Abstract
Aim:
To correlate the level of anxiety with nonadherence to antiretroviral medication.
Materials and Methods:
This observational, cross-sectional, hospital-based study was conducted in 78 patients attending antiretroviral therapy (ART) center of a tertiary care hospital of Odisha. The study duration was 6 months. Patients were designated as nonadherent by referring to the white card. Utilization of ART drugs and adverse drug reactions were included in a predesigned format. The anxiety level of all included patients was scored as per Hamilton Anxiety Rating Scale. Mean anxiety score of the adherent group was compared with that of the nonadherent group. Possible causes of nonadherence leading to high anxiety level were evaluated.
Results:
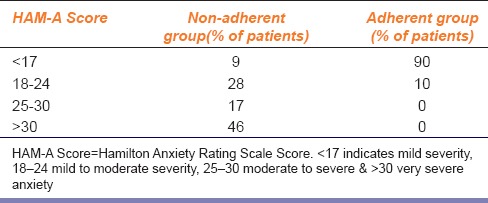
46% of patients in the nonadherent group had very severe, 17% had moderate to severe, 28% had mild to moderate and 9% had a mild level of anxiety. In the adherent group, however, mild to moderate level of anxiety was observed only in 10% patients.
Conclusions:
Anxiety is associated with sub-optimal medication adherence in HIV infected patients.
KEY WORDS: Adherence, antiretroviral therapy, Hamilton Anxiety Rating Scale, nonadherence
Introduction
About 5–11% of hospital admissions are due to complications of medication error and nonadherence.[1,2,3,4,5,6] Nonadherence to medication can lead to treatment failure and more hospitalization that can be both physically and emotionally stressful. Studies reveal that up to 50–60% patients show poor drug adherence and it is considered the most common cause of treatment failure.[7,8] Management of chronic disorders such as AIDS is complicated because of pill overload, burden of associated infective conditions, and lifelong drug therapy. Thus, the present study was planned with the aim to correlate between nonadherence to anti-HIV medication and level of anxiety using Hamilton Anxiety Rating Scale (HAM-A), and also to analyze the factors associated with anxiety that can lead to nonadherence in patients attending antiretroviral therapy (ART) center of a tertiary care hospital of Odisha.
Materials and Methods
This hospital-based, cross-sectional, observational, case-control study was conducted in patients attending ART center of a tertiary care teaching hospital of Odisha. The study continued for 6 months (July 2014 to December 2014). Permission of institutional ethics committee was obtained before starting the study. Patients within the age group of 18–60 years, on standard ART therapy and complying with the protocol were included for this study. Patients who were on any other medications for other chronic disorders and those with the previous history of anxiety or any psychological problem associated with anxiety were excluded from the study. Seventy-eight patients attending ART center of a tertiary care hospital of Odisha were interviewed for inclusion in the present study, out of which 55 patients complied with the protocol. Patients were designated as nonadherent by referring to the white card maintained by the ART center. Adherence is expressed in the white card in terms of percentage of pills taken out of a total number of pills given at previous visit by doing a pill count at every visit. Personal identification numbers were deleted to ensure anonymity. The proforma covered detailed demographic profile of patients, utilization pattern of antiretroviral drugs, adverse drug reactions (ADRs) encountered and other causes of anxiety that could have contributed to nonadherence. Symptoms of anxiety were entered in the HAM-A to reach at a total score.[9] This scale measures in a total score range of 0–56, where < 17 indicates mild severity, 18–24 mild to moderate severity, 25–30 moderate to severe, and >30 very severe level of anxiety.
Statistical Analysis
The mean anxiety score of the nonadherent group was compared with that of the adherent group using unpaired Student's t-test and P < 0.05 was taken as significant. Odds ratios (OR) with 95% confidence intervals (CI) were obtained for all causes for possible association with nonadherence. In addition, prevalence rate of each factor was calculated among the nonadherent patients.
Results
In the adherent group, only 10% patients had mild to moderate level of anxiety as per the HAM-A and rest had only mild anxiety. None of the patients had moderate to severe or very severe anxiety. On the contrary, when NA group was analyzed, 46% patients had very severe anxiety, 17% had moderate to severe anxiety, 28% had mild to moderate, and 9% had mild anxiety [Table 1]. When the mean anxiety score of nonadherent group (28.7) was compared with that of adherent group (8.5), the value was found out to be highly significant statistically (P < 0.001) suggesting high level of anxiety is associated with nonadherence to ART.
Table 1.
Comparison of anxiety level of adherent & non-adherent subjects
In the adherent group, the mean age was 36 years. The male:female ratio in this group was 1:1 suggesting no gender difference. Sixty percent of the patients had residence near to ART centre. On the other hand, the mean age of the nonadherent group was 41 years. Male:female ratio was 3:1 and 62.9% of patients have their residence far away. The educational status and monthly household income were comparable in both groups.
For most of the patients who were nonadherent, more than one factors were observed that could have increased anxiety level leading to nonadherence. The most common factor was a long distance from ART centre (62.86%); next common cause was an economical problem (31.43%). Forgetfulness and fear of ADRs contributed for 22.86% cases of nonadherence. Development of potential ADRs (8.57%), ignorance (5.71%), and noncompliance (2.86%) were other causes of nonadherent behavior [Figure 1]. When the OR with 95% CI were calculated for each of the above factors, long distance from ART center was found out to be the factor with highest OR which suggested strongest positive association.
Figure 1.
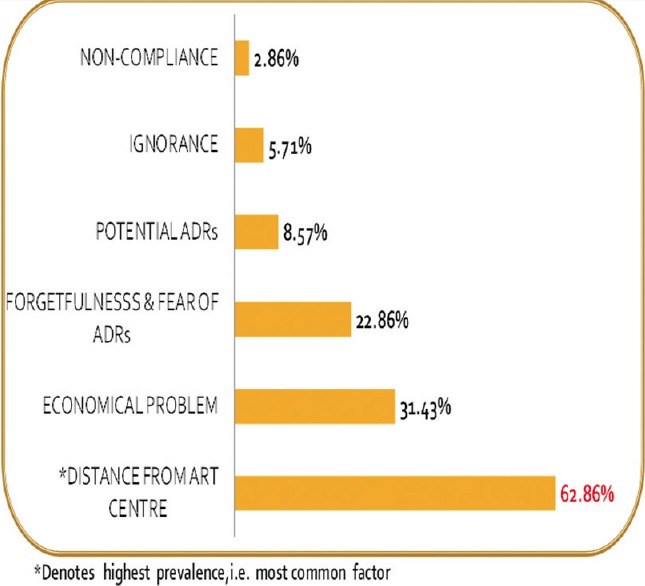
Various causes of nonadherence to antiretroviral therapy
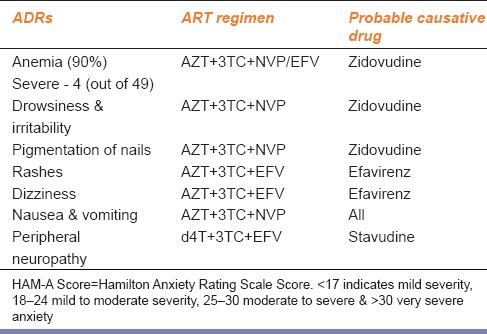
Table 2 presents different (ADRs) observed with the use of antiretroviral drugs. Anemia was observed in almost 90% of patients on Zidovudine-based therapy; out of which, 10% had severe anemia (<7 g/dl Hb). Drowsiness, irritability, and pigmentation of nails were also more commonly associated with AZT-based therapy. Use of efavirenz was associated with rashes and dizziness in these patients. Nausea and vomiting were common ADR with all the three drugs, i.e., Zidovudine, Lamivudine, and Nevirapine. Peripheral neuropathy was more commonly observed with Stavudine-based therapy.
Table 2.
Adverse drug reaction profile of patients on ART
Discussion
Nonadherence to medication is a very common problem in chronic disorders. This problem is aggravated in countries such as India because of the associated low socioeconomic condition and low educational background of the people suffering from these disorders. A number of Western studies have highlighted the association of high anxiety level with ART nonadherence. There is a possibility that anxiety level in our patients is more complicated because of the complex socioeconomic condition. Literature search revealed that there is a paucity of data regarding drug adherence in HIV-infected patients on drug therapy in our set up. Hence, this study was undertaken to quantify nonadherence to anti-HIV therapy, to probe the possible association of anxiety level with nonadherence and to explore the other causes leading to anxiety. Theofilou of Panteion University, Athens, Greece, found that anxiety is associated with sub-optimal medication adherence in diverse samples of patients with HIV.[10] Sundbom and Bingefors suggested that patients experiencing symptoms of psychological distress are at increased risk of NA and would thus benefit from extra attention.[11] St. Louis et al. of Washington University, USA, found an association between anxiety and poor rates of HIV viral suppression.[12]
Present study provides data from the Eastern region of India. The findings were quite similar to those of previous studies in this field. In contrast to mean age, which was comparable in both the groups, male:female ratio was found to be more in the nonadherent group. This male preponderance may be due to the fact that males are mostly the earning members of the family and so they have to stay out of station many times from where they cannot come for drug collection. In addition, males are more predisposed to alcoholism and substance abuse which may lead to anxiety and thus, poor adherence. Other parameters such as the educational status of the patients and monthly household income were similar in both the groups.
HAM-A is a standard procedure to measure anxiety level of the patients. A significant percentage of patients (46%) had a very severe level of anxiety among the nonadherent group. This is followed by 28% mild to moderate level of anxiety, but on the contrary, only 10% of the patients in the adherent group had mild to moderate level of anxiety. Mild anxiety is expected with any AIDS patients because of sociocultural stigma in our society.
When different causes of nonadherence to ART were traced, increased distance from ART center for the collection of ART drugs was observed to be the most strongly associated factor (~63%). This finding suggests that more number of ART centers can help ART adherence. Travel from distant areas, lack of a regular suitable vehicle, financial problems, and possible loss of wages for that day are important factors which lead to anxiety and prevent the patients from coming to ART centers for drug collection. The second most common factor associated with nonadherence was an economical problem, which could again lead to increased worry and anxiety. The third factor was forgetfulness and fear of ADRs which might be aggravated by anxiety. The development of potential ADRs might have led to even more anxiety and apprehension. Ignorance regarding the benefits of medication, their proper dosage, and the possible ADRs might be the cause of anxiety which would then lead to nonadherence.
This study evaluates the association between two very common, yet not readily apparent, problems in health care professional's practice, i.e., psychological distress and NA. While patients with symptoms of anxiety often visit their health care professional, the majority of these visits are for somatic symptoms.[13] As a consequence, the psychological distress may not be revealed.[14,15,16] It is important, therefore, to watch for early indications of psychological distress in order to identify possible future NA. A negative spiral could plausibly be initiated if the psychological distress is not discovered: Poor physical health can cause poor mental health, which can result in NA, and NA can result in even poorer physical health, and even worse mental health.[17] Consequently, health care professionals need to be conscious of the connection between psychological distress and NA. When patients obtain relief from their psychological distress, improvement in medication adherence is possible. Screening for anxiety is an important aspect of routine care. Specific interventions for anxiety can then be tested to improve outcomes in the HIV outpatient setting.
Conclusion
Our study conclusively proved that nonadherence to anti-HIV medication is associated with the severe level of anxiety in comparison to adherent patients. Distance from ART center was the most strongly associated causative factor for anti-HIV nonadherence. Anemia was the most common ADR seen in patients on ART in this study. The inclusion of questions on both intentional and nonintentional type and active approach of the patients that excludes selection bias were the strength of our study. However, the small sample size and short study duration were the limitations of this study. Further study including a larger sample size can provide additional information for this complicated problem in the management of this chronic disorder.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
References
- 1.Theofilou P, Panagiotaki H. A literature review to investigate the link between psychosocial characteristics and treatment adherence in cancer patients. Oncol Rev. 2012;6:e5. doi: 10.4081/oncol.2012.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Theofilou P. Patient adherence to treatment. J Clin Res Bioeth. 2012;3:e107. [Google Scholar]
- 3.Theofilou P. Medication adherence in Greek hemodialysis patients: The contribution of depression and health cognitions. Int J Behav Med. 2013;20:311–8. doi: 10.1007/s12529-012-9231-8. [DOI] [PubMed] [Google Scholar]
- 4.Theofilou P. Interventions to support medication adherence in individuals with chronic disease: The role of health professionals. J Community Med Health Educ. 2012;2:e104. [Google Scholar]
- 5.Theofilou P, Saborit AR. Health locus of control and diabetes adherence. J Psychol Psychother. 2012;S3:e002. [Google Scholar]
- 6.Theofilou P, Saborit AR. Predictors of asthma treatment adherence. J Psychol Psychother. 2012;S3:e001. [Google Scholar]
- 7.Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: Three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331–42. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 8.Sabaté E. Geneva, Switzerland: WHO; 2003. Adherence to Long-term Therapies: Evidence for Action. [Google Scholar]
- 9.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 10.Theofilou P. Anxiety and medication adherence in HIV. J AIDS Clin Res. 2012;S1:e001. doi: 10.4172/2155-6113S1-e001. [Google Scholar]
- 11.Sundbom LT, Bingefors K. The influence of symptoms of anxiety and depression on medication nonadherence and its causes: A population based survey of prescription drug users in Sweden. Patient Prefer Adherence. 2013;7:805–11. doi: 10.2147/PPA.S50055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shacham E, Morgan J, Onen N, Overton ET. 6th International Conference on HIV Treatment and Prevention Adherence; 22-24 May; 2011. The Negative Impact of Anxiety on HIV Care. [Google Scholar]
- 13.Stordal E, Bjelland I, Dahl AA, Mykletun A. Anxiety and depression in individuals with somatic health problems. The Nord-Trøndelag Health Study (HUNT) Scand J Prim Health Care. 2003;21:136–41. doi: 10.1080/02813430310002030. [DOI] [PubMed] [Google Scholar]
- 14.Karlsson H, Lehtinen V, Joukamaa M. Are frequent attenders of primary health care distressed? Scand J Prim Health Care. 1995;13:32–8. doi: 10.3109/02813439508996732. [DOI] [PubMed] [Google Scholar]
- 15.Ostergaard SD, Foldager L, Allgulander C, Dahl AA, Huuhtanen MT, Rasmussen I, et al. Psychiatric caseness is a marker of major depressive episode in general practice. Scand J Prim Health Care. 2010;28:211–5. doi: 10.3109/02813432.2010.501235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lecrubier Y. Widespread underrecognition and undertreatment of anxiety and mood disorders: Results from 3 European studies. J Clin Psychiatry. 2007;68(Suppl 2):36–41. [PubMed] [Google Scholar]
- 17.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]


