Arakawa et al. discovered that the autoimmune response in psoriasis is directed against melanocytes. They show that the main psoriasis risk allele HLA-C*06:02 mediates melanocyte-specific autoimmunity and identify ADAMTSL5 as a melanocyte autoantigen, which stimulates IL-17 and IFN-γ production in CD8+ T cells.
Abstract
Psoriasis vulgaris is a common T cell–mediated inflammatory skin disease with a suspected autoimmune pathogenesis. The human leukocyte antigen (HLA) class I allele, HLA-C*06:02, is the main psoriasis risk gene. Epidermal CD8+ T cells are essential for psoriasis development. Functional implications of HLA-C*06:02 and mechanisms of lesional T cell activation in psoriasis, however, remained elusive. Here we identify melanocytes as skin-specific target cells of an HLA-C*06:02–restricted psoriatic T cell response. We found that a Vα3S1/Vβ13S1 T cell receptor (TCR), which we had reconstituted from an epidermal CD8+ T cell clone of an HLA-C*06:02–positive psoriasis patient specifically recognizes HLA-C*06:02–positive melanocytes. Through peptide library screening, we identified ADAMTS-like protein 5 (ADAMTSL5) as an HLA-C*06:02–presented melanocytic autoantigen of the Vα3S1/Vβ13S1 TCR. Consistent with the Vα3S1/Vβ13S1-TCR reactivity, we observed numerous CD8+ T cells in psoriasis lesions attacking melanocytes, the only epidermal cells expressing ADAMTSL5. Furthermore, ADAMTSL5 stimulation induced the psoriasis signature cytokine, IL-17A, in CD8+ T cells from psoriasis patients only, supporting a role as psoriatic autoantigen. This unbiased analysis of a TCR obtained directly from tissue-infiltrating CD8+ T cells reveals that in psoriasis HLA-C*06:02 directs an autoimmune response against melanocytes through autoantigen presentation. We propose that HLA-C*06:02 may predispose to psoriasis via this newly identified autoimmune pathway.
Psoriasis vulgaris (OMIM no. MIM177900) is among the most frequent T cell–mediated disorders, affecting 120–180 million people worldwide by a chronically relapsing hyperproliferative skin inflammation (Griffiths and Barker, 2007; Lowes et al., 2007). Within a complex genetic predisposition, HLA-C*06:02 on psoriasis susceptibility locus PSORS1 (6p21.33) is the main psoriasis risk allele (Nair et al., 2006). HLA-C*06:02 is present in more than 60% of patients, increases the risk for psoriasis 9- to 23-fold, and decides an earlier onset and more severe disease course (Gudjonsson et al., 2003). A direct contribution of HLA-C*06:02 to psoriasis manifestation, however, could not be determined as the result of a strong linkage disequilibrium within the PSORS1 locus (Lowes et al., 2007) and a lack of experimental systems for analyzing its function in psoriasis.
HLA class I molecules present peptide antigens to CD8+ T cells. Novel psoriasis lesions develop upon epidermal influx (Conrad et al., 2007) and clonal expansion of CD8+ T cells, indicating persistent CD8+ T cell recruitment and activation by locally presented autoantigens (Chang et al., 1994; Kim et al., 2012). Potential psoriatic autoantigens have been proposed by us and others mainly based on the hypothesis that the lesional CD8+ T cells react against keratinocytes (Valdimarsson et al., 2009; Besgen et al., 2010; Lande et al., 2014). Nevertheless, the target cells and antigens that drive pathogenic CD8+ T cell responses in psoriasis lesions are still unproven. Accordingly, an autoimmune pathogenesis of psoriasis remained hypothetical to date.
We formerly established an unbiased technique to characterize αβ TCRs of single T cells (Kim et al., 2012). By this method, we identified dominant CD8+ T cell clones in psoriasis lesions and determined the molecular structure of their paired TCR α- and β-chain rearrangements. Clonal T cell expansions in autoimmune lesions result from a T cell response to locally presented autoantigens (Kent et al., 2005). Epidermal psoriatic CD8+ T cells preferentially rearrange TCR Vβ13S1 (Chang et al., 1994). Here, we reconstitute a Vα3S1/Vβ13S1 TCR from an epidermal CD8+ T cell clone isolated from a psoriasis lesion of an HLA-C*06:02–positive patient in a T hybridoma cell line. Along with human CD8αβ and NFAT-sGFP transfection, this TCR hybridoma reports on TCR signaling by robust sGFP expression (Seitz et al., 2006; Siewert et al., 2012). Assuming that the Vα3S1/Vβ13S1-TCR hybridoma carries the antigen specificity of pathogenic psoriatic CD8+ T cells, we used it to explore the mechanisms of lesional psoriatic T cell activation.
RESULTS AND DISCUSSION
Melanocytes are HLA-C*06:02–restricted autoimmune target cells of the Vα3S1/Vβ13S1 TCR
We first analyzed the reactivity of the Vα3S1/Vβ13S1 TCR in co-culture experiments with various skin cell types in association with HLA-C*06:02. We observed that primary melanocytes from both HLA-C*06:02–positive psoriasis patients and healthy donors, but not HLA-C*06:02–negative psoriasis patients or healthy individuals, activated the Vα3S1/Vβ13S1-TCR hybridoma (Fig. 1, A and B). Hybridoma activation was enhanced by preincubation of melanocytes with IFN-γ to increase the otherwise low HLA-C surface expression (McCutcheon et al., 1995) and inhibited by an HLA class I–blocking antibody (Fig. 1, B and C). To specify the role of HLA-C*06:02 in Vα3S1/Vβ13S1-TCR ligation, we co-cultured the TCR hybridoma with two inherently HLA-C*06:02–positive melanoma cell lines, WM278 (Fig. 1 D) and 1205Lu (not depicted) as melanocyte surrogates. Both of them activated the TCR hybridoma when preincubated with IFN-γ to induce HLA-C (Fig. 1 C). Two HLA-C*06:02–negative melanoma cell lines, WM9 (Fig. 1 E) and WM1232 (not depicted), activated the Vα3S1/Vβ13S1-TCR hybridoma only upon transfection with HLA-C*06:02, but not HLA-A*02:01. This effect was independent from IFN-γ and suppressed by HLA class I blockade.
Figure 1.
HLA-C*06:02-positive melanocytes are skin-specific target cells of the Vα3S1/Vβ13S1 TCR. (A and B) TCR hybridoma (round cells) activation by HLA-C*06:02–positive (left) but not HLA-C*06:02–negative (right) primary human melanocytes (elongated) in the presence of IFN-γ, as determined by combined UV-light microscopy (A) or flow cytometry and effect of melanocyte preincubation with IFN-γ or an HLA class I–blocking antibody (B). Data represent three HLA-C*06:02–positive (healthy n = 2, psoriasis n = 1) and nine HLA-C*06:02–negative subjects (healthy n = 7, psoriasis n = 2) as mean ± SD. Numbers give stimulating/total samples. *, P < 0.05; ***, P < 0.005; two tailed Fisher’s exact. Bars, 20 µm. (C) Western blot analysis of HLA-C expression in primary melanocytes or WM278 cells cultured without/with IFN-γ or HLA-C*06:02–negative WM9 cells without/with HLA-C*06:02 transfection. (D and E) Hybridoma activation by an HLA-C*06:02–positive (WM278) or HLA-C*06:02–negative (WM9) melanoma cell line transfected with HLA-C*06:02 or HLA-A*02:01 and effect of a blocking HLA antibody. (F and G) Hybridoma activation by HLA-C*06:02–negative primary keratinocytes (F) or the HLA-C*06:02–negative epithelial carcinoma cell line A431 (G) transfected with HLA-C*06:02 or HLA-A*02:01 or cotransfected with HLA-C*06:02 and mimotope #6. Data represent three (C, E, and F), five (D), and two (G) independent experiments as mean ± SD.
No hybridoma activation was seen with HLA-C*06:02–transfected primary human keratinocytes (Fig. 1 F), epithelial A431 cells (Fig. 1 G), the keratinocyte cell line, HaCaT, or HLA-C*06:02–positive primary skin fibroblasts (not depicted). This was surprising because former disease models had proposed keratinocytes as immune targets in psoriasis (Valdimarsson et al., 2009). Keratinocytes and epithelial cell lines, however, could present antigen and stimulate the TCR hybridoma upon cotransfection with HLA-C*06:02 and an appropriate Vα3S1/Vβ13S1-TCR ligand, mimotope #6 (Fig. 1, F and G) identified by peptide library screening (see Fig. 3, A and B). Together, these experiments identified melanocytes as HLA-C*06:02–restricted autoimmune target cells of the Vα3S1/Vβ13S1 TCR.
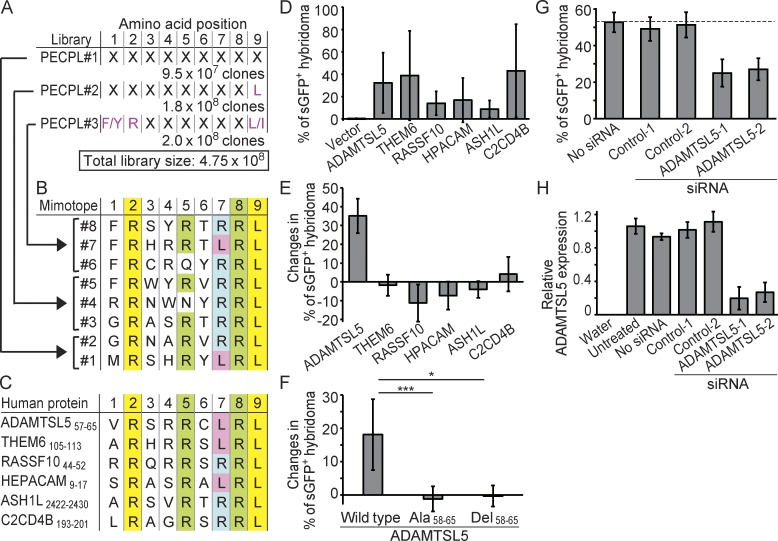
Figure 3.
ADAMTSL5 is an HLA-C*06:02–presented melanocytic autoantigen of the Vα3S1/Vβ13S1 TCR. (A) Design of PECPLs #1–3. Predefined amino acid residues are in pink; X indicates randomized. (B and C) Mimotopes derived from PECPLs #1–3 (B) and natural human TCR peptide ligands stimulating the Vα3S1/Vβ13S1 TCR (C). HLA-C*06:02 anchor positions are labeled in yellow, and other conserved amino acids in green, blue, or pink. (D) TCR hybridoma stimulation by plasmid-encoded human peptide epitopes cotransfected with HLA-C*06:02 into COS-7 cells as normalized to CD3 stimulation. (E and F) Changes in TCR hybridoma activation by full-length proteins (E) or by wild-type, epitope-mutated (Ala58-65) or epitope-deleted (Del58-65) full-length ADAMTSL5 transfected into WM278 cells preincubated with IFN-γ as compared with vector control (F). Data represent three (D and E) and five (F) independent experiments as mean ± SD; *, P < 0.05; ***, P < 0.005; two tailed Mann-Whitney U test. (G) TCR hybridoma activation by WM278 cells transfected with two different control siRNAs or siRNAs targeting ADAMTSL5 and incubated with IFN-γ as compared with mock control. Data represent three biological triplicates as mean ± SD. (H) Validation of ADAMTSL5 knockdown by qPCR in triplicates and normalized to PBGD. Data are given as mean ± SD.
CD8+ T cells in lesional psoriatic epidermis target melanocytes
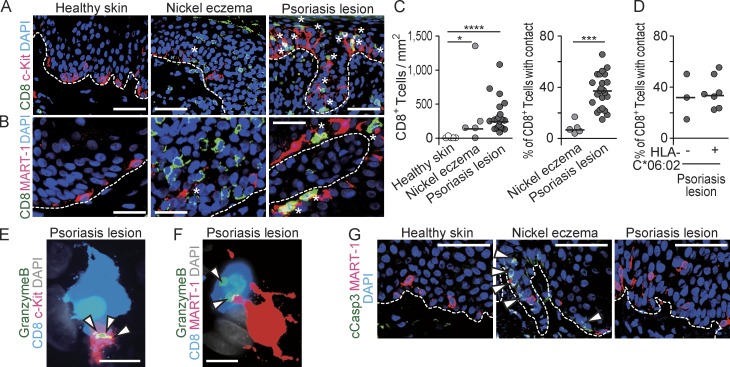
To determine whether the reactivity of the Vα3S1/Vβ13S1 TCR reflected a common pathway of psoriatic T cell activation, we assessed the epidermal distribution of CD8+ T cells in chronic psoriatic plaques (n = 23), healthy skin (n = 5), and nickel contact eczema (n = 5), another T cell–mediated inflammatory skin disease induced by a defined antigen. Tissue sections were immunostained for CD8 and the melanocyte markers MART-1 or c-Kit (Fig. 2, A and B). Consistent with a previous study (Bovenschen et al., 2005), the numbers of CD8+ T cells were significantly higher in the epidermis of psoriasis lesions and nickel eczema than in normal skin (Fig. 2 C). Significantly more CD8+ T cells exhibited direct contacts with melanocytes in psoriasis (median 37.2%, SD 15.4) than in nickel eczema (median 6.9%, SD 4.92; Fig. 2 C). In psoriasis biopsies where HLA-C*06:02 typing was available, contact frequencies in HLA-C*06:02–positive (n = 7) and negative (n = 3) samples were in a similar range (Fig. 2 D). The psoriatic CD8+ T cells polarized lytic granules containing Granzyme B toward the melanocyte contact sites (Fig. 2, E and F), indicating TCR-mediated activation. Lytic granules constitute an important effector mechanism of CD8+ T cells, but their directed release does not necessarily induce apoptosis of target cells (Knickelbein et al., 2008). Indeed, an antibody against cleaved Caspase 3 (cCASP3), a crucial mediator of apoptosis (Porter and Jänicke, 1999) detected no signs of cell death in melanocytes in psoriatic epidermis (Fig. 2 G). Instead, melanocyte numbers in psoriasis lesions were reportedly increased (Wang et al., 2013). Thus, melanocytes are likely targets of a noncytotoxic CD8+ T cell–mediated autoimmune response in psoriasis. According to the selective epidermal localization of melanocytes, a melanocyte-directed autoimmune response may explain why psoriatic inflammation is primarily confined to the skin.
Figure 2.
Melanocytes are targets of a noncytotoxic CD8+ T cell response in psoriasis lesions. (A and B) Representative immunohistologic images of CD8+ T cells (green) and melanocytes (red) stained for c-Kit (A) or MART-1 (B) in healthy skin (n = 5), nickel contact eczema (n = 5), and psoriasis (n = 23). Asterisks designate CD8+ T cells contacting melanocytes. Overlay of red and green shows as yellow and of red, green, and blue as white. Dashed lines indicate basal membrane. (C) Incidence of CD8+ T cells (left) and percentage of CD8+ T cells in contact with c-Kit+ melanocytes (right) in normal skin, nickel eczema, and psoriasis. Each dot represents one subject, and bars mark the median; *, P < 0.05; ***, P < 0.005; ****, P < 0.001; two tailed Mann-Whitney U test. (D) Percentage of CD8+ T cells in contact with c-Kit+ melanocytes in three HLA-C*06:02–negative and seven HLA-C*06:02–positive psoriasis patients. Bars indicate median. (E and F) CD8+ T cells (blue) polarizing lytic granules (Granzyme B: green; overlay with red: yellow; overlay with red and blue: white; see arrowheads) toward contact sites with c-Kit+ (E) or MART-1+ (F) melanocytes (red) in psoriasis. Data are representative of eight psoriasis lesions. (G) Staining for MART-1 (red) and cCASP3 (green) in normal skin, nickel eczema, and psoriasis (n = 3). Only keratinocytes in nickel eczema focally stained positive for cCASP3 (arrowheads). Dashed lines indicate basal membrane. Bars: (A and G) 40 µm; (B) 20 µm; (E and F) 5 µm.
HLA-C*06:02 mediates melanocyte-directed autoimmunity through autoantigen presentation
To identify a potential melanocyte autoantigen of the Vα3S1/Vβ13S1 TCR, we screened plasmid-encoded combinatorial nonamer peptide libraries (PECPLs; total library size: 4.75 × 108) for peptides that are recognized by this TCR in the context of HLA-C*06:02. Screening with a completely randomized PECPL or PECPLs with predefined library positions according to known HLA-C*06:02 anchor positions (Fig. 3 A; Falk et al., 1993; Dionne et al., 2004; Rasmussen et al., 2014) and newly identified TCR ligands recovered eight TCR peptides stimulating the Vα3S1/Vβ13S1-TCR hybridoma (Fig. 3 B). The mimotopes were remarkably similar by distinct residue preferences and shared Arg at positions P2 and P8, Leu at P9, and Arg or Leu at P7. Six mimotopes carried Arg at P5, whereas P1, P3, P4, and P6 exhibited greater diversity. This polyspecificity is consistent with the inherent property of TCRs to react with distinct, though similar peptide ligands (Birnbaum et al., 2014).
Bioinformatic searches against the human proteome and the transcriptome of 1205Lu cells did not identify proteins containing sequences identical to the mimotopes. We therefore used the convergent amino acid pattern to select 180 natural human peptides for testing as candidate antigens of the Vα3S1/Vβ13S1 TCR (not depicted). Six of them stimulated the Vα3S1/Vβ13S1-TCR hybridoma when cotransfected with HLA-C*06:02 into COS-7 cells (Fig. 3, C and D). All of them corresponded to the conserved amino acid motif of the mimotopes and contained Arg at P5 and P8, Arg or Leu at P7, and the HLA-C*06:02–anchor residues Arg at P2 and Leu at P9 (Fig. 3 C). Thus, the conserved amino acid pattern of the library mimotopes allowed for the identification of several HLA-C*06:02–restricted natural self-epitopes of the Vα3S1/Vβ13S1 TCR.
The antigenicity of full-length proteins differs from their peptide epitopes
To distinguish potential psoriatic autoantigens, we investigated whether the parent proteins of the candidate epitopes would activate the Vα3S1/Vβ13S1-TCR hybridoma, i.e., whether the epitopes would be generated from the full-length parent proteins by proteasomal degradation. Unlike the antigenic peptides, none of the corresponding full-length proteins activated the TCR hybridoma when coexpressed with HLA-C*06:02 in COS-7 cells or the human cell line, HEK293FT, although Western blot confirmed ectopic protein expression (not depicted). When overexpressed in genuinely stimulatory HLA-C*06:02–positive WM278 (Fig. 3 E) or 1205Lu cells (not depicted), however, one of the six parent proteins, ADAMTSL5, enhanced Vα3S1/Vβ13S1-TCR hybridoma activation substantially beyond the basal activation induced by vector-transfected cells. Conversely, ADAMTSL5 protein lost its ability for TCR hybridoma stimulation upon deletion (Del58–65) or alanine substitution (Ala58–65) of the peptide epitope when expressed in both HLA-C*06:02–positive WM278 (Fig. 3 F) and 1205Lu cells or HLA-C*06:02–negative WM9 cells cotransfected with HLA-C*06:02 (not depicted). Knockdown of ADAMTSL5 in WM278 cells diminished TCR hybridoma activation (Fig. 3, G and H). Thus, only ADAMTSL5 retained the antigenicity of the peptide epitope as a full-length protein in HLA-C*06:02–positive or HLA-C*06:02–transfected melanocytic target cells, corroborating its role as psoriatic autoantigen of the Vα3S1/Vβ13S1 TCR in melanocytes. These results further indicate that the number of potential autoantigens is probably much smaller than the broad TCR reactivity against different self-peptide ligands would predict (Siewert et al., 2012; Birnbaum et al., 2014), and it supports that processing of particular autoantigenic epitopes may be cell type dependent (Kniepert and Groettrup, 2014).
ADAMTSL5 is a melanocyte autoantigen in psoriasis
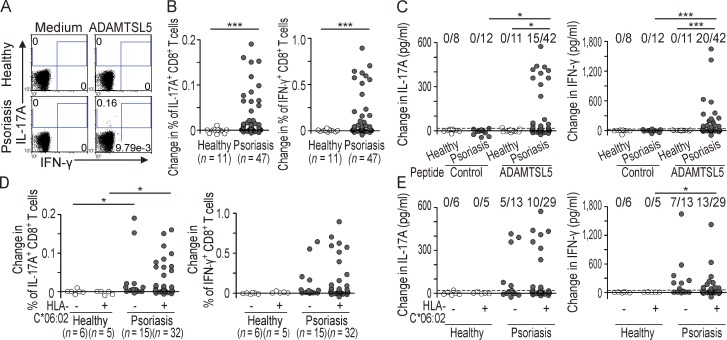
To examine whether ADAMTSL5 might represent a public autoantigen of CD8+ T cells in psoriasis, we tested the in vitro response of CD8+ T cells to a synthetic ADAMTSL5 peptide. As determined by multiparametric flow cytometry analysis, ADAMTSL5 stimulation of PBMCs markedly increased the frequencies of CD8+ T cells expressing IL-17A and IFN-γ in psoriasis patients (n = 47), whereas healthy individuals (n = 11) did not respond (each P < 0.005; Fig. 4, A and B). Analysis of culture supernatants confirmed that significantly higher proportions of psoriasis patients produced IL-17A (15/42, P < 0.05) and IFN-γ (20/42, P < 0.005) in response to ADAMTSL5 peptide stimulation compared with healthy individuals (Fig. 4 C). A control peptide lacking homology to human proteins had no effects on IL-17A and IFN-γ production, excluding unspecific peptide effects. Overall, 61.9% of psoriasis patients responded to ADAMTSL5 stimulation in terms of IL-17A and/or IFN-γ production. Given that IL-17A and IFN-γ are key mediators of psoriasis pathogenesis (Zaba et al., 2007), these responses confirmed a role of ADAMTL5 as autoantigen in a substantial proportion of psoriasis patients.
Figure 4.
ADAMTSL5 is a psoriasis autoantigen. (A) Representative flow cytometry dot plots for IL-17A– and IFN-γ–producing CD8+ T cells as the proportion of total CD8+ T cells in a healthy and psoriasis subject. (B and D) Change in the percentage of IL-17A– and IFN-γ–positive CD8+ T cells after ADAMTSL5 peptide stimulation of PBMCs from healthy and psoriasis subjects over medium control (B) and differentiated according to HLA-C*06:02 status (D). Data were assessed by multiparametric flow cytometry analysis after CD8 and intracellular cytokine staining and compared by two-tailed Mann-Whitney U test. Each dot represents one subject; *, P < 0.05; ***, P < 0.005. (C and E) Change in IL-17A and IFN-γ secretion of PBMCs stimulated with ADAMTSL5 or control peptide over medium control as evaluated by ELISA (C) and differentiated according to HLA-C*06:02 status (E). Dashed lines indicate the positive threshold. *, P < 0.05; ***, P < 0.005; two tailed Fisher’s exact test.
Approximately one third of psoriasis patients are HLA-C*06:02 negative (Table S1; Gudjonsson et al., 2003). PBMCs from both HLA-C*06:02–positive and –negative patients reacted similarly to ADAMTSL5 peptide stimulation (Fig. 4, D and E). A single autoantigenic epitope can be presented by different HLA molecules (Martin et al., 1991). The peptide-binding motifs of HLA-C*06:02 and several other HLA molecules overlap (Rasmussen et al., 2014). Similar CD8+ T cell reactivities against ADAMTSL5 and melanocytes in HLA-C*06:02–positive and –negative psoriasis patients support that HLA class I molecules other than HLA-C*06:02 may present ADAMTSL5 and promote melanocyte-specific autoimmunity as well. Thus, the specificity of the Vα3S1/Vβ13S1 TCR actually designates a common autoimmune pathway in psoriasis beyond HLA-C*06:02.
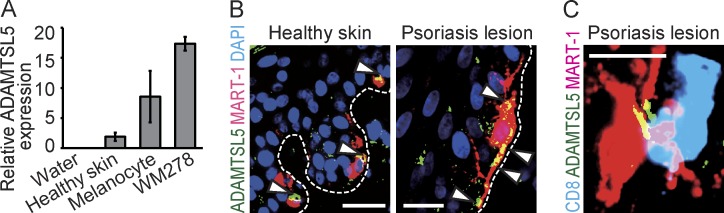
We finally examined ADAMTSL5 expression in skin and melanocytes. Melanocytes and WM278 cells highly expressed ADAMTSL5 mRNA compared with whole skin (Fig. 5 A). By immunohistology, we observed that in both healthy and lesional psoriatic epidermis, only melanocytes expressed ADAMTSL5 (Fig. 5 B). In psoriasis lesions, CD8+ T cells were seen in direct contact with ADAMTSL5-positive melanocytes (Fig. 5 C).
Figure 5.
ADAMTSL5 is selectively expressed by melanocytes in epidermis. (A) ADAMTSL5 mRNA expression in healthy skin (n = 2), primary melanocytes (n = 3), and WM278 cells was assessed by qPCR in triplicates and normalized to PBGD. Data are given as mean ± SD. (B) Immunostaining of ADAMTSL5 (green; overlay with red: yellow) and MART-1 (red) in healthy skin (n = 3) and psoriasis (n = 3). Dashed lines indicate basal membrane, and arrowheads indicate ADAMTSL5 expression by melanocytes. (C) Representative image of a CD8+ T cell (blue) contacting a melanocyte (red) expressing ADAMTSL5 (green; overlay with red: yellow) in psoriasis (n = 2). Bars: (B, left) 20 µm; (B [right] and C) 10 µm.
Overall, the autoreactivity of a TCR obtained directly from lesion-infiltrating CD8+ T cells reveals that HLA-C*06:02 may direct an autoimmune response against melanocytes in psoriasis. Identification of ADAMTSL5 as an HLA-C*06:02–restricted melanocytic autoantigen for the Vα3S1/Vβ13S1 TCR experimentally verifies that HLA-C*06:02 mediates melanocyte-specific autoimmunity through tissue-specific autoantigen presentation. Unveiling melanocytes, but not keratinocytes as previously hypothesized (Valdimarsson et al., 2009), as autoimmune target cells of the lesional psoriatic T cell response identifies a formerly unknown pathway of skin-specific psoriatic immune activation by which HLA-C*06:02 may predispose to psoriasis.
The autoimmune response against melanocytes does not necessarily exclude other cellular targets. Previous hypothesis-driven studies reported T cell responses against various self-peptides from the cathelicidin LL37 (Lande et al., 2014) or other keratinocyte proteins in psoriasis (Valdimarsson et al., 2009; Besgen et al., 2010). Because single TCRs can recognize hundreds of different peptides (Siewert et al., 2012; Birnbaum et al., 2014), HLA class I–restricted peptide autoantigens should be validated in the context of the parent proteins within the target cells. Here, we identify melanocytes as targets of the Vα3S1/Vβ13S1 TCR in an unbiased fashion and finally differentiate ADAMTSL5 as HLA-C*06:02–restricted melanocyte autoantigen from various other natural TCR peptide ligands. Thus, our data provide conclusive evidence that psoriasis is an autoimmune disease.
Beyond psoriasis, our approach allowed the unequivocal determination that HLA-based autoimmunity in humans arises through autoantigen presentation. Furthermore, this study provides experimental strategies for exploring T cell–mediated immune responses in autoimmunity, tumor immunity, or infections.
MATERIALS AND METHODS
Patients
Lesional biopsies were obtained from patients with psoriasis or nickel eczema patch test reactions, and normal skin specimens were obtained from discarded healthy skin of donors undergoing plastic surgery. Psoriasis patients with chronic plaque psoriasis were included (Table S1). Healthy donors were defined as persons without a history of psoriasis or other inflammatory or autoimmune diseases (five females and six males, median age 41.7 yr). Psoriasis patients under immunosuppressive treatments such as methotrexate, ciclosporin, or fumaric acid esters were excluded. There are no statistically significant differences in age and sex between groups. Patients and healthy individuals participated voluntarily and gave written informed consent. The study was performed in accordance with the Helsinki Declaration and approved by the Ethics Committee of the Ludwig-Maximilian-University, Munich.
Generation of Vα3S1/Vβ13S1-TCR CD8+ reporter T hybridoma
Identification of the matching Vα3S1 and Vβ13S1-TCR chains of a CD8+ T cell clone (Vα3S1-NN-Jα 45.1: CA TDAL YSGG, Vβ13S1-N(D)N-Jβ 1.1: CASSY SEGED EAFF; Arden nomenclature [Arden et al., 1995]) has been described previously (Kim et al., 2012). TCR hybridoma generation was performed as described previously (Seitz et al., 2006; Siewert et al., 2012). In brief, Vα and Vβ regions were cloned into expression plasmids pRSV-hygro (α chain) and pRSV-neo (β chain) using restriction sites SalI–PvuII or SalI–BIpI. The resulting plasmids were linearized (XmnI and NdeI, respectively) and electroporated into 58 α−β− T hybridoma cells. Functional clones were supertransfected with pLPCX-CD8α-IRES-β and pcDNA-NFAT-sGFP. TCR activation–induced NFAT-sGFP expression was determined by CD3 cross-linking with anti–mouse CD3 antibody (clone 17A2; eBioscience), flow cytometry, and fluorescence microscopy (AxioVert200M [Carl Zeiss], 520/35 BrightLine filter, Semrock, and 605/70 filter). Hybridoma batches were frequently recloned to minimize sporadic sGFP expression and decrease of activation rates that occur with prolonged culture. Clones with the highest frequencies of responding cells (usually between 30% and 60% NFAT-sGFP–positive cells after CD3 stimulation) were expanded in T hybridoma medium (see “Primary cells and cell lines” section). The different proportions of activatable hybridoma cells in different batches contribute to a certain interexperimental quantitative variability in activation rates without affecting specificity of TCR hybridoma activation (Siewert et al., 2012).
Construction of PECPLs
The nonameric PECPLs #1–3 were prepared as described previously (Siewert et al., 2012). Library designs are shown in Fig. 3 A. Sequences for all oligonucleotide primers are listed in Table S2.
Identification of Vα3S1/Vβ13S1-TCR mimotopes
PECPL screening was performed as described previously (Siewert et al., 2012). COS-7 cells were cotransfected with PECPLs and HLA-C*06:02 and co-cultured with Vα3S1/Vβ13S1-TCR hybridoma cells. After 16 h, COS-7 cells in close contact to fluorescent hybridoma cells were isolated and library peptides were amplified by nested PCR. PCR products were cloned into pcDNA.3.1D/V5-His-TOPO and transformed into Escherichia coli. The mimotope-enriched library plasmids were cotransfected with pRSV-HLA-C*06:02 into COS-7 cells, and the mimotope-containing plasmid was isolated by subcloning and sequencing.
Transcriptome analysis of 1205Lu cells
Total RNA was prepared from 6 × 106 1205Lu cells using 1.5 ml TRIzol. RNA was used for library generation after assessment for purity by UV-VIS spectrometry (NanoDrop) and for integrity by Bioanalyzer 2100 (Agilent Technologies). RNA-seq libraries were prepared from 100 ng of total quality-controlled RNA with a strand-specific protocol (RNA-seq complete kit, NuGEN). In brief, RNA was reverse transcribed with a reduced set of hexamer primers, avoiding excessive representation of rRNA in the cDNA. Second strand cDNA synthesis was performed in the presence of dUTP. After ultrasonic cDNA fragmentation, end repair Illumina-compatible adapters were ligated. Adapters contained uracil in one strand, allowing complete digestion of the second strand–derived DNA. After strand selection, the libraries were amplified, assessed for correct insert size on the Agilent Technologies Bioanalyzer, and diluted to 10 nM. Barcoded libraries were mixed in equimolar amounts and sequenced on a total of three lanes on a Genome Analyser IIx (Illumina) in single-read mode with a read length of 84 bp. Raw reads were demultiplexed by sorting for and simultaneously trimming a leading 4-bp barcode sequence at the 5′-end of each read. Obtained 80-bp reads were mapped to the hg19 release of the human genome using spliced-read mapper Tophat and the UCSC gene annotation. Mapped reads overlapping with known genes were counted with HTseq count, available from the developers of DESeq.
Identification of natural candidate peptide antigens based on mimotope sequences
Two different search strategies were used to identify human candidate peptide epitopes based on the conserved amino acid motifs of the mimotopes. We used two tools from the European Molecular Biology Open Software Suite (EMBOSS); PROPHECY was used to create a frequency matrix from sequences of positively tested antigenic peptides. With this matrix and the PROFIT tool, the taxa-specific Homo sapiens [9606] UniProt database was scanned. The list of results was further refined with information on anchor amino acids of HLA-C*06:02 ligands (Falk et al., 1993; Dionne et al., 2004; SYFPEITHI database). The matrix was constantly adjusted according to newly isolated mimotopes or tested candidate antigen peptides.
1205Lu transcriptome data were used for a selective search in melanocytic proteins. The MOTIF Search web server was searched for human genes in the “KEGG Genes” dataset containing peptide motifs that were defined according to mimotope sequences and general HLA-C*06:02 anchor positions. The motifs used for the search were (encoded in PROSITE format): R-X(4,5)-[RL]-R-[LIVY], R-X(5)-R-[LFMIVY], R-X(4)-[RLFS]-R-[LFMIVY], [AFGIRSHM]-R-[ACHNPQSTWF]-[ASRVWYC]-[NRQT]-[STVYA]-[LRFS]-R-[LFM], R-[ACHNPQSTWF]-[ASRVWYC]-[NRQT]-[STVYA]-[LRFS]-R-[LFM], and R-X-X-[NRQT]-[STVYA]-[LRFS]-R-[LFMIVY].
Cloning of HLA-C*06:02, candidate peptides, full-length proteins, and mutated ADAMTSL5
HLA-C*06:02 was amplified by PCR from cDNA of an HLA-C*06:02–positive psoriasis patient and cloned into pRSV5-neo via EcoRI and XhoI restriction sites. pRSV–HLA-A*02:01 has been described previously (Siewert et al., 2012).
For expression of short peptides, forward and reverse oligonucleotides were annealed and ligated into pcDNA3.1D/V5-His-TOPO using the Directional TOPO Expression kit (Invitrogen). Forward primers carried a 5′-CACCATG overhang and a stop codon at the 3′-end of the target sequence.
Open reading frames of THEM6 (UniProt accession no. Q8WUY1), RASSF10 (A6NK89), and C2CD4B (A6NLJ0) were PCR-amplified from 1205Lu cDNA using Taq and Pwo polymerases (both from Roche). Because of limitations in protein size for overexpression, we restricted cloning of ASH1L (Q9NR48) to a partial protein fragment corresponding to amino acids 2074–2564, comprising the ASH1L catalytic domain and the BROMO domain. Clone IRCM10B06 (BioScience) was used as template for amplification of the Hepacam (Q14CZ8) ORF. An ADAMTSL5 (NCBI Protein accession no. NP_998769) template was provided by S.S. Apte (Lerner Research Institute, Cleveland Clinic, Cleveland, OH; Bader et al., 2012). C-terminal stop codons were omitted in all constructs yielding a vector-encoded C-terminal V5-His6-tag. PCR products were cloned into pcDNA3.1D/V5-His-TOPO and confirmed by sequencing.
Internal reverse primers were designed to introduce deletion or alanine substitutions of ADAMTSL5 at amino acid positions 58–65. Mutations were introduced by PCR in combination with the ADAMTSL5 forward primer using Taq polymerase. After blunting, resulting DNA fragments were used as forward primers in a second PCR in combination with the ADAMTSL5 reverse primer. After a second blunting reaction, resulting DNA was cloned into pcDNA3.1D/V5-His-TOPO.
Western blotting
Cell lysates were separated by 10% SDS-PAGE and transferred onto nitrocellulose membranes (Schleicher & Schuell) by semi-dry electroblotting. Expression of V5-His6–tagged proteins was detected using an anti–V5-AP antibody. HLA-C expression was analyzed using an HLA-C antibody in combination with AP-conjugated anti–mouse IgG secondary antibody. Western blot for β-actin served as loading control. The Alkaline Phosphatase Conjugate Substrate kit (Bio-Rad Laboratories) was used for colorimetric detection.
Primary cells and cell lines
Primary human melanocytes were prepared as described previously (Hsu and Herlyn, 1996). Skin samples were incubated with 2.5 U/ml dispase (grade II, Boehringer Mannheim) overnight at 4°C. Epidermis was removed from dermis and incubated for 5 min at 37°C in HBSS without Ca2+ and Mg2+ containing 0.25% trypsin and 0.1% EDTA. Epidermal single-cell suspensions were expanded in melanocyte growth medium M2 (PromoCell). Primary cultured melanocytes were stained with p75NTR antibody and anti–mouse secondary antibody conjugated with Alexa Fluor 597 overnight.
Human melanoma cell lines, WM9, 1205Lu (NCBI BioSample accession no. SAMN03471797), WM1232, and WM278 (SAMN03471796) were originally obtained from the Wistar Institute. They were cultured in 2% TU medium containing MCDB153, 20% Leibovitz’s L15, 5 µg/ml insulin, 2% FCS, and 1.68 mM CaCl2. Human neonatal epidermal keratinocytes (Invitrogen) were cultured in EpiLife medium supplemented with EpiLife Defined Growth Supplement (Thermo Fisher Scientific). COS-7, HEK293FT, HaCaT (NCBI EST accession no. LIBEST_003731) and A431 (LIBEST_000407) cells were cultured in DMEM supplemented with 100 U/ml penicillin and 100 µg/ml streptomycin, 1 mM sodium pyruvate, 1× MEM nonessential amino acids, 10% FCS (Biochrom), and 10 µg/ml ciprofloxacin. HEK293FT medium additionally contained 500 µg/ml G-418.
Vα3S1/Vβ13S1-TCR hybridoma cells were cultured in RPMI 1640 containing 10% FCS, 100 U/ml penicillin, 100 µg/ml streptomycin, 1 mM sodium pyruvate, 1× MEM nonessential amino acids, and 10 µg/ml ciprofloxacin, supplemented with selection antibiotics G418 (1.5 mg/ml), hygromycin (300 µg/ml), puromycin (1 µg/ml), and blasticidin (3 µg/ml). For co-culture experiments, TCR hybridoma cells were pelleted and resuspended in hybridoma growth medium without selection antibiotics before addition to antigen-presenting cells.
Vα3S1/Vβ13S1-TCR hybridoma activation assays
sGFP induction in Vα3S1/Vβ13S1-TCR hybridoma cells was examined after 24-h co-culture with antigen-presenting cells by UV-fluorescence microscopy and/or flow cytometry. As controls, Vα3S1/Vβ13S1-TCR hybridoma cells were cultured in anti–mouse CD3 antibody–coated (clone 17A2, 2 µg/ml in PBS; eBioscience) culture plates. The percentage of NFAT-sGFP+ cells was assessed by flow cytometry and normalized to the CD3 activation value in the same experiment. pRSV-GFP or pcDNA-GFP served as transfection controls.
To increase HLA-C surface expression, 100 ng/ml IFN-γ was added 24 h before co-cultivation with TCR hybridoma cells. Anti–human HLA class I antibody (clone W6/32, LEAF grade, 1.5 µg/ml; BioLegend) was used to block HLA class I–restricted TCR hybridoma activation.
1205Lu and WM278 were seeded in 24-well plates in TU 2% medium at densities of 2.5 × 104 or 5 × 104 cells/well, respectively. HLA-C*06:02–negative cell line WM9 or WM1232 (105 cells/well) was transfected with 250 ng pRSV–HLA-C*06:02 or pRSV–HLA-A*02:01 using FuGENE HD reagent (Promega) according to the manufacturer’s instructions.
Plasmid-encoded peptides were cotransfected with pRSV–HLA-C*06:02 (250 ng each) into COS-7 or HEK293FT using FuGENE. After 24 h, medium was replaced with fresh medium containing Vα3S1/Vβ13S1-TCR hybridoma cells.
For stimulation of Vα3S1/Vβ13S1-TCR hybridoma cells by ectopic expression of full-length proteins, antigen-presenting cell lines were transfected with 250 ng expression plasmid, as described above for 1205Lu and WM278 cells. 100 ng/ml IFN-γ was added to HLA-C*06:02–positive melanocytic cell lines. HLA-C*06:02–negative antigen-presenting cell lines were cotransfected with pRSV–HLA-C*06:02.
ADAMTSL5 knockdown
ADAMTSL5-1 siRNA was designed and purchased from QIAGEN. ADAMTSL5-2 siRNA and control siRNAs 1 and 2 were obtained from MWG Eurofins. siRNA target sequences are given in Table S2. 24 h after siRNA transfection of WM278 cells, 100 ng/ml IFN-γ was added. 24 h later, medium was replaced and hybridoma cells were added and co-cultured for 24 h.
For validation of ADAMTSL5 knockdown, ADAMTSL5 mRNA levels were determined by real-time quantitative PCR (qPCR) in triplicates using Light Cycler 2.0 (Roche). Porphobilinogen deaminase (PBGD) mRNA was used as an internal standard.
Immunofluorescence staining of paraffin sections
Sections (5 µm) from formalin-fixed and paraffin-embedded tissue samples were cut on adhesive glass slides (SuperFrost plus; Menzel-Glaeser), dewaxed, and rehydrated. Heat-induced antigen retrieval used Tris-EDTA buffer (10 mM Tris Base, 1 mM EDTA, and 0.05% Tween 20, pH 9.0) at 120°C for 15 min. Sections were incubated with primary antibody or isotype controls at 4°C for 12–60 h, washed, and incubated with fluorescence-conjugated secondary antibody for 90 min. Nuclei were counterstained with DAPI. ADAMTSL5-blocking peptide was added at 5 ng/ml.
For multiple stainings, primary antibodies were used in conditions established in single-color stainings. For triple staining, anti–Granzyme B antibody was stained using the tyramide signal amplification method (TSA; PerkinElmer). All antibodies are listed in Table S3. Epidermal CD8+ T cells were defined as reported previously (Bovenschen et al., 2005).
Microscopic analysis was performed on an Axio Observer microscope (Carl Zeiss) with a Chroma ET filter-set and a CoolSNAP-HQ2 digital camera system (Photometrics). Images were merged using Basic MetaMorph Imaging Software (Visitron).
Semiquantification of CD8+ T cell to melanocyte contacts
Epidermal areas of skin sections were completely photodocumented at a 100-fold magnification with GFP, Texas Red, and DAPI filters, respectively (Visitron), and images were merged. Epidermal segments were evaluated in each photographic image using Fiji/ImageJ software (National Institutes of Health). Stained cells and direct cell contacts were counted in each overlay independently by two authors. Resulting median values in each individual were used for statistical analyses.
PBMC peptide stimulation, intracellular cytokine staining, and ELISA
PBMCs were separated by Ficoll density gradient centrifugation. Freshly isolated PBMCs were seeded to 96-well flat-bottom plates (106 cells/well) and cultured in RPMI 1640 medium supplemented with 5 IU/ml IL-2 and 10% human AB serum. Highly purified ADAMTSL5 peptide (VRSRRCLRL, purity >95%; Thermo Fisher Scientific) and an unrelated peptide (ELQGLKDD) lacking homology to human proteins were used at 10 ng/ml.
Intracellular cytokine staining was performed as described previously (Fujii et al., 2011). After 48 h of peptide stimulation, monensin (Golgi stop [BD], 0.35 µl for 200 µl culture medium) was added for 5 h. Cells were surface stained for CD8, fixed, and permeabilized in fixation buffer (eBioscience) and intracellularly stained using antibodies against IL-17A and IFN-γ. Data were analyzed by FlowJo software 887 (Tree Star). Lymphocyte gates were defined using SSC and FSC channels. Positive/negative cut-off levels for IFN-γ and IL-17A were defined by isotype control stainings of CD8+ T cells in unstimulated samples from healthy donors in each experiment.
To determine cytokine secretion, PBMCs were stimulated with peptides for 48 h as described above for intracellular cytokine staining. Culture supernatants were harvested, and IFN-γ and IL-17A were quantified in triplicates using ELISA kits (Mabtech). During the experiments, the investigator was blinded for the sample group allocation. Thresholds for positive cytokine induction by ADAMTSL5 peptide are set at mean + 3SD of healthy control samples.
HLA typing
HLA haplotypes were determined by sequence-based typing at the Laboratory for Immunogenetics and Molecular Diagnostics, University of Munich. In select experiments, HLA-C*06.02 typing was performed by PCR restriction fragment length polymorphism analysis as described previously (Tazi Ahnini et al., 1999).
Statistical analysis
Kruskal-Wallis H-test was used for multiple comparisons, and Bonferroni correction was applied. There is more than one group without normal distributions in each comparison (Shapiro-Wilk W test). Accordingly, when the p-value of Kruskal-Wallis H-test was significant, two-group comparison was performed using the Mann-Whitney U test. Different proportions in the two groups were compared using Fisher’s exact test. Two-tailed P < 0.05 was considered significant. All statistical analyses were performed using GraphPad Software version 4 and R software. Sample size was determined based on preliminary data (mean and variation) and previous publications, as well as observed effect sizes. No samples were excluded from analysis.
Online supplemental material
Table S1, included as a separate Excel file, provides patients’ data and HLA-C*06:02 status. Table S2, included as a separate Excel file, provides primer and siRNA sequences. Antibodies are listed in Table S3, included as a separate Excel file. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20151093/DC1.
Supplementary Material
ACKNOWLEDGMENTS
We thank Mr. Adrian Galinski, Mr. Sebastian Harrasser, Ms. Ursula Puchta, and Ms. Marija Rozman for their support and Prof. Ulla Knaus and Mr. Takanobu Tagawa for helpful discussion. We thank Prof. Suneel S. Apte for the ADAMTSL5 plasmid.
This project was supported by the Deutsche Forschungsgemeinschaft, grants Pr 241/4-1 and CRC-128-A5.
The Ludwig-Maximilian-University filed a patent application for the peptides with J.C. Prinz and K. Dornmair as inventors. The authors declare no additional competing financial interests.
Footnotes
Abbreviations used:
- PBGD
- porphobilinogen deaminase
- PECPL
- plasmid-encoded combinatorial nonamer peptide library
- qPCR
- quantitative PCR
References
- Arden, B., Clark S.P., Kabelitz D., and Mak T.W.. 1995. Human T-cell receptor variable gene segment families. Immunogenetics. 42:455–500. [DOI] [PubMed] [Google Scholar]
- Bader, H.L., Wang L.W., Ho J.C., Tran T., Holden P., Fitzgerald J., Atit R.P., Reinhardt D.P., and Apte S.S.. 2012. A disintegrin-like and metalloprotease domain containing thrombospondin type 1 motif-like 5 (ADAMTSL5) is a novel fibrillin-1-, fibrillin-2-, and heparin-binding member of the ADAMTS superfamily containing a netrin-like module. Matrix Biol. 31:398–411. 10.1016/j.matbio.2012.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besgen, P., Trommler P., Vollmer S., and Prinz J.C.. 2010. Ezrin, maspin, peroxiredoxin 2, and heat shock protein 27: potential targets of a streptococcal-induced autoimmune response in psoriasis. J. Immunol. 184:5392–5402. 10.4049/jimmunol.0903520 [DOI] [PubMed] [Google Scholar]
- Birnbaum, M.E., Mendoza J.L., Sethi D.K., Dong S., Glanville J., Dobbins J., Ozkan E., Davis M.M., Wucherpfennig K.W., and Garcia K.C.. 2014. Deconstructing the peptide-MHC specificity of T cell recognition. Cell. 157:1073–1087. 10.1016/j.cell.2014.03.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovenschen, H.J., Seyger M.M., and Van de Kerkhof P.C.. 2005. Plaque psoriasis vs. atopic dermatitis and lichen planus: a comparison for lesional T-cell subsets, epidermal proliferation and differentiation. Br. J. Dermatol. 153:72–78. 10.1111/j.1365-2133.2005.06538.x [DOI] [PubMed] [Google Scholar]
- Chang, J.C., Smith L.R., Froning K.J., Schwabe B.J., Laxer J.A., Caralli L.L., Kurland H.H., Karasek M.A., Wilkinson D.I., Carlo D.J., et al. 1994. CD8+ T cells in psoriatic lesions preferentially use T-cell receptor V beta 3 and/or V beta 13.1 genes. Proc. Natl. Acad. Sci. USA. 91:9282–9286. 10.1073/pnas.91.20.9282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrad, C., Boyman O., Tonel G., Tun-Kyi A., Laggner U., de Fougerolles A., Kotelianski V., Gardner H., and Nestle F.O.. 2007. α1β1 integrin is crucial for accumulation of epidermal T cells and the development of psoriasis. Nat. Med. 13:836–842. 10.1038/nm1605 [DOI] [PubMed] [Google Scholar]
- Dionne, S.O., Lake D.F., Grimes W.J., and Smith M.H.. 2004. Identification of HLA-Cw6.02 and HLA-Cw7.01 allele-specific binding motifs by screening synthetic peptide libraries. Immunogenetics. 56:391–398. 10.1007/s00251-004-0710-1 [DOI] [PubMed] [Google Scholar]
- Falk, K., Rötzschke O., Grahovac B., Schendel D., Stevanović S., Gnau V., Jung G., Strominger J.L., and Rammensee H.G.. 1993. Allele-specific peptide ligand motifs of HLA-C molecules. Proc. Natl. Acad. Sci. USA. 90:12005–12009. 10.1073/pnas.90.24.12005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujii, H., Arakawa A., Kitoh A., Miyara M., Kato M., Kore-eda S., Sakaguchi S., Miyachi Y., Tanioka M., and Ono M.. 2011. Perturbations of both nonregulatory and regulatory FOXP3+ T cells in patients with malignant melanoma. Br. J. Dermatol. 164:1052–1060. 10.1111/j.1365-2133.2010.10199.x [DOI] [PubMed] [Google Scholar]
- Griffiths, C.E., and Barker J.N.. 2007. Pathogenesis and clinical features of psoriasis. Lancet. 370:263–271. 10.1016/S0140-6736(07)61128-3 [DOI] [PubMed] [Google Scholar]
- Gudjonsson, J.E., Karason A., Antonsdottir A., Runarsdottir E.H., Hauksson V.B., Upmanyu R., Gulcher J., Stefansson K., and Valdimarsson H.. 2003. Psoriasis patients who are homozygous for the HLA-Cw*0602 allele have a 2.5-fold increased risk of developing psoriasis compared with Cw6 heterozygotes. Br. J. Dermatol. 148:233–235. 10.1046/j.1365-2133.2003.05115.x [DOI] [PubMed] [Google Scholar]
- Hsu, M.Y., and Herlyn M.. 1996. Cultivation of normal human epidermal melanocytes. Methods Mol. Med. 2:9–20. [DOI] [PubMed] [Google Scholar]
- Kent, S.C., Chen Y., Bregoli L., Clemmings S.M., Kenyon N.S., Ricordi C., Hering B.J., and Hafler D.A.. 2005. Expanded T cells from pancreatic lymph nodes of type 1 diabetic subjects recognize an insulin epitope. Nature. 435:224–228. 10.1038/nature03625 [DOI] [PubMed] [Google Scholar]
- Kim, S.M., Bhonsle L., Besgen P., Nickel J., Backes A., Held K., Vollmer S., Dornmair K., and Prinz J.C.. 2012. Analysis of the paired TCR α- and β-chains of single human T cells. PLoS One. 7:e37338. 10.1371/journal.pone.0037338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knickelbein, J.E., Khanna K.M., Yee M.B., Baty C.J., Kinchington P.R., and Hendricks R.L.. 2008. Noncytotoxic lytic granule-mediated CD8+ T cell inhibition of HSV-1 reactivation from neuronal latency. Science. 322:268–271. 10.1126/science.1164164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kniepert, A., and Groettrup M.. 2014. The unique functions of tissue-specific proteasomes. Trends Biochem. Sci. 39:17–24. 10.1016/j.tibs.2013.10.004 [DOI] [PubMed] [Google Scholar]
- Lande, R., Botti E., Jandus C., Dojcinovic D., Fanelli G., Conrad C., Chamilos G., Feldmeyer L., Marinari B., Chon S., et al. 2014. The antimicrobial peptide LL37 is a T-cell autoantigen in psoriasis. Nat. Commun. 5:5621. 10.1038/ncomms6621 [DOI] [PubMed] [Google Scholar]
- Lowes, M.A., Bowcock A.M., and Krueger J.G.. 2007. Pathogenesis and therapy of psoriasis. Nature. 445:866–873. 10.1038/nature05663 [DOI] [PubMed] [Google Scholar]
- Martin, R., Howell M.D., Jaraquemada D., Flerlage M., Richert J., Brostoff S., Long E.O., McFarlin D.E., and McFarland H.F.. 1991. A myelin basic protein peptide is recognized by cytotoxic T cells in the context of four HLA-DR types associated with multiple sclerosis. J. Exp. Med. 173:19–24. 10.1084/jem.173.1.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCutcheon, J.A., Gumperz J., Smith K.D., Lutz C.T., and Parham P.. 1995. Low HLA-C expression at cell surfaces correlates with increased turnover of heavy chain mRNA. J. Exp. Med. 181:2085–2095. 10.1084/jem.181.6.2085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair, R.P., Stuart P.E., Nistor I., Hiremagalore R., Chia N.V., Jenisch S., Weichenthal M., Abecasis G.R., Lim H.W., Christophers E., et al. 2006. Sequence and haplotype analysis supports HLA-C as the psoriasis susceptibility 1 gene. Am. J. Hum. Genet. 78:827–851. 10.1086/503821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter, A.G., and Jänicke R.U.. 1999. Emerging roles of caspase-3 in apoptosis. Cell Death Differ. 6:99–104. 10.1038/sj.cdd.4400476 [DOI] [PubMed] [Google Scholar]
- Rasmussen, M., Harndahl M., Stryhn A., Boucherma R., Nielsen L.L., Lemonnier F.A., Nielsen M., and Buus S.. 2014. Uncovering the peptide-binding specificities of HLA-C: a general strategy to determine the specificity of any MHC class I molecule. J. Immunol. 193:4790–4802. 10.4049/jimmunol.1401689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seitz, S., Schneider C.K., Malotka J., Nong X., Engel A.G., Wekerle H., Hohlfeld R., and Dornmair K.. 2006. Reconstitution of paired T cell receptor α- and β-chains from microdissected single cells of human inflammatory tissues. Proc. Natl. Acad. Sci. USA. 103:12057–12062. 10.1073/pnas.0604247103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siewert, K., Malotka J., Kawakami N., Wekerle H., Hohlfeld R., and Dornmair K.. 2012. Unbiased identification of target antigens of CD8+ T cells with combinatorial libraries coding for short peptides. Nat. Med. 18:824–828. 10.1038/nm.2720 [DOI] [PubMed] [Google Scholar]
- Tazi Ahnini, R., Camp N.J., Cork M.J., Mee J.B., Keohane S.G., Duff G.W., and di Giovine F.S.. 1999. Novel genetic association between the corneodesmosin (MHC S) gene and susceptibility to psoriasis. Hum. Mol. Genet. 8:1135–1140. 10.1093/hmg/8.6.1135 [DOI] [PubMed] [Google Scholar]
- Valdimarsson, H., Thorleifsdottir R.H., Sigurdardottir S.L., Gudjonsson J.E., and Johnston A.. 2009. Psoriasis—as an autoimmune disease caused by molecular mimicry. Trends Immunol. 30:494–501. 10.1016/j.it.2009.07.008 [DOI] [PubMed] [Google Scholar]
- Wang, C.Q., Akalu Y.T., Suarez-Farinas M., Gonzalez J., Mitsui H., Lowes M.A., Orlow S.J., Manga P., and Krueger J.G.. 2013. IL-17 and TNF synergistically modulate cytokine expression while suppressing melanogenesis: potential relevance to psoriasis. J. Invest. Dermatol. 133:2741–2752. 10.1038/jid.2013.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaba, L.C., Cardinale I., Gilleaudeau P., Sullivan-Whalen M., Suárez-Fariñas M., Fuentes-Duculan J., Novitskaya I., Khatcherian A., Bluth M.J., Lowes M.A., and Krueger J.G.. 2007. Amelioration of epidermal hyperplasia by TNF inhibition is associated with reduced Th17 responses. J. Exp. Med. 204:3183–3194. (published erratum appears in J. Exp. Med. 2008. 205:1941) 10.1084/jem.20071094 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.