Abstract
Purpose
Although long-term colorectal cancer (CRC) survivors generally report a good quality of life, fear of cancer recurrence (FCR) remains an important issue. This study investigated whether the Cancer Worry Scale (CWS) can detect high FCR, the prevalence, and characteristics of FCR in CRC survivors.
Methods
Two hundred and eleven patients who had undergone successful CRC surgery in the period 2003–2010 in the Radboud University Medical Center in the Netherlands were asked to participate. All patients were sent an information letter plus questionnaires for collecting information on demographic and medical variables, FCR, distress, and quality of life.
Results
Seventy-six patients (36 %; median age of 67.7 years range 41–88 years) completed the questionnaires a median of 5.1 years after surgery. A cut-off score of 14 or higher on the CWS was optimal to detect high FCR. Twenty-nine patients (38 %) experienced high levels of FCR, characterized by higher levels of distress, post-traumatic stress symptoms, and lower quality of life. These individuals particularly reacted to disease-related triggers, felt helpless, were worried, and experienced limitations in daily functioning. High FCR was not associated with demographic or medical variables.
Conclusion
Long after successful CRC surgery, FCR is a serious problem that impairs the quality of life for a substantial proportion of patients. With the CWS, it is possible to detect high FCR and thereby assist survivors in receiving appropriate care.
Keywords: Fear of cancer recurrence, Quality of life, Colorectal cancer, Oncology
Introduction
Early detection and improved cancer treatment have increased the survival rate of colorectal cancer (CRC) over the past decades [1]. This has made it important to pay attention to the way survivors deal with chronic or late effects of the disease and its treatment. A number of recent studies have investigated the quality of life (QoL) of CRC survivors and have shown that while QoL is reduced after treatment completion, it gradually improves over time in the absence of disease recurrence or progression [2–5]. While a systematic review found long-term CRC survivors to have good overall QoL [6], this does not necessarily mean that these individuals do not experience problems that can influence their daily functioning. Not only can CRC survivors have specific physical complaints, such as fecal, urinary, or sexual disorders [7], but they might also have an unmet need for psychosocial help with regard to fear of cancer recurrence (FCR) [8]. FCR can be defined as the fear or worry that the disease will return or progress in the same organ or in another part of the body [9]. While a normal level of FCR can keep a person alert and aware of symptoms [10], high levels of FCR can adversely affect a person’s quality of life and social activities [11–14]. Patients may focus obsessively on symptoms [10], which can restrict their ability to plan for the future and can lead to numerous unscheduled doctor appointments [15, 16]. Among the few studies reporting FCR in CRC survivors, the prevalence of high FCR ranges between 4 and 85 % [17–22]. This wide range of percentages high FCR might be attributed to the fact that there is no consensus about what are clinically relevant levels of FCR. Furthermore, it might be attributed to the use of various instruments to measure FCR for which there are few or no psychometric data or cut-off points available [10]. In the research on FCR in CRC patients, some studies did not use a FCR specific measure [18, 21], whereas others had lacking data on validity [17, 19, 20]. Therewith, interpretation and comparison of percentages high FCR is difficult. Recently, a semi-structured interview to identify patients with clinical levels of FCR was developed by Simard and Savard [22]. Based on this interview, cut-off scores on the severity subscale of the Fear of Cancer Recurrence Inventory (FCRI-SF) were determined. Therewith, it is possible to use this scale as gold standard measure for evaluating the criterion validity of different FCR scales. The aim of this study is to assess the capacity of the Cancer Worry Scale (CWS), validated in a sample of breast cancer survivors [23], as an instrument to detect high levels of FCR in a sample of CRC survivors. Furthermore, there has been little research on FCR in CRC survivors, its characteristics, and potential risk groups, mainly because earlier studies focused on the severity and prevalence of FCR. There is a lack of information about what specific triggers make survivors fearful, which strategies they use to cope with this fear, and the concrete consequences of FCR in daily life. This study focuses on the prevalence and characteristics of FCR in CRC survivors.
Methods
Participants
In March 2012, participants were recruited from the Department of Surgery, Radboud University Medical Center, Nijmegen in the Netherlands. CRC survivors who had been treated with curative intent and who were disease-free (no recurrence or metastases) 1–9 years after surgery were eligible for inclusion. Participants had to be able to read and write in Dutch.
Procedure
Documented approval from the local Medical Ethics Committee was obtained prior to start of the study. Contact data of CRC survivors were obtained by a surgeon (JW), and these individuals were sent a letter describing the purpose of the study and a booklet with questionnaires on demographic variables and psychological factors. Participants gave their informed consent by returning the booklet. Clinical data were extracted from medical records by one of the researchers (SJ).
Instruments
Fear of cancer recurrence: severity
The CWS is used in research to assess concerns about developing cancer or developing cancer again and the impact of these concerns on daily functioning. The eight items of the CWS are rated on a 4-point Likert scale ranging from “Never” to “Almost always”. Scores range from 8 to 32 [24]. A diagnostic cut-off score of 14 or higher (sensitivity 77 %; specificity 81 %) was validated for breast cancer survivors and indicates raised levels of FCR [23].
Fear of cancer recurrence: multidimensional aspects
The Fear of Cancer Recurrence Inventory (FCRI) was developed to assess the multidimensional aspects of FCR. The FCRI consists of seven subscales: triggers, severity, psychological distress, coping strategies, functioning impairments, insight, and reassurance. The 42 items are rated on a 5-point Likert scale ranging from 0 to 4. The FCRI is a reliable and valid self-report scale [25].
The subscale Triggers includes eight items, of which seven assess specific situations that make one think about the possibility of cancer recurrence; one item assesses to what degree these situations are generally avoided. The subscale Severity includes nine items assessing the presence, frequency, intensity and duration of thoughts associated with FCR, the perceived risk of recurrence, the legitimacy of worrying about cancer recurrence, and the presence of other unpleasant thoughts or images that come to mind in association with FCR. Recently, data were provided that this subscale may also be used as FCRI-short form to screen for clinical levels of FCR. A score of 13 or higher was optimal for screening whereas a score of 16 or higher was the optimal diagnostic cut-off [22]. The subscale Psychological Distress includes four items for emotions frequently triggered by thoughts about cancer recurrence. The subscale Coping Strategies assesses nine strategies that may be used to cope with FCR including denial, wishful thinking, or cognitive avoidance.
The subscale Functioning Impairments includes six items representing domains that can be disturbed by FCR. The subscale Insight includes three items and assesses the extent to which patients perceive their fear as excessive or unreasonable. The subscale Reassurance includes three items representing reassurance behaviors specific to FCR.
Distress: cancer-specific
The Impact of Event Scale (IES) was included to assess the frequency of intrusive and avoidant phenomena after or during the traumatic experience of cancer. Its 15 items (scoring 0, 1, 3, 5) are divided into two dimensions: “Intrusion” (7 items) and “Avoidance” (8 items). A total score of 9–25 reflects moderate adaptation difficulties; a score higher than 26 indicates serious adaptation difficulties [26, 27].
Distress: general
General distress was measured with the total score of the Hospital Anxiety and Depression Scale (HADS). This questionnaire includes 14 items divided into two subscales (Depression and Anxiety), each with seven items. Higher scores indicate more anxiety, depression, and psychological distress. The HADS does not contain any somatic items that could be confounded with symptoms associated with a physical illness. A total score of 11 or higher indicates high distress [28, 29].
Quality of life: cancer-related
Quality of life related to CRC was measured with the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire Core 30 (QLQ-C30) and Colorectal Cancer Module (QLQ-CR38). In this study, only scores for the functional scales and global health scale were analyzed. Higher scores on functional scales indicate better functioning and quality of life. All scores are transformed linearly and range from 0 to 100 [30, 31]. A difference of 5–10 points was considered small, 10–20 points medium and >20 points large [32].
Data-analyses
Prior to SPSS (version 20.0) data analysis, all relevant data were screened for normality and showed normal distributions. Means and frequencies were used to describe the sample. Only complete data for the CWS were analyzed; incomplete data were recorded as missing data and excluded from the analyses. Receiving operating characteristics (ROC) analysis was conducted to evaluate the performance of the CWS by providing information relevant to the full range of scores that need to be taken into account in making a threshold for high FCR in a population of CRC survivors. The accuracy properties sensitivity, specificity, and positive and negative predictive values were assessed at each cut-off point of the CWS against the FCRI-SF. Furthermore, the area under the ROC curve and its 95 % confidence interval were examined. To differentiate high FCR from low FCR, an optimal cut-off point should have high sensitivity and specificity, which maximizes the proportion of patients whose test results are accurate [33].
Multivariate ANOVAs were performed for continuous variables, to assess differences between high and low FCR, based on the cut-off score (low ≤13; high ≥14). Chi-square analyses were performed to assess differences between high and low FCR with regard to categorical variables. Pearson product moment correlations and independent sample t tests were used to assess relations between continuous variables.
For a descriptive analysis of the FCRI scores, percentages of responses to the individual questions were calculated. In order to reflect the degree of involvement with a specific item, varying from small to moderate or large, answers on the subscales Triggers, Coping, and Reassurance were combined into three answer categories: (1) “never/rarely”, (2)“sometimes”, and (3)“most of the time/all the time”. Answers on the subscales Severity, Psychological Distress, Functioning Impairments, and Insight were also divided into three answer categories: (1) “not at all/a little”, (2) “somewhat”, and (3) “a lot/a great deal”.
Results
Sample characteristics
Of 211 CRC survivors asked to participate in the study, 80 (38 %) returned the questionnaires, and 76 (36 %) of whom completed the CWS and were included in the analyses. There was no difference between responders and non-responders with regard to gender (Χ2 (1, 211) = 0.03, p = 0.87), but non-responders were significantly older (t(209) = 2.0, p = 0.046). Table 1 shows the demographic and medical characteristics of the responders.
Table 1.
Sample characteristics (n = 76)
| Age (years) | Median 67.3; range = 41–88 | |
|---|---|---|
| Sex: male | 40 | 53 % |
| Marital status | ||
| Married/partnership | 55 | 72 % |
| Not in partnership | 21 | 28 % |
| Children: yes | 64 | 84 % |
| Educational level | ||
| Primary | 03 | 04 % |
| Secondary | 43 | 57 % |
| Tertiary | 25 | 33 % |
| Other | 05 | 07 % |
| Employment status | ||
| Retired | 44 | 58 % |
| Employed | 20 | 26 % |
| Home management | 12 | 16 % |
| Unemployed/others | 15 | 20 % |
| Time since surgery (years) | Median 5.1; range = 1.3–9.2 | |
| Location of tumor | ||
| Colon | 58 | 76 % |
| Rectum | 18 | 24 % |
| Stoma: yes | 13 | 17 % |
| Disease stage | ||
| I | 13 | 17 % |
| II | 31 | 41 % |
| III | 32 | 42 % |
| Additional treatment | ||
| Chemotherapy: yes | 24 | 32 % |
| Radiotherapy: yes | 10 | 13 % |
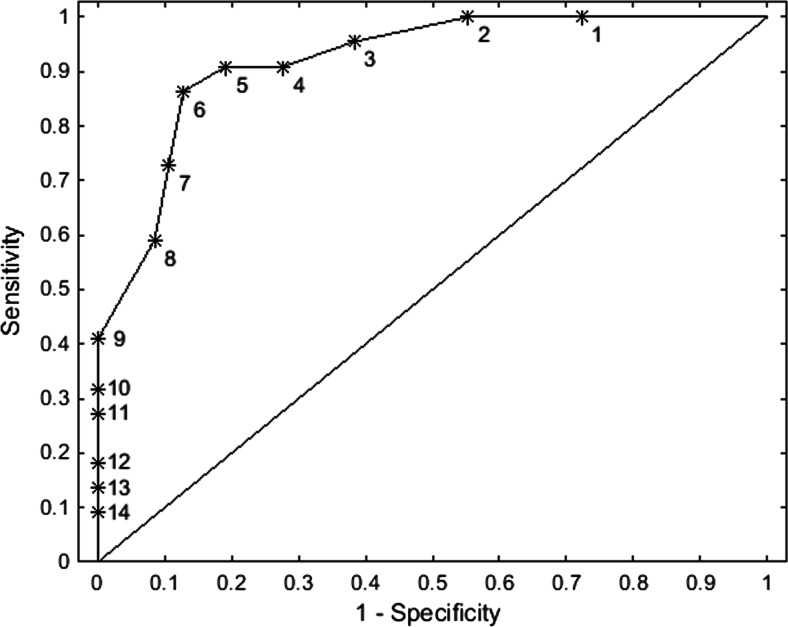
ROC analysis
The area under the curve of the ROC analysis showed a 92 % (p < 0.001; 95%CI = 0.85–0.98) probability that a randomly selected patient defined as a case by the FCRI-SF (≥16) scores higher on the CWS than a randomly selected patient defined as a non-case (Fig. 1). On the basis of the ROC curve, the optimal cut-off score to differentiate between high FCR and low FCR was 13 versus 14 (low ≤13, high ≥14), with a sensitivity of 86 % and a specificity of 87 %. The positive and negative predictive values were 76 and 93 %, respectively (Table 2).
Fig. 1.
Receiving operating characteristics curve of Cancer Worry Scale (CWS) scores against the FCRI-SF ≥ 16. Labeled points correspond to the CWS scores as follows: 1: 8 versus 9; 2: 9 versus 10; 3: 10 versus 11; 4: 11 versus 12; 5: 12 versus 13; 6: 13 versus 14; 7: 14 versus 15; 8: 15 versus 16; 9: 16 versus 17; 10: 17 versus 18; 11: 18 versus 19; 12: 20 versus 21; 13: 22 versus 23; 14: 23 versus 24
Table 2.
Accuracy measures for CWS scores according to FCRI-SF
| CWS cut-off | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|
| Score | (%) | (%) | (%) | (%) |
| 8 vs 9 | 100 | 28 | 39 | 100 |
| 9 vs 10 | 100 | 45 | 46 | 100 |
| 10 vs 11 | 96 | 61 | 54 | 97 |
| 11 vs 12 | 91 | 72 | 61 | 94 |
| 12 vs 13 | 91 | 81 | 69 | 95 |
| 13 vs 14 | 86 | 87 | 76 | 93 |
| 14 vs 15 | 73 | 89 | 76 | 88 |
| 15 vs 16 | 59 | 92 | 76 | 83 |
| 16 vs 17 | 41 | 100 | 100 | 78 |
| 17 vs 18 | 32 | 100 | 100 | 76 |
| 18 vs 19 | 27 | 100 | 100 | 75 |
| 20 vs 21 | 18 | 100 | 100 | 72 |
| 22 vs 23 | 14 | 100 | 100 | 71 |
| 23 vs 24 | 9 | 100 | 100 | 70 |
NPV negative predictive value, PPV positive predictive value
Reliability and measure of agreement
The CWS yielded a high internal consistency reliability coefficient, Cronbach α = 0.89. The correlation between the CWS and FCRI-SF was r = 0.85. In 87 % of the cases, there was agreement between the CWS and FCRI-SF concerning the presence or absence of a FCR diagnosis reflecting a Cohen’s kappa of 0.71 (SE 0.09).
Reliability
Prevalence and multidimensional aspects of high FCR
According to the established cut-off point of 14 or higher on the CWS, 29 survivors (38 %) had high levels of FCR. These individuals experienced significantly more psychological distress, functional impairments, and triggers, showed more insight, and sought reassurance more often than the individuals with lower levels of FCR (Table 3).
Table 3.
Means and standard deviations of the psychosocial variables
| Low FCR (n = 47) CWS < 14 |
High FCR (n = 29) CWS ≥ 14 |
||||
|---|---|---|---|---|---|
| EORTC QLQ-C30 | Mean | SD | Mean | SD | p value |
| Global health/QoLc | 77.6 | (19.1) | 56.7 | (26.7) | p < 0.001 |
| Physical functioningb | 81.1 | (21.9) | 68.5 | (30.7) | p = 0.052 |
| Role functioningc | 81.7 | (24.1) | 59.6 | (38.1) | p = 0.004 |
| Emotional functioningc | 93.5 | (11.3) | 72.4 | (23.9) | p < 0.001 |
| Cognitive functioningb | 86.5 | (18.9) | 68.6 | (25.1) | p = 0.001 |
| Social functioningc | 93.7 | (12.7) | 62.8 | (38.7) | p < 0.001 |
| EORTC QLQ-CR38 | |||||
| Body imagec | 91.4 | (15.1) | 70.4 | (32.8) | p < 0.001 |
| Sexual functioning | 23.0 | (22.6) | 20.4 | (19.8) | p = 0.623 |
| Future perspectivec | 88.9 | (15.9) | 56.8 | (27.4) | p < 0.001 |
| General distress | |||||
| HADS total | 5.5 | (5.0) | 13.8 | (6.9) | p < 0.001 |
| Cancer-specific distress | |||||
| IES total | 2.8 | (6.3) | 15.4 | (14.6) | p = 0.001 |
| Intrusion | 1.9 | (3.9) | 8.2 | (7.9) | p = 0.001 |
| Avoidance | 0.9 | (2.5) | 8.0 | (7.4) | p < 0.001 |
| FCRI | |||||
| Triggers | 6.3 | (5.6) | 15.5 | (5.6) | p < 0.001 |
| Psychological distress | 1.9 | (2.0) | 7.6 | (3.5) | p < 0.001 |
| Functioning impairments | 1.1 | (2.1) | 6.9 | (5.3) | p < 0.001 |
| Insight | 0.3 | (0.7) | 2.1 | (2.2) | p < 0.001 |
| Reassurance | 1.1 | (2.0) | 2.9 | (3.1) | p = 0.005 |
asmall difference 5–10 points
bmedium difference 10–20 points
clarge difference > 20 points
Relationship between FCR and demographic and medical variables
There were no differences in age (t(74) = 1.58, p = 0.12) or time since surgery (t(74) = −0.31, p = 0.76) between survivors with high or low levels of FCR. Chi-square tests showed categorical demographic (gender, partnership, children, educational level, employment status) and medical variables (location of tumor, stoma, disease stage, additional treatment) not to be associated with FCR.
Relationship between FCR and distress
Survivors with high levels of FCR experienced significantly more general distress (t(73) =−5.4, p < 0.001) and cancer-specific distress (t(26.5) =−3.9, p = 0.001) characterized by post-traumatic stress symptoms including significantly more intrusive (t(31.3) =−3.8, p = 0.001) and avoidant (t(27.2) =−4.6, p < 0.001) phenomena after the traumatic experience of cancer, than did survivors with low levels of FCR (Table 3).
Relationship between FCR and quality of life
Compared with low levels of FCR, high levels of FCR were associated with a poorer quality of life (F(1,66) = 14.1, p < 0.001) more impaired role functioning (F(1,66) = 8.7, p = 0.004), emotional functioning, (F(1,66) = 24.0, p < 0.001), cognitive functioning (F(1,66) = 11.2, p = 0.001), and social functioning (F(1,66) = 22.9, p < 0.001). Moreover, there were large (>20 points) clinically relevant differences between survivors with a high or low FCR in global quality of life, role functioning, emotional functioning, and social functioning. Survivors with a high FCR had significantly more problems with body image (F(1,70) = 13.7, p < 0.001) and future perspective (F(1,70) = 39.6, p < 0.001) than did survivors with a low FCR (Table 3).
Descriptive analyses FCRI
Triggers
Medical examinations, feeling sick or physically unwell, and an appointment with the doctor or other health professional were the most frequently reported triggers for high FCR with 48, 45 and 38 % respectively reporting them “most of the time” or “all the time”.
Psychological distress
When survivors with high FCR thought about the possibility of cancer recurrence, they felt helpless or resign and expressed worry, fear, or anxiety with 34 and 31 % respectively reporting them “most of the time” or “all the time”.
Functioning impairments
High FCR disrupted the ability to make future plans or set life goals, relationships with partner/ family, and general quality of life with 18, 17, and 17 % respectively reporting them “most of the time” or “all the time”.
Insight
Most survivors with high FCR did not feel that they worried excessively about the possibility of cancer recurrence or that other people thought they did with 76 and 86 % respectively reporting this “not at all” or “a little”.
Reassurance
Survivors with high FCR sought reassurance by going to the hospital or clinic for an examination or calling their doctor or another health professional with 21 and 21 % respectively reporting them “most of the time” or “all the time”. Few such individuals examined themselves to see if they have any physical signs of cancer with 10.7 % reporting this “most of the time” or “all the time”.
Coping strategies
Survivors with high FCR coped with this fear by trying to convince themselves that everything would be fine or think positively, trying to find a solution, and trying to replace this thought with a more pleasant with 39, 36, and 32 % respectively reporting them “most of the time” or “all the time”.
These individuals did not use coping strategies such as praying, meditating or relaxation, trying to distract themselves, or trying not think about it with 75, 61, and 57 % respectively reporting them “never” or “rarely”.
Severity
The thought that it is normal to be anxious or worried about the possibility of cancer recurrence and the experience of a lot of other unpleasant thoughts or images such as death, suffering, and consequences for family when thinking about the possibility of cancer recurrence were most frequently reported with 61 and 52 % respectively reporting them “most of the time” or “all the time”.
Discussion
This is one of the few studies to specifically focus on the prevalence and features associated with FCR in CRC survivors. FCR remains a significant problem for some CRC survivors even years after diagnosis, when routine follow-up care has normally ended. This study supported the reliability and criterion validity of the CWS in a sample of CRC survivors. Furthermore, the CWS showed good discriminatory power relative to the FCRI-SF, indicating that it is an appropriate instrument to identify those individuals who experience high FCR. Similar to the validated cut-off score in a sample of breast cancer survivors [23], a cut-off score of 14 or higher was optimal for differentiating a case from a non-case. With this cut-off point, about one third (38 %) of the survivors experienced high levels of FCR a median time of 5 years after surgery. Levels of FCR were not different for men or women, age, or medical characteristics. These findings are partly in line with the recent systematic review of Simard and colleagues [11] which showed moderate evidence (4 studies evidence; 12 studies no evidence) for a relation between FCR and gender and only weak to moderate evidence for a relation with disease and treatment characteristics. Although a relation between FCR and age is often observed in the literature, there was no significant correlation in this study. A possible explanation could be that there participated both males and females in this study. The systematic review of Simard and colleagues [11] namely revealed that in 18 studies, of which eight included samples of only males, no significant relationship with age was found. It might be the case that there is no association between age and FCR in male cancer survivors, and therewith, the relationship in this mixed sample disappeared.
In accordance with previous studies, the CRC survivors in this study reported a good global quality of life [6]. However, there were large statistically and clinically relevant differences between individuals who reported high or low levels of FCR, with high FCR being associated with a lower general quality of life, lower emotional functioning, role functioning and social functioning, and more problems with body image and future perspective. Furthermore, individuals with high FCR had higher levels of general distress and post-traumatic stress symptoms, such as avoidance and intrusions. This is consistent with the results of studies among cancer patients reporting that intrusive thoughts are more frequently related to future-oriented fears, such as FCR [34–38]. Simard and colleagues [13] revealed that the nature of these intrusive thoughts associated with FCR shares characteristics with worries, negative and uncontrollable thoughts on an issue whose outcome is uncertain but which contains the possibility a negative outcome [39]. More severe FCR tends to resemble obsession, defined as recurrent thoughts and images, experienced as intrusive and inappropriate, causing anxiety and psychological distress [40]. This was also supported by the results of this study since CRC survivors with high FCR reported unpleasant thoughts or images such as death, suffering, or consequences for family when thinking about the possibility of cancer recurrence as one of the most frequently occurring features of FCR. Furthermore, the results showed that high FCR is characterized by reactions to specific triggers, negative thoughts, and feelings accompanied by reassurance behavior. Interestingly, reassurance behavior mainly consisted of contact with one’s medical professional. Body checking occurred less frequently. An explanation for this finding might be that it is more difficult for CRC survivors to check their body for symptoms of recurrence than for breast cancer survivors. CRC survivors might be more focused on their defecation than on their body. Since CRC survivors with high FCR do not experience their fear as excessive or unreasonable (insight) but the focus seems meanwhile to be on dysfunctional thoughts or behaviors, CRC survivors with high FCR may benefit from cognitive behavior therapy [41–44].
The study had some limitations. The low response rate (38 %) and small sample size means that results might not be representative. It is possible that survivors who have been disease-free for a number of years might not want to think about hospitals and cancer research. Alternatively, it might be the survivors with the most severe problems, with high levels of FCR, or distress who do not participate. Despite the small sample size, statistically and clinically relevant differences were found between individuals with high and low levels of FCR, and descriptive analysis was possible.
Another limitation is the difference between responders and non-responders, which could be indicative of selection bias. However, compared to the Dutch cancer population at the time of this study, age categories, and gender distribution were quite similar, indicating that is was a representative sample [45].
Although reliability and criterion validity of the CWS were established in a population of CRC survivors, not all components of validity were assessed. Future research should address multiple components of validity.
Conclusions
This study emphasizes the need to focus on specific problems rather than general QoL, but these findings should be confirmed with a larger sample using a prospective design. We are currently investigating FCR, distress, and QoL in the first year after the diagnosis of CRC. Future research should aim to develop an evidence-based intervention for CRC survivors with high FCR, and the results of the current study may provide starting points for such an intervention.
Acknowledgments
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.van Erning FN, van Steenbergen LN, Lemmens VE, Rutten HJ, Martijn H, van Spronsen DJ, et al. Conditional survival for long-term colorectal cancer survivors in the Netherlands: who do best? Eur J Cancer. 2014;50:1731–9. doi: 10.1016/j.ejca.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 2.Bouvier AM, Jooste V, Bonnetain F, Cottet V, Bizollon MH, Bernard MP, et al. Adjuvant treatments do not alter the quality of life in elderly patients with colorectal cancer: a population-based study. Cancer. 2008;113:879–86. doi: 10.1002/cncr.23629. [DOI] [PubMed] [Google Scholar]
- 3.Gall CA, Weller D, Esterman A, Pilotto L, McGorm K, Hammett Z, et al. Patient satisfaction and health-related quality of life after treatment for colon cancer. Dis Colon Rectum. 2007;50:801–9. doi: 10.1007/s10350-006-0815-8. [DOI] [PubMed] [Google Scholar]
- 4.Wilson TR, Alexander DJ, Kind P. Measurement of health-related quality of life in the early follow-up of colon and rectal cancer. Dis Colon Rectum. 2006;49:1692–702. doi: 10.1007/s10350-006-0709-9. [DOI] [PubMed] [Google Scholar]
- 5.Smith-Gagen J, Cress RD, Drake CM, Romano PS, Yost KJ, Ayanian JZ. Quality-of-life and surgical treatments for rectal cancer—a longitudinal analysis using the California Cancer Registry. Psychooncology. 2010;19:870–8. doi: 10.1002/pon.1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jansen L, Koch L, Brenner H, Arndt V (2010) Quality of life among long-term (≥5 years) colorectal cancer survivors—systematic review. Eur J Cancer 46:2879–88 [DOI] [PubMed]
- 7.Wallner C, Lange MM, Bonsing BA, Maas CP, Wallace CN, Dabhoiwala NF, et al. Causes of fecal and urinary incontinence after total mesorectal excision for rectal cancer based on cadaveric surgery: a study from the Cooperative Clinical Investigators of the Dutch total mesorectal excision trial. J Clin Oncol. 2008;26:4466–72. doi: 10.1200/JCO.2008.17.3062. [DOI] [PubMed] [Google Scholar]
- 8.Santin O, Murray L, Prue G, Gavin A, Gormley G, Donnelly M. Self-reported psychosocial needs and health-related quality of life of colorectal cancer survivors. Eur J Oncol Nurs. 2015 doi: 10.1016/j.ejon.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 9.Vickberg SM. The Concerns About Recurrence Scale (CARS): a systematic measure of women’s fears about the possibility of breast cancer recurrence. Ann Behav Med. 2003;25:16–24. doi: 10.1207/S15324796ABM2501_03. [DOI] [PubMed] [Google Scholar]
- 10.Lee-Jones C, Humphris G, Dixon R, Hatcher MB. Fear of cancer recurrence—a literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psychooncology. 1997;6:95–105. doi: 10.1002/(SICI)1099-1611(199706)6:2<95::AID-PON250>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 11.Simard S, Thewes B, Humphris G, Dixon M, Hayden C, Mireskandari S, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7:300–22. doi: 10.1007/s11764-013-0272-z. [DOI] [PubMed] [Google Scholar]
- 12.Hodges LJ, Humphris GM. Fear of recurrence and psychological distress in head and neck cancer patients and their carers. Psychooncology. 2009;18:841–48. doi: 10.1002/pon.1346. [DOI] [PubMed] [Google Scholar]
- 13.Simard S, Savard J, Ivers H. Fear of cancer recurrence: specific profiles and nature of intrusive thoughts. J Cancer Surviv. 2010;4:361–71. doi: 10.1007/s11764-010-0136-8. [DOI] [PubMed] [Google Scholar]
- 14.Skaali T, Fossa SD, Bremnes R, Dahl O, Haaland CF, Hauge ER, et al. Fear of recurrence in long-term testicular cancer survivors. Psychooncology. 2009;18:580–88. doi: 10.1002/pon.1437. [DOI] [PubMed] [Google Scholar]
- 15.Cannon AJ, Darrington DL, Reed EC, Loberiza FR., Jr Spirituality, patients’ worry, and follow-up health-care utilization among cancer survivors. J Support Oncol. 2011;9:141–48. doi: 10.1016/j.suponc.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 16.Mikkelsen T, Sondergaard J, Sokolowski I, Jensen A, Olesen F. Cancer survivors’ rehabilitation needs in a primary health care context. Fam Pract. 2009;26:221–30. doi: 10.1093/fampra/cmp004. [DOI] [PubMed] [Google Scholar]
- 17.Deimling GT, Bowman KF, Sterns S, Wagner LJ, Kahana B. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology. 2006;15:306–20. doi: 10.1002/pon.955. [DOI] [PubMed] [Google Scholar]
- 18.Phipps E, Braitman LE, Stites S, Leighton JC. Quality of life and symptom attribution in long-term colon cancer survivors. J Eval Clin Pract. 2008;14:254–58. doi: 10.1111/j.1365-2753.2007.00842.x. [DOI] [PubMed] [Google Scholar]
- 19.Mullens AB, McCaul KD, Erickson SC, Sandgren AK. Coping after cancer: risk perceptions, worry, and health behaviors among colorectal cancer survivors. Psychooncology. 2004;13:367–76. doi: 10.1002/pon.751. [DOI] [PubMed] [Google Scholar]
- 20.Baker F, Denniston M, Smith T, West MM. Adult cancer survivors: how are they faring? Cancer. 2005;104(S11):2565–76. doi: 10.1002/cncr.21488. [DOI] [PubMed] [Google Scholar]
- 21.Steele N, Haigh R, Knowles G, Mackean M. Carcinoembryonic antigen (CEA) testing in colorectal cancer follow up: what do patients think? Postgrad Med J. 2007;83:612–14. doi: 10.1136/pgmj.2007.059634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simard S, Savard J. Screening and comorbidity of clinical levels of fear of cancer recurrence. J Cancer Surviv. 2015 doi: 10.1007/s11764-015-0424-4. [DOI] [PubMed] [Google Scholar]
- 23.Custers JAE, van den Berg SW, van Laarhoven HWM, Bleiker EMA, Gielissen MFM, Prins JB. The cancer worry scale: detecting fear of recurrence in breast cancer survivors. Cancer Nurs. 2014;37:E44–50. doi: 10.1097/NCC.0b013e3182813a17. [DOI] [PubMed] [Google Scholar]
- 24.Douma KFL, Aaronson NK, Vasen HFA, Gerritsma MA, Gundy CM, Janssen EP, et al. Psychological distress and use of psychosocial support in familial adenomatous polyposis. Psychooncology. 2010;19:289–98. doi: 10.1002/pon.1570. [DOI] [PubMed] [Google Scholar]
- 25.Simard S, Savard J. Fear of cancer recurrence inventory: development and initial validation of a multidimensional measure of fear of cancer recurrence. Support Care Cancer. 2009;17:241–51. doi: 10.1007/s00520-008-0444-y. [DOI] [PubMed] [Google Scholar]
- 26.Van der Ploeg E, Mooren TT, Kleber RJ, van der Velden PG, Brom D. Construct validation of the Dutch version of the impact of event scale. Psychol Assess. 2004;16:16–26. doi: 10.1037/1040-3590.16.1.16. [DOI] [PubMed] [Google Scholar]
- 27.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41:209–18. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Vodermaier A, Millman RD. Accuracy of the Hospital Anxiety and Depression Scale as screening tool in cancer patients: a systematic review and meta-analysis. Support Care Cancer. 2011;19:1899–908. doi: 10.1007/s00520-011-1251-4. [DOI] [PubMed] [Google Scholar]
- 29.Spinhoven PH, Ormel J, Sloekers PPA, Kempen GIJM, Speckens AEM, van Hemert AM. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27:363–370. doi: 10.1017/S0033291796004382. [DOI] [PubMed] [Google Scholar]
- 30.Aaronson N, Ahmedzai A, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 31.Sprangers MA, Te Velde A, Aaronson NK. The construction and testing of the EORTC colorectal cancer-specific quality of life questionnaire module (QLQ-CR38). European Organization for Research and Treatment of Cancer Study Group on Quality of Life. Eur J Cancer. 1999;35:238–47. doi: 10.1016/S0959-8049(98)00357-8. [DOI] [PubMed] [Google Scholar]
- 32.Osoba D, Rodrigues G, Myles J, Zee B, Pater J. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol. 1998;16:139–44. doi: 10.1200/JCO.1998.16.1.139. [DOI] [PubMed] [Google Scholar]
- 33.Weintraub D, Oehlberg KA, Katz IR, Stern MB. Test characteristics of the 15-item geriatric depression scale and Hamilton depression rating scale in Parkinson disease. Am J Geriatr Psychiatry. 2006;14:169–175. doi: 10.1097/01.JGP.0000192488.66049.4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kangas M, Henry JL, Bryant RA. The relationship between acute stress disorder and posttraumatic stress disorder following cancer. J Consult Clin Psychol. 2005;73:360–64. doi: 10.1037/0022-006X.73.2.360. [DOI] [PubMed] [Google Scholar]
- 35.Lebel S, Rosberger Z, Edgar L, Devins GM. Comparison of four common stressors across the breast cancer trajectory. J Psychosom Res. 2007;63:225–32. doi: 10.1016/j.jpsychores.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 36.McNally RJ. Progress and controversy in the study of posttraumatic stress disorder. Annu Rev Psychol. 2003;54:229–52. doi: 10.1146/annurev.psych.54.101601.145112. [DOI] [PubMed] [Google Scholar]
- 37.Whitaker KL, Brewin CR, Watson M. Intrusive cognitions and anxiety in cancer patients. J Psychosom Res. 2008;64:509–17. doi: 10.1016/j.jpsychores.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 38.Whitaker KL, Watson M, Brewin CR. Intrusive cognitions and their appraisal in anxious cancer patients. Psychooncology. 2009;18:1147–55. doi: 10.1002/pon.1512. [DOI] [PubMed] [Google Scholar]
- 39.Borkovec TD, Robinson E, Pruzinsky T, DePree JA. Preliminary exploration of worry: some characteristics and processes. Behav Res Ther. 1983;21:9–16. doi: 10.1016/0005-7967(83)90121-3. [DOI] [PubMed] [Google Scholar]
- 40.Rachman S. A cognitive theory of obsessions. Behav Res Ther. 1997;35:793–802. doi: 10.1016/S0005-7967(97)00040-5. [DOI] [PubMed] [Google Scholar]
- 41.Herschbach P, Berg P, Waadt S, Duran G, Engst-Hastreiter U, Henrich G, Book K, Dinkel A. Group psychotherapy of dysfunctional fear of progression in patients with chronic arthritis or cancer. Psychother Psychosom. 2010;79:31–8. doi: 10.1159/000254903. [DOI] [PubMed] [Google Scholar]
- 42.Herschbach P, Book K, Dinkel A, Berg P, Waadt S, Duran G, Engst-Hastreiter U, Hendrick G. Evaluation of two group therapies to reduce fear of progression in cancer patients. Support Care Cancer. 2010;18:471–479. doi: 10.1007/s00520-009-0696-1. [DOI] [PubMed] [Google Scholar]
- 43.Lebel S, Maheu C, Lefebvre M, Secord S, Courbasson C, Singh M, Jolicoeur L, Benea A, Harris C, Fung Kee Fung M, Rosberger Z, Catton P. Addressing fear of cancer recurrence among women with cancer: a feasibility and preliminary outcome study. J Cancer Surviv. 2014;8:485–496. doi: 10.1007/s11764-014-0357-3. [DOI] [PubMed] [Google Scholar]
- 44.Van de Wal MA, Gielissen MFM, Speckens AS, Prins JB. Managing fear of cancer recurrence with the SWORD study (Survivors’ Worries Of Recurrent Disease) Psycho-Oncology. 2013;22(Suppl 3):342. [Google Scholar]
- 45.Integraal Kankercentrum Nederland. Cijfers over kanker. Bron: Nederlandse Kankerregistratie, beheerd door IKNL© [Januari] (2015) http://www.cijfersoverkanker.nl/selecties/ Incidentie_darmkanker/img54dded375b587. Accessed 12 January 2015