Abstract
Unplanned start on dialysis remains a major problem for the dialysis community worldwide. Late-referred patients with end-stage renal disease (ESRD) and urgent need for dialysis are overrepresented among older people. These patients are particularly likely to be started on in-center hemodialysis (HD), with a temporary vascular access known to be associated with excess mortality and increased risks of potentially lethal complications such as bacteremia and central venous thrombosis or stenosis.
The present paper describes in detail our program for unplanned start on automated peritoneal dialysis (APD) right after PD catheter implantation and summarizes our experiences with the program so far. Compared with planned start on PD after at least 2 weeks of break-in between PD catheter implantation and initiation of dialysis, unplanned start may be associated with a slight increased risk of mechanical complications but apparently no detrimental effect on mortality, peritonitis-free survival, or PD technique survival.
In our opinion and experience, the risk of serious complications associated with the implantation and immediate use of a PD catheter is less than the risk of complications associated with unplanned start on HD with a temporary central venous catheter (CVC). Unplanned start on APD is a gentle, safe, and feasible alternative to unplanned start on HD with a temporary CVC that is also valid for the late-referred older patient with ESRD and urgent need for dialysis.
Keywords: Peritoneal dialysis, elderly, catheter insertion, acute start
Unplanned start on chronic dialysis due to late referral or unexpected deterioration of residual renal function remains a major problem worldwide. There is no scientific consensus on a strict definition of unplanned start on dialysis in the literature. In Denmark, approximately 30% of all incident patients starting dialysis during 2013 were late-referred (< 112 days before initiation of dialysis) and 45% started unplanned dialysis (defined as using a temporary tunnelled [if arteriovenous fistula planned] or untunnelled central venous catheter [CVC] for hemodialyis [HD] or a peritoneal dialysis [PD] catheter with less than 7 days of peritoneal rest after PD catheter implantation for PD) (1). In the US, more than 80% of patients who starts HD start with a CVC (2). Late-referred patients with urgent need for dialysis, often referred to as “parachute” or “crashlanders,” are overrepresented among the older end-stage renal disease (ESRD) population and are particularly likely to be started on HD with a temporary CVC. Unplanned start on HD is associated with excess mortality, an increased risk of infectious (e.g. bacteremia) or mechanical (e.g. central venous stenosis and thrombosis leading to failure of vascular access) complications, hemodynamic instability during the first HD sessions, post-treatment fatigue or disequilibrium, and subsequent need for frequent and prolonged hospital admissions. Despite this, in-center HD using a temporary CVC is still the default way to deliver renal replacement therapy in the unplanned and urgent setting. Finally, such patients, once started on in-center HD, are less likely to be transferred to a home-based treatment later on.
The generally held perception that PD catheter insertion should be performed at least 2 weeks before starting PD is based on evidence level C. In the European Best Practise Guidelines it is added that small dialysate volume in the supine position can be used if dialysis is required during the break-in period (3). To give the crashlanders a real choice between dialysis modalities, we established a program for unplanned start on PD right after PD catheter implantation 15 years ago (4–5). The present paper summarizes our experience with this program so far.
Decision-Making
For the late-referred crashlander without any previous nephrologic care, education, or preparation and with urgent need for initiation of dialysis within hours or days, the decision of future dialysis modality is obviously very difficult. This is particularly evident for patients with advanced age, a heavy burden of comorbidities, and severe uremic intoxication as additional factors. However, even in this scenario, it is our experience that it is possible to give unbiased dialysis information to the patient and relatives, thereby giving them a real choice of modality selection. The desire for independence, a feeling of confidence, and a home-based treatment is often decisive in the patient's final choice (6).
In our program, severe hypertension (diastolic blood pressure > 120 mmHg), severe overhydration with signs of pulmonary edema, severe hyperkalemia (s-K+ > 6.5 mmol/L), signs of uremic pericarditis or colitis are all considered contra-indications for unplanned PD, and HD is then preferred (4–5).
Unplanned Automated Peritoneal Dialysis (APD)
We use coiled, double-cuff Tenckhoff PD catheters implanted using a mini-laparotomy and local anesthesia. The surgeons use exactly the same procedure in both the planned and the unplanned setting, placing the inner cuff deep to the rectus sheath and fixed with a purse suture. In our experience, the risk of leakage is predominantly related to the dwell volume used right after the implantation, and, using the dwell volumes given in Table 1, it is rarely seen. One gram of vancomycin is given intravenously preoperatively as prophylaxis. There is no evidence that one type of PD catheter or implantation technique is superior to another. For each center starting unplanned PD, we recommend the use of the implantation technique and catheters they are most experienced in.
TABLE 1.
Standard Prescription for Unplanned Automated Peritoneal Dialysis*
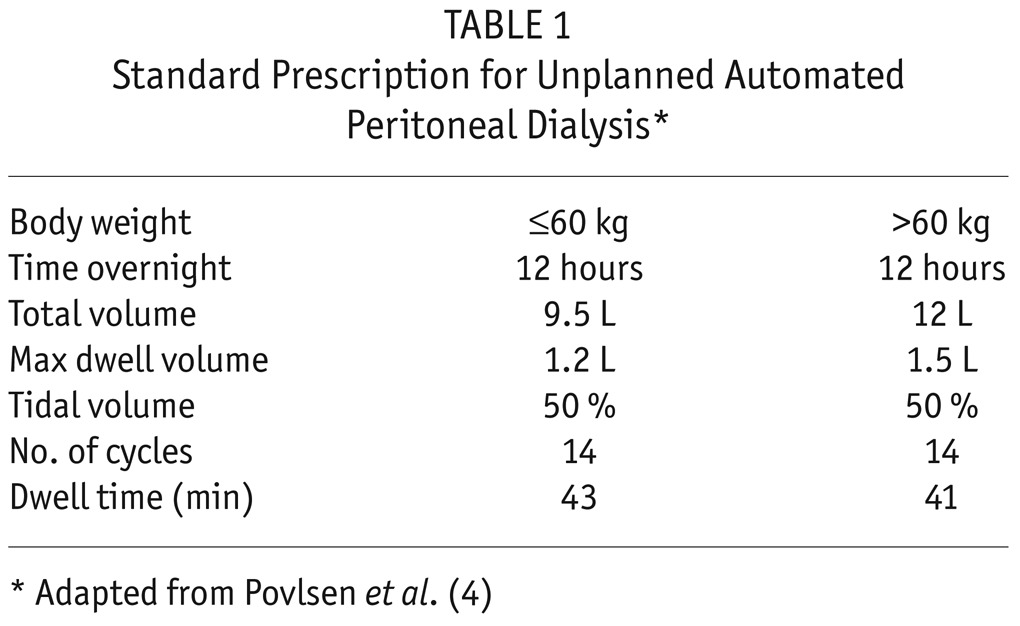
Unplanned APD (HomeChoice cyclers; Baxter Healthcare Corporation, Deerfield, IL, USA) is initiated right after PD catheter implantation using a standard prescription for 12-hour overnight treatment in the supine position as described previously (4) (Table 1). Using this prescription, the cyclers will deliver 14 cycles per session with a dwell time of approximately 45 minutes, which ensures adequate small solute clearance and fluid removal. The cyclers are pre-programmed with a chip (ProCard; Baxter Healthcare Corporation, Deerfield, IL, USA) to make it simple and to ensure that the youngest doctor on duty can prescribe the treatment and the youngest nurse on duty can carry it out. Patients are instructed to stay in bed in the supine position during the overnight treatment. The low tidal volume used is chosen to avoid too many alarms during the first night of treatment, and is gradually increased to 75 – 85% during the first week of treatment. Also in the unplanned setting, it is important to remember bowel preparation to avoid constipation after catheter implantation. After 8 – 14 days of treatment, patients are converted to a standard 8 hours or an individualized APD program ± wet day. During the stay in hospital, the autonomous patients are trained for PD by our expert PD nurses. In our program, approximately half of the patients over 65 years of age need assistance to carry out PD at home. For these patients, the assistants are trained to visit the patients at home after discharge from hospital: a longer visit in the morning to disconnect the patient from the cycler and to set up the cycler for the next night followed by a short visit in the evening to connect the patient to the cycler (5,7). However, some of these patients become autonomous later on as they become more confident with the treatment (7).
Obviously, starting older people on unplanned PD requires a prolonged stay at hospital. This should, however, be compared with the number of hospital days spent for creation of and management of complications to vascular access for HD, which may be particularly difficult in older patients with comorbidity including peripheral vascular disease. In a French study comparing patients starting unplanned PD or unplanned HD there was no difference in duration of the initial hospital stay (12). One way to reduce the number of days needed in hospital might be intermittent PD, where the patients are admitted for 1 overnight APD session 3 times weekly during the first 2 weeks after PD catheter implantation (13). Yet another way practised in some centers is to discharge the patients after a few days of unplanned APD and continue the treatment as daily APD in the outpatient clinic while the patient is trained to become autonomous.
Based on this standard prescription for unplanned PD, we observed a steady and gentle decrease in plasma urea reaching a plateau after 1 week of treatment without any of the patients having suffered from disequilibrium. Hyperkalemia and metabolic acidosis was eliminated after 1 or 2 sessions (8).
Complications
Initially, we reported that unplanned start on PD may be associated with an increased risk of mechanical complications (leakage or dysfunction due to migration, clots, or omental wrapping, resulting in surgical replacement of the PD catheter) but apparently no detrimental effect on mortality, PD technique failure, or risk of infectious complications (4–5). This has recently been confirmed in a much larger Chinese study (9) including 657 patients divided into 3 groups according to the length of the break-in period (≤ 7 days, 8 – 14 days, and > 14 days) between catheter implantation and initiation of PD. They reported that the group with a break-in period ≤ 7 days had a statistically significantly higher incidence of mechanical complications compared with the group with a break-in period > 14 days during the first 6 months of PD. However, the risk was as low as 8.4% vs 1.7%, and the majority of complications were treated conservatively, implying that there was no difference in the need for surgical intervention. Moreover, there was no detrimental effect on mortality, PD technique failure, or peritonitis-free survival.
These findings are in contrast with the experience from unplanned initiation of HD relying on temporary vascular access formation and its associated risks of potentially fatal complications in terms of bacteremias or venous stenosis and thrombosis.
Clinical Outcome
As reviewed recently (10), published data on clinical outcome after unplanned initiation of PD are very limited. However, studies from Europe (11–13) and Asia Pacific (14) all indicate that mortality after unplanned start on PD is equal to or less than mortality after unplanned start on HD. Moreover, it is evident beyond any doubt that unplanned HD patients, compared with unplanned PD patients and due to the temporary vascular access, have a much higher risk of potentially lethal bacteremias. The risk of mechanical and infectious complications associated with temporary access for unplanned HD is particularly pronounced in older patients due to the underlying vascular disease associated with their renal disease, to the burden of comorbidities, and to malnutrition.
For patients aged 65 years or older in our program, the 3-month and 1-year patient survival are 90% and 80%, respectively, while the corresponding combined technique and patient survival are 80% and 50%, respectively (5).
Perspectives
The establishment of a program for unplanned start on APD right after PD catheter implantation ensures that late-referred patients with urgent need for initiation of dialysis are also given a real choice of selecting their preferred dialysis modality. Combining this program with a program for assisted PD further ensures that more frail older patients with a large burden of comorbidity, physical disabilities, and psychosocial problem—traditionally regarded as contraindications for PD—are given a real choice to select a home-based dialysis treatment.
In our opinion and experience, the risk of serious complications associated with the implantation and immediate use of a PD catheter is by far less than the risk of complications associated with unplanned start on HD with a temporary CVC. Unplanned start on APD is also a gentle, safe, and feasible alternative to unplanned start on HD with a temporary CVC for the late-referred older patient with ESRD and urgent need for dialysis.
Key Points
Late-referred patients with urgent need for dialysis are overrepresented among the older ESRD population and are particularly likely to be started on HD with a temporary CVC.
Unplanned start on HD is associated with excess mortality and increased risks of potentially lethal infectious or mechanical complications.
Unplanned start on PD may be associated with an increased risk of mechanical complications but apparently no detrimental effect on mortality, PD technique failure, or risk of infectious complications.
Mortality after unplanned start on PD seems to be equal to or less than mortality after unplanned start on HD.
Unplanned start on APD is also a gentle, safe, and feasible alternative to unplanned start on HD with a temporary CVC for the late-referred older patient with ESRD and urgent need for dialysis.
Disclosures
JVP has received an unrestricted research grant from Baxter Healthcare.
REFERENCES
- 1. Danish Nephrology Registry , Annual Report 2013. Available from: http://www.Nephrology.dk.
- 2. United States Renal Data System 2013. Available from: http://www.usrds.org/atlas.aspx
- 3. Dombros N, Dratwa M, Feriani M, Gokal R, Heimbürger O, Krediet R, et al. European best practice guidelines for peritoneal dialysis. 3 Peritoneal access. Nephrol Dial Transplant 2005; 20(Suppl 9):ix8–12. [DOI] [PubMed] [Google Scholar]
- 4. Povlsen JV, Ivarsen P. How to start the late referred patient urgently on chronic PD. Nephrol Dial Transplant 2006; 26(Suppl 2):S56–9. [DOI] [PubMed] [Google Scholar]
- 5. Povlsen JV, Ivarsen P. Assisted peritoneal dialysis: also for the late referred elderly patient. Perit Dial Int 2008; 28:461–7. [PubMed] [Google Scholar]
- 6. Lee A, Gudex C, Povlsen JV, Bonnevie B, Nielsen CP. Patients' views regarding choice of dialysis modality. Nephrol Dial Transplant 2008; 23:3953–9. [DOI] [PubMed] [Google Scholar]
- 7. Povlsen JV, Ivarsen P. Assisted automated peritoneal dialysis (AAPD) for functionally dependent and elderly patients. Perit Dial Int 2005; 25(Suppl 3s):S60–3. [PubMed] [Google Scholar]
- 8. Povlsen JV, Ivarsen P, Jørgensen KA. Acute start on chronic peritoneal dialysis: rate of correction of azotemia and acidosis. Perit Dial Int 2004; 24(suppl 2):S45. [Google Scholar]
- 9. Liu Y, Zhang L, Lin A, Ni Z, Qian J, Fang W. Impact of break-in period on the short-term outcomes of patients started on peritoneal dialysis. Perit Dial Int 2014; 34:49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ivarsen P, Povlsen JV. Can peritoneal dialysis be applied for unplanned initiation of chronic dialysis? Nephrol Dial Transplant 2013; 0:1–6. [DOI] [PubMed] [Google Scholar]
- 11. Danish Nephrology Registry , Annual Report 2011. Available from: http://www.Nephrology.dk
- 12. Lobbedez T, Lecouf A, Ficheux M, Henri P, Hurault de Ligny B, Ryckelynck JP. Is rapid initiation of peritoneal dialysis feasible in unplanned dialysis patients? A single centre experience. Nephrol Dial Transplant 2008; 23:3290–4. [DOI] [PubMed] [Google Scholar]
- 13. Koch M, Kohnle M, Trapp R, Haastert B, Rump LC, Aker S. Comparable outcome of acute unplanned peritoneal dialysis and haemodialysis. Nephrol Dial Transplant 2012; 27:375–80. [DOI] [PubMed] [Google Scholar]
- 14. Foote C, Ninomiya T, Gallagher M, Perkovic V, Cass A, McDonald SP, et al. Survival of elderly dialysis patients is predicted by both patient and practice characteristics. Nephrol Dial Transplant 2012; 27:3581–7. [DOI] [PubMed] [Google Scholar]


