Abstract
Objective:
To evaluate adherence to medication and study factors associated with non-adherence in chronic kidney disease (CKD) patients.
Methods:
A prospective, cross-sectional, questionnaire based study was conducted in Nephrology department of a super specialty hospital. Patients above 18 years of age, suffering from CKD from six months or more were interviewed using self-designed, semi-structured questionnaire to get information about adherence to medication, diet restriction and lifestyle modification (n = 150). Morisky medication adherence questionnaire was used to calculate overall adherence. In this higher score indicates poor adherence. Main outcome measures included prevalence of non-adherence and factors associated with the same.
Results:
Average number of medicines taken by each patient was 8.0+1.612 (mean+SD) per day. Non-adherence to medication schedule was reported in 34% patients. Common causes of non-adherence were high cost (21.3%), complex dosing schedule (20%), fear of adverse effects (16%). Sixty-eight% patients were not aware about importance of taking each medicine. Sixteen% stopped taking medicines due to high cost. Forty-two% suggested that government should adopt measures to provide free medicines to poor patients. In Morisky medication adherence questionnaire high, medium and low adherence was reported in 7.3%, 55.3% and 37.3% of patients, respectively. Moderately positive correlation was observed between poor adherence and number of concurrent illnesses and number of medicines taken.
Conclusion:
Since majority of patients were not aware about importance of taking each medicine, creating awareness about the same is essential for improving adherence to therapy. Measures to provide free medicines to non-affording patients need to be implemented since high cost was other major cause of non-adherence.
KEY WORDS: Medication nonadherence, morisky medication adherence questionnaire, polypharmacy in chronic kidney disease
Introduction
Chronic kidney disease (CKD) is defined as abnormalities of kidney structure or function, present for more than 3 months, with implications for health.[1] It is a prolonged illness usually coexisting with diseases such as hypertension and diabetes. Consequently, these patients have to take a large pill burden on an average around 8–10 tablets/day.[2] This imposes high personal and monetary burden on patients and their families. Hence, adherence is a major concern in therapy of CKD. Adherence is defined as the extent to which individuals follow instructions they are given for prescribed treatments.[3]
World Health Organization estimates that only half of people with chronic diseases take their medications consistently as prescribed.[4] Nonadherence to medication can be harmful as well as expensive for patients. In CKD patients, it has been reported to cause uncontrolled hypertension, dialysis, increased medication, and hospitalization-related costs.[5] Thus, nonadherence reduces health benefits of drug therapy and augments advancement of CKD to end-stage renal disease.
Widely variable rates of nonadherence are reported in various studies depending on the type of instrument used. Previous studies have reported 26–28% CKD patients to be nonadherent.[6] Reasons for nonadherence have been shown to vary depending on disease[7,8] and characteristics of medicines prescribed.[9] Hence, it is necessary to understand nonadherence to medication in a particular disease and study factors affecting it. Various studies have reported factors such as polypharmacy, psychological factors to be responsible.[6,10] Other factors such as financial constraints, patients’ beliefs, and adverse drug reactions may be responsible for nonadherence. Hence, this study was planned to evaluate the extent of medication nonadherence within the CKD population and study factors responsible for the same.
Materials and Methods
This was a prospective, cross-sectional, questionnaire-based study carried out in nephrology department of a super specialty hospital after approval from the Institutional Ethics Committee. Patients suffering from CKD since 6 months or more, above 18 years of age, of either gender were included. Patients were included irrespective of stage of CKD and whether they were on dialysis or not. Patients meeting eligibility criteria were briefed about the study and informed consent obtained from those willing to participate. A self-developed, prevalidated, semi-structured questionnaire was used. The questionnaire was designed to obtain information about various issues concerned with medication nonadherence, exercise, dietary/fluid restrictions, and use of any nonprescribed medicines. The questionnaire was first pretested in five patients and appropriate modifications done. Morisky medication adherence questionnaire (MMAQ) was used to calculate overall adherence. Adherence was graded as high, medium, and low and higher score indicates low adherence. A total of 150 CKD patients were interviewed.
Statistical Analysis
Values are expressed as counts and percentage. Spearmann correlation test was used to find correlation among adherence, age, gender, number of medicines, and number of coexisting illnesses. GraphPad prism software version 6 was used to analyze data.
Results
One hundred and fifty patients participated in the study, out of which 84 were men and 66 were women. Mean age of respondents was 50.79 ± 9.97 (mean ± standard deviation [SD]) years. Average number of medicines taken in a day by each patient was 8.007 ± 1.612 (mean ± SD).
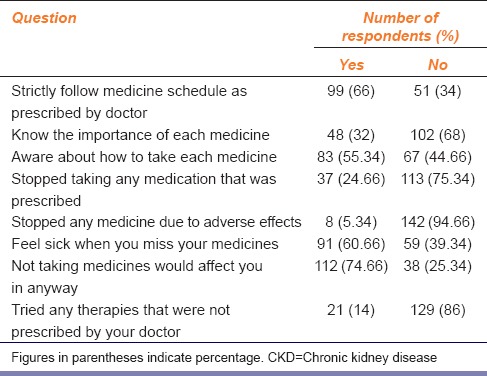
Thirty-four percentage patients did not strictly follow medicine schedule as prescribed and 68% patients were not aware about the importance of each medicine they were taking [Table 1].
Table 1.
Patients’ knowledge and practice about medicines for CKD (n=150)
In MMAQ, high, medium, and low adherence was reported in 7.3%, 55.3%, and 37.3% of patients, respectively. Not buying all medicines (24), not taking medicines for required duration (21), taking additional nonprescribed medicines (21), not taking medicine at prescribed time (18) were the commonly reported nonadherence practices (figures in parentheses indicate the number of patients).
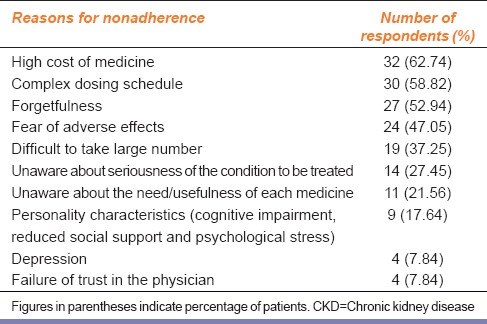
High cost (62.74%), complex dosing schedule (58.82%), and fear of adverse effects (47.05%) were the common causes of nonadherence [Table 2].
Table 2.
Reasons for nonadherence to medication in patients of CKD (n=51)
Fifty-four percentage of patients suggested that government should provide free or subsidized medicines to poor and nonaffording patients.
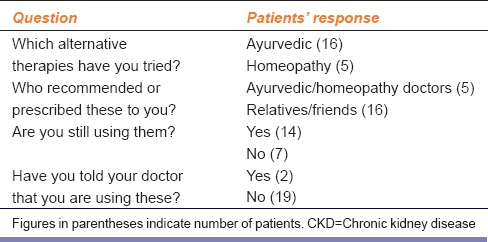
Some patients (21) used alternative therapies such as ayurvedic and homeopathy [Table 3]. Sixty-eight patients followed dietary restrictions as advised, 19 patients adhered to exercise schedule, eight practiced meditation, and eight took nutritional supplements.
Table 3.
Patients’ practice of alternative therapies for CKD (n=21)
Adherence score showed a moderately positive correlation with number of concurrent illnesses (Spearmann r: 0.5167, P < 0.0001) and number of medicines taken (Spearmann r: 0.6573, P < 0.0001). In MMAQ, higher score indicates poor adherence; hence, more the number of concurrent illnesses and the number of medicines taken, poorer is the adherence. Adherence score did not show any correlation with age or gender.
Discussion
In this study, data obtained from self-developed questionnaire showed that 34% patients were nonadherent to prescribed medication schedule whereas 37.33% patients showed low adherence in MMAQ. Thus, nearly identical rates of nonadherence were obtained by the two methods. This may be because, though grading of adherence apparently appears to be different in these two methods; both methods are subjective, based on patients’ response.
In a critical review of literature on adherence to prescribed oral medication in hemodialysis patients, percentage of nonadherent participants ranged from 3% to 80%.[11] Yet another study of 149 patients with CKD reported 17.4% to be nonadherent at baseline and 26.8% at 1 year.[6]
One of the major reasons of widely variable rates of nonadherence being reported in different studies is the inconsistency in uniform definition of nonadherence. Hence, it appears that a uniform and standard definition of nonadherence is essential to be able to study the prevalence of nonadherence in patients. Other reason for this may be that patients are known to underreport for nonadherence[12] or to report adherence according to personal definitions rather than conventional medical concepts of nonadherence.[13] Objective parameters for adherence that are easily measurable and can be verified are required to obtain reproducible and precise rates of nonadherence.
Poor adherence was found to have positive correlation with number of concurrent illnesses and number of medicines prescribed. Hence, complex medication schedule along with polypharmacy can be considered a significant predictor of nonadherence, as number of prescribed medicines is inversely related to adherence.[6,10]
Not buying all medicines and not taking medicines for required duration were the most common types of nonadherence. One of the major factors responsible for this is poor affordability. Cost has been implicated in nonadherence in several studies in patients suffering from chronic diseases. In a study of hemodialysis patients from 12 countries, proportion of patients who accepted not purchasing medicines due to high cost ranged from 3% (Japan) to 29% (United States).[14] Whether high cost is responsible for poor adherence to medication would depend on whether patients have to pay out of pocket for medicines or the expenses are covered by health insurance. In this study, majority of patients did not have any health insurance. Hence, high cost was one of the major factors responsible for poor adherence. This also reflects the views expressed by 54% of patients who suggested that government should provide free or subsidized medicines to poor patients.
Fear of adverse effects due to medication was another factor due to which patients are reluctant to adhere to the medication schedule. Adverse effects, if present, can play a crucial role in deciding whether or not patients will take their medications as prescribed.[15] Hence, health professionals can play a vital role in this matter in convincing patients that benefits of treatment outweigh risk of adverse effects.
Lack of knowledge about the usefulness of each medicine was another reason reported for nonadherence. Low knowledge about medications among patients has been reported in earlier studies.[10] Thus, it is evident that low health literacy along with complex medication schedule contributes to nonadherence, hence health professionals can play an active part in overcoming this barrier to adherence.
Though the number of patients who adhered to dietary restrictions as advised, which also includes fluid restriction, was significantly high (68%), this number should be still higher as these factors play a key role in progression of disease. Success of pharmacotherapy in CKD, particularly drugs such as phosphate binders, depends to a great extent on adherence to diet restriction. Poor adherence to these factors has been associated with increased hospitalization and death.[16] A study has reported that only 24% of hemodialysis patients had been adherent to fluid restrictions during the previous 14 days.[17] Hence, it is imperative that health professionals repeatedly emphasize upon patients about the importance of adhering to dietary and fluid restrictions.
Fourteen percentage of patients admitted to using alternative medicines which was not prescribed by their doctor. Use of such medicines in chronic illnesses has always been a matter of concern since most of these products contain a multitude of pharmacologically active ingredients which when used by patients with kidney disease, may be harmful. Further, most of the patients also accepted that they did not tell their doctor about use of these medicines. Several surveys have reported that most patients with chronic diseases did not disclose their use of alternative medicines to their conventional health care providers.[18,19] Though we did not enquire about the reasons for not disclosing the use of alternative medicines to their doctor, various reasons for nondisclosure have been reported such as the doctor did not enquire, they may disapprove of their use or they did not need to know about this use.[20] Considering this attitude of patients, it is important that health professionals be aware of use of alternative medicines in CKD patients and enquire about this use as a part of standard practice so that they can properly advise patients so as to prevent any harmful effects on kidney function.
To conclude, health professionals can play a vital role in removing most of the barriers to adherence. It is also important to consider patients’ concerns and priorities for appropriate management of this condition. Since high cost of medicines was one of the major causes of nonadherence, implementing measures to provide free or subsidized medicines to nonaffording patients need to be considered.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgment
We thank Dr. Avinash Turankar, Associate professor in Pharmacology, Government Medical College, Nagpur, for helping in statistical analysis.
References
- 1.KDIGO, CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation, prevention and management of chronic kidney disease-mineral and bone disorder. Kidney Int. 2013;3:1–150. [Google Scholar]
- 2.Manley HJ, Garvin CG, Drayer DK, Reid GM, Bender WL, Neufeld TK, et al. Medication prescribing patterns in ambulatory haemodialysis patients: Comparisons of USRDS to a large not-for-profit dialysis provider. Nephrol Dial Transplant. 2004;19:1842–8. doi: 10.1093/ndt/gfh280. [DOI] [PubMed] [Google Scholar]
- 3.McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: Scientific review. JAMA. 2002;288:2868–79. doi: 10.1001/jama.288.22.2868. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Adherence to Long-term Therapies: Evidence for Action. [Last accessed on 2015 Jan 12]. Available from: http://www.who.int/chp/knowledge/publications/adherence_report/en/
- 5.Manley HJ, Wang S, Nissenson AR. Denver, Colorado, November: 2010. Medication Non-adherence Predicts Hospitalization Rate and Healthcare Costs in Hemodialysis Patients. Renal Week 2010 American Society of Nephrology 43rd Annual Meeting. [Google Scholar]
- 6.Magacho EJ, Ribeiro LC, Chaoubah A, Bastos MG. Adherence to drug therapy in kidney disease. Braz J Med Biol Res. 2011;44:258–62. doi: 10.1590/s0100-879x2011007500013. [DOI] [PubMed] [Google Scholar]
- 7.Lacey J, Cate H, Broadway DC. Barriers to adherence with glaucoma medications: A qualitative research study. Eye (Lond) 2009;23:924–32. doi: 10.1038/eye.2008.103. [DOI] [PubMed] [Google Scholar]
- 8.Laws MB, Wilson IB, Bowser DM, Kerr SE. Taking antiretroviral therapy for HIV infection: Learning from patients’ stories. J Gen Intern Med. 2000;15:848–58. doi: 10.1046/j.1525-1497.2000.90732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DiMatteo MR. Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Med Care. 2004;42:200–9. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 10.Lindberg M, Lindberg P. Overcoming obstacles for adherence to phosphate binding medication in dialysis patients: A qualitative study. Pharm World Sci. 2008;30:571–6. doi: 10.1007/s11096-008-9212-9. [DOI] [PubMed] [Google Scholar]
- 11.Schmid H, Hartmann B, Schiffl H. Adherence to prescribed oral medication in adult patients undergoing chronic hemodialysis: A critical review of the literature. Eur J Med Res. 2009;14:185–90. doi: 10.1186/2047-783X-14-5-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: A summary of the literature. Med Care. 2004;42:649–52. doi: 10.1097/01.mlr.0000129496.05898.02. [DOI] [PubMed] [Google Scholar]
- 13.Rudd P. In search of the gold standard for compliance measurement. Arch Intern Med. 1979;139:627–8. [PubMed] [Google Scholar]
- 14.Hirth RA, Greer SL, Albert JM, Young EW, Piette JD. Out-of-pocket spending and medication adherence among dialysis patients in twelve countries. Health Aff (Millwood) 2008;27:89–102. doi: 10.1377/hlthaff.27.1.89. [DOI] [PubMed] [Google Scholar]
- 15.Awad GA. Antipsychotic medications: Compliance and attitudes toward treatment. Curr Opin Psychiatry. 2004;17:75–80. [Google Scholar]
- 16.Saran R, Bragg-Gresham JL, Rayner HC, Goodkin DA, Keen ML, Van Dijk PC, et al. Nonadherence in hemodialysis: Associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int. 2003;64:254–62. doi: 10.1046/j.1523-1755.2003.00064.x. [DOI] [PubMed] [Google Scholar]
- 17.Kugler C, Maeding I, Russell CL. Non-adherence in patients on chronic hemodialysis: An international comparison study. J Nephrol. 2011;24:366–75. doi: 10.5301/JN.2010.5823. [DOI] [PubMed] [Google Scholar]
- 18.Tangkiatkumjai M, Boardman H, Praditpornsilpa K, Walker DM. Prevalence of herbal and dietary supplement usage in Thai outpatients with chronic kidney disease: A cross-sectional survey. BMC Complement Altern Med. 2013;13:153. doi: 10.1186/1472-6882-13-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yeh GY, Davis RB, Phillips RS. Use of complementary therapies in patients with cardiovascular disease. Am J Cardiol. 2006;98:673–80. doi: 10.1016/j.amjcard.2006.03.051. [DOI] [PubMed] [Google Scholar]
- 20.Robinson A, McGrail MR. Disclosure of CAM use to medical practitioners: A review of qualitative and quantitative studies. Complement Ther Med. 2004;12:90–8. doi: 10.1016/j.ctim.2004.09.006. [DOI] [PubMed] [Google Scholar]


