Abstract
With appropriate training and adequate support, it is possible to keep the peritonitis rate of elderly peritoneal dialysis (PD) patients at a highly respectable level. In general, the latest recommendations for the treatment and prevention of PD-related infections by the International Society for Peritoneal Dialysis (ISPD) are applicable to older patients. However, there are minor differences in the spectrum of causative organisms amongst elderly patients, with coagulase-negative staphylococcal species (CNSS) and Enterobacteriaceae species being more common in elderly patients. Elderly PD patients who develop peritonitis have an excessive short-term mortality, and, amongst elderly patients, a high burden of comorbid load increases the risk of relapsing episodes. In addition, technical problems, social difficulties, and concomitant comorbid diseases often have profound effects on the risk of peritonitis as well as its management.
Keywords: Chronic kidney disease, infection, survival
The proportion of elderly people in the general population is increasing, and a similar trend can be observed in patients treated with long-term dialysis. Data from the United States Renal Data System (USRDS) show that over 60% of the end-stage renal disease patients in the US are over the age of 60 (1). Similarly, over half of the new dialysis patients in Hong Kong are now over 60 years of age (2). Peritoneal dialysis (PD) offers many potential advantages, such as a stable internal milieu and less hemodynamic disturbance than hemodialysis (3,4). Worldwide experience also suggests satisfactory tolerance to PD as long-term renal replacement therapy for older patients (5–8).
The Effect of Age on PD-Related Infections
It remains controversial whether older PD patients have a substantially increased risk of peritonitis than their younger counterparts. A number of observational studies published in the 1990s reported that age is not a major risk factor of PD-related peritonitis (9–11), and the peritonitis-free survival is similar between PD patients above and below 65 years of age (12). On the other hand, 3 retrospective studies noted that patients above 65 or 70 years old have a significantly higher peritonitis rate than younger patients (8,13,14), although there is no difference in peritonitis-free survival or the rate of exit-site infection between older and younger patients (8). More recently, a retrospective study of 391 PD patients found that older age (above 65 years) was the only identified risk factor associated with peritonitis (15). Nonetheless, we believe the important clinical question is not whether older PD patients have a higher peritonitis rate than young patients, but whether their absolute peritonitis rate is acceptable. In this regard, a retrospective dialysis registry study of 1,613 patients older than 75 years reported that the median peritonitis-free survival was 32.1 months, and neither the modality of assistance nor the center size was associated with peritonitis risk (16). Similar peritonitis rates amongst older PD patients are observed in many parts of the world. A number of studies have also shown that older PD patients have a similar rate of exit-site or tunnel infection to younger patients (8,17,18), including those who had failed hemodialysis (19) and octogenarians (20). One might therefore conclude that, with appropriate training and adequate support, older PD patients enjoy a very respectable peritonitis rate, although it may be slightly higher than that of young patients.
A number of small-scale studies have explored the specific risk factors for peritonitis amongst older PD patients. Peritonitis-free survival was found to be similar between older patients treated with continuous ambulatory PD and automated PD (21). Three large cohort studies showed that peritonitis rates did not differ between older patients who required assistance for their dialysis exchange and those who could perform the PD exchanges themselves (22–24). Another study also found that the need for a helper for dialysis exchange, as well as the burden of comorbid condition, does not affect the peritonitis rate amongst older PD patients (12). Furthermore, Taskapan et al. (25) recently showed that, with appropriate training of the staff, older PD patients in a nursing home enjoyed an excellent technique survival and a low peritonitis rate. However, in a review of a national PD registry, Nolph et al. (26) found that bedridden elderly patients had higher peritonitis rates than ambulatory ones, which was probably secondary to the increase in the risk of touch contamination and bowel dysfunction. In essence, these studies suggest that physical disability is not a major risk factor for peritonitis in older PD patients, except perhaps for those who are grossly debilitated.
As to the distribution of causative organisms, de Vecchi et al. (8) found no difference between PD patients above 70 years of age and those between 40 and 60. In a retrospective case control study, however, Holley et al. (27) found that peritonitis episodes caused by coagulase-negative staphylococcal species (CNSS) are more common amongst patients above 60 years old than in younger patients. Similarly, our previous study found that although the distribution of gram-positive and gram-negative organisms was similar between older and young PD patients, CNSS and Enterobacteriaceae species were more common in older patients, while Staphylococcus aureus and Pseudomonas species were more commonly identified in young patients (28). Taken together, available evidence suggests a subtle difference in the spectrum of causative organisms between older and young PD patients. It seems highly probable that touch contamination and bowel dysfunction are important underlying causes of peritonitis episodes in older PD patients. To the best of our knowledge, there is no study that explores the difference in causative organism for peritonitis episodes between patients who require assistance for their dialysis exchange and those who could perform the PD exchanges themselves.
Treatment of PD-Related Infections
In general, current ISPD recommendations on the treatment of PD-related infections are applicable to older patients (29). However, older PD patients are commonly malnourished (30,31), and, even though their measured body weight may be similar, the proportion of lean body mass in older patients is typically lower than in young patients (32). Older patients are also more susceptible to dose-related adverse effects of antibiotics, especially the neurotoxicity of third-generation cephalosporin and probably carbapenems (33), as well as the rupture of the Achilles tendon associated with fluoroquinolone therapy (34). Furthermore, older patients are more likely to require multiple hospital admissions and, as a result, to have antibiotic-resistant strains of bacteria as the causative organisms (35). For these reasons, the dosage of antibiotic therapy needs to be tailored individually, and clinicians should actively look out for unexpected adverse effects from the treatment (36). In addition, it is important to advise all patients about the potential side effects that they might experience so that they can contact their responsible clinicians in a timely manner should problems develop.
A considerable proportion of older patients are able to perform dialysis exchange by themselves but, should a peritonitis episode develop, would not be able to administer an intraperitoneal injection, which is more demanding on dexterity and involves the handling of needles. In addition, some patients may transiently become incapable of performing the dialysis procedure during a peritonitis episode because of the acute illness. Although few studies examine these practical aspects of peritonitis management in older patients, clinicians should be vigilant with regard to the specific needs of older patients and, depending on the local healthcare system and the patient's own social support, consider appropriate short-term assistance for dialysis exchange and intraperitoneal injection according to individual patient needs.
A number of studies have examined the impact of age on the outcome of peritonitis episodes. Piccoli et al. (37) previously reported that the direct mortality of PD-related peritonitis increased with age. Similarly, Lim et al. (38) showed that older patients have a higher peritonitis-related mortality than young patients, and Tsai et al. (39) found that old age and diabetes are the 2 major risk factors for adverse outcomes of PD-related peritonitis. Specifically, Barretti et al. (40) noted that the outcome of PD-related peritonitis due to Staphylococcus aureus is negatively influenced by age and diabetic status. Our previous study also showed that mortality related to peritonitis and the risk of relapsing episodes were higher amongst elderly PD patients than younger ones (12). It is the general clinical impression of many nephrologists that a considerable minority group of patients die of nosocomial infection or cardiovascular disease shortly after the initial presentation of peritonitis, presumably because the acute inflammatory insult disturbs the hemodynamic status or atherosclerotic plaque stability. Amongst PD patients over 60 years old, our previous study showed that the burden of comorbidity posed an additional risk of relapsing episode, but not mortality (40). However, there is no evidence to support a longer duration of antibiotic therapy in this group of patients. Taken together, older PD patients who develop peritonitis had an excessive short-term mortality, and, amongst older patients, a high burden of comorbid load increases the risk of relapsing episodes.
Prevention of PD-Related Infections
The latest ISPD recommendations for the prevention of PD-related infections also apply to older patients (41). However, a few practical points relevant to older PD patients should be highlighted.
First, as mentioned previously, older patients are more likely to require recurrent hospital admissions and, as a result, to be colonized by antibiotic-resistant organisms (35). In addition, older PD patients probably have a higher risk of touch contamination than younger ones. Taken together, it seems logical to perform more decontamination measures in older patients. However, there are few published studies in this area to support such a recommendation. Early studies have shown that a single course of mupirocin ointment is effective for the eradication of nasal Staphylococcus aureus carriage amongst hemodialysis patients as well as nursing home residents, while the addition of chlorhexidine bath gives no extra benefit (42,43). Another study showed that intermittent nasal mupirocin application is effective to prevent re-development of Staphylococcus aureus carriage in PD patients (44).
As pointed out by the ISPD recommendations, there is an association between peritonitis due to enteric organisms and severe constipation as well as enteritis (41). The recommendations also state that hypokalemia is associated with an increased risk of enteric peritonitis and should be avoided and, if present, treated (41). Since peritonitis episodes caused by enteric organisms are common amongst older PD patients, it seems logical to pay particular attention to and treat bowel dysfunction and hypokalemia, both of which are commonly present in this group of patients. Similarly, depression is common in older PD patients and has been implicated as a reversible risk factor of peritonitis (41). However, there is no published study on the effect of treating depression on peritonitis rate.
As discussed above, there is no particular increase in the risk of peritonitis in older patients who require assistance for their dialysis exchanges (22). Common clinical sense would indicate that a careful assessment of individual patients' capability, preferably before the insertion of a dialysis catheter, would be important in determining the optimal modality of PD (i.e. continuous ambulatory PD versus machine-assisted PD) and whether special assistance is required for PD exchange (in terms of equipment or personnel). We believe each dialysis unit should develop their own protocol for the assessment, which should include, but not be limited to, tests on eye-sight, dexterity, cognitive function, and personal hygiene. In some instances, a similar test needs to be conducted for the prospective assistant (for example, the patient's spouse). As stated in the ISPD recommendations (41), home visits by a PD nurse are a crucial component of training, helping to detect problems with exchange technique, adherence to protocols, and other environmental and behavior issues that increase the risk of infection and are best dealt with proactively. However, there is no consensus on the optimal timing for home visits for PD patients.
The current ISPD recommendation states that re-training is helpful in reducing peritonitis risk (41), but published data on this area are actually limited. Technique review and retraining are generally advisable after recovery from a peritonitis episode, especially when it is caused by an organism that commonly originates from touch contamination (29,41). Common clinical sense indicates that one should reassess the technique of performing dialysis exchange, and provide re-training if needed, when PD patients develop medical problems that may affect their ability to continue with the dialysis (for example, an acute stroke). In theory, older patients are at risk of progressive decline in their cognitive function. However, it remains unknown whether regular technique review or re-training would help to reduce the rate of peritonitis in older patients. Similarly, although the home environment and social supports may change with time, there has been no report on the role of regular home re-visits for PD patients. Although published data in this area are scarce, it seems sensible to conclude that for the prevention of peritonitis episodes, clinicians should pay particular attention to technical skill and the home environment for older PD patients.
Areas of Uncertainty and Further Research
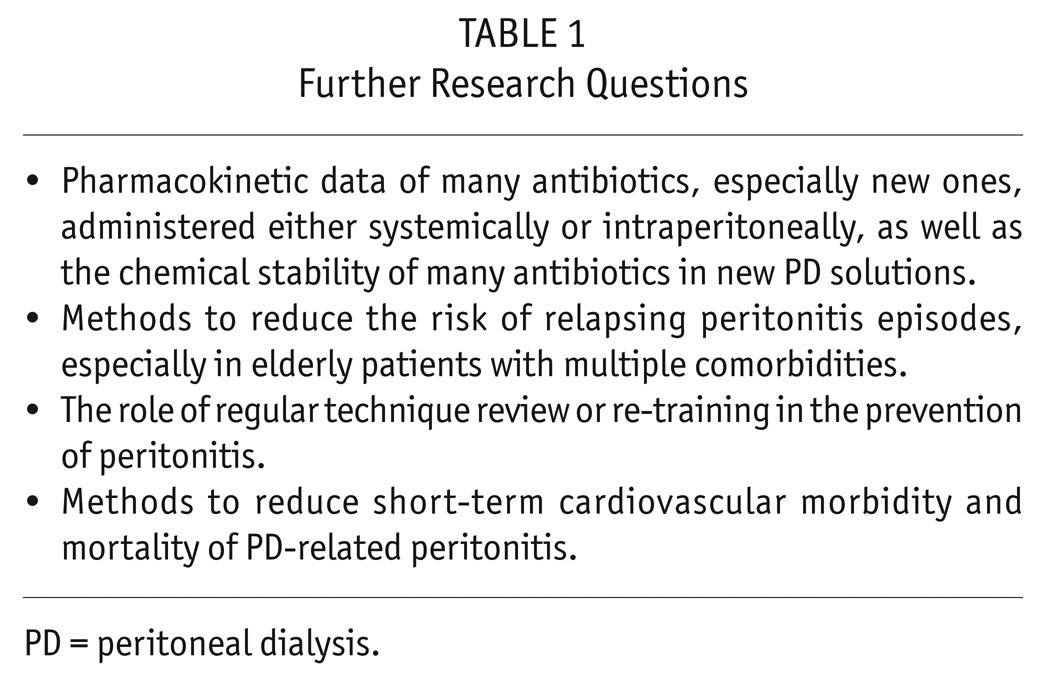
Taken together, the latest ISPD recommendations for the treatment and prevention of PD-related infections are applicable to older patients. However, there are important differences in the epidemiology and clinical behavior of PD-related infections between older and younger PD patients; technical problems, social difficulties, and concomitant comorbid diseases often have profound effects on the risk as well as the management of peritonitis. Based on our literature review, we identify a number of areas, as summarized in Table 1, that deserve special attention for further research.
TABLE 1.
Further Research Questions
Key Points
With appropriate training and adequate support, the peritonitis rate of older peritoneal dialysis (PD) patients is highly respectable.
In general, the recommendations for the treatment and prevention of PD-related infections by the International Society for Peritoneal Dialysis (ISPD) should be followed in older patients.
Older PD patients who develop peritonitis have a high short-term mortality.
Older PD patients with multiple comorbid conditions have an excessive risk of relapsing peritonitis episodes.
Technical problems, social difficulties, and concomitant comorbid diseases often have substantial effects on management of peritonitis in older PD patients.
Disclosures
CCS received a research grant from Baxter Healthcare.
REFERENCES
- 1. United States National Kidney Foundation United States Renal Data System 2012 Annual Data Report: atlas of chronic kidney disease & end-stage renal disease in the United States. Am J Kidney Dis 2013; 61(Suppl 1):e1–e480. [Google Scholar]
- 2. Ho YW, Chau KF, Choy BY, Fung KS, Cheng YL, Kwan TH, et al. Hong Kong renal registry report 2012. Hong Kong J Nephrol 2013; 15:28–43. [Google Scholar]
- 3. Sinnakirouchenan R, Holley JL. Peritoneal dialysis versus hemodialysis: risks, benefits, and access issues. Adv Chronic Kidney Dis 2011; 18:428–32. [DOI] [PubMed] [Google Scholar]
- 4. Tokgoz B. Clinical advantages of peritoneal dialysis. Perit Dial Int 2009; 29(Suppl 2):S59–61. [PubMed] [Google Scholar]
- 5. Laplante S, Krepel H, Simons B, Nijhoff A, van Liere R, Simons M. Offering assisted peritoneal dialysis is a cost-effective alternative to the current care pathway in frail elderly Dutch patients. Int J Healthc Manag 2013; 6:27–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lee S, Ryu JH, Kim H, Kim KH, Ahn HS, Hann HJ, et al. An assessment of survival among Korean elderly patients initiating dialysis: a national population-based study. PLOS ONE 2014; 9:e86776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Power A, Brown E. Optimising treatment of end-stage renal disease in the elderly. Nephron Clin Pract 2013; 124:202–8. [DOI] [PubMed] [Google Scholar]
- 8. De Vecchi AF, Maccario M, Braga M, Scalamogna A, Castelnovo C, Ponticelli C. Peritoneal dialysis in nondiabetic patients older than 70 years: comparison with patients aged 40 to 60 years. Am J Kidney Dis 1998; 31:479–90. [DOI] [PubMed] [Google Scholar]
- 9. Ross CJ, Rutsky EA. Dialysis modality selection in the elderly patient with ESRD: advantages and disadvantages of peritoneal dialysis. Adv Perit Dial 1990; 6(Suppl):11–8. [Google Scholar]
- 10. Gokal R. CAPD in the elderly – European and UK experience. Adv Perit Dial 1990; 6(Suppl):38–40. [Google Scholar]
- 11. Segoloni GP, Salomone M, Piccoli G. CAPD in the elderly: Italian multicentric study experience. Adv Perit Dial 1990; 6(Suppl):41–6. [Google Scholar]
- 12. Li PK, Law MC, Chow KM, Leung CB, Kwan BC, Chung KY, et al. Good patient and technique survival in elderly patients on continuous ambulatory peritoneal dialysis. Perit Dial Int 2007; 27(Suppl 2):S196–201. [PubMed] [Google Scholar]
- 13. Baek MY, Kwon TH, Kim YL, Cho DK. CAPD, an acceptable form of therapy in elderly ESRD patients: a comparative study. Adv Perit Dial 1997; 13:158–61. [PubMed] [Google Scholar]
- 14. Okayama M, Inoue T, Nodaira Y, Kimura Y, Nobe K, Seto T, et al. Aging is an important risk factor for peritoneal dialysis-associated peritonitis. Adv Perit Dial 2012; 28:50–4. [PubMed] [Google Scholar]
- 15. Hsieh YP, Chang CC, Wen YK, Chiu PF, Yang Y. Predictors of peritonitis and the impact of peritonitis on clinical outcomes of continuous ambulatory peritoneal dialysis patients in Taiwan – 10 years' experience in a single center. Perit Dial Int 2014; 34:85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Castrale C, Evans D, Verger C, Fabre E, Aguilera D, Ryckelynck JP, et al. Peritoneal dialysis in elderly patients: report from the French Peritoneal Dialysis Registry (RDPLF). Nephrol Dial Transplant 2010; 25:255–62. [DOI] [PubMed] [Google Scholar]
- 17. Ferńandez MA, Ortiz AM, Valenzuela M, Morales RA. Peritoneal dialysis in chronic renal failure patients over 65 years of age. Adv Perit Dial 2004; 20:128–31. [PubMed] [Google Scholar]
- 18. Dimkovic N, Oreopoulos DG. Chronic peritoneal dialysis in the elderly. Semin Dial 2002; 15:94–7. [DOI] [PubMed] [Google Scholar]
- 19. Onime A, Tzamaloukas AH, Servilla KS, Hartshorne MF. Peritoneal dialysis as salvage renal replacement therapy after complete failure of hemodialysis access in an elderly patient with multiple comorbidities. Adv Perit Dial 2007; 23:118–21. [PubMed] [Google Scholar]
- 20. Dimkovic NB, Prakash S, Roscoe J, Brissenden J, Tam P, Bargman J, et al. Chronic peritoneal dialysis in octogenarians. Nephrol Dial Transplant 2001; 16:2034–40. [DOI] [PubMed] [Google Scholar]
- 21. Kwan BC, Chow KM, Ma TK, Yu V, Law MC, Leung CB, et al. Automated peritoneal dialysis in Hong Kong: there are two distinct groups of patients. Nephrology (Carlton) 2013; 18:356–64. [DOI] [PubMed] [Google Scholar]
- 22. Issad B, Benevent D, Allonache M, Durand PY, Aguilera D, Milongo R, et al. 213 elderly uremic patients over 75 years of age treated with long-term peritoneal dialysis: a French multicenter study. Perit Dial Int 1996; 16(Suppl 1):S414–8. [PubMed] [Google Scholar]
- 23. Lobbedez T, Verger C, Ryckelynck JP, Fabre E, Evans D. Is assisted peritoneal dialysis associated with technique survival when competing events are considered? Clin J Am Soc Nephrol 2012; 7:612–8. [DOI] [PubMed] [Google Scholar]
- 24. Xu R, Zhuo M, Yang Z, Dong J. Experiences with assisted peritoneal dialysis in China. Perit Dial Int 2012; 32:94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Taskapan H, Tam P, Leblanc D, Ting RH, Nagai GR, Chow SS, et al. Peritoneal dialysis in the nursing home. Int Urol Nephrol 2010; 42:545–51. [DOI] [PubMed] [Google Scholar]
- 26. Nolph KD, Lindblad AS, Novak JW, Steinberg SM. Experiences with the elderly in the National CAPD registry. Adv Perit Dial 1990; 6(Suppl):33–7. [Google Scholar]
- 27. Holley JL, Bernardini J, Perlmutter JA, Piraino B. A comparison of infection rates among older and younger patients on continuous peritoneal dialysis. Perit Dial Int 1994; 14:66–9. [PubMed] [Google Scholar]
- 28. Szeto CC, Leung CB, Chow KM, Kwan BC, Law MC, Wang AY, et al. Change in bacterial aetiology of peritoneal-dialysis-related peritonitis over ten years: experience from a center in South-East Asia. Clin Microbiol Infect 2005; 10:837–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Li PK, Szeto CC, Piraino B, Bernardini J, Figuiredo AE, Gupta A, et al. Peritoneal dialysis-related infections recommendations: 2010 update. Perit Dial Int 2010; 30:393–423. [DOI] [PubMed] [Google Scholar]
- 30. Lacquaniti A, Bolignano D, Campo S, Perrone C, Donato V, Fazio MR, et al. Malnutrition in the elderly patient on dialysis. Ren Fail 2009; 31:239–45. [DOI] [PubMed] [Google Scholar]
- 31. Brown EA, Johansson L. Epidemiology and management of end-stage renal disease in the elderly. Nat Rev Nephrol 2011; 7:591–8. [DOI] [PubMed] [Google Scholar]
- 32. Johansen KL, Dalrymple LS, Delgado C, Kaysen GA, Kornak J, Grimes B, et al. Association between body composition and frailty among prevalent hemodialysis patients: a US Renal Data System special study. J Am Soc Nephrol 2014; 25:381–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chow KM, Szeto CC, Hui AC, Wong TY, Li PK. Retrospective review of neurotoxicity induced by cefepime and ceftazidime. Pharmacotherapy 2003; 23:369–73. [DOI] [PubMed] [Google Scholar]
- 34. Wise BL, Peloquin C, Choi H, Lane NE, Zhang Y. Impact of age, sex, obesity, and steroid use on quinolone-associated tendon disorders. Am J Med 2012; 125(12):1228.e23–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Oliveira LG, Luengo J, Caramori JC, Montelli AC, Cunha Mde L, Barretti P. Peritonitis in recent years: clinical findings and predictors of treatment response of 170 episodes at a single Brazilian center. Int Urol Nephrol 2012; 44:1529–37. [DOI] [PubMed] [Google Scholar]
- 36. Farag A, Garg AX, Li L, Jain AK. Dosing errors in prescribed antibiotics for older persons with CKD: a retrospective time series analysis. Am J Kidney Dis 2014; 63:422–8. [DOI] [PubMed] [Google Scholar]
- 37. Piccoli G, Quarello F, Salomone M, Bonello F, Paciffi A, Beltrame G, et al. Dialysis in the elderly: comparison of different dialysis modalities. Adv Perit Dial 1990; 6(Suppl):72–81. 1982844 [Google Scholar]
- 38. Lim WH, Dogra GK, McDonald SP, Brown FG, Johnson DW. Compared with younger peritoneal dialysis patients, elderly patients have similar peritonitis-free survival and lower risk of technique failure, but higher risk of peritonitis-related mortality. Perit Dial Int 2011; 31:663–71. [DOI] [PubMed] [Google Scholar]
- 39. Tsai CC, Lee JJ, Liu TP, Ko WC, Wu CJ, Pan CF, et al. Effects of age and diabetes mellitus on clinical outcomes in patients with peritoneal dialysis-related peritonitis. Surg Infect (Larchmt) 2013; 14:540–6. [DOI] [PubMed] [Google Scholar]
- 40. Barretti P, Moraes TM, Camargo CH, Caramori JC, Mondelli AL, Montelli AC, et al. Peritoneal dialysis-related peritonitis due to Staphylococcus aureus: a single-center experience over 15 years. PLOS ONE 2012; 7:e31780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Piraino B, Bernardini J, Brown E, Figueiredo A, Johnson DW, Lye WC, et al. ISPD position statement on reducing the risks of peritoneal dialysis-related infections. Perit Dial Int 2011; 31:614–30. [DOI] [PubMed] [Google Scholar]
- 42. Watanakunakorn C, Brandt J, Durkin P, Santore S, Bota B, Stahl CJ. The efficacy of mupirocin ointment and chlorhexidine body scrubs in the eradication of nasal carriage of Staphylococcus aureus among patients undergoing long-term hemodialysis. Am J Infect Control 1992; 20:138–41. [DOI] [PubMed] [Google Scholar]
- 43. Watanakunakorn C, Axelson C, Bota B, Stahl C. Mupirocin ointment with and without chlorhexidine baths in the eradication of Staphylococcus aureus nasal carriage in nursing home residents. Am J Infect Control 1995; 23:306–9. [DOI] [PubMed] [Google Scholar]
- 44. Mylotte JM, Kahler L, Jackson E. “Pulse” nasal mupirocin maintenance regimen in patients undergoing continuous ambulatory peritoneal dialysis. Infect Control Hosp Epidemiol 1999; 20:741–5. [DOI] [PubMed] [Google Scholar]


