Abstract
Chronic kidney disease (CKD) in all its stages has become an important problem for older patients, stage 3 – 5 is expected to happen in 25 to 30% of the population, and a higher prevalence can be found in residential care and nursing homes, affecting the demand for patient education. Although older patients are able and keen to learn, there are specific needs that must be addressed. The focus of this paper is to review the demands to train and maintain older patients on peritoneal dialysis (PD) at home.
Keywords: Peritoneal dialysis, nursing, elderly, older
Peritoneal dialysis (PD) patients at home require much more than just clinical management. Social and psychological support and outcomes are important for all age groups. Nurses are responsible for ensuring prevention of technique failure due to infections and supporting patients with restrictions imposed by the therapy. The burden of dialysis is well documented as it affects an individual's social and psychological well-being. The need for individuals to achieve a sense of normality is often overlooked even if it is the most important factor in their life (1). The focus of this paper is older patients on PD, their training needs, and supportive needs to maintain them at home. This is particularly relevant as the chronic kidney disease (CKD) population aged 65 years or older has grown considerably, and this growth is expected to accelerate in coming years (2,3). Chronic kidney disease stage 3 – 5 is expected to occur in 25 to 30% of the population and a higher prevalence can be found in residential care and nursing homes (4).
Therefore, the numbers of older patients requiring dialysis therapy is rising. Ensuring older patients have equal access to a home therapy means pre-dialysis education and assessment that includes a multidisciplinary team is important. There is evidence suggesting that PD intrudes less in the life of older patients and maintains patients' independence (5–7). Some have even highlighted that older patients are often more motivated and compliant with treatment and therefore the challenges for the nurses are different (8,9).
The challenges of the older patient on PD at home need to be considered in the context of specific issues relating to the aging process such as frailty, dementia, loneliness, visual and hearing impairment, cognitive dysfunction, and dexterity (2,10–12). The nursing theory of self-care is based on the concept that all individuals seek behaviors to promote personal well-being, with an emphasis on maintaining a balance between the person's ability to maintain self-care and the required demands, and on how patients cope with changes in their health status to become independent (13,14). Therefore, applying such a theory of self-care to the older person will bring a positive outcome, empowering them for treatment and using judgment skills developed over a lifetime of experience increasing self-esteem (13,14).
Self-management and ongoing support, as with any long-term condition, need to be part of the decision-making process, and the philosophy of improving self-efficacy should be integral. Many older patients have multiple morbidities, all of which can impact on their physical and mental health, affecting disability and ability in performing activities of daily life (15). Educational interventions can play a crucial role in the success of individuals in managing their own treatments. Adapting and appreciating this in the older person is particularly relevant for a home therapy like PD (16). All considered, there is strong evidence of the benefits of PD in the older patient (17–19). The aim of this paper is to provide a structure of how this can be achieved using a case study exemplar throughout.
Training and Assessment of Older Patients
One of the most important aspects before commencement of training is a full assessment of the patient, including physical and psychosocial needs, motivation to learn, reading level, barriers to learning, learning styles, family support, home circumstances, and consideration of nursing homes (20). Patient preferences encompass quality of life, asking the patient what they enjoy, if they go on holiday and aspects of life that would fit with PD.
When assessing the capability of patients for PD it is essential to identify barriers that may hinder successful self-care. In addition to the limitations inherent to CKD, older patients will have other limitations and barriers that can be more pronounced, most commonly: poor vision, frailty, cognitive dysfunction, accommodation issues, functional impairment, and a bias from renal teams that older patients cannot perform PD (2,10,11). Such barriers can be usefully divided into medical, cognitive, psychological, or social; most affect, but do not contraindicate, PD and are much more common than absolute contraindications (10).
Probably the most significant assessment at this stage is cognition as this will have considerable influence on their skills to perform or remember tasks (21). Often, formal or informal assessments of cognitive ability are not undertaken and can be one of the reasons patients are seen to fail in training (15). A simple recommended tool is the Montreal Cognitive Assessment (MOCA) tool (15) which can be performed in 10 minutes. It is recommended that it be done before and after initiation of therapies and can help to tailor interventions and supportive treatments.
Assessment of frailty needs to be understood if accurate and adequate interventions are applied. Frailty is a multidimensional syndrome of loss of reserves (i.e. lack of energy and reduced physical ability, cognition, and health), all of which give rise to vulnerability (22). There are a number of definitions, and Rockwood highlights that the many scales available reflect uncertainty about the term and its components (22). There are simple measures that can be undertaken by healthcare professionals or full geriatric assessments that require specialist geriatric team input (23).
Understanding the role of family members and caregivers and their willingness to undertake the therapy and the potential of assisted PD are also all important.
Case Study
Joan is 82 years old and lives alone with family support close by. She was seen initially by the pre-dialysis team and wanted to consider home therapy as she lived 20 miles from the center. She had a home assessment and on initial assessment was found to have no significant cognitive impairment, but she was frail and quite disabled due to osteoarthritis and was in a wheelchair. Pain and mobility issues were significant but assisted automated PD (APD) was her preferred therapy. She was very independent even with her significant mobility problems. Her training took place at home, and within 3 days she was able to connect and disconnect from the machine.
The guidelines for patient training from the International Society for Peritoneal Dialysis (ISPD) recommend that patient training should be based on adult education (24). Independently of the age of learner, the type or style of learning should be recognized and training implemented accordingly (24,25). There are a variety of tests that can be used to assess learning styles, or a simple question to the patient (i.e. “How do you learn best?”) can be sufficient to guide training. The most common learning styles are aural, kinesthetic, visual, and read/write. Table1 shows some examples on how to implement training according to patients' learning style characteristics (26).
TABLE 1.
Characteristics of Learning Styles
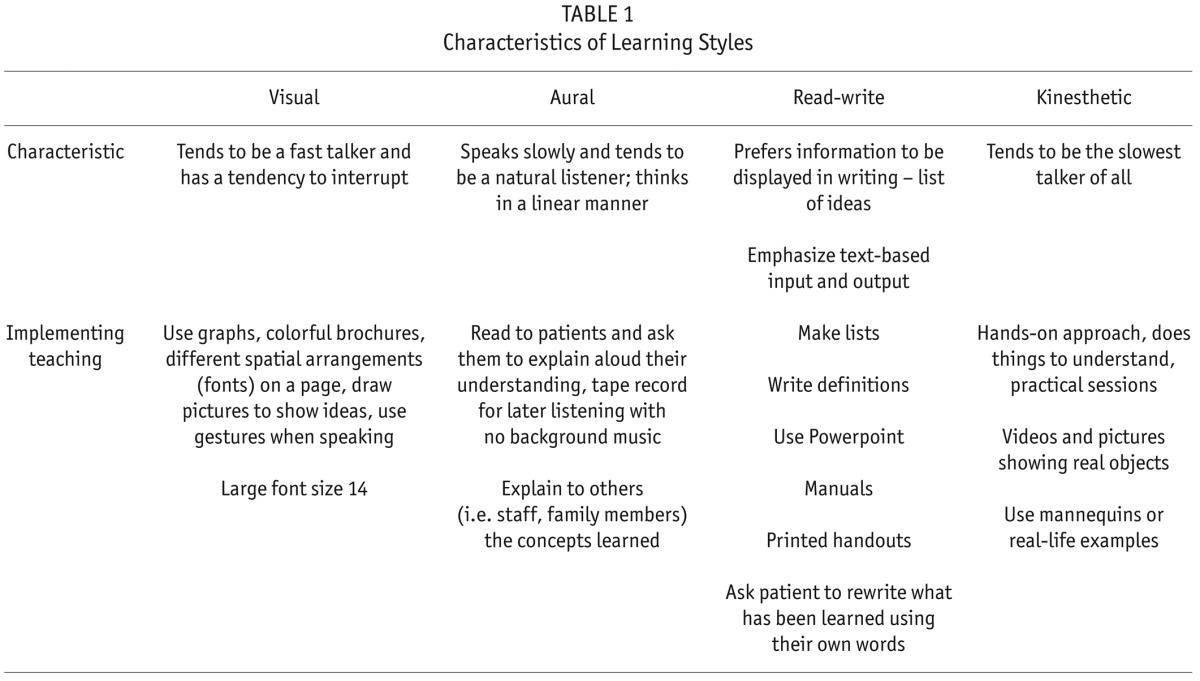
Figure 1 demonstrates the ongoing aspects for older patients from assessments required before training, aspects adopted in training and support at home. This is a cycle, and assessments need to continue once the patient is at home. Successful programs have demonstrated the importance of dedicated teams and the need for individualized support and training, advocating regarding training and testing as positive; showing improvements in peritonitis rates (27,28). Training and interventions that encompass self efficacy can also enhance self management skills (29). When planning to train older patients, various issues should be considered to enhance the patient experience:
Focus on patient's strengths and your confidence in their ability to learn;
Use the smallest amount of information to accomplish negotiated goals;
Use simple terms and everyday language and give information as vividly and explicitly as possible;
Teach 1 step at a time and use multiple methods and tools requiring fewer literacy skills;
Allow patient to restate information in their own words and use praise and encouragement;
Use tailoring and cuing for patient's coordination of procedures and use repetition to reinforce information;
Extend length of time to allow shorter days, time to read and to absorb information. Some patients may take up to 10 days before they feel confident to be self-caring;
Consider interactive components such as group work and peer support;
Focus on self-efficacy and problem-solving;
Use aids for dexterity, mannequins, aprons for training, and picture procedures;
Use simple written procedures with larger print tested and adapted to each individual;
Be realistic and know when a patient cannot manage self-care, so other support/assistance can be explored (20).
Figure 1 —
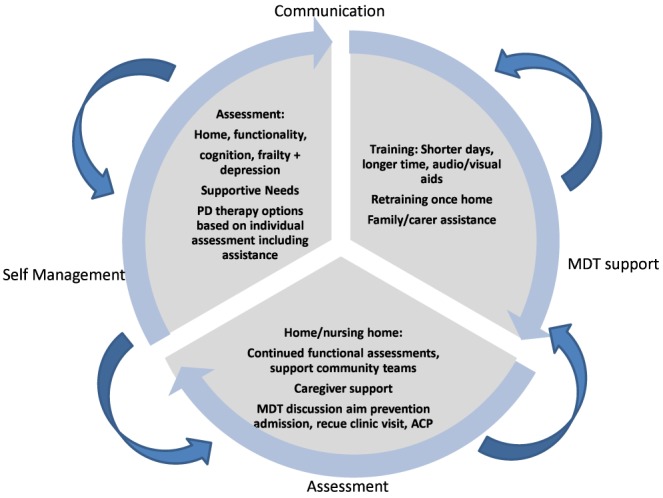
Ongoing aspects for older patients.
The educational needs of older patients may well be different from a younger age group. Experience shows that training older patients on continuous ambulatory peritoneal dialysis (CAPD) took a day longer than younger patients but with similar outcomes (30). A report from the US examining ways of improving health literacy in the older adult made some clear recommendations advocating greater rigor in the development of materials and tools designed for older adults (31). Health professionals often make information complex with too much jargon. Often older patients struggle with remembering and following a text. The therapy of choice needs to reflect their abilities. Consideration of CAPD or APD should be part of this process. If CAPD is the preferred option, then consider how many exchanges are necessary; often 2 – 3 exchanges per day are sufficient if good residual renal function is present. With the increase in utilization of assisted PD, commencing older patients on PD with assistance allows them time to adjust and learn the technique when confidence is gained over a long period of time. Being able to provide assisted PD in this population can therefore be a useful option and perhaps act as a bridge to independence and self-care. Even if the patient is not suitable for total self-care, minimal training with assisted PD can be offered as the patient may only have to troubleshoot problems, or simply be instructed on how to turn off APD if they have a problem. This may also be the case if the patient is in a nursing home and staff within that environment can be trained to assist. For patients having assisted CAPD, nurses or assistants can be trained, with minimum training required for patients (32).
The location of training varies, but the patient's home or a specific training environment is recommended (16). Nurses delivering patient training need to have adequate skills in PD and adaptability to meet individual needs with an understanding of learning and educational principles.
In summary, patient education is a key nursing role, and should enable patients to follow a medical regimen and promote well-being. Factors such as advanced age, lack of social support, dementia, or other physiological factors can interfere with learning.
Support at Home
Once an older patient has successfully completed their training for independent or assisted PD, ongoing support and assessment continue. Some important points to consider highlighted by Finkelstein to help maintain older patients at home relate to the home situation, family and social support, community support, spirituality, and caregiver burden (33). Community visits by trained PD nurses can be pivotal, providing expertise and support and developing trusting relationships with patients, families, and caregivers.
Support from family/caregivers can be particularly crucial, and many have commented on its importance and relevance, particularly as a barrier to self-care (34). The patient who lives alone often requires different levels of support and may often be unfairly biased in terms of therapy options. However, individual assessment and preference should always be considered. Support from family members and caregivers is significant and their support often influences the success and ability to maintain an older patient at home on PD. When family and caregivers are involved in the dialysis, consideration of the impact and burden on those members should be part of the routine assessments. Studies have demonstrated negative impact on family caregivers of older PD patients in particular on the mental domains of quality of life (QOL) where they are more likely to experience adverse psychological and social consequences (35,36). However with adequate support and interventions directed at caregivers, this could be improved. Families and caregivers should be included in regular assessments by talking to them alone and finding out how they are coping. Often simple measures can help by encouraging social activities and considering support from other sources. In particular, those of lower educational status and economic conditions may require enhanced support (35). Supportive programs of care included in rehabilitation often provide networks and peer support for family and caregivers (37). Support groups have reported good patient engagement, including physical and social activities (38).
Publications from Hong Kong on CAPD in the older patient have demonstrated the importance of family support (39,40). Support can often be through systems and pathways other than renal services; spirituality is often one way patients and families draw on support and coping (41–43). Being aware of local groups and initiatives specifically designed for the older person can be very helpful and in many countries, although often voluntary, is a resource that is available.
The continued assessment of cognition and frailty are all important. Evaluating early cognitive symptoms must involve family members and individuals who know the patient well. Full geriatric assessments can be carried out by specialists, and these teams can not only help and support the patients but also consider appropriate interventions. Depression is a common psychological problem within the dialysis population and its diagnosis can remain undetected and correlates physiological stresses, anxiety, and social support (44). These factors are all relevant in the older patient who may rely on social support. Depression can also affect cognition, as mentioned earlier. It is therefore important to recognize signs and symptoms of depression in the patient and families/caregivers and refer appropriately.
An older patient who experiences worsening mobility, frailty, or even visual problems may need adjustments within the home so that they can continue safely with the therapy. Older patients at home without a family member or caregiver to support them may often find hemodialysis (HD) as the only other option offered. Consider assisted PD if that is available, other types of assistance and social support, or even a nursing home.
All of these aspects require good communication and involvement of the wider multidisciplinary team (MDT) such as social workers, occupational therapists, physiotherapists, dieticians, and primary care providers. They can often help with adjustments required in the home, more supportive care, dietary considerations, and assistance with meals. Perhaps the most difficult and poorly communicated aspects of the older patient are their expectation of the therapy, and their wishes need to be addressed on a regular basis with the MDT. The use of advance care plans can help to address their concerns and allow the patient to decide on their future care and management (45). An example would be a patient expressing wishes to not transfer to HD even if PD therapy has become too difficult to continue at home. This requires open discussion, clear documentation and a team approache to ensure the patient's wishes are fulfilled. It is often even burden-some for these patients to attend clinics; keeping them at home and liaising with the team can avoid unnecessary visits to the hospital.
Maintaining older patients at home on PD requires dedication, belief in the patient's wishes, regular review, and assessments. Many older patients are motivated and manage for many years on the therapy with minimal support and therefore an individual approach will guarantee this population is treated and managed equally.
Case Study
One year into therapy it became clear that Joan found it difficult to attend the hospital for appointments due to the travel and distances. She would be out of the house all day and her pain exacerbated by the visit. After some discussion, it was agreed that Joan would not attend clinics and would have blood taken in the community. An advance care plan was also written up as Joan did not want to have HD if PD failed or she herself could no longer manage. Her doctor and local teams were contacted to ensure they were aware of her decision and how she wanted to be managed at home.
Joan had a good quality of life and managed many weekends away with her family when therapy was held off. She had good residual renal function and could often have nights off her therapy.
She has continued on assisted APD for 3 years with no admissions to hospital and no episodes of infections. She values the daily visit and contact by the assisted team and, even with her disabilities, makes her own greeting cards and regularly sends in a crop of fruit from her garden.
Key Messages
PD for the elderly should not be a contra-indication. With full support and additional assistance, they can maintain a good quality of life and should have equal access to choices of different therapies;
Regular assessment of elderly patients is essential and part of routine care;
Assessment of cognition, frailty, and depression should be undertaken by the team;
Communicate with the patient regularly on their preferences and expectations using advance care plans as necessary;
Develop research and evidence based on support systems/rehabilitation programs required to maintain older patients at home;
Support for caregivers/family needs to be an integral part of the management of older patients.
REFERENCES
- 1. Curtin RB, Mapes D, Schatell D, Burrows-Hudson S. Self-management in patients with end stage renal disease: exploring domains and dimensions. Nephrol Nurs J 2005; 32(4):389–95. [PubMed] [Google Scholar]
- 2. Berger JR, Hedayati SS. Renal replacement therapy in the elderly population. Clin J Am Soc Nephrol 2012; 7(6):1039–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sesso Rde C, Lopes AA, Thome FS, Lugon JR, Watanabe Y, Santos DR. Chronic dialysis in Brazil: report of the Brazilian dialysis census, 2011. J Bras Nefrol 2012; 34(3):272–7. [DOI] [PubMed] [Google Scholar]
- 4. Brown EA. Should older patients be offered peritoneal dialysis? Perit Dial Int 2008; 28(5):444–8. [PubMed] [Google Scholar]
- 5. Brown EA, Johansson L. Dialysis options for end-stage renal disease in older people. Nephron Clin Pract 2011; 119:C10–3. [DOI] [PubMed] [Google Scholar]
- 6. Fan SLS, Sathick I, McKitty K, Punzalan S. Quality of life of caregivers and patients on peritoneal dialysis. Nephrol Dial Transpl 2008; 23(5):1713–9. [DOI] [PubMed] [Google Scholar]
- 7. Brown EA, Johansson L. Epidemiology and management of end-stage renal disease in the elderly. Nat Rev Nephrol 2011; 7(10):591–8. [DOI] [PubMed] [Google Scholar]
- 8. Kutner NG. Improving compliance in dialysis patients: does anything work? Semin Dial 2001; 14(5):324–7. [DOI] [PubMed] [Google Scholar]
- 9. Kutner NG, Zhang R, McClellan WM, Cole SA. Psychosocial predictors of non-compliance in haemodialysis and peritoneal dialysis patients. Nephrol Dial Transplant 2002; 17(1):93–9. [DOI] [PubMed] [Google Scholar]
- 10. Oliver MJ, Garg AX, Blake PG, Johnson JF, Verrelli M, Zacharias JM, et al. Impact of contraindications, barriers to self-care and support on incident peritoneal dialysis utilization. Nephrol Dial Transplant 2010; 25(8):2737–44. [DOI] [PubMed] [Google Scholar]
- 11. Luker KA, Caress AL. Evaluating computer-assisted-learning for renal patients. Int J Nurs Stud 1992; 29(3):237–50. [DOI] [PubMed] [Google Scholar]
- 12. Lim WH, Dogra GK, McDonald SP, Brown FG, Johnson DW. Compared with younger peritoneal dialysis patients, elderly patients have similar peritonitis-free survival and lower risk of technique failure, but higher risk of peritonitis-related mortality. Perit Dial Int 2011; 31(6):663–71. [DOI] [PubMed] [Google Scholar]
- 13. O'Shaughnessy M. Application of Dorothea Orem's theory of self-care to the elderly patient on peritoneal dialysis. Nephrol Nurs J 2014; 41(5):4. [PubMed] [Google Scholar]
- 14. Ricka R, Vanrenterghem Y, Evers GC. Adequate self-care of dialysed patients: a review of the literature. Int J Nurs Stud 2002; 39(3):329–39. [DOI] [PubMed] [Google Scholar]
- 15. Kalirao P, Pederson S, Foley R, Kolste A, Tupper D, Zaun D, et al. Cognitive impairment in peritoneal dialysis patients. Am J Kidney Dis 2011; 57(4):612–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schaepe C, Bergjan M. Educational interventions in peritoneal dialysis: a narrative review of the literature. Int J Nurs Stud 2015; 52(4):882–98. [DOI] [PubMed] [Google Scholar]
- 17. Brown E, Pryde K, Schmalzhal C. Assisted automated peritoneal dialysis (AAPD) – results of a feasibility study. Brit J Renal Med 2006; 11(2):23. [Google Scholar]
- 18. Brown EA, Dratwa M, Povlsen JV. Assisted peritoneal dialysis – an evolving dialysis modality. Nephrol Dial Transplant 2007; 22(10):3091–2. [DOI] [PubMed] [Google Scholar]
- 19. Finkelstein FO, Afolalu B, Wuerth D, Finkelstein SH. The elderly patient on CAPD: helping patients cope with peritoneal dialysis. Perit Dial Int 2008; 28(5):449–51. [PubMed] [Google Scholar]
- 20. McCormick J. Relating to teaching and learning. In: Butera AEME, ed. Contemporary Nephrology Nursing: prinicples and practice. Pitman: American Nephrology Nurses' Association; 2006; 885–902. [Google Scholar]
- 21. Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimers disease: recommendations from the National Institute on Aging-Alzheimers Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2014; 7(3):270–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173(5):489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fit for frailty; Consensus best practice guidance for the care of older people living with frailty in community and outpatient settings. British Geriatric Society, 2014. Available at: http://www.bgs.org.uk/campaigns/fff/fff_full.pdf [Google Scholar]
- 24. Bernardini J, Price V, Figueiredo A. Peritoneal dialysis patient training, 2006. Perit Dial Int 2006; 26(6):625–32. [PubMed] [Google Scholar]
- 25. Knowles MS, Holton IEF, Swanson RA. Aprendizagem de resultados, uma abordagem a efetividade da educação corporativa. Rio de Janeiro: Elsevier, 2009. [Google Scholar]
- 26. Hawk TF, Shah AJ. Using learning style instruments to enhance student learning. Decision Sci J Innovative Educ 2007; 5(1):1–19. [Google Scholar]
- 27. Fang W, Ni Z, Qian J. Key factors for a high-quality peritoneal dialysis program — the role of the PD team and continuous quality improvement. Perit Dial Int 2014; 34(Suppl 2):S35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gadola L, Poggi C, Poggio M, Sáez L, Ferrari A, Romero J, et al. Using a multidisciplinary training program to reduce peritonitis in peritoneal dialysis patients. Perit Dial Int 2013; 33(1):38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Su C-Y, Lu X-H, Wang T. Promoting self-mangement improves the health status of patients having peritoneal dialysis. J Adv Nurs 2009; 65(7):1381–9. [DOI] [PubMed] [Google Scholar]
- 30. Li PK, Law MC, Chow KM, Leung CB, Kwan BC, Chung KY, et al. Good patient and technique survival in elderly patients on continuous ambulatory peritoneal dialysis. Perit Dial Int 2007; 27(Suppl 2):S196–201. [PubMed] [Google Scholar]
- 31. Improving Health Literacy for Older Adults: Expert Panel Report: US Department of Health and Human Services: CDC, 2009. Available at: http://www.cdc.gov/healthliteracy/pdf/olderadults.pdf [Google Scholar]
- 32. Lobbedez T, Moldovan R, Lecame M, de Ligny BH, El Haggan W, Ryckelynck J-P. Assited peritoneal dialysis. Experience in a French renal department. Perit Dial Int 2006; 26(6):671–6. [PubMed] [Google Scholar]
- 33. Finkelstein F, Afolalu B, Wuerth D, Finkelstein S. The elderly patient on CAPD: helping patients cope with peritoneal dialysis. Perit Dial Int 2008; 28(5):449–51. [PubMed] [Google Scholar]
- 34. Oliver MJ, Garg A, Blake PG, Johnson J, Verrelli M, Zacharias J, et al. Impact of contraindications, barriers to self care and support on incident dialysis utilisation. Nephrol Dial Transplant 2010; 25:2737–44. [DOI] [PubMed] [Google Scholar]
- 35. Belasco A, Barbosa D, Battencourt A, Diccini S, Sesso R. Quality of life of family caregivers of elderly patients on haemodialysis and peritoneal dialysis. Am J Kidney Dis 2006; 48(6):955–63. [DOI] [PubMed] [Google Scholar]
- 36. Fan S, Sathick I, McKitty K, Punzalan S. Quality of life of caregivers and patients on peritoneal dialysis. Nephrol Dial Transplant 2008;23:1713–9. [DOI] [PubMed] [Google Scholar]
- 37. Wang L, Dong J, Gan H, Wang T. Empowerment of patients in the process of rehabilitation. Perit Dial Int 2006; 27(Suppl 2):S32–4. [PubMed] [Google Scholar]
- 38. Cheng YY, Wong YF, Chu BYC, Lam WO, Ho YW. Rehabilitating a dialysis patient. Perit Dial Int 2003; 23(Suppl 2):S81–3. [PubMed] [Google Scholar]
- 39. Hiramatsu M, Japanese Society for Elderly Patients on Peritoneal Dialysis How to improve survival in geriatric peritoneal dialysis patients. Perit Dial Int 2007; 27(Suppl 2):S185–9. [PubMed] [Google Scholar]
- 40. Hiramatsu M. Improving outcome in geriatric peritoneal dialysis patients. Perit Dial Int 2003; 23(Suppl 2):S84–9. [PubMed] [Google Scholar]
- 41. de Guzman A, Chy M, Concepcion A, Conferido A, Corectico K. The language of coping: understanding Filipino geriatric patients' haemodialysis lived experiences. Educational Gerontology 2009; 35:769–83. [Google Scholar]
- 42. Kelly J. Spirituality as a coping mechanism. Dimens Crit Care Nurs 2004; 23(4):162–8. [DOI] [PubMed] [Google Scholar]
- 43. Weil C. Exploring hope in pateints with end-stage renal disease on chronic haemodialysis. Nephrol Nurs J 2000; 27(2):20. [PubMed] [Google Scholar]
- 44. Ye XQ, Chen WQ, Lin JX, Wang RP, Zhang ZH, Yang X, et al. Effect of social support on psychological-stress-induced anxiety and depressive symptoms in patients receiving peritoneal dialysis. J Psychosom Res 2008; 65(2):157–64. [DOI] [PubMed] [Google Scholar]
- 45. Holley J. Advance directives and advanced care planning in patients with end-stage renal disease. In: Chambers E, Germain M, Brown E, eds. Supportive Care for the Renal Patient. Oxford: Oxford University Press; 2004. [Google Scholar]


