Abstract
Background: The intestinal coccidian protozoa Cyclospora cayetanensis has emerged as an important cause of parasitic diarrhea among children living in developing countries. This study aimed to determine the prevalence of Cyclospora among the school children of Kathmandu with reference to various associated risk factors.
Methodology: A total of five hundred and seven stool samples from students between the age of 3–14 years, studying in 13 different schools in Kathmandu were collected during the study period (May–November, 2014) and processed at the Public Health Research Laboratory, Institute of Medicine, Kathmandu, Nepal. A modified acid fast staining technique (Kinyoun’s method) was used to detect oocyst of Cyclospora from the formal-ether concentrated stool samples.
Results: Cyclospora was detected in 3.94% (20/507) of the stool samples examined. The prevalence was found to be highest among the students in the 3–5 year age group i.e. 10.15% (13/128), peaking during the rainy season (June–August). The detection rate was found to be significantly higher (p < 0.05) among children presenting with diarrheal symptoms, household keeping livestock and consumers of raw vegetables/fruits, showing a prevalence of 10.57% (11/104), 10.11% (9/89) and 7.25% (14/193) respectively.
Conclusion: Consumption of untreated drinking water, fresh produce (raw fruits/vegetables) without proper washing and the presence of livestock at home were found to be predisposing factors for higher susceptibility of infection due to Cyclospora. This finding confirms the existence of a public-health issue with potentially serious consequences whereby children can be infected through exposure to oocysts in contaminated food and water and get ill as a result.
Keywords: Cyclospora cayetanensis, School Children, Prevalence and Kathmandu
Introduction
The coccidian parasite Cyclospora cayetanensis has been recognized as a new cause of prolonged diarrhea among children in developing countries [1, 2]. The organism produces environmentally resistant oocysts, which are excreted in the feces of the infected individuals [3]. The major risk factors associated with the transmission of the parasite have been identified as the consumption of oocysts in contaminated water and contaminated food produce [3–6]. Direct person-to-person transmission is unlikely because the immature oocysts that are shed in feces require days or weeks in the environment to become infective [7]. Patients normally report symptoms of nausea, vomiting, anorexia leading to weight loss, abdominal cramping and pain with increased gas, flatulence, fatigue and watery diarrhea [8–10]. The modified acid fast staining technique and hot safranin staining technique can be used to detect the oocysts of the parasite from the stool samples [11, 12]. Children in lower age groups are more susceptible to infection with Cyclospora due to a less developed immune system and poor personal hygiene [1]. Little data is available on the prevalence of Cyclospora among school children in Nepal [4, 13–16]. To the best of our knowledge, this is one of the few studies carried out to assess the prevalence of Cyclospora infection under endemic conditions with primary focus on school children. This study is expected to provide a deeper insight into the prevalence of Cyclospora among apparently healthy school children and thereby to encourage further studies in immunocompetent hosts.
Methods
Study site and study population
The study was conducted in Kathmandu, the capital city of Nepal from May to November 2014. Kathmandu is situated at an average elevation of 1,400 meters (4,600 ft) above the sea level and has an approximate population density of 4,416 per square km within a total area of 50.67 square kilometers (19.56 sq. mi).
The study population was school children between the ages of 3–14 years. Thirteen different schools were selected randomly for the study purpose from among the schools within Kathmandu district. A total of five hundred and seven stool samples were collected during the school hour from children at the selected schools.
Study design, sample collection and transportation
The cross-sectional type study was conducted among the school children of Kathmandu. Non-probability sampling technique was adopted for the study. Fresh stool specimens were collected in a clean, dry, screw-capped, leak-proof plastic container. Students were advised to bring about 30 grams or nearly 30 ml of stool sample and to avoid contamination with urine, water and other substances. The single stool specimen collected from each student was then transported, maintaining cold chain, as quickly as possible to the Public Health Research Laboratory, Institute of Medicine, Kathmandu for laboratory examination.
Fecal examination and microscopy
Macroscopic examination was done by observing the stool sample with the naked eye, and information on: consistency, presence/absence of mucus and blood was recorded before microscopic examination of the samples. The fecal samples were then processed by direct-smear technique, in both normal saline solution and 1% iodine solution after formalin ether concentration for the identification of protozoa and helminthes [17, 18]. Fecal samples suspected by direct wet mount to contain Cyclospora-like organisms were selected for further laboratory investigation using a modified acid fast staining technique (Kinyoun’s method) for the identification of oocysts of Cyclospora by microscopy [11, 18]. A commercially available staining reagent (HIMedia K005 for ZN Acid Fast Stains) was used for staining of the stool samples. The morphology of the stained oocysts was then observed and dimensions measured using cell sensation software version 1.12 for DP73 camera installed to the Olympus BX53 microscope used for the microscopy. A positive control slide provided by CDC was observed side by side during the microscopy of stool samples to prevent any discrepancy in the identification. No additional confirmatory testing such as Cyclospora direct fluorescent antibody staining was performed in the course of this study.
Data analysis
The data obtained were entered in MS Excel version 2007 and analyzed using SPSS version 16 for Windows. Two-tailed Pearson’s Chi-square test was used to test the significance of attributes between study variables. A value of α < 0.05 was assumed wherever applicable, and 95% confidence interval along with the exact p-values was represented. The p-value < 0.05 was considered statistically significant.
Ethical considerations
This study was approved by the Institutional Review Board, Institute of Medicine, Research Department, Kathmandu, Nepal [Ref: 282(6-11-E)2]. Prior to sample collection, a questionnaire on various demographic, socio-economic and health-related parameters was completed with the help of teachers and sent to parents in order to gather further information related to each subject after obtaining the necessary written/oral informed consent from teachers and parents.
Results
Among the 507 participants, 236 were male and 271 were female. Cyclospora oocysts were detected in 3.94% (20/507) of the children examined (8 males and 12 females, gender ratio 1:1.5). Cyclospora, Giardia co-infection was seen in 35% (7/20) and Cyclospora, Cryptosporidium co-infection in 5% (1/20) of the Cyclospora positive cases.
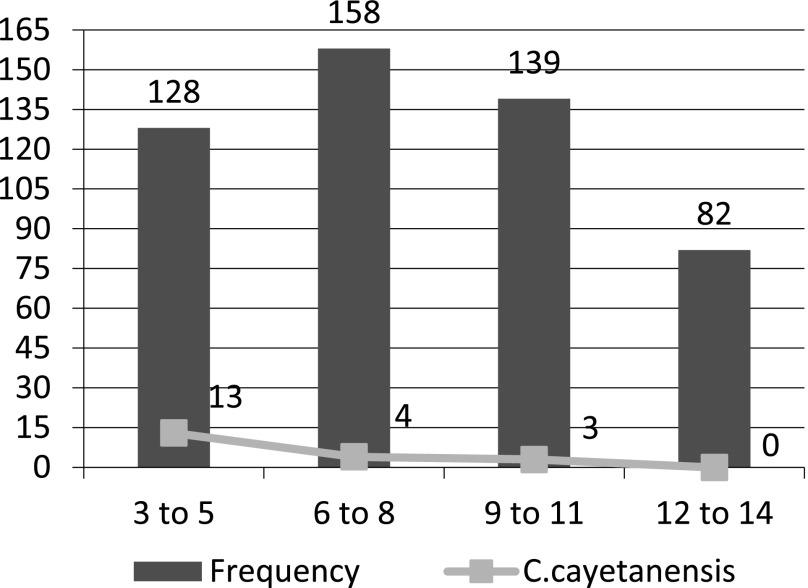
Age-wise distribution of the children with Cyclospora infection:
Age-wise distribution of the Cyclospora infected cases showed the highest prevalence of 10.15% (13/128) among children in the 3–5 year age-group, followed by the children in the 6–8 year age-group, i.e., 2.53% (4/158) as shown in Fig. 1.
Fig. 1.
Age-wise distribution of Cyclospora infection.
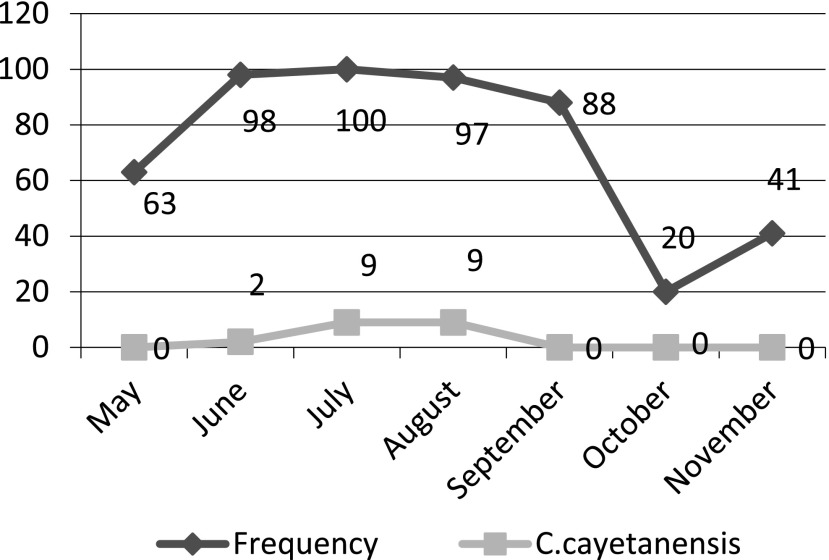
Month-wise detection pattern of Cyclospora oocysts
The monthly distribution pattern of Cyclospora infection showed the highest infection rate during the month of August, i.e., 9.8% (9/97) followed by July, i.e., 9% (9/100) and June, i.e., 2.04% (2/98) with no infection detected during the month of May, September, October or November (Fig. 2).
Fig. 2.
Monthly detection pattern of Cyclospora oocyst.
Clinical characteristics of children with Cyclospora infection
Out of the 507 participants, 20.51% (104/507) were symptomatic while remaining 79.49% (403/507) were asymptomatic. Among the 20 cases found to be positive for Cyclospora oocyst in the stool sample, 11 had diarrhea-like symptoms while 9 had no diarrhea-related symptoms (Table 1). The diarrheal episode among the 11 cases ranged from 5 days to 9 days.
Table 1.
Distribution of Cyclospora infection among children with and without diarrhea related symptoms.
| Case type | Cyclospora positive | Cyclospora negative | Total |
|---|---|---|---|
| Presence of Diarrhea related symptoms | 11 (10.57%) | 93 | 104 |
| Absence of diarrhea related symptoms | 9 (2.23%) | 394 | 403 |
| Grand Total | 20 (3.94%) | 487 | 507 |
[χ2cal = 15.18, p = 9.7 × 10−5]
Mode of drinking water consumption and Cyclospora infection
Out of the total participants, 1.2% (3/244) of the children consuming treated water and 6.46% (17/263) consuming untreated water for drinking purpose were found to be positive for Cyclospora oocyst (Table 2).
Table 2.
Distribution of Cyclospora infection on the basis of mode of drinking water consumption.
| Mode of water consumption | Cyclospora positive | Cyclospora negative | Total |
|---|---|---|---|
| Consumers of treated water | 3 (1.22%) | 241 | 244 |
| Consumers of untreated water | 17 (6.46%) | 246 | 263 |
| Grand Total | 20 (3.94%) | 487 | 507 |
[χ2cal = 9.152, p = 0.002484]
Livestock presence at home and Cyclospora infection
Among the total 20 cases found to be positive for Cyclospora oocysts, nine children reared livestock at their home while 11 did not have any form of livestock at home (Table 3).
Table 3.
Distribution of Cyclospora infection on the basis of livestock presence at home.
| Livestock | Cyclospora positive | Cyclospora negative | Total |
|---|---|---|---|
| Livestock presence at home | 9 (10.11%) | 80 | 89 |
| Livestock absence at home | 11 (2.63%) | 407 | 418 |
| Grand Total | 20 | 487 | 507 |
[χ2cal = 10.837, p = 0.000995]
Fresh produce (raw fruits/vegetables) consumption practice among the children and Cyclospora infection
With regard to fresh produce consumption, Cyclospora infection was found to be present in 7.25% (14/193) of the children consuming raw vegetables/fruits without proper washing compared to 1.91% (6/314) of those not consuming raw vegetables/fruits (Table 4).
Table 4.
Distribution of Cyclospora infection on the basis of fresh produce (raw vegetable/fruits) consumption habit.
| Fresh produce consumption | Cyclospra positive | Cyclospora negative | Total |
|---|---|---|---|
| Raw vegetables/fruits consumers | 14 (7.25%) | 179 | 193 |
| Non consumers of raw vegetables/fruits | 6 (1.91%) | 308 | 314 |
| Total | 20 | 487 | 507 |
[χ2cal = 9.0057, p = 0.002691]
Discussion
Cyclospora infection is generally associated with diarrhea among children in developing countries while traveler’s diarrhea, food and waterborne outbreaks usually occur in developed countries [1, 19]. The disease is endemic to Nepal, remaining asymptomatic with annual reported cases of cyclosporiasis as high as 40% [20]. In the context of Nepal, poor hygiene among children and the lack of proper sanitary practices favor the infection of Cyclospora, which was found to be the case in our study as well. The infection rate of Cyclospora in our study was lower than the prevalence of 7.9% reported in another study conducted among diarrheal children in Nepal [16]. A prevalence of 2.22% of Cyclospora infection, which is similar to our finding, was reported in a study conducted among school children in Thailand [21]. The highest risk of infection of Cyclospora occurs in the first five years of life [1, 22–25], which is consistent with our finding of a higher infection rate among children in the 3–5 year age group. Diarrhea is one of the important symptoms of cyclosporiasis [8]. Parameters like diarrheal complaint and frequency, abdominal pain, vomiting and fever were taken as indices to determine the symptomatic cases and asymptomatic cases, accessed through a questionnaire during the study. The higher detection rate of Cyclospora oocysts among children presenting with diarrheal symptoms in our study was statistically significant (p < 0.05). Cyclospora infection markedly increases during the warm and rainy season, a fact that reflects the increased oocyst contamination of surface and domestic water supplies [4, 5, 14, 26]. In our study the prevalence of Cyclospora infection was found to be higher during the months of June, July and August, which mark the peak of the monsoon season in this part of the world. This finding is in harmony with previous studies conducted in Nepal [4, 14, 27]. Waterborne oocysts are a common source of infection for Cyclospora [3]. Oocysts of Cyclospora have been reported to be resistant to chlorination [28, 29]. We considered water consumed after implementing any method including roll boiling for five minutes, filtration using conventional ceramic candle filter (pore size 1–5 μm), EuroguardTM and bottled mineral water as treated water. The higher detection rate of Cyclospora oocysts among the children consuming untreated water in our study was found to be statistically significant (p < 0.05). In Kathmandu, the municipal supply of tap water is the major source of drinking water. However, there is a flaw in the supply system, namely the fact that the sewage drainage and water supply pipelines run parallel to each other in very close proximity and that the water supply can be contaminated through seepage into the pipes from sewage [16]. Thus, fecal contamination of drinking water could be the reason behind the higher prevalence of Cyclospora among children drinking municipal tap water without adopting any treatment measure. Meanwhile, the role of animals as a natural reservoir of C. cayetanensis is uncertain but of increasing concern [2]. Domestic animals have been implicated as a risk factor for Cyclospora infection [25, 30]. Oocysts resembling those of C. cayetanensis have been described in several animals, including chickens, ducks, mice, rats, dogs and primates from different parts of Nepal [4]. This study endeavored to find out the relation between livestock rearing and the risk of infection with Cyclospora. A significant relationship (p < 0.05) between Cyclospora infection and presence of livestock at home was seen in this study. Contamination of food has long been proposed as a possible route for transmission of Cyclospora [10]. The detection rate of Cyclospora oocysts was significantly higher (p < 0.05) among the students who consumed fresh produce (raw vegetables/fruits) without proper washing. In Kathmandu, human excreta are frequently used as manure in raising crops. Likewise, open defecation by children in fields and free grazing of cattle along riversides is seen. These practices can lead to contamination of river water which in turn is used to irrigate fields and wash harvested crops. Thus, the contamination of vegetables by the oocysts occurs, resulting in the higher infection rate among consumers of raw vegetables and fruits. Furthermore, the oocysts of Cyclospora are shed unsporulated and can remain in the environment under harsh conditions for a longer time maintaining infectivity [3].
Conclusion
The results obtained from this study implicates Cyclospora to be an important cause of childhood diarrhea, associated with consumption of untreated drinking water, fresh produce without proper washing and livestock presence at home. Efforts to supply safe drinking water and conduct health education could be some of the practical arbitration measures needed to control the infection of Cyclospora in developing countries.
Acknowledgements
We would like to thank Mr. Naveen Shrestha for helping with the manuscript review as well as statistical analysis. We are also grateful to Mrs. Sarala Sherchand and the entire team of the Research Department, Institute of Medicine, Nepal for their support and encouragement during the study. We are in debt to all the participants of this research program, without whose contribution it would not have been a success.
Conflict of Interest Statement
We declare that we have no conflict of interest.
References
- 1.Ortega YR, Sterling CR, Gilman RH. Cyclospora cayetanensis. Adv Parasitol 1998; 40: 399–418. [DOI] [PubMed] [Google Scholar]
- 2.Chacin-Bonilla L. Epidemiology of Cyclospora cayetanensis: A review focusing in endemic areas. Acta Trop 2010; 115: 181–193. [DOI] [PubMed] [Google Scholar]
- 3.Mansfield LS, Gajadhar AA. Cyclospora cayetanensis, a food- and waterborne coccidian parasite. Vet Parasitol 2004; 126: 73–90. [DOI] [PubMed] [Google Scholar]
- 4.Sherchand JB, Cross JH. Emerging pathogen Cyclospora cayetanensis infection in Nepal. Southeast Asian J Trop Med Public Health 2001; 2: 143–150. [PubMed] [Google Scholar]
- 5.Shields JM, Olson BH. Cyclospora cayetanensis: a review of an emerging parasitic coccidian. Int J Parasitol 2003; 33: 371–391. [DOI] [PubMed] [Google Scholar]
- 6.Herwaldt BL, Beach MJ. The return of Cyclospora in 1997: another outbreak of cyclosporiasis in North America associated with imported raspberries. Cyclospora Working Group. Ann Intern Med 1999; 130: 210–220. [DOI] [PubMed] [Google Scholar]
- 7.Herwaldt B. The ongoing saga of U.S. outbreaks of cyclosporiasis associated with imported fresh produce: what Cyclospora cayetanensis has taught us and what we have yet to learn? Institute of Medicine. Addressing foodborne threats to health: policies, practices, and global coordination. Washington DC: National Academies Press; 2006. pp 85–115. [Google Scholar]
- 8.Brennan MK, MacPherson DW, Palmer J, Keystone JS. Cyclosporiasis: a new cause of diarrhea. Cmaj 1996; 155: 1293–1296. [PMC free article] [PubMed] [Google Scholar]
- 9.Ortega YR, Nagle R, Gilman RH, et al. . Pathologic and clinical findings in patients with cyclosporiasis and a description of intracellular parasite life-cycle stages. J Infect Dis 1997; 176: 1584–1589. [DOI] [PubMed] [Google Scholar]
- 10.Ortega YR, Sanchez R. Update on Cyclospora cayetanensis, a food-borne and waterborne parasite. Clin Microbiol Rev 2010; 23: 218–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baxby D, Blundell N, Hart CA. The development and performance of a simple, sensitive method for the detection of Cryptosporidium oocysts in faeces. J Hyg 1984; 93: 317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Visvesvara GS, Moura H, Kovacs-Nace E, et al. . Uniform staining of Cyclospora oocysts in fecal smears by a modified safranin technique with microwave heating. J Clin Microbiol 1997; 35: 730–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sherchand J, Cross J. Parasitic epidemiological studies of Cyclospora cayetanensis in Nepal. Southeast Asian J Trop Med Pub Health 2004; 35: 1–8. [Google Scholar]
- 14.Kimura K, Rai SK, Rai G, et al. . Study on cyclospora cayetanensis associated with diarrheal disease in Nepal and Loa PDR. Southeast Asian J Trop Med Public Health 2005; 36: 1371–1376. [PubMed] [Google Scholar]
- 15.Sherchand S, Joshi D, Adhikari N, et al. . Cyclosporiasis Among School Going Children of Kathmandu Valley. Nepal J Sci Tech 2010; 11: 193–198. [Google Scholar]
- 16.Sherchan J, Sherpa K, Tandukar S, et al. . Infection of Cyclospora cayetanensis in Diarrheal Children of Nepal. J Nepal Pediatrics Society 2010; 30: 23–30. [Google Scholar]
- 17.Garcia L. Macroscopic and Microscopic Examination of Fecal Specimens. Diagnostic Medical Parasitology. 5th ed. Washington DC: ASM Press; 2007. pp 782–830. [Google Scholar]
- 18.Weber R, Bryan RT, Juranek DD. Improved stool concentration procedure for detection of Cryptosporidium oocysts in fecal specimens. J Clin Microbiol 1992; 30: 2869–2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karanis P, Kourenti C, Smith H. Waterborne transmission of protozoan parasites: a worldwide review of outbreaks and lessons learnt. J Water Health 2007; 5: 1–38. [DOI] [PubMed] [Google Scholar]
- 20.Sherchand J, Cross J, Jimba M, et al. . Study of Cyclosporacayetanensisin health care facilities, sewage water and green leafy vegetables in Nepal. Southeast Asian Journal Trop Med Public Health 1999; 30: 58–63. [PubMed] [Google Scholar]
- 21.Thima K, Mori H, Praevanit R, et al. . Recovery of Cyclospora cayetanensis among asymptomatic rural Thai schoolchildren. Asian Pac J Trop Med 2014; 7: 119–123. [DOI] [PubMed] [Google Scholar]
- 22.Hoge CW, Echeverria P, Rajah R, et al. . Prevalence of Cyclospora species and other enteric pathogens among children less than 5 years of age in Nepal. J Clin Microbiol 1995; 33: 3058–3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Madico G, McDonald J, Gilman RH, et al. . Epidemiology and treatment of Cyclospora cayetanensis infection in Peruvian children. Clin Infect Dis 1997; 24: 977–981. [DOI] [PubMed] [Google Scholar]
- 24.Chacin-Bonilla L, Estevez J, Monsalve F, et al. . Cyclospora cayetanensis infections among diarrheal patients from Venezuela. Am J Trop Med Hyg 2001; 65: 351–354. [DOI] [PubMed] [Google Scholar]
- 25.Bern C, Ortega Y, Checkley W, et al. . Epidemiologic differences between cyclosporiasis and cryptosporidiosis in Peruvian children. Emerg Infect Dis 2002; 8: 581–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Herwaldt BL. Cyclospora cayetanensis: a review, focusing on the outbreaks of cyclosporiasis in the 1990s. Clin Infect Dis 2000; 31: 1040–1057. [DOI] [PubMed] [Google Scholar]
- 27.Ghimire T, Mishra P, Sherchand J. The seasonal outbreaks of Cyclosporaand Cryptosporidium in Kathmandu, Nepal. J Nepal Health Research Council 2005; 3: 39–48. [Google Scholar]
- 28.Rabold JG, Hoge CW, Shlim DR, et al. . Cyclospora outbreak associated with chlorinated drinking water. Lancet 1994; 344 (8933): 1360–1361. [DOI] [PubMed] [Google Scholar]
- 29.Soave R, Herwaldt BL, Relman DA. Cyclospora. Infect Dis Clin North Am 1998; 12: 1–12. [DOI] [PubMed] [Google Scholar]
- 30.el-Karamany EM, Zaher TI, el-Bahnasawy MM. Role of water in the transmission of cyclosporiarsis in Sharkia Governorate, Egypt. J Egypt Soc Parasitol 2005; 35: 953–962. [PubMed] [Google Scholar]