Abstract
Objectives:
This study aimed to identify the current knowledge, attitude, and perception (KAP) of the future prescribers about antimicrobial (AM) education so that the identified lacunae in the training curriculum can be effectively addressed.
Materials and Methods:
A questionnaire-based survey was carried out in the 2nd year students of medical and the dental undergraduate (UG) courses at a tertiary care teaching center in Jaipur. Each respondent completed the given questionnaire independently in the allocated time. A scoring system was used to rate the KAP of the respondents as poor, average, or good.
Results:
Statistically significant differences were found in the KAP of the medical and dental future prescribers (P = 0.0086, 0.0002, and <0.0001 for the KAP, respectively).
Conclusion:
The attitude of the UG students towards AM education is good, but the deficiencies in the knowledge and perception need to be improved further. Suitable interventions to address these lacunae must be planned.
KEY WORDS: Antimicrobial pharmacology, antimicrobial stewardship education, clinical case-based learning, dental undergraduates, medical undergraduates
Introduction
With the increasing antimicrobial (AM) resistance and the cost of AMs, the implementation of AMs education in the undergraduate (UG) curriculum is crucial as mere guidelines are not enough to change the behavior of the future prescribers.[1,2]
This study delineates the knowledge, attitude, and perception (KAP) of the UG about AM, which exemplifies the principles of AM stewardship so that the loopholes in the teaching curriculum can be stitched in time. Understanding of the KAP of our future prescribers about AMs education will facilitate better and more effective education for them.
Materials and Methods
This study was approved by the Institutional Ethics Committee of Mahatma Gandhi Medical College and conducted during October 2014 for 2 weeks. At the end of the pharmacology demonstration class, all the students’ were briefly described the aims and the objectives of the study and the importance of participation in the study. At first, the medical students were approached and during the subsequent week, the dental students were recruited in a similar manner. A written informed consent was sought from those who wished to participate. Neither threat nor any pressure was generated on the students who denied participation. 80% of the students from each faculty participated in this study. A total of 120 medical and 48 dental students who volunteered for this study were presented with a structured and pretested questionnaire in English, which was designed after modifications from the work of Abbo and Rocha. Senior Professors from the Departments of Microbiology, Pharmacology, Medicine and Community Medicine, who are the experience holders with research and academic experience in their respective subjects, validated the questionnaire for its content and relevance.
The questionnaire had three sections. The first assessed the knowledge of the respondents about rational AM prescribing practices, the second section judged the attitude of the prescribers about AM stewardship education and the third section analyzed how the respondents rate their acquired skills and knowledge of AM taught to them as a part of their 2nd year curriculum. The respondents answered the questionnaire independently in 20 min without using any reference materials, notes, or assistance. The collected data was analyzed using (SPSS for Windows, version 16.0 Chicago, SPSS Inc.), Excel 2007 with statistical significance evaluated using two sided P value at a 5% level of significance.
Scoring
For knowledge, each correct answer was given a score of 1 while each wrong answer was given a score of 0. Each question in the knowledge section only had one correct answer and three wrong answers. This way, a respondent could score a maximum of 12 and a minimum of 0 in this section. For attitude, a score of 1 was given to “disagree,” a score of 2 was given to “don’t know,” and a score of 3 was given to “agree.” There were four negatively-framed statements for which reverse scoring was done which means a score of 1 was given to “agree,” 2 to “don’t know,” and 3 to “disagree.” This way, a respondent could score a maximum of 24 and a minimum of 8 in the attitude section. For perception, each “yes’ response received a score of 1 while each “no” received a score of 0. Therefore, a respondent could score a maximum of 12 and a minimum of 0 in the practice section. The total KAP scores were calculated and analyzed by statistical tests for their significance. The scores were also classified as poor, average, and good.
Results
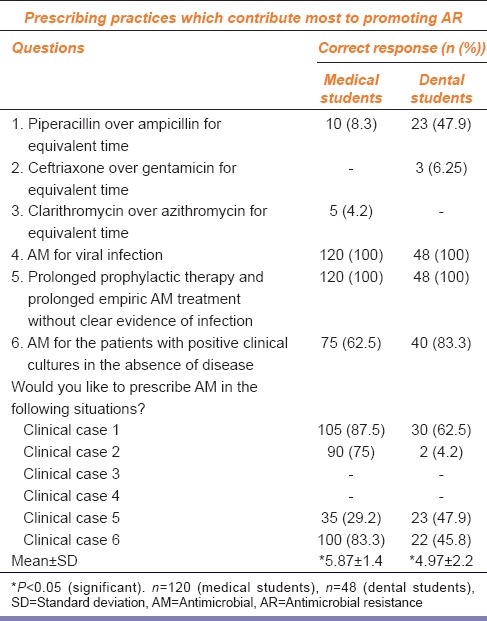
A total of 120 medical and 48 dental UG participated in the study of which only 50% and 33% could answer the questions, respectively, in the knowledge section. Statistically significant difference was noted in the knowledge of medical and the dental UG (P = 0.0086) [Table 1]. Classification of the medical respondents on the basis of poor (0–4), average (5–8), and good (9–12) knowledge scores indicated 20, 95, and 5 students in respective categories in contrast to 15 and 33 dental respondents in poor and average categories only.
Table 1.
Knowledge of the students about good prescribing practices and the frequency of antibiotics use in a given clinical case
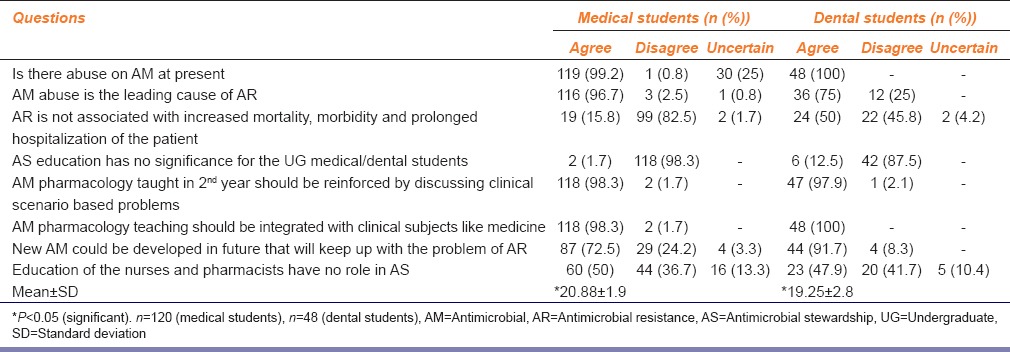
Attitude
98% medical and all dental students had a positive attitude for integrating the AM pharmacology teaching with the clinical subject of medicine [Table 2]. Statistically significant differences were noted in the attitude of the medical and the dental students (P = 0.0002). Classification of the medical respondents on the basis of poor (8–12), average (13–18), and good (19–24) attitude scores indicated 1, 11, and 108 students in respective categories in contrast to 17 and 31 dental respondents in average and good categories.
Table 2.
Attitude of the students about education for antimicrobial stewardship
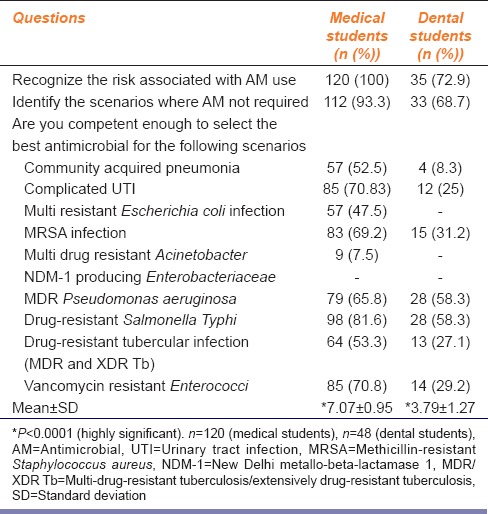
Perception
Table 3 shows statistically significant differences in the perception of both the medical and dental UG (P<0.0001). Classification of the medical respondents on the basis of poor (0–4), average (5–8), and good (9–12) perception scores indicated all 120 students in the average category in contrast to 28 and 20 dental respondents in poor and average categories.
Table 3.
Perception of the students about their acquired knowledge and skills
Discussion
Few studies have specifically assessed the perception and attitude of the UG medical students.[3,4] This study is noteworthy and unique as it not only assesses the attitude, perception of UG students who hailed from two specific UG courses of medical and dentistry but also provides insight of their current knowledge of common clinical scenarios.
The respondent's scored average in their knowledge about specific AMs. Not even 50% of the respondents knew that prescribing broad spectrum AM when narrow spectrums are equally effective, is a fallacious practice contributing to AM resistance.[5,6] When the respondent's knowledge was assessed by prefabricated clinical scenario based questions it was found that 30% of the medical and 4% of the dental respondents had only average knowledge about the given clinical scenarios based questions. These findings differ from another study where 39% of the respondents scored above average[7] for the clinical scenario based questions.
A previous study conducted with 2nd year UG students has emphasized the importance and advantages of the clinical case-based learning in Pharmacology teaching.[8] Contemporary medical and dental curriculum suffers from the problem that teaching pharmacology along with simultaneous reinforcement through discussing interactive clinical problem-solving scenarios for selecting rational AM drug has a time constraint.[4] The majority of the UGs experience great hardships when they enter into clinical practice. If the UGs become familiar with the AM, with reinforced skills for the patient care it will contribute towards rational use of AM and form the pedestal for successful AM stewardship program in future.[9,10]
In our study, 98% of the medical and 87% of the dental UG had a positive attitude towards the AM stewardship education. Some similarity can be drawn from the study of Huang et al. which highlights that 74% of the medical students favored AM stewardship education in China.[11] The majority (98%) of the medical and all the dental UG believed that AM pharmacology teaching in a 2nd year should be integrated with clinical subjects. These results were also consistent with the previous study of Vasundara et al.[12] The positive attitude of the respondents toward the statement that new AM could be developed in future to resolve the problem of AM resistance suggests that they rely on new AM for solving the problems of AM resistance. Inappropriate prescribing of AM known at present can pose serious AM resistance which would be difficult to tackle even with newer AM. Surprisingly, almost 50% of the medical and the dental respondents were unaware of the importance of the education of the nurses and pharmacists in AM stewardship program.
The results on attitude and perception of the respondents’ further support the previous study of Davey et al. which highlighted the need to train the future prescribers about rational AM prescribing.[13] It is worth noting that Medical Colleges in many foreign countries such as the UK, the USA have revamped their curricula for training good AM prescribing practices at UG level itself.[1] Such initiatives of teaching approach to AM use and choice of therapy by the clinical case-based approach in the medical, dental, pharmacy, nursing curriculum should be taken in India also. Respondent's perception about AM education is consistent with the findings from previous surveys of Abbo et al.[3] Future prescribers should have sound knowledge about drug resistant microorganisms which are currently increasing and the choice of AMs to treat them based on the isolate reports.
Our study prompts the need for introduction of certain interventions, for example, interactive sessions and clinical case-based learning with special emphasis on the irrational prescribing practices in which AM are not required or can be delayed safely for some time. Such education should be introduced at the 2nd year of UG curriculum itself, as it improves the rational prescribing. Newer and innovative teaching methods such as open access learning sites imparting the recent, accurate information for AM use should be introduced.
The strength of our study was that the survey was voluntary, and the respondents were not allowed to take any assistance for filling the questionnaire, so the actual KAP of the volunteers were collected. However, the respondents in this study hailed from single Medical and Dental College.
Despite this limitation, this study suggests integrating AM pharmacology teaching with the clinical subjects to encourage and strengthen AM stewardship education.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgment
We express our sincere thanks to all the students who volunteered to participate in this study.
References
- 1.Pulcini C, Gyssens IC. How to educate prescribers in antimicrobial stewardship practices. Virulence. 2013;4:192–202. doi: 10.4161/viru.23706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spellberg B. The antibiotic crisis: Can we reverse 65 years of failed stewardship? Arch Intern Med. 2011;171:1080–1. doi: 10.1001/archinternmed.2011.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abbo LM, Cosgrove SE, Pottinger PS, Pereyra M, Sinkowitz-Cochran R, Srinivasan A, et al. Medical students’ perceptions and knowledge about antimicrobial stewardship: How are we educating our future prescribers? Clin Infect Dis. 2013;57:631–8. doi: 10.1093/cid/cit370. [DOI] [PubMed] [Google Scholar]
- 4.Dyar OJ, Pulcini C, Howard P, Nathwani D ESGAP (ESCMID Study Group for Antibiotic Policies) European medical students: A first multicentre study of knowledge, attitudes and perceptions of antibiotic prescribing and antibiotic resistance. J Antimicrob Chemother. 2014;69:842–6. doi: 10.1093/jac/dkt440. [DOI] [PubMed] [Google Scholar]
- 5.Sanchez GV, Roberts RM, Albert AP, Johnson DD, Hicks LA. Effects of knowledge, attitudes, and practices of primary care providers on antibiotic selection, United States. Emerg Infect Dis. 2014;20:2041–7. doi: 10.3201/eid2012.140331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bowes J, Yasseen AS 3rd, Barrowman N, Murchison B, Dennis J, Moreau KA, et al. Antimicrobial stewardship in pediatrics: Focusing on the challenges clinicians face. BMC Pediatr. 2014;14:212. doi: 10.1186/1471-2431-14-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rocha MC, Fiol F, Miranda F, Rocha J, Filho SB, Barreiros RC. Profile of prescribers and prescription of antibiotics in upper respiratory infections in pediatrics. Rev Paul Pediatr. 2012;30:471–8. [Google Scholar]
- 8.Gupta K, Arora S, Kaushal S. Modified case based learning: Our experience with a new module for pharmacology undergraduate teaching. Int J Appl Basic Med Res. 2014;4:90–4. doi: 10.4103/2229-516X.136786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.MacDougall C, Polk RE. Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev. 2005;18:638–56. doi: 10.1128/CMR.18.4.638-656.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sbarbaro JA. Can we influence prescribing patterns? Clin Infect Dis. 2001;33(Suppl 3):S240–4. doi: 10.1086/321856. [DOI] [PubMed] [Google Scholar]
- 11.Huang Y, Gu J, Zhang M, Ren Z, Yang W, Chen Y, et al. Knowledge, attitude and practice of antibiotics: A questionnaire study among 2500 Chinese students. BMC Med Educ. 2013;13:163. doi: 10.1186/1472-6920-13-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vasundara K, Kanchan P, Pundarikaksha HP, Girish K, Prassana S, Jyothi R. An imperative need to change pharmacology curriculum: A pilot survey. Indian J Pharmacol. 2010;42:420. doi: 10.4103/0253-7613.71901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davey P, Garner S. Professional Education Subgroup of SACAR. Professional education on antimicrobial prescribing: A report from the Specialist Advisory Committee on Antimicrobial Resistance (SACAR) Professional Education Subgroup. J Antimicrob Chemother. 2007;60(Suppl 1):i27–32. doi: 10.1093/jac/dkm154. [DOI] [PubMed] [Google Scholar]


