Abstract
Apart from individual alcohol drinking behavior, the context or places where people drink play a significant role in HIV transmission risk. In this paper, we review the research that has been conducted on alcohol venues to identify the social and structural factors (e.g., social norms, sexual behavior) that are associated with HIV risk in these places, to review HIV prevention interventions based in alcohol venues, and to discuss appropriate methodologies for alcohol venue research. Alcohol venues are defined here as places that sell or serve alcohol for onsite consumption, including bars, bottle stores, nightclubs, wine shops, and informal shebeens. Despite the many established HIV risk factors at play in alcohol venues, limited prevention strategies have been implemented in such places. A total of 11 HIV prevention interventions or programs were identified. HIV prevention interventions in alcohol venues may be conducted at the individual, social, or structural level. However, multilevel interventions that target more than one level appear to lead to the most sustainable behavior change. Strategies to incorporate alcohol venues in biomedical prevention strategies including antiretroviral therapy for alcohol users are also discussed.
Keywords: HIV/AIDS, alcohol use, alcohol venues, structural interventions, multilevel interventions
Alcohol use does not occur in a vacuum, and the context or venue in which people drink alcohol has been shown to play an important role in alcohol-related HIV risk. Worldwide, people meet new sex partners in places where alcohol is consumed (1). Further, even after controlling for alcohol use, merely attending an alcohol venue is associated with high-risk sex (2). In recognition of such findings, there have been repeated calls for implementing HIV prevention strategies in alcohol venues (3–5). Unfortunately these calls have mostly gone unanswered, as most studies on alcohol consumption and HIV ignore the venue. However, in order to avert new HIV infections, particularly in places where alcohol use is prevalent, prevention interventions must go beyond the individual to target alcohol venues. In this paper, we review the research that has been done on alcohol venues. Our aims are to provide an overview of the social and environmental factors that may influence HIV risk in alcohol venues, to assess the HIV prevention interventions based in alcohol venues, and to discuss different methodological approaches to venue research. Ultimately, our intent is to provide information about what HIV risk factors might operate in alcohol venues and how to study them in an effort to guide the content and design of HIV prevention interventions in such places.
What are the HIV risk factors in alcohol venues?
Literature Review
We conducted a qualitative review of the literature with the intention of identifying factors in or related to alcohol venues that might influence risk for HIV. We sought to include literature that may subjectively inform this topic from outside the area of HIV or sexual risk behavior. Therefore this review was informal rather than systematic. In our literature search and in this paper we defined alcohol venues, or simply “venues,” as places that sell or serve alcohol for onsite consumption. Therefore, we also include homes in this review. Although alcohol might not necessarily be sold in homes, they sometimes represent places where people go to drink alcohol and socialize (i.e., parties).
We used single search terms or combinations of terms like “alcohol venues;” “bars;” “nightclubs;” and “HIV.” After scanning titles and abstracts, we read articles that were deemed directly (e.g., a study of condom use among patrons in alcohol venues) or indirectly (e.g., a study of violent or aggressive behavior in bars) relevant to alcohol venues and HIV.
In reviewing the literature we recognized that there are many different types of venues in different regions of the world including bars, taverns, bottle stores, dance or nightclubs, and karaoke bars. Specific countries have unique alcohol venues that are well-established HIV risk environments, including wine shops in India and informal shebeens in South Africa. Several populations have also been included in relevant studies, including college students and general populations in Western countries, patrons of formal and informal drinking venues in southern Africa, and men who have sex with men, female sex workers, and male clients from different regions. With these different venues, populations, and regions in mind, we describe the factors in venues that may contribute to higher risk for HIV, starting with distal factors like venues in neighborhoods to more proximal factors like risky sexual behaviors.
Proximity
In general, research has demonstrated that accessibility to alcohol venues is associated with risk for HIV. One study across neighborhoods in Namibia showed that higher density of drinking establishments was associated with higher prevalence of HIV (6). Similar to disparities in HIV, research suggests that alcohol venues are concentrated in disadvantaged minority and lower-income neighborhoods (7). Proximity to drinking venues may elevate both alcohol use and sexual risks for HIV. For example, geo-coded individual-level data combined with alcohol license data in California, U.S. showed that within a one-mile radius of residential homes, the number of alcohol venues is associated with heavy episodic drinking (8). This positive association between alcohol outlet density and both alcohol consumption and alcohol-related harms (e.g., injury, violence) is quite robust among studies in the United States (9–13). However, a study in South Africa showed an opposite pattern – women who attended distant versus nearby informal neighborhood drinking venues known as shebeens reported greater alcohol use and sex partners, and were more likely to report having an STI, including HIV; these patterns were not found among men (14). The authors interpreted this finding in terms of the gender-role norms and social stigma surrounding drinking and sex in South Africa. It may be that among women but not men, attending a more distant venue helps ensure greater anonymity and freedom to engage in riskier behaviors. These findings suggest that culture, gender, and other demographic and contextual factors might moderate the association between alcohol venue proximity and behavioral risks for HIV. Therefore, HIV risk reduction structural interventions that reduce outlet density may have population-specific efficacy.
Physical Characteristics of Venues
Studies of alcohol venues suggest that certain aspects of the physical environment of venues may contribute to alcohol use and alcohol-related harms. In an ethnographic study of nightlife venues that cater to tourists in Sunny Beach, Bulgaria, it was found that overcrowding, shattered glass on the floor, dancing on furniture, and staff practices including a violent security staff and irresponsible alcohol serving were among the most dangerous conditions for patrons (15). Other research suggests that even cues or primes about alcohol use may increase alcohol consumption in venues. An experimental study demonstrated that customers spent more money on alcohol in bars where they were exposed to music that made lyrical references to alcohol, compared to control bars (16). With respect to sexual behavior, venues may have physical characteristics that are more conducive to sex taking place, including dim lighting, dark corners, and uni-sex bathrooms (17). Thus, changing physical aspects of venues may be a worthwhile endeavor for HIV risk reduction interventions.
Confluence of HIV-related Risks in Venues
Singer has theorized about the co-occurrence of substance use, violence, and AIDS or what he has termed “syndemics” among disadvantaged populations (18,19). Generally, research has shown that individuals who report a greater number of psychosocial problems like experiencing violence (e.g., intimate partner violence or childhood abuse), alcohol use, drug use, and poor mental health are at greater risk of HIV via risky sexual behaviors (20–23). Among alcohol venue patrons, this association has been found among women who attend shebeens in South Africa (24). The results from this research suggest a process whereby women who experience violence might cope or respond with greater alcohol use, and/or experience poor mental health, which in turn increases unprotected sex (25). This process involving the confluence of multiple HIV-related risks may be found not only in individuals, but also in places, creating a syndemic-promoting environment. Apart from high rates of drinking, drug use and violence are also likely to co-occur in alcohol venues. These same places afford opportunities to meet sex partners and form the framework for establishing sexual networks.
Drug use, reported both onsite and among patrons, is common in alcohol venues. Nightclubs are venues where alcohol and drugs, particularly “club drugs” (e.g., MDMA or ecstasy), are used in combination and contribute to unsafe sex and alcohol-related harms (26–30). Using club drugs is positively associated with unsafe sex and alcohol use among men who have sex with men (MSM) in the U.S. (31). Not surprisingly, club drug use is associated with increased HIV acquisition risk among MSM after controlling for other factors (32). In college party settings, merely having illicit drugs available has been shown to increase the likelihood of heavy drinking (33). In South Africa, some shebeen-goers have reported that they have used methamphetamine (meth) in a succession of substances, following marijuana and alcohol use (34). Another study among South African shebeen-goers showed that current meth use is associated with numerous sexual risk behaviors for HIV, including multiple partners, condom unprotected sex, transactional sex, and sexually transmitted infection (35). This study also showed that current meth use mediated the relationship between having experienced childhood sexual abuse and subsequent sexual risks for HIV.
Violence, another piece in the HIV syndemic puzzle, is a relatively frequent occurrence among patrons and in alcohol venues. The evidence suggests that people who drink more and/or attend alcohol venues frequently are more likely to perpetrate violence, including childhood physical abuse and intimate partner violence (36,37). For women, consuming more alcohol is associated with a greater likelihood of experiencing violence. A prospective study among shebeen-going women in South Africa found that recent alcohol use mediated the relationship between experience of gender-based violence and engaging in unprotected sex (25). Among female sex workers (FSWs) who work in wine shops in India, consuming alcohol more frequently and before sex was associated with reporting forced sex (38). A study of heterosexual couples in the U.S. showed that men’s, and not women’s drinking in bars or public places (versus quietly at home) was associated with greater reports of both male- and female-perpetrated partner violence (39). While this evidence suggests that individuals who attend alcohol venues are more likely to experience violence, there is also evidence that violence and aggression are relatively frequent occurrences within the setting of alcohol venues. Heavy drinking, particularly among men in public versus private places, has been shown to increase the likelihood of alcohol-related aggression, fighting, and injury (40,41). Barroom aggression between men appears to occur as a function of the combination of alcohol use, alcohol expectancies, and environmental characteristics of the bar (42,43). In sum, the convergence of alcohol use, drug use, and violence may contribute to varying degrees of risk in alcohol venues, or even across different times within a venue. Research has yet to systematically examine whether the confluence of multiple risk factors may increase sexual risks for HIV across alcohol venues.
Venue Staff
Owners, managers, bartenders, and other venue staff play important roles in influencing HIV risks in venues. For example, research suggests that door staff (i.e., “bouncers”) sometimes encourage aggressive behavior (44), and that bartenders themselves consume alcohol during working hours (45). However, venue staff influence the health and safety of patrons particularly through their alcohol serving practices. It is illegal to sell alcohol to individuals who appear obviously intoxicated occurs, and yet it occurs. Studies using actors who feign intoxication while attempting to purchase alcohol have shown that these pseudo-intoxicated patrons are successful in their attempts over 50% of the time (46–48). For example, in one study across 135 on-premise venues (i.e., establishments that sell alcohol for onsite consumption) across neighborhoods in Northern California in the U.S. the actors were able to purchase alcohol in 58% of attempts (48). In a larger study of 372 venues that included both off- and on-premise venues in 11 communities in the U.S., 79% of venues sold alcohol to the actors/patrons (47). In Tijuana, Mexico most if not all sex work venues have an unwritten policy that a male client must purchase at least 2 alcoholic beverages before transactional sex takes places with the FSW. Interventions should engage venue staff and owners to promote responsible alcohol serving and to change policies that increase HIV risk. To encourage cooperation, researchers must fully engage venue owners and staff in the process, from intervention development to dissemination of findings (e.g., formation of community advisory boards that include venue owners and staff). Interventions that focus on manager training to promote responsible alcohol serving practices appear to show promise in reducing illegal alcohol sales. For example, in one randomized trial evaluating the efficacy of a training program for venue owners and managers sale rates to pseudo-intoxicated patrons reduced 23%, but returned to baseline 3 months later (49). Thus, intervening solely with venue staff is insufficient to sustain reduced risks for HIV.
Social Norms and Influence
As places that serve alcohol, alcohol venues implicitly promote norms to consume. Therefore, although individuals may have different motivations for patronizing venues (e.g., socializing, meeting sex partners), they may end up consuming more alcohol than planned. In Tijuana, Mexico, bars represent the primary places where male clients meet FSWs. Male clients have described these venues as high risk partly as a function of social norms dictating heavy alcohol consumption (50). One study compared alcohol-serving to non-serving commercial sex venues among FSWs in Guangxi, China on both alcohol use and on “pro-alcohol social environment,” measured in terms of institutional norms (e.g., clients ask and mammies require FSWs to drink), institutional practices (e.g., drinking during work), risk perception (e.g., alcohol makes clients happier), and peer norms (e.g., the majority of other FSWs drink) (51). Results showed that FSWs in alcohol-serving commercial sex venues reported a higher pro-alcohol social environment than FSWs in non-alcohol-serving venues, and that within alcohol-serving venues, a higher pro-alcohol environment was associated with more hazardous drinking. Another study of college students across California universities used mathematical modeling to show that within settings light drinkers can become moderate drinkers when moderate drinkers spend more time in these settings, and that moderate drinkers may change environments and become heavy drinkers (52). In sum, patrons of alcohol venues appear to form a social network through which higher or lower norms for heavy alcohol use are promoted.
Sex Relations in Alcohol Venues
Apart from being influenced by the more distal factors reviewed thus far, alcohol venues are high-risk places for HIV particularly because they are places where alcohol use and sex commonly intersect. The Priorities for Local AIDS Control Efforts (PLACE) method is an assessment tool to identify places where HIV transmission is most likely to occur (1,53). In studies conducted across multiple regions, including Mexico, South Africa, Zimbabwe, Central Asia, and Russia approximately 75% of places where people meet new sex partners are alcohol venues (54–57). In South Africa, the proportion is 94%. In a study of South African shebeen-goers, for both men and women and controlling for confounds, those who reported meeting sex partners in shebeens were more likely to have a pattern of higher risk behaviors for HIV compared to those who did not report meeting sex partners in shebeens (58). Other research conducted in South African shebeens has shown that gender-mutually understood norms exist in which women agree to have sex in exchange for accepting alcohol from a man (59,60). There is also evidence that sexual intercourse sometimes takes place within dark corners of shebeens, or that patrons seek out places like the toilets or behind the house (17).
Alcohol venues increase the likelihood of alcohol use in sexual contexts, which has been shown to be associated with condom unprotected sex (61,62). In a population-based study in Zimbabwe, ever attending a beer hall was associated with more risky sexual behavior, experiencing STI symptoms, and being infected with HIV (63). Among FSWs in Indonesia and Thailand, meeting clients in alcohol venues versus brothels is associated with higher alcohol use prior to sex with clients (64)(65). A similar finding was reported by a national study of MSM in the U.S.; men who reported meeting their most recent new male sex partner in a bar versus online or in a bathhouse were most likely to report alcohol use prior to or during sex (66). There is also evidence that venues moderate the association between sex with alcohol and unprotected sex. In one study among male clients of FSWs in Tijuana, Mexico, reporting more frequent intoxication during sex was associated with greater unprotected sex but only among men who reported meeting FSWs in a bar versus somewhere else (67). Overall, the evidence suggests that alcohol venues promote risky sexual behavior and condomless sex in different ways. These ways include serving as the primary places where new sex partners are met, through norms promoting not only alcohol use but also sex, and by increasing the likelihood of alcohol use occurring before or during sex.
Prevention Strategies in Venues
Despite the known intersection of alcohol use and sex in alcohol venues, condoms and health behavior messages appear to be rarely found in venues. A study of high risk places, the majority of which were alcohol venues in Zambia found that a substantial proportion did not have condoms available, and that reported condom use was lower in places where condoms were not available (68). A population-based survey in Zimbabwe found that less than 5% of respondents who have been to a beer hall reported experiencing an HIV prevention activity in a beer hall in the last 6 months (63). MSM who were surveyed in bars/clubs versus bathhouses or on the internet reported being the least likely to be interested in seeing more information on HIV and interacting with a health outreach worker (69). Thus, researchers must discover strategies that increase the engagement of venue patrons in HIV prevention (e.g., health messages, condom distribution, HIV testing).
Contextual influence versus self-selection: What is the direction of the relationship?
Factors related to alcohol venues may work to increase people’s risks for HIV, or people with certain characteristics may seek out venues that cater to their social and behavioral preferences. Although not studied in terms of risks for HIV, alcohol researchers have tested these directional hypotheses of social influence versus self-selection for some time. In 1987, a Canadian national survey showed that patrons of taverns, lounges, nightclubs and private clubs differ in sociodemographics that are related to the social functions associated with the different types of venues, lending support to the self-selection hypothesis (70). Another study conducted with a general population sample in the U.S. demonstrated similar results such that age, gender, and ethnicity were associated with selection of different drinking locations (71). Gruenewald subsequently proposed a social ecological model to argue that complementary processes exist in which alcohol sellers “niche market” to specific types of drinkers, drinkers attend and return to venues where they find similar others, and in turn the social stratification increases levels of alcohol-related problems in specific venues (72). Support for this model was found in a multilevel study using a general population sample from fifty cities throughout California, suggesting that indeed, contexts and drinker characteristics act jointly to influence alcohol consumption and alcohol-related harms (73). The implications of these findings are that interventions that target both individual and venue characteristics should function best at reducing alcohol use and alcohol-related HIV risks.
How can alcohol venues be included in HIV prevention interventions?
At the beginning of the HIV epidemic, HIV prevention interventions were mostly guided by theories and models focused on individual-level determinants of risk behavior (74–76). Since then, there has been a growing recognition that social and structural factors also matter and help to determine behavioral risks for HIV (77). Structural level HIV prevention strategies focus on altering macro-level factors like economic, racial, and gender inequities (78). At a smaller scale, micro-structural approaches focus on social influence and social settings (79). Both macro- and micro-structural HIV prevention strategies not only help to target factors outside the individual to reduce risks for HIV, but also arguably lead to more sustainable behavior change than individual-focused approaches. Although an intervention targeting individuals may initially work to promote individuals’ healthy behavior, people may revert to their unhealthy ways because of the influence of risk-enabling social and structural factors (3,80). In this case alcohol venues represent an important place where individual, social, and structural interventions should be targeted for HIV prevention (81).
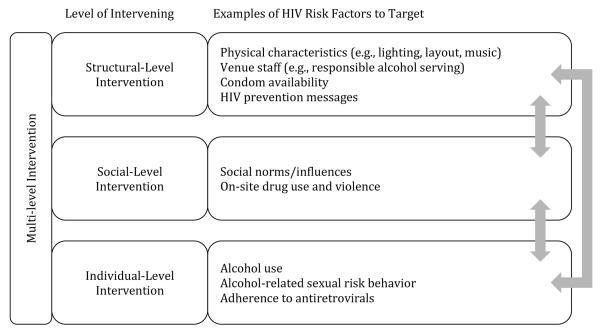
Alcohol venues may be included in HIV prevention interventions in three different ways – by recruiting from alcohol venues for individual interventions, intervening in venues for social interventions, and intervening on venues for structural interventions (Figure 1). Patrons of alcohol venues are at risk of acquiring or transmitting HIV as a function of their sex behaviors and facilitated by their drinking. Alcohol venue patrons are a key population to target for recruitment into individual-level interventions designed to primarily reduce alcohol use and alcohol-related risks. This population is especially key in regions where both alcohol use and HIV are prevalent. Therefore, interventionists interested in targeting alcohol users may recruit people from alcohol venues, without necessarily having interest in changing elements of the venues themselves. For example, one study conducted in South Africa recruited men and women from shebeens to participate in HIV/alcohol risk reduction workshops (82). The participants were drinkers from local shebeens, but the intervention was conducted at a local community center. The intervention demonstrated efficacy in increasing condom use and reducing HIV risks for the light-moderate drinkers but not the heavy-problem drinkers.
Figure 1.
HIV intervention approaches including alcohol venues
Social-level interventions may also be conducted on-site in venues with the goal of altering the environment, in particular the social norms in the venues. Finally, researchers may be interested in intervening on the venues themselves with the goal of altering the venue’s structural or contextual characteristics. Figure 1 displays some examples of the HIV risk factors targeted in and outside of alcohol venues within each level of intervention approach. A structural intervention might aim to alter the “risk-enabling” environment of alcohol venues by improving lighting and layout to deter from patrons having sex within the venue, provide condoms for free or for purchase, promote responsible alcohol serving practices by training staff, and holding HIV prevention educational activities within the venues. A social influence intervention might aim to recruit patrons to be agents of change to shift social norms towards safer alcohol- and sexual-related HIV risk behaviors. Interventions with the people in venues might also aim to reduce onsite drug use and aggression or violence. Targeting individual alcohol use and condom use among the patrons would further enhance efficacy of these approaches. In an era where antiretroviral therapies are emerging for use in HIV prevention, an individual-level intervention might also promote adherence to antiretrovirals, either among patrons who are HIV-positive or those using medications as pre-exposure prophylaxis. Such an approach could have significant potential given that alcohol use has been shown to be a robust barrier to proper adherence (83–86). A multilevel approach may target two or all three levels with the ultimate goal of reducing HIV transmission.
What interventions have been based in alcohol-venues?
Literature Review
A review of the research shows a surprisingly limited number of interventions that have included alcohol venues in HIV prevention interventions. In 2010, Kalichman conducted a review of HIV risk reduction interventions based in alcohol venues and identified a total of nine randomized trials, quasi-experimental studies, or public health evaluations (3). We sought to update this review by conducting a new literature search. We used a combination of search terms like “HIV;” and “intervention;” and “alcohol venues.” In line with the original Kalichman review, we searched only for interventions or programs that targeted patrons in alcohol venues and studied HIV, STI, or condom use as the primary outcome (and not merely alcohol consumption). We identified two new additional interventions to the older review, one of which has reported outcomes. A summary of all eleven interventions is presented in Table 1. Of the 11 studies, five were interventions delivered at the social level, two at the structural level, and two were multilevel in combining social and structural approaches. The two new studies included in this review were both multilevel interventions. The first, conducted by Kalichman and colleagues and reported in 2013, was a multilevel intervention combining a social-structural intervention with individual sexual risk reduction counseling. The second was conducted by Morojele and colleagues and reported in 2014 and was a multilevel intervention combining a social influence intervention with individualized alcohol and HIV counseling.
Table 1.
HIV prevention intervention based in alcohol venues.
| Authors | Target Population and Venues |
Intervention and Study Design |
Summary of Findings | Effectiveness |
|---|---|---|---|---|
| Social Influence Interventions | ||||
| Kelly et al. 1992 | Gay bars in three southeastern U.S. small cities |
POL intervention; multiple baseline quasi- experimental design with staggered intervention implementation; observations between 3 and 9 months postintervention. |
The POL model intervention demonstrated 15 percent to 24 percent reductions in USI across all three cities. Similar outcomes occurred for numbers of sex partners and increases in condom use during anal sex. |
Intervention led to safer behavior. |
| Kelly et al. 1997 | Gay bars in eight small U.S. cities |
POL intervention, community-level RCT; observation over 1-year postintervention. |
Intervention cities demonstrated less USI than control cities by a factor of nearly four- fold. Condom use increased from 45 percent protected acts to 67 percent, with no increase occurring in the control cities. |
Greater behavior change in the intervention compared to control. |
| Miller 1998 | Gay bars with significant male prostitution in New York City |
Adaptation of POL intervention; multiple baseline quasi- experimental design with staggered intervention implementation; observations occurred in each bar five times at 2- month intervals. |
The intervention demonstrated significant reductions in paid USI across venues. Frequencies of unpaid USI were not affected by the intervention. Bars with more stable patrons and Latino and White men benefited from the intervention, whereas Black men did not. |
Intervention led to safer behavior. |
| NIMH Collaborative HIV/STD Prevention Trial 2008 | Wine shop customers in impoverished slums, India |
C-POL intervention; 24 wine shops within impoverished slum communities; community-level RCT conducted in India and four other countries; observation over 2 years. |
Comparable reductions in HIV/STI transmission risk behaviors occurred in the intervention and control communities. Both conditions also demonstrated comparable reductions in new STI. |
Behavior became safer overall, although no significant differences in behavior change between intervention and control groups. |
| Fritz et al. 2011 | Men in beer halls in Zimbabwe |
Peer education using elements of POL model; Twelve beer halls randomized to peer influence intervention or a standard message and access to condoms |
Men in intervention and control beer halls reported equal amounts of behavior change. No significant group differences in unprotected sex acts within and across partner types, condom use, and numbers of partners. |
Equal amount of behavior change across intervention and control groups. |
| Structural Interventions | ||||
| Blank et al. 2005 | Gay bars and clubs identified through syphilis case interviews, New York City |
“Hot Shot” public health program offering screening, diagnostic, and referral services to men in venues during evening hours; uncontrolled public health evaluation; 1-year observation period. |
Implementation of portable health services in venues resulted in four new syphilis and seven new HIV detections. Packaging STI and HIV services with general health programming was deemed feasible and potentially effective. |
No behavioral outcomes reported. |
| Rou et al. 2008 | Female sex workers in bars, massage parlors, dance halls, and beauty parlors, China |
Enhanced STI clinic services with STI/HIV education and sex worker condom promotion outreach; five sites in two provinces participated in the public health evaluation with no control condition; 1-year observation period. |
Reductions in multiple risk indicators were observed across venues during the observation period. Condom use with last client increased from 55 percent to 67 percent, prevalence of gonorrhea declined from 26 percent to 4 percent, and prevalence of Chlamydia decreased from 41 percent to 26 percent. |
Behavior became safer over time. |
| Multilevel Social Influence and Structural Interventions | ||||
| Flowers et al. 2002 | Gay bars in Glasgow, Scotland |
Peer-led sexual health promotion conducted in venues, gay-specific sexual health services in hospitals, and free phone- hotline service; two- city quasi-experimental trial; 3- year observation period. |
Peer education and associated services failed to demonstrate reductions in USI and increases in knowledge of sex partner HIV status or negotiated safety. Increases in HIV testing and hepatitis B vaccination were observed for men with direct contact with the intervention, but not for the Glasgow community in general. |
Significant effect for engaging men in STI services; no community- wide effects; no differences in behavior change. |
| Morisky et al. 2006 | Female sex workers in bars, nightclubs, discos, beer gardens, and karaoke bars, Philippines |
Four conditions: peer counseling and social influence for HIV risk reduction, manager training to reinforce employee health and structural health improvement, peer counseling with manager training, no-intervention control condition; quasi- experimental design with venues nested in four cities randomized to one of four conditions; 2-year observation period. |
Increases in condom use at last sex and reductions in self-reported STI occurred in the combined peer/manager intervention condition compared with the control site. These effects were bolstered by more positive condom attitudes and increased condom promotion within the venues. Sites receiving either the peer or manager interventions demonstrated variable patterns of risk reduction relative to the control site. |
Combined peer/manager intervention led to significant behavior change relative to control. |
| Multilevel Structural and Individual Intervention | ||||
| Kalichman et al. 2013 | Men in shebeens in Cape Town, South Africa |
Twelve matched pairs of township neighborhoods randomized to receive either an HIV prevention intervention or an attention-matched control intervention on relationship violence. Intervention included individual sexual risk reduction counseling, workshops to increase conversations about safer sex, and community educational events. |
Men in the HIV prevention workshops demonstrated greater condom use and more HIV prevention-orientated conversations compared to men in the control. Patterns of community level changes in condom use were not consistent over time. |
Significant behavior change among men; inconsistent community-wide behavior change. |
| Multilevel Social Influence and Individual Intervention | ||||
| Morojele et al. 2014 | Bar patrons in Tshwane, South Africa |
Public health evaluation of an intervention delivered in two alcohol venues; Patrons from the two bars were trained using the POL model, and individualized alcohol use and HIV risk reduction counseling was delivered in the venues |
The intervention was feasible and acceptable. |
No behavioral outcomes reported. |
Adapted from Kalichman SC. Social and Structural HIV Prevention in Alcohol-Serving Establishments. Alcohol Res Health J Natl Inst Alcohol Abuse Alcohol. 2010;33(3):184–94.
Kalichman et al. (87) conducted a community-level trial in South African shebeens. In this study, twelve matched pairs of shebeens were randomly assigned to receive either a multilevel HIV/alcohol risk reduction intervention or a time-matched structurally equivalent gender violence prevention intervention. The interventions targeted men and the drinking environment. Men were recruited from the venues using a chain/snowball sampling procedure that aimed to intervene with networks of men who drink at the shebeens. The men attended intensive educational and skills building workshops over the course of the week that included communication skills building akin to those used in the POL model. The intent was to saturate the drinking venues with men who received both individual behavior change and social message skills training. In addition, posters and flyers with prevention messages were placed in the shebeens to reinforce the communications and provide visual cues for initiating conversations. The shebeens were also used to house community-based prevention events that included the use of song and drama to educate community members in HIV/alcohol or gender violence prevention. Thus, men received individual behavior change interventions, skills for altering social communications, and the shebeens received prevention material and were converted to places for prevention events. The results showed that men made the expected individual level behavior changes. However, men also sustained those changes longer than has been observed in individual change interventions alone. The researchers concluded that shifts in community norms and alterations in the structural environment accounted for the greater durability in behavior change.
Morojele and colleagues also conducted a multilevel intervention in alcohol venues in South Africa (88). In this study, the researchers implemented a multilevel intervention in two licensed drinking establishments, one in a city and one in a township in Gauteng province. At the social level the intervention used the popular opinion leader (POL) model and recruited and trained a total of 39 patrons from both bars. In this model, sociometric methods are used to identify patrons in the venue who are seen as credible and exert social influence. These individuals are sought out and recruited to serve as risk reduction messengers in the venue. After being motivated through altruism, these opinion leaders are trained in communication skills and educated in risk education strategies with the aim of saturating the venue with credible prevention messages. At a second level the intervention delivered brief counseling and motivational interviewing to individual patrons in the two bars in an effort to target alcohol use and HIV sexual risk behaviors. While this specific multilevel intervention has been shown to be feasible and acceptable, whether it worked to promote healthy behavior change has not been reported.
Summarized in Table 1, we will not reiterate in detail the description and findings of the other nine interventions previously reviewed. The five studies that delivered social influence interventions implemented the POL model; two targeted MSM in gay bars in the U.S. (89,90), one targeted male sex workers in gay bars in New York City (91), one targeted wine shop customers in India (92), and one targeted men in beer halls in Zimbabwe (93). Whereas the three POL interventions delivered in gay bars were successful in producing experimental and quasi-experimental evidence of significant reductions in unprotected sex, the other two studies did not demonstrate efficacy in that both experimental and control groups reported similar amounts of behavior change.
The two structural intervention studies were conducted as public health program evaluations and did not include a control group. Both studies offered STI diagnostic and treatment services in the venues. One of these was delivered to venue-based FSWs in China and observed improved condom use with clients and reduced STIs over the course of the study period (94). The other study was delivered in gay bars in New York City and was deemed feasible, although no behavior or STI outcomes were reported (95).
The two multilevel interventions previously reviewed combined social influence and structural interventions. One delivered the POL model combined with enhanced STI and sexual health services and a free sexual health hotline service in gay bars in Glasgow, Scotland (96). This quasi-experiment demonstrated increases in engagement of men into STI services, and a promotion of sexual health behavior among men who had conversations with peer educators. The other study was conducted with venue-based FSWs in the Philippines and delivered a peer-led intervention, as well as a structural intervention in which managers at venues received HIV education (80). The study used a quasi-experimental design that was able to show positive effects of both the individual peer counseling component and manager component, while the combination of the two demonstrated the greatest effect on reductions on incident STIs over the study period.
Discussion of Intervention Findings
Overall, the interventions that appear to be the most successful at producing and sustaining behavior change are those target both social and structural aspects of the venue, particularly interventions that aim to shift social norms (studies highlighted in grey rows in Table 1).
Network interventions demonstrate that promoting informed conversations about HIV/AIDS and safer sex can shift descriptive and injunctive norms regarding sexual relationships and sexual behaviors beyond the individuals exposed to the intervention. In one example of a group delivered risk reduction and social influence intervention, Kelly et al. trained individuals in safer sex and risk reduction skills as well as communication skills that focused on HIV prevention advocacy training (97). The basic premise for this intervention model is that people who become public advocates for a cause tend to adopt personal attitudes that are congruent with their public statements. The concept underlying this approach is rooted in attitude formation theories, particularly in the area of cognitive dissonance (98). Actively serving as an HIV risk reduction advocate in one’s social networks can ultimately support one’s own behavior change by shifting social norms and expectations to support behavior change efforts. In a similar intervention model that was tailored for injection drug users, Latkin et al. integrated a small group skills building intervention with advocacy training and outreach components (99,100). Latkin et al. showed that members of the skills training groups were more than three times as likely to report cessation of drug injection, almost three times as likely to report reductions in needle sharing, and over seven times more likely to report increased condom use with casual partners (99). Kelly et al. used a similar approach to reducing HIV risks from a multilevel social network intervention for gay men in Bulgaria (101). What is perhaps most compelling about this type of intervention model is that it combines effective individual-level risk reduction with social-structural changes that ultimately support maintenance of behavior change over time. By training individuals to serve as agents of behavior change in their social networks, advocacy training interventions are essentially promoting what Friedman et al. have called intravention: prevention activities that are conducted by and sustained through the ongoing actions of members of communities-at-risk (102). Multilevel interventions aim to change cultures of risk into cultures of support for risk reduction. Applied to alcohol venues, this intervention approach has been successful with gay men, FSWs in the Philippines, and with men from shebeens in South Africa. It did not appear successful however with wine shop customers in India or men in beer halls in Zimbabwe. For POL/social-structural influence interventions to be successful, it might be that social networks should be somewhat close-knit and/or characterized by a relatively high degree of trust between members. Further, it is important to note that managers of venues where FSWs are based have a stake in the sexual health of their FSWs. For structural interventions that target venue managers or staff, this type of buy-in is sure to be key in improving efficacy, as well as feasibility and accessibility of venue-based interventions. In the next sections we review some methodological advances that might be applied in alcohol venue HIV prevention research.
How can we move forward with alcohol venue HIV prevention research?
To best understand the characteristics of alcohol venues that might influence HIV transmission behaviors, research methods must be able to capture the depth and breadth of venue-related factors. This means that measures should aim to assess the venues themselves as independent units, along with the characteristics of patrons and employees. Most of the HIV prevention research studies on venues, including many of those reviewed here, appear to focus on examining patron-level, rather than venue-level differences (103). As an example, one study sought to examine “venue-specific characteristics” that might affect MSM’s sexual risk behaviors in China (104). In this study, MSM from bars, recreational centers, saunas, parks, and dorms were surveyed. The results showed differences across these venue types in demographic characteristics, unprotected anal intercourse, HIV knowledge, drug and alcohol use, and HIV prevalence. While this and other studies that collect venue-based surveys offer some important data regarding venue-related HIV risks, the methodological approach used does not provide information about the characteristics of the venues themselves that may or may not explain differential risks for HIV. Multilevel modeling, qualitative and mixed method, and event-level studies, offer unique ways to study and model venues as units.
Multilevel Modeling
Researchers interested in studying patrons from different alcohol venues may capitalize on the relatively recent methodological advancement offered by multilevel modeling. Multilevel modeling approaches offer a way to systematically study both venue- and individual-level factors in HIV risk, and statistically account for the clustered nature of the data. One study of 213 FSWs who worked in 43 different bars in Tijuana, Mexico measured both venue-level (e.g., geographic proximity to the main sex work strip in Tijuana, availability of condoms in the workplace, bars with clientele from the U.S.) and individual-level (e.g., income, drug use, history of HIV testing) predictors of sex worker registration (105), which has been shown to be associated with decreased drug use and increased condom use (106,107). In another study, information about male patrons’ attitudes and behaviors within twelve different shebeens in South Africa were aggregated and examined as predictors of female patrons’ risky sex behaviors (108). The results showed that in venues where men reported drinking alcohol more frequently, women from those venues reported greater unprotected sex. Both of these studies used multilevel modeling and offer examples of the different venue-level factors that might be measured to understand the complexities of sexual risks in alcohol venues.
Qualitative and Mixed Methods
While some aspects of alcohol venues may be adequately captured with quantitative measures (e.g., amount of alcohol purchased and served), others are not (e.g., “rowdiness”). Qualitative or mixed methods research that incorporates the use of one or multiple methods including ethnographies, focus groups, and in-depth interviews, can help to richly characterize alcohol venues. One study was conducted to create a taxonomy of alcohol venues in Dominican Republic tourism town in terms of risk for HIV transmission (109). The researchers collected data using direct observations by interviewers and venue-based surveys delivered to a key informant in 135 different alcohol venues. Using latent class analysis, the researchers identified different categories of venue structural features (e.g., whether sex work took place in the venue, availability of condoms), venue patrons (e.g., whether the venue was primarily patronized by local Dominicans, Haitians, foreign tourists, or a combination), and HIV risk behaviors in the venue (e.g., same-sex behavior, transactional sex, heavy drinking). The results showed a convergence such that venues with the greatest structural risks were most likely to have high population-mixing between locals and tourists, who in turn engaged in the riskiest behaviors. In a different study of six alcohol venues in Buenos Aires, Argentina, researchers conducted five ethnographic observations in each of the venues to richly and comprehensively characterize each place across different dates, patrons, and activities (110). The ethnographers collected information about the area surrounding the venue, characteristics of clientele, personnel and interactions with patrons, areas for alcohol consumption and sexual behavior onsite, condom availability, HIV prevention materials, and other information about events that took place in the venue. They also created maps to provide a visual representation of the space. The researchers found that the venues were very different and the dynamics within them were complex, such that a single intervention approach might work within one setting but not another. For example, the authors described how a POL-type intervention might be effective in the settings where conversations are a typical activity, like dance clubs, but not where silence is predominant and where conversations might interfere with desired activities, like sex clubs. As a final example of a mixed method study in alcohol venues, researchers triangulated quantitative and qualitative data to identify correlates of male clients meeting FSWs in nightlife venues, and to gauge clients’ narratives about macro-level factors in the venues like social norms for heavy drinking (50). In sum, these studies provide examples of unique approaches to gathering rich data about alcohol venues as the unit of analyses.
Event-level Studies
Whereas the evidence reviewed suggests that alcohol venues do indeed play a role in predicting condom use, studies that collect data at the event-level can help elucidate the ties between condom use and venue context. Event-level studies have been conducted and reviewed to examine the relationship between alcohol use and condom use (61), and to examine whether this relationship is moderated by type of sexual encounter (111). However, we could not identify any event-level studies aimed at examining venue or drinking context with condom use as the outcome. One study using a national survey of university students in Canada asked respondents about their three most recent drinking events to examine the likelihood of aggressive behavior (112). The results showed that aggression was more likely to occur when drinking took place at a fraternity/sorority, residence, or a bar/disco/pub/tavern (compared with drinking at someone’s home, a restaurant or other). A similar approach may be used in alcohol venue and condom use research, but should distinguish between venues where drinking occurred and where sex occurred, as they may not be the same location.
Prospective Studies
Although they do not allow for causal inferences to be made, research using prospective study designs would help shed light on the direction of the relationship between alcohol venues and HIV risk. For example, studies could follow individuals and assess reasons for patronizing specific venues, study the characteristics of the venues themselves, and assess HIV risk behavior over time. A cohort study following women who patronize twelve different alcohol venues in Cape Town, South Africa across one year was shown to be highly feasible. The women completed four quarterly assessments with average retention over 90%. Although the purpose of this study was not to test competing hypotheses of self-selection versus venue influence, it did show that after controlling for time, venue characteristics predicted women’s unprotected sex over the course of the year (108).
Conclusions
Overall, our review suggests that while individual characteristics might help influence self-selection into different alcohol venues, alcohol venues play an absolute role in influencing risks for HIV. Risky social and sexual networks intersect in drinking venues. Altering the social environment of alcohol venues can shape behavior to increase condom use, reduce numbers of partners, and promote safer sexual relationships. Safer sex supportive social norms can also sustain individual behavior changes. Thus, ignoring the social context that embeds drinking and meeting sex partners may account for short-lived change often seen from behavioral interventions. In addition, there have been few multilevel HIV prevention interventions that exploit the opportunities afforded by venues. Future research should be directed toward developing and testing interventions that target behavior change in natural risk environments, particularly drinking venues. In order to fully and adequately understand the HIV risk factors at play in alcohol venues, studies should take advantage of the methodological and statistical advancements described earlier. While each venue has its own culture and each country has its own unique venue structure, common features cut across cultures and countries that allow for universalities in intervention design. For example, while the specific messages may vary, opinion leader models capitalize on interpersonal communication. Although network structures vary, the flow of communication through social relations is the vehicle for shifting social norms. The advantages of bringing prevention materials, messages, and even services such as testing into drinking establishments can be negotiated with venue owners and managers. Finally, future multilevel HIV prevention interventions may also need to target behavioral outcomes beyond condom use. In particular, as antiretroviral therapy and other new prevention technologies are brought to scale, alcohol venues will be important places for promotion and intervention. Alcohol use is a known impediment to medication adherence and ignoring it as well as its social context will surely undermine the use of HIV treatments as prevention and antiretroviral pre-exposure prophylaxis. Intervening in alcohol venues should be considered an essential element of advancing HIV prevention in any risk population.
Acknowledgments
Preparation of this manuscript was supported by a career development award to the first author K01DA036447.
References
- 1.Weir SS, Pailman C, Mahlalela X, Coetzee N, Meidany F, Boerma JT. From people to places: focusing AIDS prevention efforts where it matters most. AIDS Lond Engl. 2003 Apr 11;17(6):895–903. doi: 10.1097/01.aids.0000050809.06065.e0. [DOI] [PubMed] [Google Scholar]
- 2.Cain D, Pare V, Kalichman SC, Harel O, Mthembu J, Carey MP, et al. HIV risks associated with patronizing alcohol serving establishments in South African Townships, Cape Town. Prev Sci Off J Soc Prev Res. 2012 Dec;13(6):627–34. doi: 10.1007/s11121-012-0290-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kalichman SC. Social and Structural HIV Prevention in Alcohol-Serving Establishments. Alcohol Res Health J Natl Inst Alcohol Abuse Alcohol. 2010;33(3):184–94. [PMC free article] [PubMed] [Google Scholar]
- 4.Fritz K, Morojele N, Kalichman S. Alcohol: The Forgotten Drug in HIV/AIDS. Lancet. 2010 Aug 7;376(9739):398–400. doi: 10.1016/S0140-6736(10)60884-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schneider M, Chersich M, Neuman M, Parry C. Alcohol consumption and HIV/AIDS: the neglected interface. Addiction. 2012;107(8):1369–71. doi: 10.1111/j.1360-0443.2012.03824.x. [DOI] [PubMed] [Google Scholar]
- 6.Nichols BE, Nkalamo D, Whitcomb BW. Density of drinking establishments and HIV prevalence in a migrant town in Namibia. AIDS Behav. 2012 May;16(4):829–34. doi: 10.1007/s10461-011-9956-4. [DOI] [PubMed] [Google Scholar]
- 7.Truong KD, Sturm R. Alcohol environments and disparities in exposure associated with adolescent drinking in California. Am J Public Health. 2009 Feb;99(2):264–70. doi: 10.2105/AJPH.2007.122077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Truong KD, Sturm R. Alcohol outlets and problem drinking among adults in California. J Stud Alcohol Drugs. 2007 Nov;68(6):923–33. doi: 10.15288/jsad.2007.68.923. [DOI] [PubMed] [Google Scholar]
- 9.Livingston M. Alcohol outlet density and assault: a spatial analysis. Addiction. 2008;103(4):619–28. doi: 10.1111/j.1360-0443.2008.02136.x. [DOI] [PubMed] [Google Scholar]
- 10.Scribner RA, MacKinnon DP, Dwyer JH. Alcohol outlet density and motor vehicle crashes in Los Angeles County cities. J Stud Alcohol Drugs. 1994;55(4):447. doi: 10.15288/jsa.1994.55.447. [DOI] [PubMed] [Google Scholar]
- 11.Scribner R, Cohen D, Kaplan S, Allen SH. Alcohol availability and homicide in New Orleans: conceptual considerations for small area analysis of the effect of alcohol outlet density. J Stud Alcohol Drugs. 1999;60(3):310. doi: 10.15288/jsa.1999.60.310. [DOI] [PubMed] [Google Scholar]
- 12.Weitzman ER, Folkman A, Folkman MKL, Wechsler H. The relationship of alcohol outlet density to heavy and frequent drinking and drinking-related problems among college students at eight universities. Health Place. 2003;9(1):1–6. doi: 10.1016/s1353-8292(02)00014-x. [DOI] [PubMed] [Google Scholar]
- 13.Zhu L, Gorman DM, Horel S. Alcohol outlet density and violence: a geospatial analysis. Alcohol Alcohol. 2004;39(4):369–75. doi: 10.1093/alcalc/agh062. [DOI] [PubMed] [Google Scholar]
- 14.Eaton LA, Kalichman SC, Pitpitan EV, Cain DN, Watt MH, Sikkema KJ, et al. The relationship between attending alcohol serving venues nearby versus distant to one’s residence and sexual risk taking in a South African township. J Behav Med. 2013 Feb 13; doi: 10.1007/s10865-013-9495-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tutenges S. Safety problems among heavy-drinking youth at a Bulgarian nightlife resort. Int J Drug Policy. 2009 Sep;20(5):444–6. doi: 10.1016/j.drugpo.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 16.Engels RCME, Slettenhaar G, ter Bogt T, Scholte RHJ. Effect of alcohol references in music on alcohol consumption in public drinking places. Am J Addict Am Acad Psychiatr Alcohol Addict. 2011 Dec;20(6):530–4. doi: 10.1111/j.1521-0391.2011.00182.x. [DOI] [PubMed] [Google Scholar]
- 17.Morojele NK, Kachieng’a MA, Mokoko E, Nkoko MA, Parry CDH, Nkowane AM, et al. Alcohol use and sexual behaviour among risky drinkers and bar and shebeen patrons in Gauteng province, South Africa. Soc Sci Med 1982. 2006 Jan;62(1):217–27. doi: 10.1016/j.socscimed.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 18.Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq Creat Sociol. 2013;24(2):99–110. [Google Scholar]
- 19.Singer M. Introduction to syndemics: a critical systems approach to public and community health. Jossey-Bass Inc Pub; 2009. [Google Scholar]
- 20.Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: a literature review of the syndemic. J Womens Health 2002. 2011 Jul;20(7):991–1006. doi: 10.1089/jwh.2010.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003 Jun;93(6):939–42. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parsons JT, Grov C, Golub SA. Sexual Compulsivity, Co-Occurring Psychosocial Health Problems, and HIV Risk Among Gay and Bisexual Men: Further Evidence of a Syndemic. Am J Public Health. 2012 Jan;102(1):156–62. doi: 10.2105/AJPH.2011.300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med Publ Soc Behav Med. 2007 Aug;34(1):37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pitpitan EV, Kalichman SC, Eaton LA, Cain D, Sikkema KJ, Watt MH, et al. Co-occurring Psychosocial Problems and HIV Risk Among Women Attending Drinking Venues in a South African Township: A Syndemic Approach. Ann Behav Med Publ Soc Behav Med. 2013 Apr;45(2):153–62. doi: 10.1007/s12160-012-9420-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pitpitan EV, Kalichman SC, Eaton LA, Sikkema KJ, Watt MH, Skinner D. Gender-based violence and HIV sexual risk behavior: alcohol use and mental health problems as mediators among women in drinking venues, Cape Town. Soc Sci Med 1982. 2012 Oct;75(8):1417–25. doi: 10.1016/j.socscimed.2012.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pm G. Club drugs: MDMA, gamma-hydroxybutyrate (GHB), Rohypnol, and ketamine. Am Fam Physician. 2004 Jun;69(11):2619–26. [PubMed] [Google Scholar]
- 27.L L, J A, F M. Drugs and alcohol consumption and sexual behaviours in night recreational settings in Portugal. Adicciones. 2008 Dec;21(4):309–25. [PubMed] [Google Scholar]
- 28.Demant J. Affected in the nightclub. A case study of regular clubbers’ conflictual practices in nightclubs. Int J Drug Policy. 2013 May;24(3):196–202. doi: 10.1016/j.drugpo.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 29.Duff C. Party drugs and party people: examining the “normalization” of recreational drug use in Melbourne, Australia. Int J Drug Policy. 2005 Jun;16(3):161–70. [Google Scholar]
- 30.Wise J. Alcohol, not drugs, causes most problems at nightclubs. BMJ. 1997 Nov 8;315(7117):1177–80. [Google Scholar]
- 31.Mattison AM, Ross MW, Wolfson T, Franklin D. Circuit party attendance, club drug use, and unsafe sex in gay men. J Subst Abuse. 2001 Sep;13(1–2):119–26. doi: 10.1016/s0899-3289(01)00060-8. [DOI] [PubMed] [Google Scholar]
- 32.Drumright LN, Patterson TL, Strathdee SA. Club Drugs as Causal Risk Factors for HIV Acquisition Among Men Who Have Sex with Men: A Review. Subst Use Misuse. 2006 Jan 1;41(10-12):1551–601. doi: 10.1080/10826080600847894. [DOI] [PubMed] [Google Scholar]
- 33.Clapp JD, Reed MB, Holmes MR, Lange JE, Voas RB. Drunk in Public, Drunk in Private: The Relationship Between College Students, Drinking Environments and Alcohol Consumption. Am J Drug Alcohol Abuse. 2006 Jan 1;32(2):275–85. doi: 10.1080/00952990500481205. [DOI] [PubMed] [Google Scholar]
- 34.Watt MH, Meade CS, Kimani S, MacFarlane JC, Choi KW, Skinner D, et al. The impact of methamphetamine (“tik”) on a peri-urban community in Cape Town, South Africa. Int J Drug Policy. 2014 Mar;25(2):219–25. doi: 10.1016/j.drugpo.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meade CS, Watt MH, Sikkema KJ, Deng LX, Ranby KW, Skinner D, et al. [cited 2012 Aug 17];Methamphetamine use is associated with childhood sexual abuse and HIV sexual risk behaviors among patrons of alcohol-serving venues in Cape Town, South Africa. Drug Alcohol Depend [Internet] doi: 10.1016/j.drugalcdep.2012.05.024. Available from: http://www.sciencedirect.com/science/article/pii/S0376871612001871. [DOI] [PMC free article] [PubMed]
- 36.Freisthler B. Alcohol Use, Drinking Venue Utilization, and Child Physical Abuse: Results from a Pilot Study. J Fam Violence. 2011 Apr;26(3):185–93. doi: 10.1007/s10896-010-9352-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhan W, Shaboltas AV, Skochilov RV, Kozlov AP, Krasnoselskikh TV, Abdala N. Alcohol misuse, drinking contexts and intimate partner violence in St. Petersburg, Russia: results from a cross-sectional study. BMC Public Health. 2011;11:629. doi: 10.1186/1471-2458-11-629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Go VF, Srikrishnan AK, Parker CB, Salter M, Green AM, Sivaram S, et al. High prevalence of forced sex among non-brothel based, wine shop centered sex workers in Chennai, India. AIDS Behav. 2011 Jan;15(1):163–71. doi: 10.1007/s10461-010-9758-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cunradi CB, Mair C, Todd M, Remer L. Drinking context and intimate partner violence: evidence from the California community health study of couples. J Stud Alcohol Drugs. 2012 Sep;73(5):731–9. doi: 10.15288/jsad.2012.73.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rossow I. Alcohol-related violence: the impact of drinking pattern and drinking context. Addict Abingdon Engl. 1996 Nov;91(11):1651–61. doi: 10.1046/j.1360-0443.1996.911116516.x. [DOI] [PubMed] [Google Scholar]
- 41.Lund I. Drinking on the premises in Norway: young adults’ use of public drinking places. Addict Behav. 2007 Dec;32(12):2737–46. doi: 10.1016/j.addbeh.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 42.Leonard KE, Collins RL, Quigley BM. Alcohol consumption and the occurrence and severity of aggression: an event-based analysis of male to male barroom violence. Aggress Behav. 2003;29(4):346–65. [Google Scholar]
- 43.Graham K, Bernards S, Osgood DW, Wells S. Bad nights or bad bars? Multi-level analysis of environmental predictors of aggression in late-night large-capacity bars and clubs. Addict Abingdon Engl. 2006 Nov;101(11):1569–80. doi: 10.1111/j.1360-0443.2006.01608.x. [DOI] [PubMed] [Google Scholar]
- 44.Roberts JC. Bouncers and barroom aggression: A review of the research. Aggress Violent Behav. 2009 Jan;14(1):59–68. [Google Scholar]
- 45.Tutenges S, Bøgkjær T, Witte M, Hesse M. Drunken environments: a survey of bartenders working in pubs, bars and nightclubs. Int J Environ Res Public Health. 2013 Oct;10(10):4896–906. doi: 10.3390/ijerph10104896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lenk KM, Toomey TL, Erickson DJ. Propensity of Alcohol Establishments to Sell to Obviously Intoxicated Patrons. Alcohol Clin Exp Res. 2006 Jul;30(7):1194–9. doi: 10.1111/j.1530-0277.2006.00142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Toomey TL, Wagenaar AC, Kilian G, Fitch O, Rothstein C, Fletcher L. Alcohol sales to pseudo-intoxicated bar patrons. Public Health Rep Wash DC. 1974 Aug;114(4):337–42. doi: 10.1093/phr/114.4.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Freisthler B, Gruenewald PJ, Treno AJ, Lee J. Evaluating alcohol access and the alcohol environment in neighborhood areas. Alcohol Clin Exp Res. 2003 Mar;27(3):477–84. doi: 10.1097/01.ALC.0000057043.04199.B7. [DOI] [PubMed] [Google Scholar]
- 49.Toomey TL, Erickson DJ, Lenk KM, Kilian GR, Perry CL, Wagenaar AC. A randomized trial to evaluate a management training program to prevent illegal alcohol sales. Addict Abingdon Engl. 2008 Mar;103(3):405–13. doi: 10.1111/j.1360-0443.2007.02077.x. discussion 414–5. [DOI] [PubMed] [Google Scholar]
- 50.Goldenberg SM, Strathdee SA, Gallardo M, Nguyen L, Lozada R, Semple SJ, et al. How important are venue-based HIV risks among male clients of female sex workers? A mixed methods analysis of the risk environment in nightlife venues in Tijuana, Mexico. Health Place. 2011 May;17(3):748–56. doi: 10.1016/j.healthplace.2011.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang C, Li X, Hong Y, Stanton B, Chen Y, Zhou Y, et al. Pro-alcohol-use social environment and alcohol use among female sex workers in China: beyond the effects of serving alcohol. World Health Popul. 2012;13(4):15–27. doi: 10.12927/whp.2012.22923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mubayi A, Greenwood P, Wang X, Castillo-Chávez C, Gorman DM, Gruenewald P, et al. TYPES OF DRINKERS AND DRINKING SETTINGS: AN APPLICATION OF A MATHEMATICAL MODEL. Addict Abingdon Engl. 2011 Apr;106(4):749–58. doi: 10.1111/j.1360-0443.2010.03254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. [cited 2015 Feb 7];PLACE: Priorities for Local AIDS Control Efforts — MEASURE Evaluation [Internet] Available from: http://www.cpc.unc.edu/measure/tools/hiv-aids/place.
- 54. [cited 2015 Feb 7];PLACE in Mexico Focusing AIDS Prevention in Border Towns 2001 — MEASURE Evaluation [Internet] Available from: http://www.cpc.unc.edu/measure/publications/tr-04-26.
- 55. [cited 2015 Feb 7];PLACE in Zimbabwe: Identifying Gaps in HIV Prevention among Orphans and Young People in Hwange District, 2006 — MEASURE Evaluation [Internet] Available from: http://www.cpc.unc.edu/measure/publications/tr-08-66.
- 56. [cited 2015 Feb 7];PLACE in Central Asia: A Regional Strategy to Focus AIDS Prevention in Almaty and Karaganda, Kazakhstan; Osh, Kyrgyzstan; Tashkent, Uzbekistan 2002. — MEASURE Evaluation [Internet] Available from: http://www.cpc.unc.edu/measure/publications/tr-04-25.
- 57. [cited 2015 Feb 7];PLACE in Russia: Identifying Gaps in HIV Prevention in St. Petersburg, 2002. — MEASURE Evaluation [Internet] Available from: http://www.cpc.unc.edu/measure/publications/tr-04-21.
- 58.Kalichman SC, Simbayi LC, Vermaak R, Jooste S, Cain D. HIV/AIDS risks among men and women who drink at informal alcohol serving establishments (Shebeens) in Cape Town, South Africa. Prev Sci Off J Soc Prev Res. 2008 Mar;9(1):55–62. doi: 10.1007/s11121-008-0085-x. [DOI] [PubMed] [Google Scholar]
- 59.Townsend L, Ragnarsson A, Mathews C, Johnston LG, Ekström AM, Thorson A, et al. “Taking care of business”: alcohol as currency in transactional sexual relationships among players in Cape Town, South Africa. Qual Health Res. 2011 Jan;21(1):41–50. doi: 10.1177/1049732310378296. [DOI] [PubMed] [Google Scholar]
- 60.Watt MH, Aunon FM, Skinner D, Sikkema KJ, Kalichman SC, Pieterse D. [cited 2012 Feb 14];“Because he has bought for her, he wants to sleep with her”: Alcohol as a currency for sexual exchange in South African drinking venues. Soc Sci Med 1982 [Internet] 2012 Jan 25; doi: 10.1016/j.socscimed.2011.12.022. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22326304. [DOI] [PMC free article] [PubMed]
- 61.Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annu Rev Sex Res. 2000;11:125–57. [PMC free article] [PubMed] [Google Scholar]
- 62.Pitpitan EV, Kalichman SC, Garcia RL, Cain D, Eaton LA, Simbayi LC. Mediators of behavior change resulting from a sexual risk reduction intervention for STI patients, Cape Town, South Africa. J Behav Med. 2014 Sep 2; doi: 10.1007/s10865-014-9591-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lewis JJC, Garnett GP, Mhlanga S, Nyamukapa CA, Donnelly CA, Gregson S. Beer halls as a focus for HIV prevention activities in rural Zimbabwe. Sex Transm Dis. 2005 Jun;32(6):364–9. doi: 10.1097/01.olq.0000154506.84492.61. [DOI] [PubMed] [Google Scholar]
- 64.Safika I, Johnson TP, Levy JA. A venue analysis of predictors of alcohol use prior to sexual intercourse among female sex workers in Senggigi, Indonesia. Int J Drug Policy. 2011 Jan;22(1):49–55. doi: 10.1016/j.drugpo.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nemoto T, Iwamoto M, Sakata M, Perngparn U, Areesantichai C. Social and cultural contexts of HIV risk behaviors among Thai female sex workers in Bangkok, Thailand. AIDS Care. 2013;25(5):613–8. doi: 10.1080/09540121.2012.726336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Grov C, Hirshfield S, Remien RH, Humberstone M, Chiasson MA. Exploring the venue’s role in risky sexual behavior among gay and bisexual men: an event-level analysis from a national online survey in the U.S. Arch Sex Behav. 2013 Feb;42(2):291–302. doi: 10.1007/s10508-011-9854-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pitpitan EV, Wagner KD, Goodman-Meza D, Semple SJ, Chavarin C, Strathdee SA, et al. Context Matters: The Moderating Role of Bar Context in the Association Between Substance Use During Sex and Condom Use Among Male Clients of Female Sex Workers in Tijuana, Mexico. AIDS Behav. 2013 May 3; doi: 10.1007/s10461-013-0491-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sandøy IF, Zyaambo C, Michelo C, Fylkesnes K. Targeting condom distribution at high risk places increases condom utilization-evidence from an intervention study in Livingstone, Zambia. BMC Public Health. 2012 Jan 5;12:10. doi: 10.1186/1471-2458-12-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grov C, Crow T. Attitudes about and HIV risk related to the “most common place” MSM meet their sex partners: comparing men from bathhouses, bars/clubs, and Craigslist.org. AIDS Educ Prev Off Publ Int Soc AIDS Educ. 2012 Apr;24(2):102–16. doi: 10.1521/aeap.2012.24.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cosper RL, Okraku IO, Neumann B. Tavern Going in Canada: A National Survey of Regulars at Public Drinking Establishments. J Stud Alcohol Drugs. 1987 May 1;48(03):252. doi: 10.15288/jsa.1987.48.252. [DOI] [PubMed] [Google Scholar]
- 71.Treno AJ, Alaniz ML, Gruenewald PJ. The use of drinking places by gender, age and ethnic groups: an analysis of routine drinking activities. Addiction. 2000;95(4):537–51. doi: 10.1046/j.1360-0443.2000.9545376.x. [DOI] [PubMed] [Google Scholar]
- 72.Gruenewald PJ. The spatial ecology of alcohol problems: niche theory and assortative drinking. Addiction. 2007;102(6):870–8. doi: 10.1111/j.1360-0443.2007.01856.x. [DOI] [PubMed] [Google Scholar]
- 73.Gruenewald PJ, Remer LG, LaScala EA. Testing a social ecological model of alcohol use: the California 50-city study. Addiction. 2014;109(5):736–45. doi: 10.1111/add.12438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 75.Jemmott JB, 3rd, Jemmott LS, Hacker CI. Predicting intentions to use condoms among African-American adolescents: the theory of planned behavior as a model of HIV risk-associated behavior. Ethn Dis. 1991;2(4):371–80. [PubMed] [Google Scholar]
- 76.Albarracin D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behavior as models of condom use: a meta-analysis. Psychol Bull. 2001;127(1):142. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Parker RG, Easton D, Klein CH. Structural barriers and facilitators in HIV prevention: a review of international research. Aids. 2000;14:S22–32. doi: 10.1097/00002030-200006001-00004. [DOI] [PubMed] [Google Scholar]
- 78.Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. The Lancet. 2008;372(9640):764–75. doi: 10.1016/S0140-6736(08)60887-9. [DOI] [PubMed] [Google Scholar]
- 79.Latkin CA, Knowlton AR. Micro-social structural approaches to HIV prevention: a social ecological perspective. AIDS Care. 2005;17(S1):102–13. doi: 10.1080/09540120500121185. [DOI] [PubMed] [Google Scholar]
- 80.Morisky DE, Stein JA, Chiao C, Ksobiech K, Malow R. Impact of a social influence intervention on condom use and sexually transmitted infections among establishment-based female sex workers in the Philippines: A multilevel analysis. Health Psychol. 2006;25(5):595–603. doi: 10.1037/0278-6133.25.5.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.DiClemente CC. Mechanisms, determinants and processes of change in the modification of drinking behavior. Alcohol Clin Exp Res. 2007 Oct;31(10 Suppl):13s–20s. doi: 10.1111/j.1530-0277.2007.00489.x. [DOI] [PubMed] [Google Scholar]
- 82.Kalichman SC, Simbayi LC, Vermaak R, Cain D, Smith G, Mthebu J, et al. Randomized Trial of a Community-based Alcohol-related HIV Risk-reduction Intervention for Men and Women in Cape Town South Africa. Ann Behav Med. 2008 Oct 4;36(3):270–9. doi: 10.1007/s12160-008-9067-2. [DOI] [PubMed] [Google Scholar]
- 83.Samet JH, Cheng DM, Libman H, Nunes DP, Alperen JK, Saitz R. Alcohol consumption and HIV disease progression. J Acquir Immune Defic Syndr 1999. 2007;46(2):194. doi: 10.1097/QAI.0b013e318142aabb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Palepu A, Horton NJ, Tibbetts N, Meli S, Samet JH. Uptake and adherence to highly active antiretroviral therapy among HIV-infected people with alcohol and other substance use problems: the impact of substance abuse treatment. Addiction. 2004;99(3):361–8. doi: 10.1111/j.1360-0443.2003.00670.x. [DOI] [PubMed] [Google Scholar]
- 85.Chander G, Lau B, Moore RD. Hazardous alcohol use: a risk factor for non-adherence and lack of suppression in HIV infection. J Acquir Immune Defic Syndr 1999. 2006;43(4):411. doi: 10.1097/01.qai.0000243121.44659.a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010;112(3):178–93. doi: 10.1016/j.drugalcdep.2010.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kalichman SC, Simbayi LC, Cain D, Carey KB, Carey MP, Eaton L, et al. Randomized community-level HIV prevention intervention trial for men who drink in South African alcohol-serving venues. Eur J Public Health. 2014 Oct;24(5):833–9. doi: 10.1093/eurpub/ckt172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Morojele NK, Kitleli N, Ngako K, Kekwaletswe CT, Nkosi S, Fritz K, et al. Feasibility and acceptability of a bar-based sexual risk reduction intervention for bar patrons in Tshwane, South Africa. SAHARA J J Soc Asp HIVAIDS Res Alliance SAHARA Hum Sci Res Counc. 2014 Apr 22;:1–9. doi: 10.1080/17290376.2014.890123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kelly JA, St Lawrence JS, Stevenson LY, Hauth AC, Kalichman SC, Diaz YE, et al. Community AIDS/HIV risk reduction: the effects of endorsements by popular people in three cities. Am J Public Health. 1992 Nov;82(11):1483–9. doi: 10.2105/ajph.82.11.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kelly JA, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, et al. Randomised, controlled, community-level HIV-prevention intervention for sexual-risk behaviour among homosexual men in US cities. The Lancet. 1997 Nov 22;350(9090):1500–5. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- 91.Miller RL, Klotz D, Eckholdt HM. HIV prevention with male prostitutes and patrons of hustler bars: replication of an HIV preventive intervention. Am J Community Psychol. 1998 Feb;26(1):97–131. doi: 10.1023/a:1021886208524. [DOI] [PubMed] [Google Scholar]
- 92.NIMH Collaborative HIV/STD Prevention Trial Effectiveness of a Community-Level HIV/STD Prevention Intervention in Promoting Safer Sexual Behaviors in High-Risk Populations. International AIDS Conference; Mexico City. 2008. [Google Scholar]
- 93.Fritz K, McFarland W, Wyrod R, Chasakara C, Makumbe K, Chirowodza A, et al. Evaluation of a peer network-based sexual risk reduction intervention for men in beer halls in Zimbabwe: results from a randomized controlled trial. AIDS Behav. 2011;15(8):1732–44. doi: 10.1007/s10461-011-9922-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rou K, Wu Z, Sullivan SG, Li F, Guan J, Xu C, et al. A five-city trial of a behavioural intervention to reduce sexually transmitted disease/HIV risk among sex workers in China. AIDS Lond Engl. 2007 Dec;21(Suppl 8):S95–101. doi: 10.1097/01.aids.0000304703.77755.c7. [DOI] [PubMed] [Google Scholar]
- 95.Blank S, Gallagher K, Washburn K, Rogers M. Reaching out to boys at bars: utilizing community partnerships to employ a wellness strategy for syphilis control among men who have sex with men in New York City. Sex Transm Dis. 2005 Oct;32(10 Suppl):S65–72. doi: 10.1097/01.olq.0000175401.37527.de. [DOI] [PubMed] [Google Scholar]
- 96.Flowers P, Hart GJ, Williamson LM, Frankis JS, Der GJ. Does bar-based, peer-led sexual health promotion have a community-level effect amongst gay men in Scotland? Int J STD AIDS. 2002 Feb;13(2):102–8. doi: 10.1258/0956462021924721. [DOI] [PubMed] [Google Scholar]
- 97.Kelly JA, McAuliffe TL, Sikkema KJ, Murphy DA, Somlai AM, Mulry G, et al. Reduction in risk behavior among adults with severe mental illness who learned to advocate for HIV prevention. Psychiatr Serv Wash DC. 1997 Oct;48(10):1283–8. doi: 10.1176/ps.48.10.1283. [DOI] [PubMed] [Google Scholar]
- 98.Festinger L. A Theory of Cognitive Dissonance. Stanford University Press; 1962. p. 308. [Google Scholar]
- 99.Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: outcome of a network-oriented peer outreach intervention. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2003 Jul;22(4):332–9. doi: 10.1037/0278-6133.22.4.332. [DOI] [PubMed] [Google Scholar]
- 100.Latkin CA, Hua W, Davey MA. Factors Associated with Peer HIV Prevention Outreach in Drug-Using Communities. AIDS Educ Prev. 2004 Dec;16(6):499–508. doi: 10.1521/aeap.16.6.499.53794. [DOI] [PubMed] [Google Scholar]
- 101.Kelly JA, Amirkhanian YA, Kabakchieva E, Vassileva S, Vassilev B, McAuliffe TL, et al. Prevention of HIV and sexually transmitted diseases in high risk social networks of young Roma (Gypsy) men in Bulgaria: randomised controlled trial. BMJ. 2006 Nov 25;333(7578):1098. doi: 10.1136/bmj.38992.478299.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Friedman SR, Maslow C, Bolyard M, Sandoval M, Mateu-Gelabert P, Neaigus A. Urging others to be healthy: “intravention” by injection drug users as a community prevention goal. AIDS Educ Prev Off Publ Int Soc AIDS Educ. 2004 Jun;16(3):250–63. doi: 10.1521/aeap.16.3.250.35439. [DOI] [PubMed] [Google Scholar]
- 103.Pitpitan EV, Kalichman SC, Eaton LA, Strathdee SA, Patterson TL. HIV/STI risk among venue-based female sex workers across the globe: a look back and the way forward. Curr HIV/AIDS Rep. 2013 Mar;10(1):65–78. doi: 10.1007/s11904-012-0142-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhao J, Chen L, Cai W-D, Tan J-G, Tan W, Zheng C-L, et al. HIV Infection and Sexual Behaviors Among Non-Commercial Men Who Have Sex with Men at Different Venues. Arch Sex Behav. 2014 May;43(4):801–9. doi: 10.1007/s10508-013-0167-0. [DOI] [PubMed] [Google Scholar]
- 105.Gaines TL, Rusch MLA, Brouwer KC, Goldenberg SM, Lozada R, Robertson AM, et al. Venue-level correlates of female sex worker registration status: a multilevel analysis of bars in Tijuana, Mexico. Glob Public Health. 2013;8(4):405–16. doi: 10.1080/17441692.2013.779386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sirotin N, Strathdee SA, Lozada R, Abramovitz D, Semple SJ, Bucardo J, et al. Effects of government registration on unprotected sex amongst female sex workers in Tijuana; Mexico. Int J Drug Policy. 2010 Nov;21(6):466–70. doi: 10.1016/j.drugpo.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sirotin N, Strathdee SA, Lozada R, Nguyen L, Gallardo M, Vera A, et al. A comparison of registered and unregistered female sex workers in Tijuana, Mexico. Public Health Rep Wash DC 1974. 2010 Aug;125(Suppl 4):101–9. doi: 10.1177/00333549101250S414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pitpitan EV, Kalichman SC, Eaton LA, Sikkema KJ, Watt MH, Skinner D, et al. Men’s Behavior Predicts Women’s Risks for HIV/AIDS: Multilevel Analysis of Alcohol-Serving Venues in South Africa. under review. [DOI] [PMC free article] [PubMed]
- 109.Guilamo-Ramos V, Jaccard J, McCarthy K, Quiñones Z, Lushin V, Skinner-Day M, et al. Taxonomy of Caribbean tourism alcohol venues: Implications for HIV transmission. Drug Alcohol Depend. 2013 Sep 1;132(1-2):238–43. doi: 10.1016/j.drugalcdep.2013.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Balán IC, Barreda V, Marone R, Avila MM, Carballo-Diéguez A. Venues, Patrons, and Alcohol Use Dynamics: The Creation of a High Risk Sexual Environment. AIDS Behav. 2014 Apr 2; doi: 10.1007/s10461-014-0759-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Leigh BC. Alcohol and condom use: a meta-analysis of event-level studies. Sex Transm Dis. 2002;29(8):476–82. doi: 10.1097/00007435-200208000-00008. [DOI] [PubMed] [Google Scholar]
- 112.Wells S, Mihic L, Tremblay PF, Graham K, Demers A. Where, With Whom, and How Much Alcohol Is Consumed on Drinking Events Involving Aggression? Event-Level Associations in a Canadian National Survey of University Students. Alcohol Clin Exp Res. 2008;32(3):522–33. doi: 10.1111/j.1530-0277.2007.00596.x. [DOI] [PubMed] [Google Scholar]