Abstract
Individuals aged over 70 years at the time of starting dialysis have a varied and often challenging existence on dialysis. Canadian data suggest those starting dialysis between the ages of 75 and 79 years will have an average life expectancy of 3.2 years, while based on US data, patients can expect an average life expectancy of 25 months. A substantial proportion of these patients will, however, experience transient or permanent loss of personal independence within the first few months to years on dialysis. Preliminary data from patients recently started on peritoneal dialysis (PD) suggest patients and families adapt, but that the adaptation often involves limiting activities and altering the social role the patient has within the family. As data emerge, it will be possible to hypothesize whether this adaptation is beneficial in the long term, or whether these adaptations are permissive, allowing the patient to play a sick role leading to an accelerated transition to frailty and possibly death. Future research will hopefully inform us whether the functional dependency can be identified early and whether it is preventable. In the interim, repair rather than prevention is possible through rehabilitation. We therefore advocate that programs providing PD care consider the integration of protocols whereby patients may undergo formal evaluation to identify those who would benefit from walking or personal care aids, rehabilitation interventions, and, when needed, personal support.
Keywords: Peritoneal dialysis, elderly, geriatric assessment, rehabilitation
Individuals aged over 70 years at the time of starting dialysis have a varied and often challenging existence on dialysis. Canadian data suggest those starting dialysis between the ages of 75 and 79 years will have an average life expectancy of 3.2 years (1), while based on US data, patients can expect an average life expectancy of 25 months (2,3). A substantial proportion of these patients will, however, experience transient or permanent loss of personal independence within the first few months to years on dialysis (4–7).
Functional Status and Fall Risk in the Peritoneal Dialysis Population
Patients established on peritoneal dialysis (PD) appear to be at similar risk of all geriatric syndromes to that of hemodialysis (HD) patients. Cognitive dysfunction appears equally common and severe as in the HD population, as does functional decline (8,9). Functional decline may manifest in multiple ways. In the early stages, patients experience difficulty with household tasks such as housekeeping, grocery shopping, or preparing meals. As the decline progresses, they (or family members) report increasing difficulty with completing routine daily personal hygiene tasks such as bathing, brushing teeth, or dressing. Patients with chronic kidney disease (CKD) appear to have a higher burden of functional decline than those with either no disease or other forms of chronic disease. The population maintained on chronic PD is no different. In a small single-center study of patients aged 65 years and older established on PD, only 11% of patients reported being fully independent in all activities of daily living. Of those with some form of dependence, many had only mild impairments; however, 64% had limitations affecting personal care (9). The presence of functional limitations does not appear to deter from the use of PD as a dialysis modality (10), particularly as assisted PD is increasingly available, but it may impact on quality of life and lead to high levels of caregiver stress (11,12). Perhaps more concerning is that the fall risk in the older PD population is estimated at 1.7 falls per patient-year, with more than 50% of patients experiencing one or more falls (13). Accidental falls do not often result in injury or the need for hospitalization, but their occurrence alone is predictive of increased mortality risk, likely due to the associated frailty (13).
Comprehensive Geriatric Assessment
Comprehensive geriatric assessment (CGA) is a term used to describe the formal evaluation of patients using a ‘geriatric lens’ (Figure 1). The assessment is often conducted over several visits, in the home and the clinic, by a variety of health-care professionals such as nursing, physiotherapy, occupational therapy and social work. Evaluation includes a detailed medical history including treatment targets; assessment of the home environment and social support structure (including both how these are impacted by those symptoms that may be poorly controlled and how the environment itself influences a patient's ability to manage their medical conditions); functional history; and an assessment of personal values and lifestyle preferences. This information is then coupled with a full assessment of strength, sensory function, balance, cognition, depression, nutrition, and communication skills and used to identify potential areas of concern (14). A variety of tools used to evaluate patients are available (15), many of which have been well validated. As each has advantages and disadvantages, the choice of tools should be left to the individual units/clinicians. One particularly useful, and easy, method that can be used to follow a patient over time is to sequentially assess their ‘life-space mobility’ (16). The life-space mobility tool, in essence, captures how far the patient moves around in their day-to-day functioning (ranging from their sleeping accommodation to travel outside of their city) and how frequently they do so. Changes in life-space mobility have been shown to be predictive of poorer health outcomes, with a more rapid deterioration seen with worsening levels of renal disease (17).
Figure 1 —
Selected components of the Comprehensive Geriatric Assessment.
A key component of CGA is the medical assessment. The physician is responsible for evaluating the burden of symptoms and prioritizing the medical conditions based on the life expectancy and the patients' values. The detailed history includes medical conditions often overlooked by specialists as coincidental such as cataract, or osteoarthritis, to allow for a more holistic approach for the individual. For example, if a patient has prioritized symptom control and quality of life over longevity, the physician may chose to prioritize treatment of osteoarthritis (use of a non-steroidal anti-inflammatory drug transiently) over cardio-preventative measures (avoidance of any non-steroidal anti-inflammatory drug).
Patients with complex multimorbidity and functional dependency are often seen by a number of specialists and are therefore at risk of polypharmacy (18). A key component of the medical assessment, done if possible in collaboration with a trained pharmacist, is to evaluate each medication and its need, placing a particularly high emphasis on the immediate benefits vs long-term benefits; the impact of subtle or ‘unimportant’ side effects such as constipation or dizziness; as well as considering any potential negative effects on other medical conditions. Multidisciplinary healthcare workers use the findings of the CGA to create a care plan that maximizes the functional and/or cognitive abilities of older individuals and provide support for the areas that are deficient, thus allowing them to remain in their home setting as long as possible (19).
What is Geriatric Rehabilitation?
One definition used for rehabilitation is a “process by which form and function are restored following injury or illness, such that life can be lived to the fullest capacity compatible with the degree of abilities and disabilities” (20). The definition has 2 important features: first, it emphasizes that restoration of function is likely to occur only in those with a recent loss of function and, secondly, that rehabilitation involves a process through which patients regain function through both learning or re-learning new skills and adaptation of skills or assistive devices to minimize the impact of the new disability.
Interdisciplinary team care is an essential part of geriatric rehabilitation. Team members include nurses, occupational therapists, physiotherapists, physicians, psychologists, pharmacists, social workers, and speech therapists. Through daily interactions, particularly with the nurses, patients gradually learn to assume self-care responsibilities outside of their therapy sessions. Rehabilitation may be performed in the home, as an outpatient or as an inpatient, depending on resources and patient needs. In an ideal setting, dialysis units could provide services that would allow for integrated physical rehabilitation and PD support and (where necessary) retraining.
The Evidence for Rehabilitation in Dialysis Care
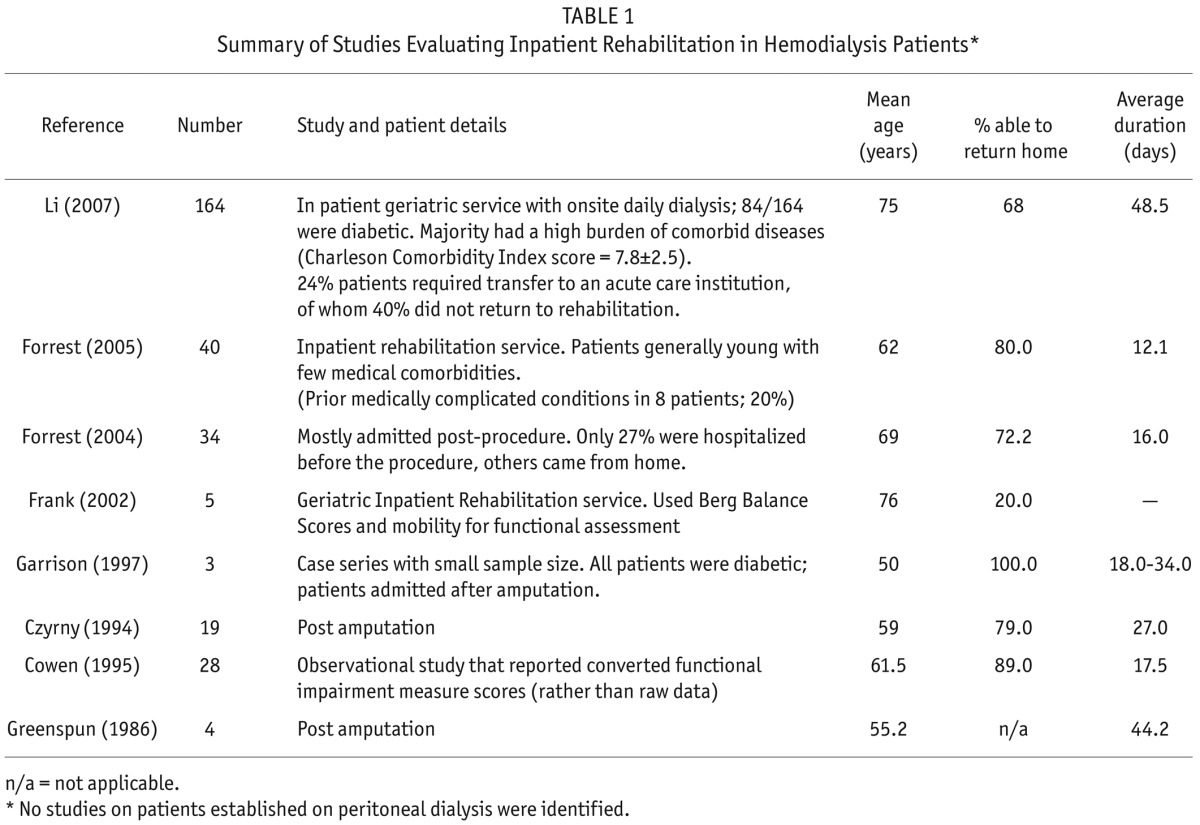
Although a number of published reports have used rehabilitation in their dialysis units, most have focused on patients undergoing HD (21–24). To our knowledge, no reports describe rehabilitation outcomes in the PD population. Geriatric renal rehabilitation has not been widely incorporated into routine dialysis care and, in many cases, is available only on a case-by-case basis. Published results suggest variable outcomes, as measured by the proportion of patients returning home, with anywhere between 20% to 100% of patients returning to their previous home environment (25–32). In the largest and most recent report, approximately 70% of patients undergoing rehabilitation while also undergoing chronic HD returned home (Table 1) (32,33). At the time of admission, patients had a significant burden of comorbidity and high levels of functional dependence. In our unit, HD is offered on-site, on a daily dialysis schedule. Staffing levels have been increased in both the dialysis suite and on the ward to accommodate the higher burden of comorbidity and higher dependency levels (32).
TABLE 1.
Summary of Studies Evaluating Inpatient Rehabilitation in Hemodialysis Patients*
The Nephrologist's Role in Dialysis-Related Geriatric Rehabilitation
Ideally nephrologists should play a large role in identifying patients who could benefit from rehabilitation. However, as few nephrologists receive training in rehabilitation medicine (and there is scant literature about screening or referral protocols), this can be challenging. A practical first step is to introduce using the CGA at predetermined times such as dialysis initiation, hospitalization, after an accidental fall(s), or if there is a change in social status (e.g. changing residence or the death of a caregiver or key family member). Nephrologists also play an important role in helping the rehabilitation team evaluate and, if necessary, reset health targets for older dialysis patients. They have a better understanding of the prognosis and natural history of renal disease. Minor fluid shifts can have a significant effect on the symptoms of fatigue, and although less marked in the PD population, this can impact on the ability to participate well in therapy or exercise classes. In our experience, the physiotherapist is often the first to report differences in the patient's participation. While there may be many reasons for this, it is appropriate to assess whether either fatigue due to overzealous ultrafiltration or dyspnea due to minor overload is responsible. Some patients benefit from relaxing dialysis goals temporarily. This may include tolerating higher phosphate levels, or allowing more flexible exchange timings. By removing or relaxing dietary restrictions, patients are more likely to meet their protein-energy requirements during this period of repair and recovery. Particularly for patients with labile diabetes, the target blood glucose range may be adjusted to glycosylated hemoglobin of 8 – 9% (34).
Nephrologists are often responsible for medication rationalization. Polypharmacy is common in PD patients, and an inpatient stay is an ideal time to consider discontinuation of medications such as gastric acid suppressants, sedatives, and laxatives. Pain and pruritus management is often overlooked. Although often the symptoms cannot be fully controlled, an attempt at doing so, or even acknowledgment of the burden of symptoms, can improve patient well-being. Arthritis affecting the hands or shoulders or pain from peripheral neuropathy may limit the use of assistive devices such as walkers or rolators, and therefore should be addressed. The altered metabolism of many drugs used in pain control make treatment protocols challenging and the reader is encouraged to read further on the topic (35–39).
Conclusion
Increasingly, the medical community is becoming aware that our objectives are not the same as patient objectives. Both patients and caregivers are severely limited by functional, cognitive, or social disabilities associated with their disease and their treatments. Through the introduction of a CGA, and with the help of rehabilitation programs, nephrologists may be able to improve quality of life and patient-reported outcomes. Although the literature is limited, there do not appear to be significant barriers to the success of geriatric rehabilitation in PD populations.
Key Points
Geriatric assessment is critical in establishing what possible barriers are present that may impact successful PD, and establishing a care plan to promote maximal functionality
Elderly patients established on PD have a heavy degree of functional loss and often need help even with personal care
Elderly patients established on PD are at high risk of falls
The success of geriatric rehabilitation in the PD population has not been established, but there are no reasons to suspect it would be different from that seen in the HD population
The effect of assisted PD on changes in functional independence over time remain unknown
Disclosures
SVJ has received investigator-initiated research funding from Fresenius Medical Care, Canada (2015/6).
REFERENCES
- 1. Jassal SV, Trpeski L, Zhu N, Fenton S, Hemmelgarn B. Changes in survival among elderly patients initiating dialysis from 1990 to 1999. CMAJ 2007; 177(9):1033–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Survival in nursing home residents. 2010. [Online.] Available at: http://www.usrds.org/2010/slides/flash/vol1_06_nursing_home_10/aP%20Lite%20Flash/index.html Accessed 30 May 2011.
- 3. Kurella M, Covinsky KE, Collins AJ, Chertow GM. Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med 2007; 146(3):177–83. [DOI] [PubMed] [Google Scholar]
- 4. Ifudu O, Paul H, Mayers JD, Cohen LS, Brezsnyak WF, Herman AI, et al. Pervasive failed rehabilitation in center-based maintenance hemodialysis patients. Am J Kidney Dis 1994; 23(3):394–400. [DOI] [PubMed] [Google Scholar]
- 5. Ifudu O, Mayers J, Matthew J, Tan CC, Cambridge A, Friedman EA. Dismal rehabilitation in geriatric inner-city hemodialysis patients. JAMA 1994; 271(1):29–33. [PubMed] [Google Scholar]
- 6. Cook WL, Jassal SV. Functional dependencies among the elderly on hemodialysis. Kidney Int 2008; 73(11):1289–95. [DOI] [PubMed] [Google Scholar]
- 7. Jassal SV, Chiu E, Hladunewich M. Loss of independence in patients starting dialysis at 80 years of age or older. New Engl J Med 2009; 361(16):1612–3. [DOI] [PubMed] [Google Scholar]
- 8. Kalirao P, Pederson S, Foley RN, Kolste A, Tupper D, Zaun D, et al. Cognitive impairment in peritoneal dialysis patients. Am J Kidney Dis 2011; 57(4):612–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ulutas O, Farragher J, Chiu E, Cook WL, Jassal SV. Functional disability in older adults maintained on peritoneal dialysis therapy. Perit Dial Int 2014; Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Prakash S, Perzynski AT, Austin PC, Wu CF, Lawless ME, Paterson JM, et al. Neighborhood socioeconomic status and barriers to peritoneal dialysis: a mixed methods study. Clin J Am Soc Nephrol 2013; 8(10):1741–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Belasco A, Barbosa D, Bettencourt AR, Diccini S, Sesso R. Quality of life of family caregivers of elderly patients on hemodialysis and peritoneal dialysis. Am J Kidney Dis 2006; 48(6):955–63. [DOI] [PubMed] [Google Scholar]
- 12. Fan SL, Sathick I, McKitty K, Punzalan S. Quality of life of caregivers and patients on peritoneal dialysis. Nephrol Dial Transplant 2008; 23(5):1713–9. [DOI] [PubMed] [Google Scholar]
- 13. Farragher J, Chiu E, Ulutas O, Tomlinson G, Cook WL, Jassal SV. Accidental falls and the risk of mortality amongst older adults maintained on chronic peritoneal dialysis. Clin J Am Soc Nephrol 2014; 9(7): 1248–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Geriatric nephrology: improving dialysis rounds. 2012. [cited 2013]; Available from: http://www.asn-online.org/kidneydisease/geriatrics/rounds/.
- 15. University of Iowa IGEC Geriatric assessment tools. Iowa: [Online.] Available at: http://www.healthcare.uiowa.edu/igec/tools Accessed 2 September 2014. [Google Scholar]
- 16. Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc 2003; 51(11):1610–4. [DOI] [PubMed] [Google Scholar]
- 17. Bowling CB, Muntner P, Sawyer P, Sanders PW, Kutner N, Kennedy R, et al. Community mobility among older adults with reduced kidney function: a study of life-space. Am J Kidney Dis 2014; 63(3):429–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jyrkka J, Enlund H, Lavikainen P, Sulkava R, Hartikainen S. Association of polypharmacy with nutritional status, functional ability and cognitive capacity over a three-year period in an elderly population. Pharmacoepidemiol Drug Saf 201; 20(5):514–22. [DOI] [PubMed] [Google Scholar]
- 19. Farragher J, Jassal SV. Rehabilitation of the geriatric dialysis patient. Semin Dial 2012; 25(6):649–56. [DOI] [PubMed] [Google Scholar]
- 20. Clark GSS. Rehabilitation of the geriatric patient. In: DeLisa J, Gans BM, Bockenek WL, eds. Rehabilitation Medicine: Principles and Practice. 3rd ed. Philadelphia: Lippencott; 1993; 42–65. [Google Scholar]
- 21. Mercer TH, Koufaki P, Naish PF. Nutritional status, functional capacity and exercise rehabilitation in end-stage renal disease. Clin Nephrol 2004; 61(Suppl 1):S54–9. [PubMed] [Google Scholar]
- 22. Painter P. The importance of exercise training in rehabilitation of patients with end-stage renal disease. Am J Kidney Dis 1994; 24(1 Suppl 1):S2–9; discussion S31–2. [PubMed] [Google Scholar]
- 23. Johansen KL, Painter PL, Sakkas GK, Gordon P, Doyle J, Shubert T. Effects of resistance exercise training and nandrolone decanoate on body composition and muscle function among patients who receive hemodialysis: a randomized, controlled trial. J Am Soc Nephrol 2006; 17(8):2307–14. [DOI] [PubMed] [Google Scholar]
- 24. Kutner NG, Zhang R, Huang Y, Herzog CA. Cardiac rehabilitation and survival of dialysis patients after coronary bypass. J Am Soc Nephrol 2006; 17(4):1175–80. [DOI] [PubMed] [Google Scholar]
- 25. Greenspun B, Harmon RL. Rehabilitation of patients with end-stage renal failure after lower extremity amputation. Arch Phys Med Rehabil 1986; 67(5):336–8. [PubMed] [Google Scholar]
- 26. Czyrny JJ, Merrill A. Rehabilitation of amputees with end-stage renal disease. Functional outcome and cost. Am J Phys Med Rehabil 1994; 73(5):353–7. [DOI] [PubMed] [Google Scholar]
- 27. Cowen TD, Huang CT, Lebow J, DeVivo MJ, Hawkins LN. Functional outcomes after inpatient rehabilitation of patients with end-stage renal disease. Arch Phys Med Rehabil 1995; 76(4):355–9. [DOI] [PubMed] [Google Scholar]
- 28. Garrison SJ, Merritt BS. Functional outcome of quadruple amputees with end-stage renal disease. Am J Phys Med Rehabil 1997; 76(3):226–30. [DOI] [PubMed] [Google Scholar]
- 29. Frank CM, Morton AR. Rehabilitation of geriatric patients on hemodialysis: a case series. Geriatr Today 2002; 5:136–9. [Google Scholar]
- 30. Forrest GP. Inpatient rehabilitation of patients requiring hemodialysis. Arch Phys Med Rehabil 2004; 85(1):51–3. [DOI] [PubMed] [Google Scholar]
- 31. Forrest G, Nagao M, Iqbal A, Kakar R. Inpatient rehabilitation of patients requiring hemodialysis: improving efficiency of care. Arch Phys Med Rehabil 2005; 86(10):1949–52. [DOI] [PubMed] [Google Scholar]
- 32. Li M, Porter E, Lam R, Jassal S. Quality improvement through the introduction of interdisciplinary geriatric hemodialysis rehabilitation care. Am J Kidney Dis 2007; 50(1):90–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jassal SV, Chiu E, Li M. Geriatric hemodialysis rehabilitation care. Adv Chronic Kidney Dis 2008; 15(2):115–22. [DOI] [PubMed] [Google Scholar]
- 34. Guiding principles for the care of older adults with multimorbidity: an approach for clinicians: American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. J Am Geriatr Soc 2012; 60(10):E1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Davison SN, Mayo PR. Pain management in chronic kidney disease: the pharmacokinetics and pharmacodynamics of hydromorphone and hydromorphone-3-glucuronide in hemodialysis patients. J Opioid Manag 2008; 4(6):335–6, 339–44. [PubMed] [Google Scholar]
- 36. Murtagh FE, Chai MO, Donohoe P, Edmonds PM, Higginson IJ. The use of opioid analgesia in end-stage renal disease patients managed without dialysis: recommendations for practice. J Pain Palliat Care Pharmacother 2007; 21(2):5–16. [PubMed] [Google Scholar]
- 37. Tomasello S. Central nervous system medications. Semin Dial 2010; 23(5):469–72. [DOI] [PubMed] [Google Scholar]
- 38. Wyne A, Rai R, Cuerden M, Clark WF, Suri RS. Opioid and benzodiazepine use in end-stage renal disease: a systematic review. Clin J Am Soc Nephrol 2011; 6(2):326–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McQuillan R, Jassal SV. Neuropsychiatric complications of chronic kidney disease. Nat Rev Nephrol 2010; 6(8):471–9. [DOI] [PubMed] [Google Scholar]



