of new antibiotics being developed is declining. Many current primary care guidelines, however, still recommend antibiotics as a first line treatment,7 8 at least when standard measures do not lead to symptom relief. As urinary tract infection is often self limiting,9 10 11 and less antibiotic prescribing lowers levels of antibiotic resistance,12 13 14 15 efforts should be made to reduce rates of prescription.
Earlier trials assessed placebo compared with antibiotic treatment for urinary tract infection as well as delayed prescription of antibiotics.9 11 16 These trials reported a delayed resolution of symptoms and prolonged time to bacterial clearance but no serious complications. From qualitative studies and surveys, we know that many affected women are aware of the potential disadvantages of antibiotics and might agree to avoid or postpone such treatment.17 18 19
In a pilot study we compared symptomatic (ibuprofen) with antibiotic treatment (ciprofloxacin) in 79 women with uncomplicated urinary tract infection. Although this study was inadequately powered for a definitive result, it showed that ibuprofen was not inferior for symptom resolution, with 24/36 women recovering without antibiotic treatment.10 In the current study we assessed whether the number of antibiotic prescriptions issued for uncomplicated urinary tract infection can be reduced by symptomatic treatment with ibuprofen, reserving antibiotics for women who return with worsening or recurrent symptoms, and without an increase in symptom burden, recurrences, or complications.
Methods
Trial design and participants
ICUTI (Immediate versus Conditional treatment of Urinary Tract Infection) was a double blind randomised multicentre comparative effectiveness trial with two parallel active treatment arms (ibuprofen and fosfomycin). The study was conducted according to the Good Clinical Practice Guidelines and the declaration of Helsinki. Safety data were monitored throughout and assessed every six months by the data and safety monitoring board. Serious adverse events were defined as adverse events leading to admission to hospital, disability, permanent damage, or risk of dying or death.
The detailed study protocol has been published elsewhere.20 From February 2012 to February 2014 practice staff and general practitioners in 42 general practices in northern Germany systematically approached women aged 18-65 with typical symptoms of urinary tract infection for consent. The upper age limit was chosen as until 2013 fosfomycin was approved only for patients up to age 65.
The study was designed as a pragmatic trial in a general practice setting.21 Inclusion criteria were dysuria and/or frequency/urgency of micturition, with or without lower abdominal pain. The main exclusion criteria were any signs of upper urinary tract infection (fever, loin tenderness); current conditions that could increase the likelihood of potentially complicated courses (such as pregnancy or renal diseases); urinary tract infection within the past two weeks; and urinary catheterisation. We also excluded patients currently treated with non-steroidal drugs for pain or antibiotics and those with a history of gastrointestinal ulcers or severe acute or exacerbated chronic conditions.20 Dipstick tests and urine culture were performed, but the results did not affect eligibility.
Participating general practitioners were trained in good clinical practice to ensure patient safety and data quality. In addition to electronic database monitoring, an independent monitor (IFS Göttingen) made one on-site monitoring visit per practice and study nurses from the academic teams made further quality management visits to ensure correct documentation. No major or safety problems were detected; some minor corrections, for example completion of missing data, were instigated and problems with screening failures were discussed.
Randomisation and masking
We used a computerised random number generator to carry out randomisation in blocks of six in a 3:3 ratio. The trial biometrician was not involved in patient recruitment and data collection. The block-wise randomisation implied stratification by site.
An independent pharmacy identically prepared and packed drug units, which were labelled with a code number from the random list. Practices were supplied with packs of six blinded drug units. At inclusion, general practitioners assigned the code number from the drug unit to the patient and all patient related data. Practice teams as well as academic study teams were blinded to allocation and had no access to the random list. For emergency unblinding, sealed opaque envelopes for each random number were kept in the investigator site files, and a random list was kept in the trial pharmacy.
Procedures
The practice teams were asked to assess all women presenting with symptoms of acute urinary tract infection consecutively for inclusion and exclusion criteria. Eligible women completed a questionnaire to score severity of symptoms and impairment of activity. They also provided a urine sample for dipstick, culture, and pregnancy tests. To assess bias and external validity of study findings, symptom questionnaires were also collected from women who declined to take part in the trial or had exclusion criteria. Participating women were handed out the blinded trial drug package containing either ibuprofen tablets (3×400 mg daily for three days plus 1×1 sachet placebo granules) or fosfomycin-trometamol (1×3 g sachet plus 3×3 placebo tablets for three days), according to randomisation. After inclusion, women were asked to start drug treatment themselves. Drug packages had to be returned and were checked for residual drugs.
Women were advised to consult their general practitioners again if symptoms persisted or worsened. In this case, antibiotic treatment was initiated at the discretion of the general practitioner on the basis of the results of urine culture from the baseline visit. Participants received an emergency card providing the telephone number of the trial pharmacy in case emergency unblinding was required. Women scored their daily symptoms and activity impairment in a diary. Study nurses collected data on symptoms as well as drug intake and further antibiotic prescriptions by telephone calls on day 1, 3, 5, and 7, or until recovery. On day 28, data on antibiotic prescriptions, adverse events, and recurrent urinary tract infections were also collected. All data were recorded into a web based data entry system.
One central laboratory in Göttingen performed all urine cultures. The cut off for positive culture was bacterial count >102 cfu/mL. Susceptibility test were performed by disk diffusion according to DIN 58 940 and DIN 58 959 with European Committee on Antimicrobial Susceptibility Testing breakpoints.22
Outcomes
Two co-primary endpoints examined both benefits and risks: the total number of courses of antibiotics on days 0-28 (for urinary tract infection or other conditions)2 23 and burden of symptoms on days 0-7, measured as area under the curve of the sums of daily symptom scores. The symptom score included dysuria, frequency/urgency of micturition, and low abdominal pain, each on a five point scale from 0 (not at all) to 4 (strong/frequent).10 The area under the curve of symptom sum scores has been used before in other trials to measure overall severity and duration of symptoms.24 25 The trial was to be considered as having a positive outcome if superiority in the first and non-inferiority in the second co-primary endpoint could be proved.
Secondary outcomes were the numbers of severe adverse events, complications (febrile urinary tract infection, pyelonephritis, septic syndrome), all adverse events, relapses (recurrent urinary tract infection after initial resolution of symptoms) up to day 28 and within six and 12 months,7 and women without symptoms at days four and seven (defined as a symptom sum score of 0); symptom load until day four and symptom load with regard to specific symptoms until day seven (specified in the trial protocol as symptom burden until day four, related to each of the three symptoms until day seven 7), assessment of activity impairment on days 1-7, measured with a five item score (range 0-4), referring to the time during which a woman’s work or personal activities had been impaired because of urinary tract infection26; and the number of daily defined doses of antibiotics per patient (the latter will be reported in a separate paper). As the wording in the trial registry was not as specific as in the protocol, we use in this paper terms and definitions for outcomes as given in the trial protocol. To determine whether there were differences within the groups based on the results of the urine cultures, we performed a post hoc outcome analysis stratified on the basis of positive or negative results on urine culture. After publication of the protocol but before unblinding the data we decided to split the early follow-up period regarding recurrent urinary tract infections into two periods according to the German urinary tract infection guideline7: early relapse of symptoms (recurrence of symptoms up to day 14, after initial resolution) and recurrence of urinary tract infection after initial resolution from day 15 up to day 28. Rates of recurrent urinary tract infection within the prolonged follow-up at six and 12 months will be reported separately once the follow-up is finished.
Statistical analysis
The sample size calculated for both co-primary outcomes was driven by the non-inferiority part of the trial. If we assume a coefficient of variation of 80%, we would require a sample size of 2×210=420 evaluable patients to reach a power of 90% for the proof of non-inferiority in case of equivalence of the two study arms (one sided α=0.025).27 As we assumed a dropout rate of 15%, we needed to randomise 494 women to achieve the sample size of 420 patients in the per protocol population.20
The primary analysis consisted of two statistical tests as described in the study protocol.20 The first co-primary endpoint—“number of courses of antibiotic treatment”—was tested for superiority of the ibuprofen group with an exact Mann-Whitney rank sum test with a one sided test level of 2.5%. The second co-primary endpoint was tested for non-inferiority of ibuprofen compared with fosfomycin by calculating a two sided 95% confidence interval for the ratio of the symptom burden of the ibuprofen and fosfomycin groups based on a covariance analysis of the log symptom burden with adjustment for baseline log symptom sum score. Non-inferiority was assumed if the total confidence interval was below the non-inferiority margin of 125%. As no standard was available for this kind of study, we followed the suggested margins for bioequivalence studies, which accept levels of 80-120% of the reference as bioequivalent. We analysed the first co-primary endpoint in the intention to treat population, which consisted of all randomised patients with at least one report on use or non-use of antibiotics. The second co-primary endpoint was analysed in the per protocol population, which consisted of all intention to treat patients with complete seven day follow-up symptom score and subsequently in the intention to treat population. In this population, we had to impute a small number of missing values to calculate the area under the curves. For this purpose we applied an expectation-maximisation algorithm to the available score data to estimate means and covariances based on a normality assumption and chose imputations that maximise the likelihood. As the differences to the analysis of the per protocol population were small, we have presented both endpoints in the same intention to treat population for direct comparability.
The secondary endpoints were analysed with exact Mann-Whitney U rank sum tests and χ2 tests at two sided α=0.05 without adjustment for multiplicity or analogous to the second co-primary endpoint.
Patient involvement
No patients were involved in designing the study or explicitly setting outcome measures; however, outcomes were chosen to reflect daily practice and patient preferences described in earlier studies.18 19 Preliminary results were disseminated to study participants through their general practitioners. A lay information flyer with final results will be sent to all participating practices and can be used to inform patients with urinary tract infections.
Results
Randomisation and baseline characteristics
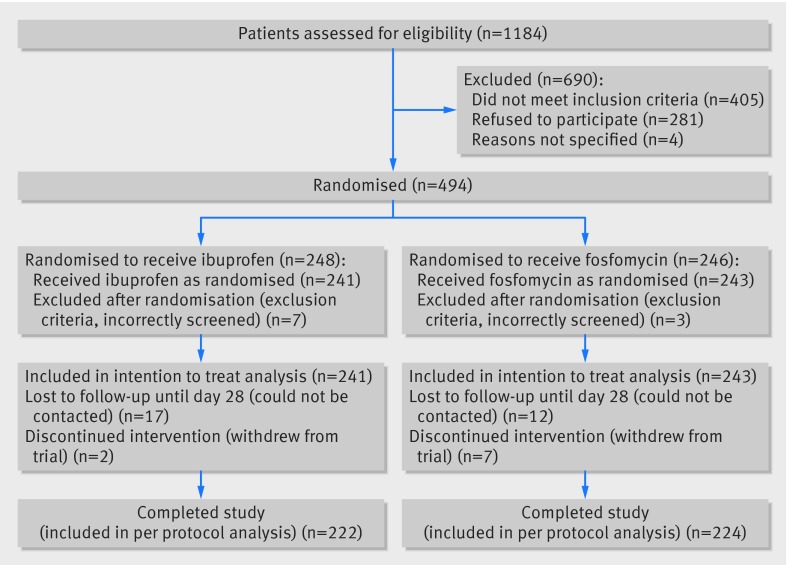
A total of 1184 women with suspected urinary tract infection were screened, 779 were considered eligible, and 494 were randomly assigned to the treatment or control groups (fig 1). On average, 12 women per practice were included in 42 practices.Ten women with exclusion criteria had been included incorrectly by general practitioners and were therefore excluded immediately after recruitment by a masked researcher. The intention to treat population comprised 241 women in the ibuprofen group and 243 in the fosfomycin group. Three women, in whom exclusion criteria were detected later after inclusion, remained in this population. Two women in the ibuprofen group and seven in the fosfomycin group refused further participation and withdrew from the trial.
Fig 1 Flow of participants through trial of ibuprofen versus fosfomycin for women with urinary tract infection
There were no major differences in baseline characteristics between both groups (table 1). Minor differences concerned duration of symptoms (110 (46%) women in the fosfomycin group versus 87 (36%) in the ibuprofen group had symptoms for more than two days) and recurrent urinary tract infections being reported more often by women assigned to the fosfomycin group (54 (23%) versus 42 (17%)).
Table 1.
Baseline characteristics of women with uncomplicated urinary tract infection randomised to ibuprofen or fosfomycin. Figures are numbers of women (percentage) unless stated otherwise
| Ibuprofen (n=241) | Fosfomycin (n=243) | |
|---|---|---|
| Mean (SD) age (years) | 37.3 (14.6) | 37.3 (14.3) |
| Median (IQR) age (years) | 36.0 (24.0-50.0) | 34.0 (24.0-49.0) |
| Duration of symptoms at inclusion (days)*: | ||
| <1 | 50 (21) | 49 (21) |
| 1-2 | 104 (43) | 80 (34) |
| >2-7 | 66 (27) | 82 (34) |
| >7 | 21 (9) | 28 (12) |
| Symptoms at inclusion*: | ||
| Dysuria | 224 (93) | 218 (91) |
| Frequency/urgency | 231 (96) | 232 (97) |
| Low abdominal pain | 172 (71) | 169 (71) |
| Mean (SD) symptom severity sum score† | 6.0 (2.2) | 6.1 (2.5) |
| Median (IQR) symptom severity sum score† | 6.0 (4.0-8.0) | 6.0 (4.0-8.0) |
| Mean (SD) dysuria score‡ | 2.3 (1.0) | 2.3 (1.1) |
| Median (IQR) dysuria score‡ | 3.0 (2.0-3.0) | 2.0 (1.0-3.0) |
| Mean (SD) frequency/urgency score‡ | 2.4 (1.1) | 2.4 (1.1) |
| Median (IQR) frequency/urgency score‡ | 2.0 (2.0-3.0) | 2.0 (2.0-3.0) |
| Mean (SD) low abdominal pain score‡ | 1.3 (1.1) | 1.4 (1.1) |
| Median (IQR) low abdominal pain score‡ | 1.0 (0.0-2.0) | 1.0 (0.0-2.0) |
| Recurrent UTI§ | 42 (17) | 54 (23) |
| Mean (SD) activity impairment score¶ | 9.6 (5) | 8.9 (6) |
| Dipstick results**: | ||
| Leukocytes positive | 205 (85) | 200 (83) |
| Erythrocytes positive | 180 (75) | 189 (78) |
| Nitrite positive | 53 (22) | 46 (19) |
| Culture results: | ||
| Urine culture positive†† | 179/237 (76) | 181/234 (77) |
| E coli | 143/179 (80) | 142/181 (79) |
| Proteus mirabilis | 12/179 (7) | 8/181 (4) |
| Staphylococcus saprophyticus | 8/179 (5) | 8/181 (4) |
| Enterococcus faecalis | 3/179 (2) | 8/181 (4) |
| Streptococcus agalactiae | 0/179 (0) | 2/181 (1) |
| Klebsiella pneumoniae | 3/179 (2) | 1/181 (1) |
| Other uropathogens | 10/179 (6) | 9/181 (5) |
| Not specified | 0/179 (0) | 3/181 (2) |
| Susceptibility to fosfomycin (rate): | ||
| All uropathogens | 168/181 (93) | 162/177 (92) |
| E coli | 142/143 (99) | 142/142 (100) |
SD=standard deviation; IQR=interquartile range; UTI=urinary tract infection.
*n=239 in fosfomycin group.
†Range 0-12. Sum of daily symptom sum scores of dysuria, frequency/urgency of micturition, and low abdominal pain, each on a five point scale from 0 (not at all) to 4 (very strong/frequent).
‡Range 0-4
§UTI within past year.
¶Activity impairment assessment, sum score range 0-20.
**n=242 in fosfomycin group.
††Bacterial count >102 cfu/mL.
Primary outcomes
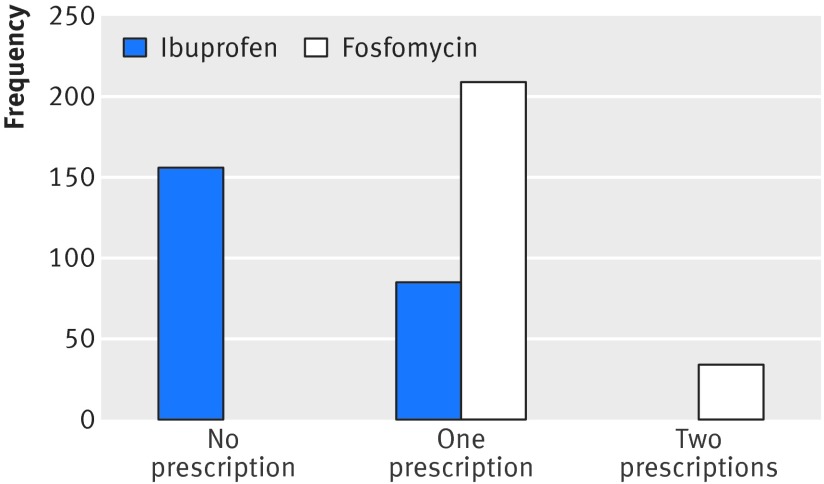
The number of courses of antibiotic treatment within 28 days was significantly lower in the ibuprofen group. The number of all courses in the fosfomycin group was 283 (243 as part of the study plus 34 courses prescribed additionally for urinary tract infection and six courses prescribed for other reasons, such as bronchitis and otitis media) compared with 94 in the ibuprofen group (81 for urinary tract infection and 13 for other reasons). This corresponds to an incidence rate reduction of 66.5% (95% confidence interval 58.8% to 74.4%; P<0.001), showing a substantial reduction of antibiotics use. Figure 2 shows the distribution of the individual number of courses of antibiotics by randomisation group. Although significantly more women received prescriptions of antibiotics in the follow-up period (21.2%), the total number receiving antibiotics was lower in the ibuprofen group by 64.7% (P<0.001, table 2).
Fig 2 Total number of antibiotic prescriptions by randomisation group on days 0-28 (range 0-2, intention to treat population)
Table 2.
Summary of primary and key secondary outcomes in women with uncomplicated urinary tract infection randomised to ibuprofen or fosfomycin. Figures are numbers (percentage) of women unless stated otherwise
| Ibuprofen (n=241) | Fosfomycin (n=243) | % mean difference (95% CI) | P value | |
|---|---|---|---|---|
| Primary endpoints | ||||
| Women who received antibiotics: | ||||
| Total | 85 (35) | 243 (100) | −64.7 (−70.7 to −58.7) | <0.001 |
| By randomisation | 0 (0) | 243 (100) | −100 | — |
| During follow-up (all)* | 85 (35) | 34 (14) | 21.2 (13.8 to 28.7) | <0.001 |
| During follow-up (for UTI) | 75 (31) | 30 (12) | 18.8 (11.6 to 25.9) | <0.001 |
| Mean (SD) symptom burden day 0-7† | 17.3 (11.0) | 12.1 (8.2) | 5.3 (3.5 to 7.0) | <0.001 |
| Secondary endpoints | ||||
| Adverse events in patients: | ||||
| Patients reporting serious adverse events‡ | 4 (2) | 0 (0) | 1.7 (0.0 to 3.3) | 0.06 |
| Serious adverse events probably drug related | 1 (0.4) | 0 (0) | 0.4 (−0.4 to 1.2) | 0.32 |
| Patients reporting adverse events‡ | 42 (17) | 57 (24) | −6.0 (−13.2 to 1.1) | 0.12 |
| Relapses/complications: | ||||
| All recurrent UTI until day 28 | 27 (11) | 34 (14) | −2.8 (−8.7 to 3.1) | 0.41 |
| Early relapse of symptoms (up to day 14)§ | 13 (5) | 7 (3) | 2.5 (−1.0 to 6.1) | 0.18 |
| Recurrence of UTI (day 15-28)§ |
14 (6) | 27 (11) | −5.3 (−10.2 to −0.4) | 0.049 |
| Pyelonephritis§ | 5 (2) | 1 (0.4) | 1.7 (−0.3 to 3.6) | 0.12 |
| Febrile UTI/ (day 0-7)§ | 3 (1) | 0 | 1.2 (−0.2 to 2.6) | 0.12 |
| Worsening symptoms (day 0-7)§ | 8 (3) | 5 (2) | 1.3 (−1.6 to 4.1) | 0.42 |
| Patients without symptoms day 4§ | 91/234 (39) | 129/229 (56) | −17.4 (−26.4 to −8.5) | <0.001 |
| Patients without symptoms day 7¶ | 163/232 (70) | 186/227 (82) | −11.7 (−19.4 to −4.0) | 0.004 |
| Mean (SD) symptom duration after randomisation (days) | 5.6 (2.2) | 4.6 (2.2) | 0.98 (0.59 to 1.38) | <0.001 |
| Mean (SD) symptom burden day 0-4† | 13.1 (7.1) | 10.1 (5.9) | 3.0 (1.9 to 4.2) | <0.001 |
| Mean (SD) symptom burden with regard to dysuria day 0-7 | 6.8 (4.6) | 4.5 (3.6) | 2.3 (1.5 to 3.0) | <0.001 |
| Mean (SD) symptom burden with regard to frequency/urgency day 0-7 | 6.5 (4.1) | 4.6 (3.4) | 1.8 (1.1 to 2.5) | <0.001 |
| Mean (SD) symptom burden with regard to low abdominal pain day 0-7 | 4.1 (4.3) | 2.9 (3.1) | 1.2 (0.5 to 1.8) | 0.001 |
| Mean (SD) activity impairment assessment day 0-7 | 30.3 (24.5) | 19.5 (16.7) | 10.8 (7.1 to 14.6) | <0.001 |
SD=standard deviation; UTI=urinary tract infection.
*Including antibiotic prescriptions for other reasons—for instance, acute bronchitis, otitis.
†Defined as area under curve (AUC) of daily symptom sum scores day 0-7.
‡As rated by patients.
§As rated by general practitioners.
¶Symptom free is defined as symptom sum score=0.
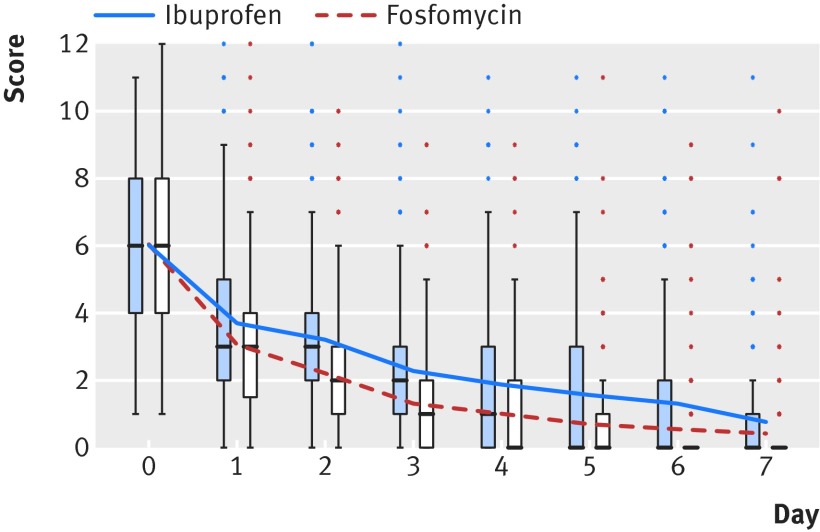
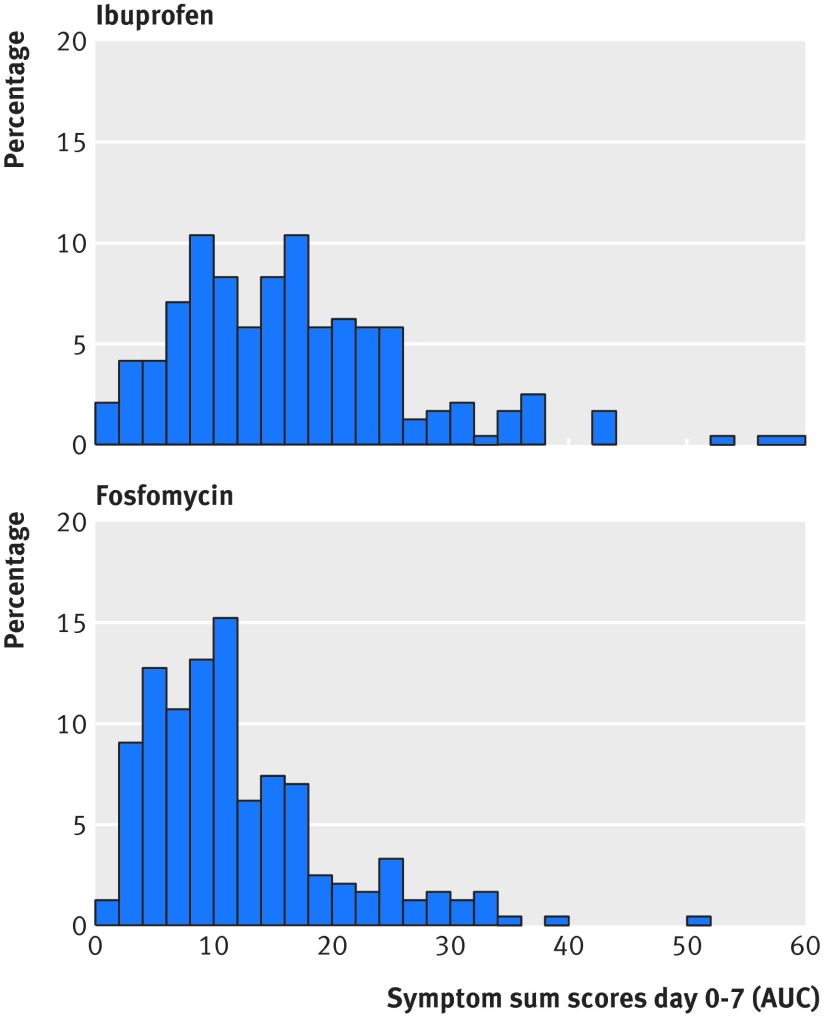
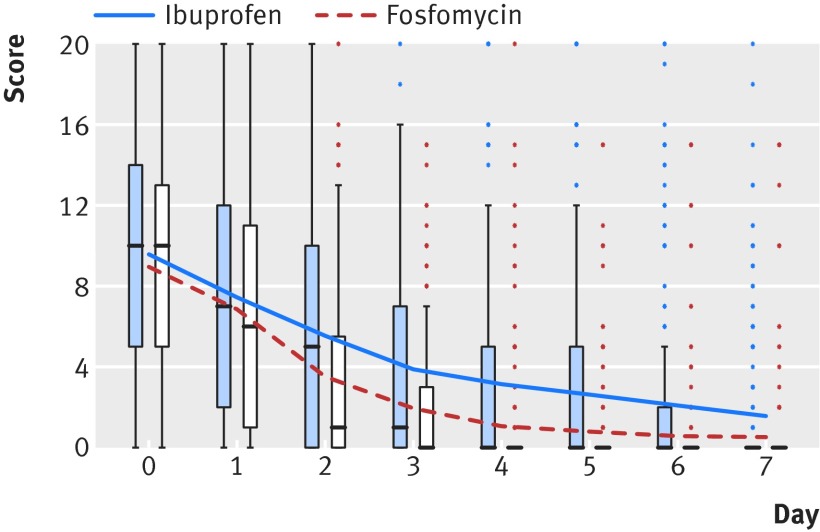
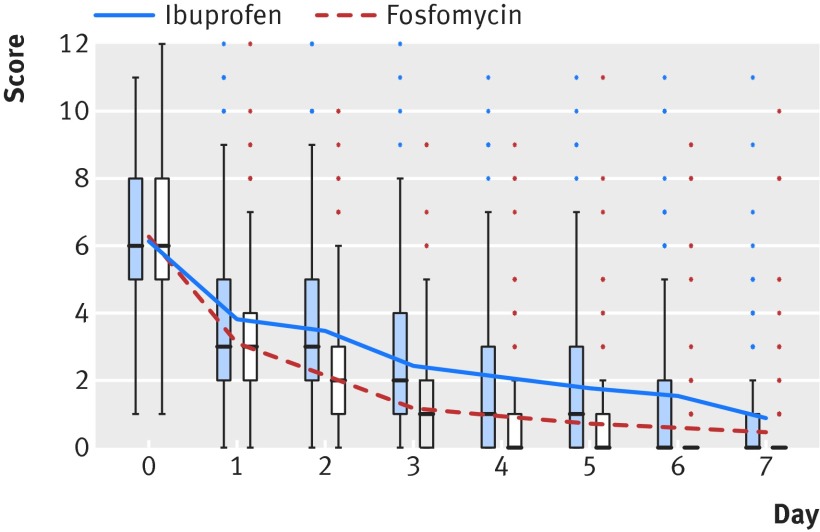
As shown in figure 3, the symptom burden sum score decreased in both groups, from six points on day 0 down to less than one point on day seven, on average. Figure 4 shows the corresponding distribution of the symptom burden area under the curve by randomisation group. Table 2 shows the unadjusted mean symptom burden. With an area under the curve ratio of 140% (areaibu/areafos=140.5%, 95% confidence interval 125.4% to 157.3%) calculated by the adjusted analysis of log disease burden, the non-inferiority margin of 125% was significantly exceeded. We can therefore reject the hypothesis of non-inferiority. The reported effects were essentially the same when we restricted analyses to the per protocol population.
Fig 3 Symptom sum score for dysuria, frequency/urgency, and low abdominal pain on days 0-7by randomisation group (range 0-12, intention to treat population)
Fig 4 Distribution of area under curve (AUC) of symptom sum scores for dysuria, frequency/urgency, and low abdominal pain on days 0-7 by random group (intention to treat population)
Secondary outcomes
All secondary outcomes related to symptoms favoured the fosfomycin group. On days 0-4, the total symptom burden (area under the curve) in the ibuprofen group was significantly higher than in the fosfomycin group. The same results were shown when we considered symptoms individually: for each symptom (dysuria, frequency/urgency, abdominal pain) a higher symptom burden on days 0-7 was seen in the ibuprofen group (table 2).
With a mean duration of 5.6 days, symptoms lasted about a day longer in the ibuprofen group. On day four, 129 (56%) women in the fosfomycin group versus 91 (39%) in the ibuprofen group were symptom free (P<0.001, table 3). Up to day seven these rates increased to 82% and 70%, respectively (P<0.001, table 3).
Table 3.
Patients without symptoms* on day 1-7, intention to treat population of women with uncomplicated urinary tract infection randomised to ibuprofen or fosfomycin. Figures are numbers (percentage) of women unless stated otherwise
| Day without symptoms | Ibuprofen (n=241) | Fosfomycin (n=243) | % mean difference (95% CI) | P value |
|---|---|---|---|---|
| 1 | 12/240 (5) | 21/231 (9) | −4.1 (−8.7 to 0.5) | 0.10 |
| 2 | 30/237 (13) | 45/230 (20) | −6.9 (−13.6 to 0.3) | 0.045 |
| 3 | 57/237 (24) | 101/230 (44) | −19.9 (−28.3 to −11.5) | <0.001 |
| 4 | 91/234 (39) | 129/229 (56) | −17.4 (−26.4 to −8.5) | <0.001 |
| 5 | 118/234 (50) | 152/229 (66) | −15.9 (−24.8 to 7.1) | 0.001 |
| 6 | 133/233 (57) | 178/227 (78) | −21.3 (−29.6 to −13.0) | <0.001 |
| 7 | 163/232 (70) | 186/227 (82) | −11.7 (−19.4 to −4.0) | 0.004 |
*Defined as symptom sum score=0.
Women in the ibuprofen group showed slightly higher scores in impairment of activity—that is, more of their work or regular activities had been impaired by the urinary tract infection (table 4, fig 5). On day seven, 2% of the women overall still felt impaired most or all the time.
Table 4.
Assessment of impairment of activity on day 0-7, intention to treat population of women with uncomplicated urinary tract infection randomised to ibuprofen or fosfomycin. Figures are mean (SD) scores
| AIA sum score day* | Ibuprofen (n=241) | Fosfomycin (n=243) | % mean difference (95% CI) | P value |
|---|---|---|---|---|
| 0 | 9.6 (5.4) (n=241) | 8.9 (5.5) (n=238) | 0.6 (−0.3 to 1.6) | 0.20 |
| 1 | 7.4 (5.7) (n=240) | 6.8 (5.5) (n=231) | 0.6 (−0.4 to 1.6) | 0.24 |
| 2 | 5.6 (5.4) (n=237) | 3.5 (4.4) (n=230) | 2.1 (1.2 to 3.0) | <0.001 |
| 3 | 3.9 (4.8) (n=237) | 1.9 (3.4) (n=230) | 2.0 (1.3 to 2.8) | <0.001 |
| 4 | 3.2 (4.8) (n=234) | 1.1 (2.9) (n=229) | 2.1 (1.4 to 2.8) | <0.001 |
| 5 | 2.6 (4.7) (n=234) | 0.8 (2.4) (n=229) | 1.8 (1.2 to 2.5) | <0.001 |
| 6 | 2.1 (4.4) (n=233) | 0.6 (2.4) (n=227) | 1.5 (0.8 to 2.1) | <0.001 |
| 7 | 1.6 (3.5) (n=232) | 0.6 (2.3) (n=227) | 1.0 (0.5 to 1.6) | <0.001 |
*Activity impairment assessment (AIA) sum scores for five items day 0-7 (range 0-20).
Fig 5 Sum scores for assessment of activity impairment related to urinary tract infection (5 items, range 0-20, intention to treat population)
Subgroup analysis
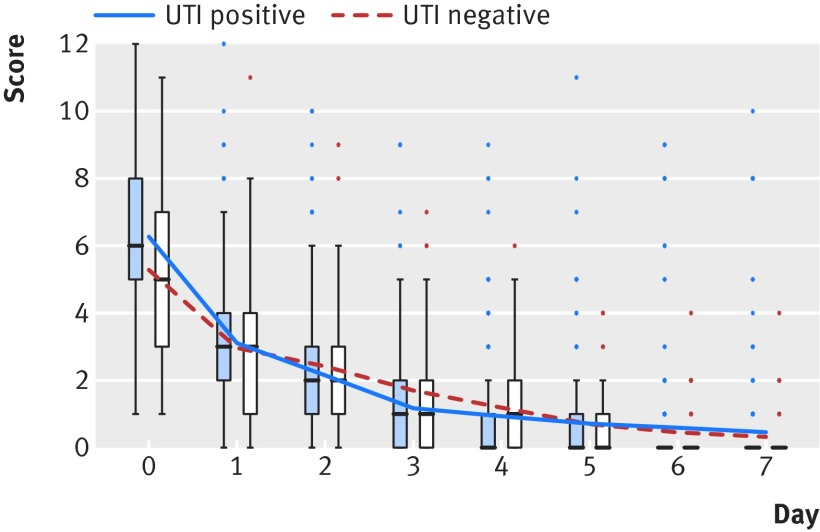
In women with a positive result on urine culture, an average of 0.49 antibiotic treatment courses per patient was prescribed in the ibuprofen group versus 1.18 per patient in the fosfomycin group, corresponding to a reduction by 58.5% (95% confidence interval 49.8% to 67.0%, P<0.001). In women with a negative result 0.10 antibiotic treatment courses per patient were prescribed in the ibuprofen group versus 1.11 in the fosfomycin group—that is, a reduction by 90.7% (74.3% to 99.9%, P<0.001). Symptom burden in patients with negative urine culture results did not differ significantly, whereas in patients with positive results, the ibuprofen group again showed a higher burden of symptoms (figs 6 and 7). In contrast with the ibuprofen group there was no difference in the symptom burden between those with positive and those with negative results on urine culture in the fosfomycin group (fig 8). Table 5 shows differences between women with positive and negative results on urine culture at baseline.
Fig 6 Symptom sum score for women with negative results on urine culture (subgroup analysis, n=111, intention to treat population) on days 0-7
Fig 7 Symptom sum score for women with positive results on urine culture (subgroup analysis, n=360, intention to treat population) on days 0-7
Fig 8 Symptom sum score for women in fosfomycin group with positive versus negative results on urine culture (subgroup analysis, n=234, intention to treat population) on days 0-7
Table 5.
Baseline data from women with proved urinary tract infection (UTI): positive versus negative results on urine culture
| Characteristics | UTI positive (n=360) | UTI negative (n=111) | All (n=471) | |
|---|---|---|---|---|
| Mean (SD) age (years) | 37.7 (14.5) | 35.8 (14.2) | 37.3 (14.4) | |
| Median (IQR) age (years) | 36.0 (24.0-49.0) | 33.0 (23.0-45.0) | 35.0 (24.0-49.0) | |
| No (%) with recurrent UTI | 66/357 (19) | 25/110 (23) | 91/467 (20) | |
| Urinary tract infection symptoms | ||||
| Mean (SD) symptom duration score | 5.2 (2.2) (n=359) | 4.7 (2.3) (n=111) | 5.1 (2.2) (n=470) | |
| Mean (SD) symptom severity score | 6.2 (2.3) (n=358) | 5.5 (2.4) (n=110) | 6.0 (2.3) (n=468) | |
| Median (IQR) symptom severity score | 6.0 (5.0-8.0) | 5.5 (4.0-7.0) | 6.0 (4.0-8.0) | |
| Mean (SD) dysuria | 2.4 (1.0) (n=358) | 1.9 (1.2) (110) | 2.3 (1.1) (n=468) | |
| Median (IQR) dysuria | 3.0 (2.0-3.0) | 2.0 (1.0-3.0) | 3.0 (2.0-3.0) | |
| Mean (SD) frequency/urgency score | 2.4 (1.1) (n=358) | 2.2 (1.0) (n=110) | 2.4 (1.1) (n=468) | |
| Median (IQR) frequency/urgency score | 2.0 (2.0-3.0) | 2.0 (1.0-3.0) | 2.0 (2.0-3.0) | |
| Mean (SD) lower abdominal pain score | 1.4 (1.1) (n=358) | 1.3 (1.1) (n=110) | 1.4 (1.1) (n=468) | |
| Median (IQR) lower abdominal pain score | 1.0 (0-2.0) | 1.0 (0-2.0) | 1.0 (0-2.0) | |
| No (%) with dysuria | 338/358 (94) | 92/110 (84) | 430/468 (92) | |
| No (%) with frequency/urgency | 345/358 (96) | 107/110 (97) | 452/468 (97) | |
| No (%) with low abdominal pain | 251/358 (70) | 80/110 (73) | 331/468 (71) | |
| Mean (SD) activity impairment score | 9.4 (5.4) (n=358) | 8.8 (5.7) (n=109) | 9.3 (5.5) (n=467) | |
| Median (IQR) activity impairment score | 10.0 (5.0-13.0) | 9.0 (4.0-12.0) | 10.0 (5.0-13.0) | |
| No (%) with dipstick results: | ||||
| Leukocytes positive | 316/360 (88) | 82/111 (74) | 398/471 (85) | |
| Erythrocytes positive | 292/360 (81) | 73/111 (66) | 365/471 (78) | |
| Nitrite positive | 83/360 (23) | 12/111 (11) | 95/471 (20) | |
SD=standard deviation; IQR=interquartile range.
Safety
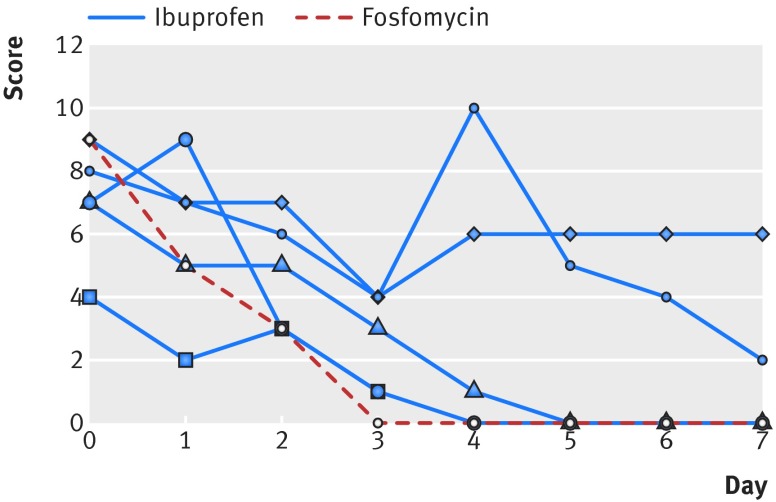
The number of complications differed between groups: there were five cases of pyelonephritis in the ibuprofen group and one in the fosfomycin group (P=0.12). Women who developed pyelonephritis had a higher initial symptom score than average (7.5 versus 6). Five women with pyelonephritis consulted their general practitioners with symptoms of upper urinary tract infection (fever, loin tenderness) in the first seven days; one at day 16. Figure 9 shows the courses of symptoms in women with pyelonephritis. All women were treated as outpatients and recovered fully.
Fig 9 Symptom scores of women with pyelonephritis according to treatment with ibuprofen or fosfomycin on days 0-7
The rate of recurrent urinary tract infection was comparable in both groups. There were, however, significantly more recurrences after day 14 in the fosfomycin group (11% versus 6% in the ibuprofen group, P=0.049, table 2). Of these, 5/14 (36%) women in the ibuprofen group had a prior history of recurrent urinary tract infections compared with 16/27 (60%) in the fosfomycin group. In contrast, more women in the ibuprofen group had early relapses of symptoms (up to day 14), but the difference was not significant. (5% versus 3%; P=0.18, table 2).
There were no significant differences between groups in adverse events not related to urinary tract infection. In the fosfomycin group 57/243 women reported 64 adverse events, whereas in the ibuprofen group 42/241 reported 51 adverse events. Gastrointestinal symptoms (nausea, diarrhoea) were reported more often in the fosfomycin group (15 versus 6). Rashes or vaginal thrush were rare (table 6).
Table 6.
Details on adverse events, intention to treat population of women with uncomplicated urinary tract infection randomised to ibuprofen or fosfomycin
| Classification* | Ibuprofen (n=241) | Fosfomycin (n=243) |
|---|---|---|
| Certain infections and parasitic diseases—such as unspecified viral infection, worms | 3 | 0 |
| Diseases of blood and blood forming organs—such as anaemia | — | 1 |
| Endocrine, nutritional and metabolic diseases—such as goitre | 1 | — |
| Mental and behavioural disorders—such as grief, psychosomatic disorders | 2 | 3 |
| Diseases of the nervous system—such as headache, migraine | 3 | 2 |
| Diseases of the genitourinary system—such as vaginal thrush, local infection | 3 | 1 |
| Diseases of eye and ear—such as unspecific eye lid swelling, otitis, tinnitus | 3 | 5 |
| Diseases of circulatory system—such as hypertonia | — | 1 |
| Diseases of respiratory system—such as upper/lower respiratory infections, asthma | 13 | 12 |
| Diseases of digestive system—such as, nausea, diarrhoea, abdominal pain, vomiting | 6 | 15 |
| Diseases of skin—such as allergy, rash, naevi, eczema, photodermatosis | 3 | 4 |
| Diseases of musculoskeletal system—such as back pain, shoulder syndrome, cervical syndrome | 12 | 14 |
| Injuries and other external causes—such as fall, insect bites | 1 | 4 |
| Symptoms not elsewhere classified—such as abnormal transpiration, non-specific symptoms | 1 | 2 |
| Total No of adverse events | 51 | 64 |
*Classification corresponds to international statistical classification of diseases and related health problems (ICD).
Four patients in the ibuprofen group reported serious adverse events that required hospital admission. One (gastrointestinal haemorrhage) was likely to be drug related; the other three were considered to be unrelated to the drugs (table 7). The woman with gastrointestinal haemorrhage turned out to have an undetected stomach ulcer and alcohol induced hepatitis. Because of a misunderstanding and curiosity, and without having symptoms, one woman unblinded herself using the pharmacy emergency number.
Table 7.
Details of serious adverse events in women with uncomplicated urinary tract infection randomised to ibuprofen or fosfomycin
| Diagnosis | Age (years) | Beginning (days from randomisation) | Hospital admission | Trial drug |
|---|---|---|---|---|
| Bleeding gastric ulcer | 58 | 22 | Yes | Ibuprofen |
| Cardiac palpitations | 37 | 1 | Yes | Ibuprofen |
| Missed miscarriage* | 18 | 63 | Yes | Ibuprofen |
| Acute appendicitis | 21 | 18 | Yes | Ibuprofen |
*One woman assigned to ibuprofen group proved to be pregnant despite negative pregnancy test result at inclusion. Both GP and gynaecologist thought miscarriage was not associated treatment drug.
Non-participants
Non-participants reported higher symptom scores than participants at baseline (8.9 versus 6.0). They had symptoms for longer before visiting the practice, had more recurrent urinary tract infections, and felt more impaired in their daily activities (table 8).
Table 8.
Baseline data of participants and non-participants with uncomplicated urinary tract infection. Figures are number (percentage) of women unless stated otherwise
| Characteristics | Participants (n=484) | Non-participants (n=519) | P value |
|---|---|---|---|
| Duration of symptoms (days): | |||
| <1 | 99/480 (20) | 108/511 (21) | 0.84 |
| 1-2 | 184/480 (38) | 147/511 (29) | 0.001 |
| >2-7 | 148/480 (31) | 192/511 (38) | 0.03 |
| >7 | 49/480 (10) | 64/511 (13) | 0.25 |
| Mean (SD) symptom severity at baseline | 6 (2.3) | 8.9 (2.7) | <0.001 |
| Mean (SD) activity impairment assessment at baseline | 9.3 (5.5) | 14.4 (5.5) | <0.001 |
| Recurrent UTI | 96/479 (20.0) | 127/481 (26.4) | 0.02 |
SD=standard deviation; UTI=urinary tract infection.
Discussion
Principal findings
While initial symptomatic treatment with ibuprofen reduced the overall number of antibiotic treatment courses in women with uncomplicated urinary tract infection by 67%, compared with immediate antibiotic treatment with fosfomycin, this strategy resulted in higher burden of symptoms and more cases of pyelonephritis.
Two thirds of the women in the ibuprofen group, however, recovered without antibiotic treatment. Within 28 days, 34% of the ibuprofen group received antibiotic treatment for persistent or worsening symptoms compared with 14% of the fosfomycin group. These findings are similar to data in the pilot study.10 In our trial, lower antibiotic consumption was “bought” at the expense of a higher burden of symptoms until day seven in the ibuprofen group, with an area under the curve ratio of 140%. Although, to our knowledge, ibuprofen has not previously been compared with placebo in women with urinary tract infection, it is likely to be effective for symptom relief. While in our trial 67% of women in the ibuprofen group recovered without antibiotics, in a previous randomised controlled trial comparing antibiotics with placebo 54% of those in the placebo group recovered9 and in another trial 28% recovered without any antibiotics within a week.16 A protocol on a similar urinary tract infection trial has been published recently, comparing mecillinam with ibuprofen in a higher dose (3×600 mg).28
As for safety aspects, there were more cases of pyelonephritis in the ibuprofen group, and the same trend was observed in worsening symptoms, febrile urinary tract infections, and symptoms of early relapse (up to day 14). Few data exist on the epidemiology of pyelonephritis.5 29 In a meta-analysis of randomised controlled trials comparing placebo with antibiotics, the incidence of pyelonephritis ranged from 0.4% to 2.6% of all urinary tract infections.30 The pyelonephritis rate in the ibuprofen group in our trial was comparably high (2.1%). As the study was not powered to detect significant differences for pyelonephritis, it remains unclear whether this is accidental or due to the lack of antibiotic treatment or possibly due to an effect of ibuprofen on the urogenital system. Further research on this particular outcome is needed.
In our trial, ibuprofen was used to ease symptoms of urinary tract infection. An additional antimicrobial effect against E coli has been postulated by Obad and colleagues but could not be confirmed.31 Currently the same hypothesis is being investigated by Vik and colleagues.28
Recurrent urinary tract infections (day 14-28) were more common in the fosfomycin group. This could be because more women with a history of recurrent urinary tract infection were randomised into the fosfomycin group. Additionally, antimicrobial treatment might result in recurrent urinary tract infections: in a recent trial women with asymptomatic bacteriuria treated with antibiotics had significantly higher rates of subsequent symptomatic urinary tract infection during 12 months’ follow-up than untreated women.32
For external validity and to comply with routine general practice, we chose a symptomatic approach as recommended in primary care guidelines.7 8 33 Therefore, we did not wait for culture results before inclusion and randomisation, and women with negative results on culture remained in the trial. Symptoms and results of urine tests, including the number of negative urine cultures at inclusion, were comparable with other trials in primary care.11 16 34 35 A subgroup analysis stratified for urine culture results in the ibuprofen group showed significant differences in both co-primary outcomes: women with negative results showed significantly lower symptom burden, and antibiotic use was significantly more reduced in women with positive culture results. Although this was a subgroup analysis, and hence hypothesis generating, these results suggest that urine culture results largely predict the (individual) benefit of antibiotics, though a considerable proportion of those with a positive results did not need antibiotics anyway. Proof of bacterial growth might usefully be included in future antibiotic strategies to curtail unnecessary prescriptions. If sufficiently reliable, point of care tests could reduce the time to targeted treatment compared with conventional culture results, which are available only after several days. A European trial is testing the effectiveness of a point of care test for urinary tract infection with results available within 24 hours in general practices.36 Further studies could also provide information on which women with positive test results would require antibiotics and which are likely to recover with symptomatic treatment.
The overall rates of adverse events were comparably low in both groups. The only serious adverse event related to the drug in the ibuprofen group was a gastrointestinal haemorrhage in a woman with alcohol disease, undetected stomach ulcer, and alcohol induced hepatitis. Although rare in otherwise healthy younger women, risks for this serious side effect should be assessed carefully before ibuprofen is prescribed.
Strength and limitations
We were able to enrol more than half of all potentially eligible women, ensuring external validity. While the collection of baseline data from non-participants was a strength of our study, comparison showed that inclusion was biased towards patients with less severe symptoms. This could be caused by self selection, with women with more severe symptoms expressing a preference for antibiotics or general practitioners perceiving sicker patients as unsuitable for the trial.37 Results therefore have to be interpreted carefully as they might apply only to patients with mild to moderate symptoms rather than all women with an uncomplicated urinary tract infection.
Another limitation was that both symptom score and the resulting measurement of the area under the curve were not validated, and the relevance for affected patients was not formally proved. In our pilot study the primary outcome had been symptom resolution at day 4. This did not adequately feature the severity of symptoms or their duration beyond day 4. We therefore chose the area under the curve of symptom sum score up to day 7 as a pragmatic comprehensive outcome that summarises the aspects of symptom severity and duration relevant to patients, instead of focusing on a single aspect at a prespecified point in time. The validated disease specific activity impairment score showed similar courses.
To further improve outcome measures in future trials, patients’ experiences and preferences have to be assessed carefully. Patients should be involved in the development of scores and outcomes. As shown in previous trials, the strategy of delayed prescription could be a welcome and safe alternative for patients who are willing to try treatment other than with antibiotics but want to avoid a reconsultation. This strategy did not reduce antibiotic consumption as effectively as in our trial, but the rate of complications was lower.38
The higher rate of pyelonephritis and the fact that more women experienced worsening symptoms and febrile urinary tract infection when treated with ibuprofen needs to be assessed further in controlled trials with larger patient samples. Furthermore, factors associated with successful symptomatic treatment—particularly in patients with positive results on urine culture—should be analysed to develop a decision aid as a tool for physicians and patients to assess whether to treat symptomatically or not.
Conclusions
We have to reject the hypothesis of non-inferiority of initial symptomatic treatment, and we cannot generally recommend the ibuprofen first approach. This treatment option, however, can be discussed with women with mild to moderate symptoms in a shared decision making approach or within a strategy of delayed prescription. Future research is needed to identify patients for whom symptomatic treatment is sufficient as it has the potential to considerably reduce the number of antibiotic prescriptions for women with mild to moderate symptoms of urinary tract infection, in particular those with negative results on culture.
What is already known on this topic
Women with uncomplicated urinary tract infection are usually treated with antibiotics
It is unknown if symptomatic treatment is a suitable alternative approach with regard to symptoms and to what extent such treatment can reduce the overall antibiotic prescription rate
What this study adds
Compared with fosfomycin, initial treatment with ibuprofen substantially reduced antibiotic use in women aged 18-65 with mild to moderate symptoms of urinary tract infection but was less effective for symptom relief, and there were more cases of pyelonephritis
This treatment regimen can be discussed with women who are willing to avoid antibiotics or to accept a delayed prescription
We thank all participating women and all general practice investigators and their teams (Drs Albrecht, Annweiler, Baumgarten, Beverungen, Borchers, Böttcher, Brockstedt, Brucker, Buck, Coutelle, Dickow, Dockhorn, Egidi, Ertel, Falkenstein, Fleige, Gemen, Gerken, Glatzel, Gosewisch, Heiken, Hermann, Hiller, Hilgenberg, Holm, Keske, Kiwit-Putzer, Klinger-Bültemann, Knöpfel, Koch, Köhler, Löber, Lückerath, Meggers, Meier-Ahrens, Menke, Müller, Neidhardt, Preiskorn, Rötterink, Schaper, Schelp, Schmiemann, Schmitz, Seker, Stegemann, Wilde, Zedler, Zimny). We are grateful to our dedicated research nurses H Schneider-Rudt, C Tomala, J Westphal, and K Jürgensen-Muziol. We also thank Ludwig Balzer for support in the statistical analysis and Frank Sullivan for checking of some English language points.
Data Safety and Monitoring Board: Norbert Donner-Banzhoff (Philipps-University Marburg, Department of General Practice, Preventive and Rehabilitation Medicine), Jürgen Brockmöller (University Medical Centre Göttingen, Clinical Pharmacology), Helmut Eiffert (University Medical Centre Göttingen, Institute for Medical Microbiology), Wilhelm Niebling (University Medical Centre Freiburg, Division of General Practice), Andreas Sönnichsen (Institute for General Practice and Family Medicine, Faculty of Health, Witten/Herdecke), Hans-Joachim Trampisch (Ruhr-University Bochum, Department of Medical Informatics and Epidemiology).
Contributors: IG and JB contributed equally to the manuscript and share first authorship. All authors conceived the concept and designed and supervised to study; acquired, analysed, and interpreted the data; and drafted and revised the manuscript. KW carried out the statistical analysis. EH-P obtained funding. The Institute for Clinical Research, Göttingen (IFS), pharmacy of the Charité (Berlin), medical laboratory AMEDES Holding AG (Göttingen) contributed administrative, material, and technical support. EH-P and IG are guarantors.
Funding: The trial was funded by the German Federal Ministry of Education and Research (BMBF) No 01KG1105. The funder had no role in trial design, data collection, analysis, or reporting.
Competing interests: All authors have completed the uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: support from the German Federal Ministry of Education and Research for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; and no other relationships or activities that could appear to have influenced the submitted work. The University of Göttingen was responsible for the initiation, quality control and financial management the clinical study but did not participate in the collection, clinical project management, analysis, and interpretation of data.
Ethical approval: This study was approved by the ethics committee of Hannover Medical School (No 5986M). All participants provided written informed consent.
Transparency: The guarantors affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies are disclosed.
Data sharing: Patient level data are available on reasonable request from the corresponding author. Patient consent was not obtained but the presented data are anonymised and risk of identification is low.
References
- 1.Hooton TM. Clinical practice. Uncomplicated urinary tract infection. N Engl J Med 2012;366: 1028-37. 10.1056/NEJMcp1104429 22417256 [DOI] [PubMed] [Google Scholar]
- 2.Ong DS, Kuyvenhoven MM, van Dijk L, Verheij TJ. Antibiotics for respiratory, ear and urinary tract disorders and consistency among GPs. J Antimicrob Chemother 2008;62: 587-92. 10.1093/jac/dkn230 18544602 [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2013. www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf.
- 4.World Health Organization. Antimicrobial resistance: Global Report on Surveillance 2014 2014. http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf.
- 5.Foxman B. Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin North Am 2014;28: 1-13. 10.1016/j.idc.2013.09.003 24484571 [DOI] [PubMed] [Google Scholar]
- 6.Donnan PT, Wei L, Steinke DTet al. Presence of bacteriuria caused by trimethoprim resistant bacteria in patients prescribed antibiotics: multilevel model with practice and individual patient data. BMJ 2004;328: 1297. 10.1136/bmj.328.7451.1297 15166067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Epidemiology, diagnostics, therapy and management of uncomplicated bacterial community acquired urinary tract infection in adults: German S3-Guideline 2010. http://www.awmf.org/leitlinien/detail/ll/043-044.html.
- 8.The Dutch College of General Practitioners. Urineweginfecties M05 2013. https://www.nhg.org/standaarden/samenvatting/urineweginfecties.
- 9.Christiaens TCM, De Meyere M, Verschraegen G, Peersman W, Heytens S, De Maeseneer JM. Randomised controlled trial of nitrofurantoin versus placebo in the treatment of uncomplicated urinary tract infection in adult women. Br J Gen Pract 2002;52: 729-34. 12236276 [PMC free article] [PubMed] [Google Scholar]
- 10.Bleidorn J, Gágyor I, Kochen MM, Wegscheider K, Hummers-Pradier E. Symptomatic treatment (ibuprofen) or antibiotics (ciprofloxacin) for uncomplicated urinary tract infection?--results of a randomized controlled pilot trial. BMC Med 2010;8: 30. 10.1186/1741-7015-8-30 20504298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Little P, Moore MV, Turner Set al. Effectiveness of five different approaches in management of urinary tract infection: randomised controlled trial. BMJ 2010;340: c199. 10.1136/bmj.c199 20139214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patrick DM, Hutchinson J. Antibiotic use and population ecology: how you can reduce your “resistance footprint”. CMAJ 2009;180: 416-21. 10.1503/cmaj.080626 19221355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Butler CC, Dunstan F, Heginbothom Met al. Containing antibiotic resistance: decreased antibiotic-resistant coliform urinary tract infections with reduction in antibiotic prescribing by general practices. Br J Gen Pract 2007;57: 785-92. 17925135 [PMC free article] [PubMed] [Google Scholar]
- 14.Gyssens IC. Antibiotic policy. Int J Antimicrob Agents 2011;38(Suppl): 11-20. 10.1016/j.ijantimicag.2011.09.002 22018989 [DOI] [PubMed] [Google Scholar]
- 15.Gottesman BS, Carmeli Y, Shitrit P, Chowers M. Impact of quinolone restriction on resistance patterns of Escherichia coli isolated from urine by culture in a community setting. Clin Infect Dis 2009;49: 869-75. 10.1086/605530 19686074 [DOI] [PubMed] [Google Scholar]
- 16.Ferry SA, Holm SE, Stenlund H, Lundholm R, Monsen TJ. The natural course of uncomplicated lower urinary tract infection in women illustrated by a randomized placebo controlled study. Scand J Infect Dis 2004;36: 296-301. 10.1080/00365540410019642 15198188 [DOI] [PubMed] [Google Scholar]
- 17.Knottnerus BJ, Geerlings SE, Moll van Charante EP, ter Riet G. Women with symptoms of uncomplicated urinary tract infection are often willing to delay antibiotic treatment: a prospective cohort study. BMC Fam Pract 2013;14: 71. 10.1186/1471-2296-14-71 23721260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leydon GM, Turner S, Smith H, Little PUTIS team. Women’s views about management and cause of urinary tract infection: qualitative interview study. BMJ 2010;340: c279. 10.1136/bmj.c279 20139217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Willems CS, van den Broek D’Obrenan J, Numans ME, Verheij TJ, van der Velden AW. Cystitis: antibiotic prescribing, consultation, attitudes and opinions. Fam Pract 2014;31: 149-55. 10.1093/fampra/cmt077 24317602 [DOI] [PubMed] [Google Scholar]
- 20.Gágyor I, Hummers-Pradier E, Kochen MM, Schmiemann G, Wegscheider K, Bleidorn J. Immediate versus conditional treatment of uncomplicated urinary tract infection - a randomized-controlled comparative effectiveness study in general practices. BMC Infect Dis 2012;12: 146. 10.1186/1471-2334-12-146 22742538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Loudon K, Treweek S, Sullivan F, Donnan P, Thorpe KE, Zwarenstein M. The PRECIS-2 tool: designing trials that are fit for purpose. BMJ 2015;350: h2147. 10.1136/bmj.h2147 25956159 [DOI] [PubMed] [Google Scholar]
- 22.Mauch H, Podbielski A, Herrmann M, Gatermann SG, Fünfstück R, Handrick W. Harnwegsinfektionen: Qualitätsstandards in der mikrobiologisch-infektiologischen Diagnostik. 2nd ed. Urban & Fischer Verlag/Elsevier GmbH 2005.
- 23.Cals JW, Butler CC, Hopstaken RM, Hood K, Dinant GJ. Effect of point of care testing for C reactive protein and training in communication skills on antibiotic use in lower respiratory tract infections: cluster randomised trial. BMJ 2009;338: b1374. 10.1136/bmj.b1374 19416992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Linde M, Mellberg A, Dahlöf C. The natural course of migraine attacks. A prospective analysis of untreated attacks compared with attacks treated with a triptan. Cephalalgia 2006;26: 712-21. 10.1111/j.1468-2982.2006.01097.x 16686911 [DOI] [PubMed] [Google Scholar]
- 25.Hanania NA, Boota A, Kerwin E, Tomlinson L, Denis-Mize K. Efficacy and safety of nebulized formoterol as add-on therapy in COPD patients receiving maintenance tiotropium bromide: Results from a 6-week, randomized, placebo-controlled, clinical trial. Drugs 2009;69: 1205-16. 10.2165/00003495-200969090-00005 19537837 [DOI] [PubMed] [Google Scholar]
- 26.Wild DJ, Clayson DJ, Keating K, Gondek K. Validation of a patient-administered questionnaire to measure the activity impairment experienced by women with uncomplicated urinary tract infection: the Activity Impairment Assessment (AIA). Health Qual Life Outcomes 2005;3: 42. 10.1186/1477-7525-3-42 16022727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Julious SA. Sample sizes for clinical trials with normal data. Stat Med 2004;23: 1921-86. 10.1002/sim.1783 15195324 [DOI] [PubMed] [Google Scholar]
- 28.Vik I, Bollestad M, Grude Net al. Ibuprofen versus mecillinam for uncomplicated cystitis--a randomized controlled trial study protocol. BMC Infect Dis 2014;14: 693. 10.1186/s12879-014-0693-y 25516016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Pinxteren B, Knottnerus BJ, Geerlings SEet al. NHG-Standaard Urineweginfecties (derde herziening). Huisarts Wet 2013;56: 270-80. [Google Scholar]
- 30.Falagas ME, Kotsantis IK, Vouloumanou EK, Rafailidis PI. Antibiotics versus placebo in the treatment of women with uncomplicated cystitis: a meta-analysis of randomized controlled trials. J Infect 2009;58: 91-102. 10.1016/j.jinf.2008.12.009. 19195714 [DOI] [PubMed] [Google Scholar]
- 31.Obad J, Šušković J, Kos B. Antimicrobial activity of ibuprofen: new perspectives on an “Old” non-antibiotic drug. Eur J Pharm Sci 2015;71: 93-8. 10.1016/j.ejps.2015.02.011 25708941 [DOI] [PubMed] [Google Scholar]
- 32.Cai T, Mazzoli S, Mondaini Net al. The role of asymptomatic bacteriuria in young women with recurrent urinary tract infections: to treat or not to treat?Clin Infect Dis 2012;55: 771-7. 10.1093/cid/cis534 22677710 [DOI] [PubMed] [Google Scholar]
- 33.Scottish Intercollegiate Guidelines Network. Management of suspected bacterial urinary tract infection in adults 2012. www.sign.ac.uk/pdf/sign88.pdf.
- 34.Giesen LG, Cousins G, Dimitrov BD, van de Laar FA, Fahey T. Predicting acute uncomplicated urinary tract infection in women: a systematic review of the diagnostic accuracy of symptoms and signs. BMC Fam Pract 2010;11: 78. 10.1186/1471-2296-11-78 20969801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baerheim A, Digranes A, Hunskaar S. Equal symptomatic outcome after antibacterial treatment of acute lower urinary tract infection and the acute urethral syndrome in adult women. Scand J Prim Health Care 1999;17: 170-3. 10.1080/028134399750002593 10555247 [DOI] [PubMed] [Google Scholar]
- 36.Bates J, Thomas-Jones E, Pickles Tet al. Point of care testing for urinary tract infection in primary care (POETIC): protocol for a randomised controlled trial of the clinical and cost effectiveness of FLEXICULT™ informed management of uncomplicated UTI in primary care. BMC Fam Pract 2014;15: 187. 10.1186/s12875-014-0187-4 25425162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Donovan JL, de Salis I, Toerien M, Paramasivan S, Hamdy FC, Blazeby JM. The intellectual challenges and emotional consequences of equipoise contributed to the fragility of recruitment in six randomized controlled trials. J Clin Epidemiol 2014;67: 912-20. 10.1016/j.jclinepi.2014.03.010 24811157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Little P, Stuart B, Hobbs FDet al. DESCARTE investigators. Antibiotic prescription strategies for acute sore throat: a prospective observational cohort study. Lancet Infect Dis 2014;14: 213-9. 10.1016/S1473-3099(13)70294-9 24440616 [DOI] [PubMed] [Google Scholar]