Abstract
Objectives
High turnover rates among nursing assistants (NAs) in nursing homes have costly implications for facility operation and quality, while low rates of NA profession retention can deplete the stock of experienced staff. This study assesses the extent to which the same factors are associated with NAs' intent to leave a particular job versus the NA profession.
Methods
We used data for 2,328 NAs from the 2004 National Nursing Assistant Survey to model: (a) two measures of facility retention (whether NAs expect to leave their current job within one year and whether they are also searching for a new job); and (b) NA profession retention, measured by whether NAs do not expect their next job to be as a nursing assistant.
Results
Substantially different factors affect facility versus profession retention. Facility characteristics (including supervisor qualities, training/safety and benefits) primarily affect facility retention while NA profession retention is negatively associated with income and education.
Discussion
Facilities can implement specific actions to retain NAs, though such policies may have limited effect on retention in the profession. Broader enhancements of career opportunities may be necessary for profession retention, though balance between retention and promotion may be important.
Keywords: Turnover, Intent to leave
Introduction
Despite the growth of long term care alternatives such as assisted living, nursing homes will continue to be an important source of health care and living arrangement for many of the nation's elderly. One challenge faced by nursing homes is the task of hiring and retaining nursing assistants (NAs). Although turnover may in some cases reflect elimination of poor performers, NA turnover often results in replacement costs, lost productivity, compromised quality, and lowered morale (2002). One study estimated that up to 80% of the cost to replace employees is spent for indirect or hidden costs that include departing and incoming employee inefficiency and the cost of the position while vacant (Phillips, 1990). Furthermore, NA turnover can compromise quality of care (Cohen-Mansfield, 1997), while poor quality of care can exacerbate turnover (Anderson et al., 2005). The American Association of Homes and Services for the Aging (2007) reports that the average annual national turnover rate for NAs is 71% and that NA turnover costs more than $4 billion per year. An assessment of long-term care workforce issues (Institute for the Future of Aging Services, 2007) cited current vacancy rates of 12% for nursing assistants in nursing homes and predicted substantial future increases in shortages given aging of the population.
Facility and profession turnover may happen for a variety of reasons, both random and purposeful. The NA profession is characterized by relatively poor wages and benefits, and the nature of work is both physically and emotionally demanding. These factors cause recruitment and retention problems which manifest themselves in high turnover rates (Reinhard & Stone, 2001). Studies have shown that in addition to compensation and benefits, nursing assistants are highly concerned with job security, interactive aspects of their jobs, involvement in care planning and work-related decisions, and professional growth potential (Atchison, 1998; Bowers, Esmond, & Jacobson, 2003; Parsons, Simmons, Penn, & Furlough, 2003). Leaving a job or the NA profession generally requires an alternative employment option for the worker, and measures such as intent to leave are not always predictive of actual departures from a facility. Some studies have focused on factors associated with job satisfaction or organizational commitment, defined as the relative strength of an individual's linkage to the employing organization. In an extensive review of the literature, Wagner (2007) identified intent to leave as an important antecedent of turnover as well as an important mediating variable in modeling the effect of organizational commitment on turnover.
Although many assessments of job satisfaction or turnover use only facility-level data or involve small samples of individuals from a limited number of facilities or states, recent work has expanded our understanding of factors associated with facility turnover. Castle (2005) found that a 10% increase in turnover among top management is correlated with a 21% increase in the odds that a facility will have high NA turnover. Kash and colleagues (2006) concluded that NA turnover is reduced by higher administrative expenditures and higher NA wages. Castle and Engberg (2006) found that lower staffing levels, lower quality, for-profit ownership, and higher bed size were associated with higher NA turnover. Donoghue and Castle (2006) found that factors such as nurse to bed ratio, quality of care deficiencies, and case mix predict voluntary and involuntary turnover differently. Using surveys of nursing aides at facilities in five states, Castle and colleagues (2007) hypothesized that job satisfaction is an important antecedent of both intent to leave and turnover; their study also showed that training, benefits, and work schedule were predictive of intent to leave, and that, in addition to these factors, facility quality of care and workplace support were predictive of turnover.
While factors associated with facility NA turnover have been studied, the literature investigating the reasons why NAs leave their profession is sparse. Stone and Weiner (2001) concluded that, in addition to facility-specific experiences, other factors as varied as societal perceptions of the occupation, local economic conditions, and public policies affect the choice to remain in the profession. Hiring a NA without prior experience is likely to be more costly in terms of initial training required than hiring an experienced NA. If the quality of care provided by experienced NAs is higher than the quality provided by novice NAs, then patient outcomes may be improved through increased professional retention. More generally, NAs who plan to leave the field in the future may be less committed to their work than those whose long-term career plans revolve around continuing to being a NA. As with facility turnover, small rates of departure from the NA profession may be efficient, and some progression to higher positions in long term care may be desirable. Yet high levels of departure from the NA profession detract from the possibility of accruing a competent and experienced employee pool.
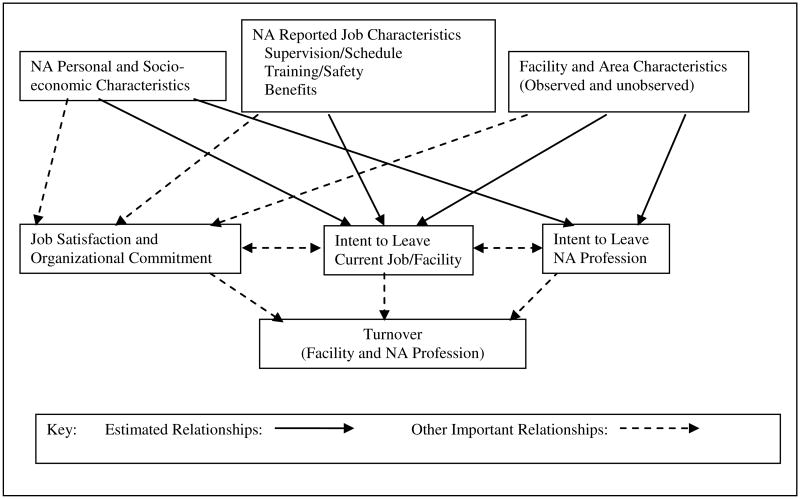
This analysis uses data from the 2004 National Nursing Assistant Survey (NNAS) to investigate NA retention in their current job as well as the profession as measured by intent to leave. Figure 1 summarizes the conceptual model for this study, which is closely aligned with the model used by Castle and colleagues (2007) except that we view job satisfaction and organizational commitment as being jointly determined with intent to leave. This distinction is important since Castle and colleagues specified job satisfaction as an antecedent to intent to leave but did not find intent to leave to be separately predictive of actual turnover once job satisfaction was controlled. Identification of the separate effects of job satisfaction and intent to leave is simply not possible with cross-sectional surveys of nursing assistants. The goal of this study is to determine whether the factors that predict NAs' intent to leave their current job at a facility also predict their intent to leave the NA profession. We hypothesize that factors unique to a facility (e.g., supervisor/scheduling) will predict intent to leave the current job/facility, while factors related to both the current job and other jobs (e.g., the NA's initial training or socio-economic characteristics) will predict intent to leave the profession.
Figure 1. Conceptual Model of Facility and NA Profession Turnover.
The model estimates the effects of NA-reported perceptions of key facility attributes known to be related to turnover, NA personal characteristics, and other observed and unobserved characteristics of the facilities. The cross-sectional nature of the survey used for this study precludes determination of the effect of intent to leave on actual turnover, and only the relationships depicted by the solid lines in Figure 1 are estimated. The analyses show that substantially different factors affect NAs' intent to leave their current jobs versus the NA profession. The findings imply that different strategies or policies may be required for improving the two different types of retention.
Methods
Data and Empirical Approach
The NNAS was designed to provide, among other things, information on factors that contribute to NAs' job satisfaction and likelihood of staying in their jobs. (Squillace, Remsburg, Bercovitz, Rosenoff, & Branden, 2006). From the original 2004 National Nursing Home Survey (NNHS) sample of 1500 facilities, 790 nursing homes were selected to participate in the NNAS. Seventy-six percent (582 homes) provided contact information for nursing assistants working directly for the facilities. The NNAS excluded nursing assistants not already certified or in training for certification unless they were trained prior to 1987, contract nursing assistants, and assistants working fewer than 16 hours per week. A total of 3,017 (71%) of 4,542 eligible nursing assistants completed an interview, resulting in a combined facility and person response rate of 53%. The survey was administered when NAs were not at work to minimize fears of job loss or other negative reprisals given the potentially sensitive nature of the work-related questions.
The NNAS is the first national survey gathering NA data at the individual level. Person level data allow for more information and precision than facility observations when analyzing factors that affect facility or NA profession retention, and the availability of multiple respondents per facility strengthens the ability to identify individual and facility factors associated with retention. The model is:
where the subscript i represents the individual NA respondent and h represents the nursing home. The model uses three dichotomous self-reported measures of intent to leave yih. Two measures reflecting intent to leave the facility are: (1) a broad measure of whether the respondent is very or somewhat likely to leave their current job in the next year; and (2) a stronger measure of whether the respondent is actively searching for a job in addition to being very or somewhat likely to leave their current job within one year. Although some NAs may seek promotion to a different job within the same facility, we expect that most workers who expect to leave their current job also expect to leave their current facility. The second measure represents a stronger stage of intent to leave and is likely to be more highly correlated with subsequent departures from the facility. Intent to leave the NA profession is measured by whether the NA does not think his/her next job will be as a nursing assistant but instead will be as something else. We interpret this variable as referring only to being a NA in a nursing home since that is the surveyed population; an individual may still intend to remain in the field of long-term care. The error term consists of one component, μh, which only varies between facilities, and another component, εih, which varies across facilities and individual respondents.
Following prior studies of turnover (Castle et al., 2007; Price, 2001), the three vectors of explanatory variables include characteristics related to the working environment and facility reported by the NA, NA personal characteristics, and other facility characteristics. Personal characteristics include gender, race, Hispanic ethnicity, age, marital status, having at least one child in the household, citizenship status, whether the NA works at the facility full-time, the commute time in minutes (for the facility intent to leave models only), and income and education. The remaining factors consist of characteristics of the work setting as well as area characteristics that are external to both the individual and the organization. For this study, characteristics of the work setting have two important dimensions: whether they are observed or not observed, and whether the observed factors are constant (or are reported as constant) within a facility for all NAs.
Three categories of measures that have been identified as important in prior studies and are reported by NAs in the NNAS include supervision quality/scheduling, training/safety, and benefits (Castle et al., 2007). All of these measures have at least some variation across NAs within facilities. While some within-facility variation may be due to erroneous knowledge on the part of the NA (e.g., whether the facility has lifting devices available) or employment status (e.g., health insurance may not be available to part-time workers), the worker's perceptions of these measures or choices available to them are potentially important in modeling intent to leave the facility or profession.
We used three measures of supervision quality/scheduling. The NNAS has a series of ten questions assessing the quality of the supervisor (whether the supervisor provides clear instructions, treats all NAs equally, deals with NA complaints and concerns, is open to new ideas, is supportive of progress in the NA's career, helps NAs with tasks when needed, listens when the NA is worried about resident's care, supports NAs working in teams, disciplines NAs not performing well, and tells the NA when doing a good job); we constructed an index as a count of the number of times the NA strongly agreed with these statements. We also included a measure of whether the NAs feel they are respected a great deal by their supervisors and a scheduling measure of whether they have enough or more than enough time for all of their duties. While overall training has been shown to be important (Iowa CareGivers Association, 2000), training related to preventing injuries may be particularly relevant. NAs have among the highest back and shoulder injury rates in the United States (Myers, Silverstein, & Nelson, 2002), and nursing homes can provide training or assistive devices to reduce the injury rates (Garg, 1999). We therefore included the following five measures related to the NA's training/safety experience: whether the NA felt their initial training (which may or may not have occurred at the facility) prepared them well for working in a nursing home; whether the NA perceived their initial training as excellent or good in preventing work injuries; whether the NA had a lot of say in topics covered in classes paid for or offered by the current employer; whether the facility always has lifting devices available; and whether the NA had at least one work-related injury in the past. Measures of benefits provided by the facility include: the hourly pay rate; whether the NA gets paid time off for holidays, vacation/personal days, or sick days; and whether health insurance is offered.
In addition to the NA-reported measures, the existing literature shows that a number of additional facility characteristics (e.g., other aspects of management/administration and work environment, case mix, quality of care staffing turnover, occupancy rate, organizational policies, growth opportunities, reputation, etc.) and area characteristics (e.g., unemployment, wages/benefits in the market, etc.) are important determinants of facility turnover (Banaszak-Holl & Hines, 1996; Castle & Engberg, 2006; Castle et al., 2007; Charlene Harrington & Swan, 2003). Public use versions of the NNHS and NNAS cannot be merged due to confidentiality concerns, however, and only three facility variables (ownership, bed size, and urban/rural location) from the NNHS are included in the public use versions of the NNAS. We test facility fixed effects models to account for all facility characteristics (observed or unobserved) that do not vary across observations for all NAs at each facility, thereby providing strong protection against omitted facility variable bias.
In the fixed effects models, the estimated coefficients for the NA-reported measures reflect variation in intent to leave in relation to within-facility variation in a variable. For example, the facility fixed effects control for the cost of labor in each facility's market area and any between-facility variation in wages, while the coefficient for the wage rate reported by the NA captures the effect of any within-facility variation in wages on the likelihood of retention. While the limited number of NA respondents per facility means that the facility coefficients would not necessarily be representative of the specific facility relationship with the dependent variable in a population sense, the availability of within-facility variation in the measures enables estimation of the NA-reported variables in the model as well as the determination of the role of facility characteristics as a whole. However, the limited number of NA observations may preclude precise estimation of the effect of some of these variables separately from the facility fixed effects.
Although a logit model could be used, estimation of facility fixed effects using a logit model is problematic due to lack of variation in the intent to leave variables among NAs at some facilities. We therefore estimate linear probability models (LPM) using ordinary least squares and linear facility fixed effects models (FE) to determine the importance of controlling for unobserved facility characteristics. We deal with missing data by using complete case analysis of observations with valid responses for all model variables. We estimate preliminary versions (logit models without fixed effects, and subgroup analysis using full-time workers only or only workers who expect to stay in the profession) to test the robustness of the models. Final models are estimated using survey weights and robust standard errors.
Results
Analysis Sample and Descriptive Statistics
One hundred twenty NNAS respondents left their facilities before the survey was administered and were given a different survey that did not include many of the measures used in this analysis. The main reasons for further exclusions were missing responses on paid sick days (8.6%) and injury (6.7%). After exclusions for missing data, the final analysis sample consists of 2,328 nursing assistants at 577 nursing homes. The number of NAs at each facility ranged from one to eight; the analysis sample had an average of four NAs per facility, and 32 facilities had only one NA respondent.
Table 1 includes population-weighted statistics for 120 respondents who quit prior to the full survey, the 2,897 respondents still employed by the facilities at the time of the survey, and the 2,328 respondents in the complete case analysis sample. Compared to the 2,897 stayers, the 120 leavers tended to be younger, have lower income and wages, and were more likely to have worked at a for-profit facility. The ability to control for these factors helps to ensure that response bias does not affect our estimates, though concern about any unobserved differences between our analysis sample and the full population of NAs remains. The descriptive statistics are very similar for the stayers and the NA analysis sample, and they reflect usual characteristics for NAs (e.g., primarily female, under age 45, household income under $30,000, and the majority having a high school education but no further degree).
Table 1. Descriptive Population (Weighted) Statistics for Original and Analysis Samples.
| NAs who left prior to survey | All stayers responding to NNAS | Sample used in analysis | |
|---|---|---|---|
|
|
|||
| Observations | 120 | 2,897 | 2,328 |
| Intent to Leave Measures | |||
| NA is very or somewhat likely to leave current job in the next year (broad intent to leave facility) | 0.45 | 0.43 | |
| NA is very or somewhat likely to leave current job in the next year and is currently looking for a job (strong intent to leave facility) | 0.20 | 0.20 | |
| NA does not expect his/her next job to be as a nursing assistant | 0.47 | 0.48 | |
| Main Reasons for Intent to Leave Facility (NAs very or somewhat likely to leave current job) | |||
| Poor pay | 0.37 | 0.38 | |
| Found a new or better job | 0.27 | 0.27 | |
| Problems with working conditions/policies | 0.16 | 0.16 | |
| Too many residents to care for | 0.13 | 0.12 | |
| Poor benefits | 0.11 | 0.11 | |
| Problems with supervisor | 0.11 | 0.11 | |
| NA Reported Supervisor/Scheduling | |||
| Index of positive supervisor qualities (Range: 1-10) | 5.28 | 5.30 | |
| NA is respected a great deal by their supervisor | 0.58 | 0.58 | |
| NA has enough or more than enough time for duties | 0.45 | 0.44 | |
| NA Reported Facility Training/Safety | |||
| Initial training prepared NA well for working in a nursing home | 0.66 | 0.66 | |
| Initial training excellent or good in preventing work injuries | 0.90 | 0.90 | |
| NA has a lot of say in topics covered in classes facility pays for§ | 0.23 | 0.25 | |
| Lifting devices always available | 0.88 | 0.87 | |
| One or more work-related injuries in the past year | 0.58 | 0.60 | |
| NA Reported Facility Benefits | |||
| Hourly wageˆ | 9.46* | 10.34 | 10.36 |
| Paid time off for holidays | 0.74 | 0.74 | |
| Paid time off for vacation/personal days | 0.86 | 0.86 | |
| Paid time off for sick days | 0.73 | 0.74 | |
| Health insurance available at job§ | 0.91 | 0.91 | |
| Personal Characteristics | |||
| Male | 0.18 | 0.08 | 0.08 |
| Not white | 0.41 | 0.47 | 0.46 |
| Hispanic | 0.05 | 0.10 | 0.10 |
| Age | |||
| Age 18-30 | 0.48* | 0.31 | 0.31 |
| Age 31-35 | 0.39 | 0.37 | 0.37 |
| Age 46-60 | 0.11* | 0.26 | 0.27 |
| Age 61+ | 0.02 | 0.06 | 0.05 |
| Marital Status | |||
| Married | 0.43 | 0.51 | 0.52 |
| Widowed | 0.03 | 0.04 | 0.04 |
| Separated, divorced, never married | 0.54 | 0.44 | 0.44 |
| 1+ children in household | 0.59 | 0.59 | |
| Citizen | 0.91 | 0.92 | |
| Full-time | 0.66 | 0.73 | 0.74 |
| Commute in minutes (Range: 1-150 minutes) | 19.86 | 19.75 | |
| Income | |||
| Household income less than $10,000 | 0.23* | 0.10 | 0.09 |
| Household income $10,000 - less than $30,000 | 0.57 | 0.56 | 0.56 |
| Household income $30,000 - less than $50,000 | 0.16 | 0.24 | 0.24 |
| Household income $50,000+ | 0.05 | 0.10 | 0.10 |
| Education | |||
| Less than high school | 0.16 | 0.13 | 0.13 |
| GED or high school diploma | 0.62 | 0.62 | 0.62 |
| Some college or more | 0.22 | 0.25 | 0.24 |
| Other Facility Characteristics | |||
| For-profit | 0.68* | 0.59 | 0.57 |
| Bed size | |||
| 3-49 beds | 0.07 | 0.05 | 0.05 |
| 50-99 beds | 0.27 | 0.28 | 0.28 |
| 100-199 beds | 0.57 | 0.56 | 0.55 |
| 200+ beds | 0.10 | 0.11 | 0.12 |
| Geographic region | |||
| Metropolitan area | 0.72 | 0.76 | 0.75 |
| Micropolitan area | 0.19 | 0.13 | 0.13 |
| Rural | 0.09 | 0.11 | 0.11 |
Notes:
p<.05 for statistical tests of leavers versus stayers.
Missing values coded as a negative response.
Values truncated at 99th percentile for stayers ($15.75) to reduce effect of high outliers.
Data for 120 NAs who left their facilities between the time they were identified as eligible for the NNAS and when the survey was administered could not be used because they responded to a different survey. All variables are dichotomous except for the hourly wage and commute time.
All NA-reported variables had at least a moderate level of within-facility variation. The supervisor and scheduling variables show substantial variation, with NAs not feeling satisfied with supervision, respected or having enough time for their jobs in many cases. Initial training as well as training to prevent work injuries is usually perceived as good, and most facilities provide lifting devices, yet injury rates are high. Most facilities offer paid time off work for various reasons. A surprisingly high proportion (91%) of respondents said that health insurance was available through their employer; data from the NNHS show that only 12% of facilities offer fully paid insurance to NAs but an additional 69% offer partially paid policies, so the take-up rate of insurance may be considerably lower.
Weighted statistics for the retention measures in the analysis sample show that 43% of respondents said it was very or somewhat likely that they would not be in their current job one year later, while 20% said that they were very or somewhat likely not to be in their current job one year later and that they were actively looking for a job. Nearly half (48%) did not expect their next job to be as a nursing assistant. Even though intent to leave may not always result in turnover, these statistics are consistent with the high documented rates of turnover in the industry. The NNAS asks respondents who are very or somewhat likely to leave their reasons for leaving; the six most important reasons indicated by these 1,062 respondents (shown in Table 1) were poor pay, already having a new or better job, problems with working conditions/policies, too many residents to care for, poor benefits, or problems with supervisor. The ranking of reasons was similar regardless of whether the person also planned to leave the profession.
Surprisingly little correlation exists between the measures of intent to leave the facility and the NA profession, as shown by the distribution of observations in Table 2. Although a chi-square test shows the broad intent to leave facility measure and intent to leave the profession are correlated (p=0.026), roughly 56% (555/1068 or 713/1260) expect their next job to be as a NA regardless of whether the NA expects to leave the current job. Regardless of whether the respondent expects their next job to be as a NA, roughly 48% (513/1060) or 43% (555/1268) are very or somewhat likely to leave their current job in the next year. The similarities in these distributions suggest that very different processes may be driving these decisions.
Table 2. Relationship Between Intent to Leave Facility and Intent to Leave Profession.
| NA does not expect his/her next job to be as a nursing assistant | |||
|---|---|---|---|
| NA is very or somewhat likely to leave their current job in the next year | Yes | No | Total |
| Yes | 513 | 555 | 1,068 |
| No | 547 | 713 | 1,260 |
| Total | 1,060 | 1,268 | 2,328 |
| p=0.026 for a chi-square test of association between the two measures. | |||
| NA does not expect his/her next job to be as a nursing assistant | |||
| NA is very or somewhat likely to leave their current job in the next year and is currently looking for a job | Yes | No | Total |
| Yes | 229 | 282 | 511 |
| No | 831 | 986 | 1,817 |
| Total | 1,060 | 1,268 | 2,328 |
p=0.712 for a chi-square test of association between the two measures.
We used F-tests and Hausman tests to compare the LPM and FE models (Wooldridge, 2006). Based on F-tests, Table 3 shows that facility fixed effects are important in explaining variation in the likelihood that a NA is very or somewhat likely to leave their current job within one year after the interview but are not supported (p=0.11) for the model whether a NA does not expect to remain in the NA profession. The Hausman test supports the use of fixed effects for the strong facility retention measure (p=0.054) but does not support fixed effects for the profession retention measure (p=0.32). One reason why the statistical support for the fixed effects is not strong in all models may be the fact that the number of NA respondents per facility is limited, and a large number of degrees of freedom is used up in the FE models. Comparison of estimated coefficients between the FE and LPM models showed that coefficients were virtually identical in sign and significance, with only modest changes in magnitude. Therefore, we use the fixed effects models for the two measures of intent to leave the facility (with the statistical evidence most strongly in favor of the fixed effects for the dependent variable indicating an active job search as well as intent to leave) but use the LPM for the analysis of the intent to leave the NA profession.
Table 3. Results from Tests for Estimation Model Selection.
| Intent to Leave Facility | Intent to Leave Facility and Looking for Job | Intent to Leave Profession | |
|---|---|---|---|
| Dependent Variable | NA is very or somewhat likely to leave their current job in the next year | NA is very or somewhat likely to leave their current job in the next year and is currently looking for a job | NA does not expect his/her next job to be as a nursing assistant |
| F-test of facility fixed effects in LPM§ | F(576, 1721) = 1.12 Prob > F = 0.0440 | F(576, 1721) = 1.15 Prob > F = 0.0169 | F(576, 1722) = 1.08 Prob > F = 0.1144 |
| Hausman test of FE versus LPM (preferred model from Breusch-Pagan test)§ | chi2(30) = 39.16 Prob>chi2 = 0.1221 | chi2(30) = 43.43 Prob>chi2 = 0.0537 | chi2(29) = 32.03 Prob>chi2 = 0.3185 |
Tests were conducted in unweighted models without robust standard errors. See Wooldridge (2006) for a description of all statistical tests.
Model Results
Table 4 shows results for the preferred models for all retention measures. The most important point is that differences exist in which variables significantly predict facility retention versus NA profession retention.
Table 4. Estimation Results for Models of Facility and Profession Intent to Leave (n=2,328).
| Intent to Leave Facility | Intent to Leave Facility and Looking for Job | Intent to Leave NA Profession | |
|---|---|---|---|
| NA-Reported Supervisor/Scheduling | |||
| Index of positive supervisor qualities | -0.020 [0.006]** | -0.016 [0.004]** | -0.007 [0.005] |
| NA is respected a great deal by their supervisor | -0.070 [0.034]* | -0.067 [0.029]* | -0.044 [0.034] |
| NA has enough or more than enough time for duties | -0.012 [0.028] | 0.032 [0.023] | -0.055 [0.028] |
| NA-Reported Facility Training/Safety | |||
| Initial training prepared NA well for working in a nursing home | 0.018 [0.029] | 0.023 [0.025] | -0.057 [0.030] |
| Initial training excellent or good in preventing work injuries | -0.038 [0.041] | -0.031 [0.033] | 0.045 [0.045] |
| NA has a lot of say in topics in classes paid by facility | -0.067 [0.032]* | -0.009 [0.026] | 0.039 [0.032] |
| Lifting devices always available | -0.139 [0.040]** | -0.127 [0.039]** | -0.020 [0.041] |
| One or more work-related injuries in the past year | 0.046 [0.028] | 0.040 [0.023] | 0.037 [0.028] |
| NA-Reported Facility Benefits | |||
| Hourly wage | -0.041 [0.010]** | -0.027 [0.010]** | 0.001 [0.007] |
| Paid time off for holidays | -0.037 [0.036] | -0.016 [0.032] | -0.019 [0.033] |
| Paid time off for vacation/personal days | -0.113 [0.038]** | -0.084 [0.032]** | -0.022 [0.038] |
| Paid time off for sick days | -0.070 [0.039] | -0.032 [0.033] | 0.021 [0.033] |
| Health insurance available at job | 0.005 [0.054] | -0.039 [0.045] | -0.017 [0.045] |
| Personal Characteristics | |||
| Male | -0.039 [0.046] | 0.007 [0.041] | -0.029 [0.052] |
| Not white | 0.053 [0.040] | -0.008 [0.033] | 0.118 [0.030]** |
| Hispanic | -0.051 [0.051] | -0.127 [0.046]** | -0.080 [0.041] |
| Age (reference category: age 61+) | |||
| Age 18-30 | 0.073 [0.066] | 0.151 [0.047]** | -0.061 [0.070] |
| Age 31-35 | -0.009 [0.063] | 0.122 [0.044]** | -0.095 [0.069] |
| Age 46-60 | -0.130 [0.063]* | 0.084 [0.043]* | -0.163 [0.069]* |
| Marital Status (reference category: married) | |||
| Widowed | 0.179 [0.073]* | 0.026 [0.055] | 0.027 [0.081] |
| Separated, divorced, never married | -0.011 [0.029] | 0.014 [0.025] | 0.005 [0.029] |
| 1+ children in household | -0.047 [0.030] | -0.018 [0.024] | -0.003 [0.029] |
| Citizen | -0.058 [0.063] | 0.069 [0.053] | 0.039 [0.055] |
| Full-time | -0.063 [0.032]* | -0.028 [0.028] | -0.016 [0.031] |
| Commute in minutes | 0.001 [0.001] | 0.001 [0.001] | |
| Income (reference category: $50,000+) | |||
| Household income less than $10,000 | 0.008 [0.066] | -0.020 [0.056] | -0.155 [0.062]* |
| Household income $10,000 - less than $30,000 | -0.011 [0.048] | -0.028 [0.041] | -0.127 [0.049]** |
| Household income $30,000 - less than $50,000 | -0.009 [0.048] | -0.014 [0.041] | -0.143 [0.051]** |
| Education (reference category: less than high school) | |||
| GED or high school diploma | 0.068 [0.039] | 0.029 [0.035] | 0.137 [0.038]** |
| Some college or more | 0.135 [0.047]** | 0.079 [0.041] | 0.237 [0.044]** |
| Other Facility Characteristics | |||
| Facility fixed effects? | Yes | Yes | No |
| For-profit | -0.102 [0.028]** | ||
| Bed size (reference category: 200+ beds) | |||
| 3-49 beds | -0.037 [0.060] | ||
| 50-99 beds | -0.082 [0.054] | ||
| 100-199 beds | -0.062 [0.052] | ||
| Geographic region (reference area: rural) | |||
| Metropolitan area | 0.056 [0.034] | ||
| Micropolitan area | 0.050 [0.037] | ||
| R2 | 0.47 | 0.42 | 0.09 |
Robust standard errors in brackets.
significant at 1%,
significant at 5%
For the facility retention measures, at least some of the NA-reported measures are statistically significant. Having a supervisor with positive qualities, respect from their supervisor, a lot of say in class topics, lifting devices available, higher wages, and paid vacation/personal days are all negatively associated with the broad intent to leave facility measure; all these factors except having a lot of say in class topics are also negatively associated with the strong intent to leave facility measure. Some of these effects are large, both in absolute magnitude and relative to the average likelihood of expecting to remain at the facility for at least one year of 57%; for example, having lifting devices always available reduces the likelihood of intent to leave the current facility job by 13 to 14 percentage points. In contrast, none of the NA-reported variables are statistically significant in the intent to leave NA profession model. Some of the lack of statistical significance may be due to limited within-facility variation in these measures. For example, whether the NA reports having enough time for their duties or whether they feel their initial training prepared them well to work in a nursing home are negatively associated with intent to leave the profession at p<0.06. Similarly, having work-related injuries in the past year is suggestive of greater intent to leave the current job (e.g., facility) but not at conventional levels of statistical significance. Other considerations may also apply; for example, the lack of statistical significance for the effect of health insurance availability may be due to the inability to control for the comprehensiveness or price of the health insurance offering.
A few of the personal characteristics are significantly related to the two measures of intent to leave the facility. For example, younger respondents are more likely to be actively searching for a job in addition to reporting an intention to leave their current job, while Hispanics are less likely to be actively searching for a job and non-whites are more likely to intend to leave the profession. Having more education is positively associated with a greater intent to leave the facility (broad measure) and profession; the effects are especially strong for the intent to leave the profession. Having income greater than $50,000 is strongly associated with intent to leave the profession but not with either of the measures of intent to leave a particular job/facility.
The results from the specification tests show that many facility characteristics (observed and unobserved) are significantly associated with intent to leave a particular facility, as evidenced by the substantially higher R-squared values relative to the LPM model (results not shown). For the LPM model for intent to leave the NA profession, only for-profit status was significantly and negatively associated with intent to leave.
Our robustness checks showed that (a) logit without fixed effects versus LPM models and (b) models with full time workers only had results that were extremely similar to results in Table 4 in terms of magnitude, sign and significance of coefficients. Estimations using only workers who expected to stay in the profession had results that were similar in magnitude to the results in Table 4, though modest shifts in magnitude and significance occurred, possibly because of the substantially reduced sample size.
Discussion
The key finding from this analysis, which contributes to the literature substantially by studying factors associated with NA profession retention, is that the factors determining facility and profession retention are very different. Facility retention is affected by a number of NA-reported facility characteristics (supervision/scheduling, training/safety, and benefits); in contrast, only NA reports of poor scheduling and initial training are borderline indicative of intent to leave the NA profession. Higher education leads to greater likelihood of intent to leave facility and profession. Higher income, being of white race, and of age 46-60 (relative to being over age 60) all reduce the likelihood of intending to leave the NA profession. Facility and area characteristics (observed and unobserved) have strong effects on the likelihood of intending to stay in a current job.
The different relationships detected by the analysis are quite plausible. The index of supervisor qualities may represent the degree to which the NA feels that facility administration respects the nursing assistants' opinions, directly affecting the propensity to stay at a particular job or facility. Conversely, such a measure would not necessarily affect a decision to continue seeking employment as a NA in the future. The same logic holds for availability of lifting devices; the lack of statistical significance in the profession regression suggests that the NAs perceive that lifting device availability is a feature of an individual nursing home and not the profession itself. It is possible, of course, that lift availability may serve as a general proxy for other important aspects of facility quality. It was surprising that the scheduling measure of whether the NA had enough time to complete task was not significant in the facility intent to leave regressions and only of borderline significance in the intent to leave the NA profession model since resident-to-staff ratios are cited as low in many facilities (Harrington, 2005). These factors contrast with the educational status and household income of NAs, which may reflect the degree of opportunities to seek employment in alternative facilities or professions. The fact that benefit measures were not significant in explaining profession retention may be due to the fact that job benefits for NAs were not modeled in relation to other alternative occupations.
The results presented in this paper are subject to some limitations. First, missing data may lead to biased coefficient estimates. Some NAs (120) are not included because they left their facility before responding to the survey, and data for NAs from only 577 of the original target sample of 790 nursing homes were available for the analysis. It is not possible to adjust for these omissions, which when combined with additional deletions due to missing responses result in an effective response rate of less than 50 percent. Still, the NNAS represents the first nationally representative survey for assessing intent to leave either the current job or the NA profession. Controlling for a number of observed measures and using weights in the analysis may help counter any bias from the low response rates. While the availability of only a few facility measures (ownership, size, and location) on the NNAS might seem to be a limitation, the ability to use facility fixed effects provides for strong control for all facility-specific factors.
In total, the results are interesting and potentially important for policy. In light of continued growth in the elderly population in the United States, establishing and maintaining a well-qualified NA workforce may be even more important in the future than it is today. A recent report considers a range of problems pertaining to the long-term care workforce and provides an excellent summary of the situation:
“The dilemmas peculiar to the recruitment and retention of the paraprofessional workforce are perhaps the most complex and difficult to resolve. Wages are not adequate to support young families with children. The job is often not well-designed, creating inefficiencies, unnecessary job burdens and subjecting occupants to high rates of injury. There are few opportunities for career advancement. Supervision is poor or non-existent. In addition, low unemployment rates for all entry-level personnel, coupled with increasing levels of education among minority populations, provide this labor pool with far more choices than low-income women have had in the past.” (Institute for the Future of Aging Services, 2007)
Our study results reinforce these points, ranging from the effects of supervision quality on to intent to leave the current job/facility to the relationships between education and income to the intent to leave the NA profession. As new policies are promulgated, it is important to know that facilities may undertake specific actions to reduce their own turnover, but more problematic to know that facility-specific policies have relatively little bearing on decisions to remain in the NA profession. The same report (Institute for the Future of Aging Services, 2007) identifies five goals to address the problems cited above: “(1) expand the supply of personnel coming into the long-term care field; (2) create more competitive long-term care jobs through wage and benefit increases; (3) improve working conditions and the quality of longer-term care jobs; (4) make larger and smarter investments in the development and continuing education of the long-term care workforce; and (5) moderate the demand for long-term care personnel.” The results from this study do not address the first or fifth goal, except to note that it does not make sense to increase the supply of people coming into the field unless rates of NA profession retention can be increased. Yet the results do reinforce the importance of the second, third, and fourth recommendations, which are accompanied by proposals of specific initiatives many of which are relevant for the NA workforce.
For example, initiatives such as “Better Jobs, Better Care” (www.bjbc.org) that seek to achieve changes in long-term care policy and practice to reduce high vacancy and turnover rates represent a major step toward this goal. Actions such as empowering NAs regarding input to their training needs and safety protections can be beneficial in reducing intent to leave or turnover and subsequently improving quality of care. The significance of the facility fixed effects most likely indicates the importance of factors such as good facility management in improving facility retention of NAs. Yet the findings regarding income and education mean that financial compensation and benefits for NAs must be competitive relative to other occupations to improve not only facility retention but also profession retention. For profession retention, balance between retention and promotion along a more encompassing career ladder is undoubtedly important.
The NNAS is a very rich source of other information not analyzed in this study, including what the respondent was doing prior to becoming a NA, whether they would become a NA again now that they have experience with the job, and information on prior jobs. More detailed assessments could be made of the relation between other measures and intent to leave the current job. Yet the fact that almost half of the respondents do not expect their next job to be as a NA raises questions pertaining to what the respondents expect to do next that can not easily be answered with the NNAS. For example, do respondents plan to take time to raise a family, return to school, seek training for an alternative occupation within health care or long-term care such as becoming a licensed nurse, or seeke alternative occupations outside of health care or long-term care? Answers to these questions, which may require panels of people working in other low-wage industries as well as long-term care, are important in order to stem departures from the NA profession and to develop efficient career trajectories for nursing assistants in nursing homes.
References
- American Association of Homes and Services for the Aging. Aging Services: The Facts. 2007 Retrieved April 21, 2007, from http://www.aahsa.org/aging_services/default.asp.
- Anderson RA, Ammarell N, Bailey D, Colon-Emeric C, Corazzini KN, Lillie M, et al. Nurse assistant mental models, sensemaking, care actions, and consequences for nursing home residents. Qualitative Health Research. 2005;15(8):1006–1021. doi: 10.1177/1049732305280773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atchison JH. Perceived job satisfaction factors of nursing assistants employed in Midwest nursing homes. Geriatric Nursing. 1998;19:135–138. doi: 10.1016/s0197-4572(98)90057-x. [DOI] [PubMed] [Google Scholar]
- Banaszak-Holl J, Hines MA. Factors associated with nursing home staff turnover. The Gerontologist. 1996;36:512–517. doi: 10.1093/geront/36.4.512. [DOI] [PubMed] [Google Scholar]
- Bowers B, Esmond S, Jacobson N. Turnover Reinterpreted: CNAs Talk About Why They Leave. Journal of Gerontological Nursing. 2003;29(3):36–43. doi: 10.3928/0098-9134-20030301-09. [DOI] [PubMed] [Google Scholar]
- Brannon D, Zinn JS, Mor V, Davis J. An exploration of job, organizational, and environmental factors associated with high and low nursing assistant turnover. The Gerontologist. 2002;42(2):159–168. doi: 10.1093/geront/42.2.159. [DOI] [PubMed] [Google Scholar]
- Castle NG. Turnover begets turnover. The Gerontologist. 2005;45(2):186–195. doi: 10.1093/geront/45.2.186. [DOI] [PubMed] [Google Scholar]
- Castle NG, Engberg J. Organizational characteristics associated with staff turnover in nursing homes. The Gerontologist. 2006;46(1):62–73. doi: 10.1093/geront/46.1.62. [DOI] [PubMed] [Google Scholar]
- Castle NG, Engberg J, Anderson R, Men A. Job satisfaction of nurse aides in nursing homes: Intent to leave and turnover. Gerontologist. 2007;47(2):193–204. doi: 10.1093/geront/47.2.193. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J. Turnover Among Nursing Home Staff. Nursing Management. 1997;28:59–64. [PubMed] [Google Scholar]
- Donoghue C, Castle NG. Voluntary and involuntary nursing home staff turnover. Research on Aging. 2006;28:454–472. [Google Scholar]
- Garg A. Long-term effectiveness of “Zero-Lift Program” in seven nursing homes and one hospita. 1999 Retrieved April 24, 2007. from http://www.aft.org/topics/no-lift/Zero_Lift_Report.pdf.
- Harrington C. Nurse Staffing in Nursing Homes in the U.S. Journal of Gerontological Nursing. 2005;31(2):18–23. doi: 10.3928/0098-9134-20050201-06. [DOI] [PubMed] [Google Scholar]
- Harrington C, Swan JH. Nursing home staffing, turnover, and case mix. Medical Care Research and Review. 2003;60:366–392. doi: 10.1177/1077558703254692. [DOI] [PubMed] [Google Scholar]
- Institute for the Future of Aging Services. The Long-Term Care Workforce: Can the Crisis be Fixed? Problems, Causes and Options. Washington, D.C: 2007. [Google Scholar]
- Iowa CareGivers Association. Certified Nursing Assistant Recruitment and Retention Pilot Project Final Report. 2000 Retrieved January 3, 2008. from http://www.iowacaregivers.org/uploads/pdf/DHSreport.pdf.
- Kash BA, Castle NG, Naufal GS, Hawes C. Effect of staff turnover on staffing: a closer look at registered nurses, licensed vocational nurses, and certified nursing assistants. The Gerontologist. 2006;46(5):609–619. doi: 10.1093/geront/46.5.609. [DOI] [PubMed] [Google Scholar]
- Myers D, Silverstein B, Nelson NA. Predictors of shoulder and back injuries in nursing home workers: A prospective study. American Journal of Industrial Medicine. 2002;41(6):466–476. doi: 10.1002/ajim.10076. [DOI] [PubMed] [Google Scholar]
- Parsons SK, Simmons WP, Penn K, Furlough M. Determinants of satisfaction and turnover among nursing assistants: the results of a statewide survey. Journal of Gerontological Nursing. 2003;29(3):51–58. doi: 10.3928/0098-9134-20030301-11. [DOI] [PubMed] [Google Scholar]
- Phillips DJ. The Price Tag On Turnover. Personnel Journal. 1990;69(2):58–61. [Google Scholar]
- Price J. Reflections on the determinants of voluntary turnover. International Journal of Manpower. 2001;22:600–624. [Google Scholar]
- Reinhard S, Stone R. Promoting quality in nursing homes: The Wellspring Model 2001 [Google Scholar]
- Squillace MR, Remsburg RE, Bercovitz A, Rosenoff E, Branden L. An Introduction to the National Nursing Assistant Survey [Electronic Version] 2006 Retrieved August 22, 2007 from http://aspe.hhs.gov/daltcp/reports/2006/NNASintro.pdf. [PubMed]
- Stone R, Weiner J. Who Will Care for Us? Addressing the Long-Term Care Workforce Crisis. 2001 Retrieved August 27, 2007. [Google Scholar]
- Wagner CM. Organizational commitment as a predictor variable in nursing turnover research: literature review. Journal of Advanced Nursing. 2007;60(3):235–247. doi: 10.1111/j.1365-2648.2007.04421.x. [DOI] [PubMed] [Google Scholar]
- Wooldridge J. Introductory Econometrics: A Modern Approach. Thomson/South-Western; 2006. [Google Scholar]