Abstract
AIM: To assess the safety of single-incision laparoscopic cholecystectomy (SILC) for acute cholecystitis.
METHODS: All patients who underwent SILC at Sano Hospital (Kobe, Japan) between January 2010 and December 2014 were included in this retrospective study. Clinical data related to patient characteristics and surgical outcomes were collected from medical records. The parameters for assessing the safety of the procedure included operative time, volume of blood loss, achievement of the critical view of safety, use of additional trocars, conversion to laparotomy, intraoperative and postoperative complications, and duration of postoperative hospital stay. Patient backgrounds were statistically compared between those with and without conversion to laparotomy.
RESULTS: A total of 100 patients underwent SILC for acute cholecystitis during the period. Preoperative endoscopic treatment was performed for suspected choledocholithiasis in 41 patients (41%). The mean time from onset of acute cholecystitis was 7.7 d. According to the Updated Tokyo Guidelines (TG13) for the severity of cholecystitis, 86 and 14 patients had grade I and grade II acute cholecystitis, respectively. The mean operative time was 87.4 min. The mean estimated blood loss was 80.6 mL. The critical view of safety was obtained in 89 patients (89%). Conversion laparotomy was performed in 12 patients (12%). Postoperative complications of Clavien-Dindo grade III or greater were observed in 4 patients (4%). The mean duration of postoperative hospital stay was 5.7 d. Patients converted from SILC to laparotomy tended to have higher days after onset.
CONCLUSION: SILC is feasible for acute cholecystitis; in addition, early surgical intervention may reduce the risk of laparotomy conversion.
Keywords: Acute cholecystitis, Single-port access surgery, Single incision laparoscopic cholecystectomy, Single incision laparoscopic surgery, Laparo-endoscopic single-site surgery
Core tip: Single-incision laparoscopic cholecystectomy (SILC) has attracted attention as a minimally invasive procedure. A scar-less operation can be achieved by making a skin incision at the umbilicus. However, the safety of this procedure for acute cholecystitis has not been established. We reported 100 consecutive cases of SILC for acute cholecystitis and their surgical outcomes. SILC was safely performed in approximately 80% of cases in this series. We believe that the results of this study indicate the feasibility of SILC for acute cholecystitis.
INTRODUCTION
Cholecystectomy is widely performed as a basic treatment for acute cholecystitis. In the Updated Tokyo Guidelines issued in 2013 (TG13), early cholecystectomy is recommended as the first treatment choice, except for severe cases with organ failure[1]. Laparoscopic cholecystectomy (LC) is now a mainstream procedure. When performed by skilled surgeons, LC is considered a safe procedure even for acute cholecystitis[2].
In recent years, single-incision laparoscopic surgery (SILS) has attracted attention as a minimally invasive procedure. In SILS, multiple devices are inserted from a single skin incision into the abdominal cavity to reduce the length and number of incisions. In particular, scarless operations can be achieved by making skin incisions at the umbilicus[3]. Because cholecystectomy is performed in a nearly fixed visual field and because it does not require wide-range maneuvers, SILS is easily incorporated into cholecystectomy. SILC is becoming established as a procedural option.
However, there are limited reports on surgical outcomes of SILC for acute cholecystitis. Because maneuverability is limited in SILC compared with that in conventional LC, the safety of this procedure for acute cholecystitis has not yet been established. If SILC is as safe as conventional LC, SILC will become the procedure of choice for patients who desire better aesthetic outcomes. Although successful completion of SILC is a prerequisite for better aesthetic outcomes, data on acute cholecystitis are limited. At our hospital, we have focused on SILC and cases of acute cholecystitis. Thus, in order to address these clinical questions, we conducted a retrospective study of past cases. The objectives of this study were to assess the safety of SILC for acute cholecystitis and to investigate requirements for successful completion of SILC.
MATERIALS AND METHODS
This study included all patients who underwent SILC for acute cholecystitis at Sano Hospital (Kobe, Japan) between January 2010 and December 2014. Although SILC is, in principle, performed for all patients requiring cholecystectomy, four patients for whom laparoscopy had not been selected at the discretion of their attending physicians and one patient suspected to have concomitant gallbladder cancer were excluded. According to TG13[4], acute cholecystitis was diagnosed in patients who met all the following diagnostic criteria: (1) local inflammatory signs; (2) systemic inflammatory findings; and (3) characteristic imaging findings. Data were collected from medical records and analyzed. The parameters used to assess the safety of the surgery included operative time, volume of blood loss, achievement of the critical view of safety, use of additional trocars, conversion to laparotomy, intraoperative and postoperative complications, and duration of postoperative hospital stay.
Surgical technique
We performed SILC using a standard technique with conventional trocars and instruments. A 20-mm incision was first made at the umbilicus. An optical port, a 5-mm trocar, and 5-mm forceps were inserted in the incision. These three instruments were placed in a triangle to maximize their spacing. In addition, a 3- or 5-mm instrument was inserted beside the optical port. We did not use any devices specialized for SILS.
It is feasible to perform nearly the same surgical procedure as conventional LC because the potential interference of each device is minimized by direct insertion of two instruments without trocar. We made every effort to create the critical view of safety, as described by Strasberg. To prevent bile duct injury, we converted to open surgery when we could not create the critical view of safety or could not identify the cystic duct.
Drainage tubes were not routinely placed, even in cases of severe inflammation. However, we placed a drainage tube from the right lateral abdomen to the liver bed in cases of suspected remnant abscess or bile leakage.
Statistical analysis
The t test was used to assess differences in patient age, body mass index (BMI), and days from onset. The Fisher exact test was used to assess differences in all other factors. All tests were two-sided, and P-values less than 0.05 were considered to indicate a statistically significant difference. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria)[5].
RESULTS
Patient characteristics
During the study period, 100 patients underwent SILC for acute cholecystitis. Their mean age was 66.8 years. The male-to-female ratio was 51:49. Their mean BMI was 23.9 kg/m2. A history of some type of abdominal operation was found in 26 patients (26%). Choledocholithiasis was suspected in 41 patients (41%), based on imaging studies, and endoscopic lithotomy was performed before SILC. The mean time from the onset of acute cholecystitis to cholecystectomy was 7.7 d. According to TG13[4] guidelines for the severity of cholecystitis, 86 patients and 14 patients had grades I and II acute cholecystitis, respectively (Table 1).
Table 1.
Patient characteristics
| Acute cholecystitis (n = 100) | |
| Mean age (yr ± SD) | 66.8 ± 14.4 |
| Sex | |
| Male | 51 |
| Female | 49 |
| Mean BMI (kg/m2 ± SD) | 23.9 ± 3.3 |
| History of abdominal surgery | 26 (26%) |
| Suspected choledocholithiasis | 41 (41%) |
| Mean time from onset (d ± SD) | 7.7 ± 4.1 |
| TG13 severity grading | |
| Grade I(mild) | 86 (86%) |
| Grade II (moderate) | 14 (14%) |
SD: Standard deviation; BMI: Body mass index; TG13: Updated Tokyo Guidelines.
Surgical outcomes
The surgical outcomes are shown in Table 2. The mean operative time was 87.4 min, and the mean estimated blood loss volume was 80.6 mL. The critical view of safety was achieved in 89 patients (89%), although anterograde dissection of the gall bladder starting from the fundus was required for 42 of these patients. Additional trocar insertion was required in 9 patients (9%). SILC was converted to laparotomy in 12 patients (12%). A drainage tube was placed in 13 patients (13%), including 4 patients with necrotizing cholecystitis. Postoperative complications of Clavien-Dindo grade III or greater were observed in 4 patients (4%). The complications included leakage of bile from the stump of the cystic duct and passage of stones into the common bile duct in two patients each. These complications were resolved in all four patients using only endoscopic treatment. The mean postoperative hospital stay was 5.7 d.
Table 2.
Surgical outcomes
| Acute cholecystitis (n = 100) | |
| Mean operative time (min ± SD) | 87.4 ± 39.3 |
| Mean estimated blood loss (mL ± SD) | 80.6 ± 162.4 |
| Achievement of critical view of safety | 89 (89%) |
| Additional trocar insertion | 9 (9%) |
| Conversion to laparotomy | 12 (12%) |
| Postoperative complication | 4 (4%) |
| Bile leakage | (2) |
| Stone passage into the CBD | (2) |
| Mean duration of postoperative hospital stay (d ± SD) | 5.7 ± 5.1 |
SD: Standard deviation; CBD: Common bile duct.
Histological diagnosis
Histological diagnoses of the resected gallbladders included acute-on-chronic cholecystitis in 61 patients, edematous cholecystitis in 9 patients, necrotizing cholecystitis in 8 patients, suppurative cholecystitis in 5 patients, and xanthogranulomatous cholecystitis in 1 patient. Incidental adenocarcinomas were founded in 3 patients (Table 3).
Table 3.
Histological diagnoses of resected gallbladder for acute cholecystitis
| n = 100 | |
| Edematous cholecystitis | 9 |
| Necrotizing cholecystitis | 8 |
| Suppurative cholecystitis | 5 |
| Chronic cholecystitis | 74 |
| (Acute on chronic cholecystitis) | (61) |
| Xanthogranulomatous cholecystitis | 1 |
| Adenocarcinoma | 3 |
Comparison of patients with and without conversion to laparotomy
The results of comparison between patients with and without conversion to laparotomy are shown in Table 4 and Figure 1. Despite the lack of statistical significance, the number of days after onset tended to be higher in patients who were converted from SILC to laparotomy.
Table 4.
Comparison of patients with and without conversion to laparotomy
| Without conversion (n = 88) | With conversion (n = 12) | P value | |
| Mean age (yr ± SD) | 66.1 ± 14.5 | 71.6 ± 13.3 | NS |
| Sex | |||
| Male | 44 | 7 | NS |
| Female | 44 | 5 | |
| Mean BMI (kg/m2 ± SD) | 23.9 ± 3.1 | 24.1 ± 4.7 | NS |
| History of abdominal surgery | 22 (25%) | 4 (33.3%) | NS |
| TG13 severity grading | |||
| Grade I (mild) | 82 (93.2%) | 4 (33.3%) | P < 0.001 |
| Grade II (moderate) | 6 (6.8%) | 8 (66.7%) | |
| Mean time from onset (d ± SD) | 7.5 ± 4.0 | 9.1 ± 4.4 | NS |
SD: Standard deviation; NS: Not significant; BMI: Body mass index; TG13: Updated Tokyo Guidelines.
Figure 1.
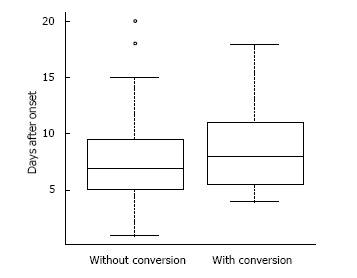
Time after onset of acute cholecystitis. Patients with conversion to laparotomy show a tendency toward increased preoperative days from onset.
Learning curve
The mean operative times of every five consecutive cases of SILC performed by a chief surgeon are shown in Figure 2. There were no obvious trends suggestive of a learning curve.
Figure 2.
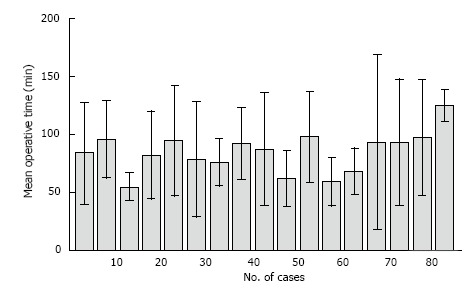
Mean operative time for every five consecutive cases of single-incision laparoscopic cholecystectomy for acute cholecystitis. All 85 cases performed by a chief surgeon are shown above. The standard deviation of each group is also shown. There are no obvious trends suggestive of a learning curve.
DISCUSSION
Although Navarra et al[6] first reported SILC in 1997, it did not initially attract much attention. However, SILC has been rapidly adopted since 2009, with improvements to platforms and devices dedicated for SILS[7-11]. Since then, SILS has been increasingly used, mainly because of its excellent aesthetic outcome; it has been widely applied not only to cholecystectomy, but also to appendectomy, colectomy, gastrectomy, urologic procedures, and gynecologic procedures[12-16]. LC in particular is relatively easy to perform with SILS, and SILC is routinely performed. The reasons for this include: (1) the surgical field is limited to the liver bed; (2) the direction of scopes and devices remains almost constant; (3) the procedure is mainly indicated for benign conditions; and (4) many patients undergoing the procedure are young. However, the drawbacks of SILS include: (1) the limited maneuverability of scopes and devices that may interfere with one another; and (2) difficulty in setting devices at different angles, as all devices are oriented in the same direction. Compared with conventional LC, SILC is technically more difficult. Because advanced endoscopic surgical techniques are required to perform SILC, it is a difficult procedure for less experienced surgeons. However, these obstacles have been gradually eliminated owing to advances such as the innovation of techniques appropriate for SILS, development of dedicated platforms, and introduction of pre-bending forceps[7,17-20].
Several randomized controlled trials (RCTs) have revealed that SILC is as safe as conventional LC[21-23]. However, to our knowledge, no RCT has assessed only patients with acute cholecystitis, for which SILC is technically more difficult, and the safety of SILC for acute cholecystitis has not been established. Thus, we reviewed 100 consecutive cases of SILC performed for acute cholecystitis and reported their surgical outcomes. The operative time tended to be longer in patients with cholecystitis; this likely reflects the difficulty of operative maneuvers. Moreover, the volume of intraoperative blood loss also tended to be higher; this may be attributable to the facts that (1) the gallbladder and its surrounding tissue affected by acute inflammation are more likely to bleed because they are congested and become edematous; and (2) the hepatic parenchyma is easily damaged because of inflammatory adherence of the gallbladder to the liver bed. These findings suggest that SILC for acute cholecystitis involves some level of difficulty. Thus, application of SILC should require careful consideration.
However, we performed SILC in all patients with acute cholecystitis who were judged to require cholecystectomy, and SILC was successfully completed without additional trocars in approximately 80% of cases. These findings indicate that SILC is applicable to many patients, even those with acute cholecystitis. Moreover, because the complication rate in this study is not higher than that reported in another study[23], we believe that SILC for acute cholecystitis is as safe as other surgical procedures under the conditions described in this study. In other words, the results of our study suggest that SILC can be performed in patients with acute cholecystitis without compromising safety. At minimum, there appears to be no need to exclude patients with acute cholecystitis from SILC.
New procedures typically have learning curves. However, there was no evidence of a learning curve for SILC for acute cholecystitis in this study. This observation may be owing to the quality of the surgeons in our study. All surgeons who participated in this study were experienced and skilled in laparoscopic surgery and had each experienced more than 10 cases of SILC. Moreover, our SILC surgical procedure can be learned in a short time because of its similarity to conventional LC. However, the learning curve may be more obvious in less experienced surgeons.
SILC was introduced in our hospital in 2009. It was performed only in select patients during the early period after introduction while accumulating knowledge and standardizing the techniques used during the surgical procedure. Since January 2010, SILC has been applied to all patients, except those with gallbladder cancer. When the procedure is performed, we place the most emphasis on safety. Our policy is to convert SILC to laparotomy without hesitation when any difficulties present during the laparoscopic operation. The rate of conversion to laparotomy in the present study was slightly higher in patients with acute cholecystitis, likely owing to this policy. Consequently, no serious complications occurred, and excellent safety was demonstrated. Although the incidence of complications related with the bile duct was slightly high, this is likely because our institution specializes in endoscopic treatment. Many patients with suspected common bile duct problems seek treatment at our hospital. In fact, 41% of patients in this study were recommended to our facility for suspected choledocholithiasis and they underwent endoscopic treatment before cholecystectomy. This factor may have contributed to the increased incidence of these complications. Although bile leakage occurred in two patients with acute cholecystitis, it was not caused by damage during a laparoscopic operation, as neither case had been converted to laparotomy. While the common bile duct was not damaged in any of the patients, leakage was resolved by endoscopic biliary drainage after surgery. To maintain the safety of SILC, surgeons should never perform reckless operative maneuvers and convert to laparotomy before performing risky maneuvers.
However, a desire to avoid conversion to laparotomy is reasonable without compromising safety in terms of aesthetic outcome. In this study, SILC was converted to laparotomy in 12 patients (12%). The main reason for conversion was difficulties during the laparoscopic operation because of severe inflammatory fibrosis (10 patients). Operation difficulties owing to inflammation are reported related to the elapsed time between disease onset and operation[24]. The results of this study indicate that the number of preoperative days after onset tended to be higher in patients who were converted from SILC to laparotomy. Based on these findings, SILC performed as early as possible may permit resection before development of inflammatory fibrosis, and thus reduce the risk of laparotomy conversion. Avoiding laparotomy results in a less invasive procedure, less postoperative pain, and shorter postoperative hospital stay, making the merits offered by SILC more attractive. The TG13 recommends performing cholecystectomy within 72 h[25]. Unfortunately, we could not perform early surgery in many cases because of the lack of smooth cooperation with the first-contact physicians, limited availability of operation theater space, and lack of anesthetist availability. Despite our efforts to overcome these issues, some patients were unable to undergo early cholecystectomy. Conversely, in patients for whom early operation is not feasible, conservative treatment and elective SILC after complete suppression of inflammation may be preferable.
In conclusion, the results of this study suggest that SILC is feasible for acute cholecystitis and that early surgical intervention may reduce the risk of conversion to laparotomy. Although an aesthetic outcome is important, the decision to convert to laparotomy should be made based on other factors. We hope that SILC will be considered a safe procedure and be more widely used.
COMMENTS
Background
Cholecystectomy is widely performed as a basic treatment for acute cholecystitis. Laparoscopic cholecystectomy (LC) is considered a safe procedure and widely performed for acute cholecystitis.
Research frontiers
Recently, single-incision laparoscopic cholecystectomy (SILC) has been rapidly adopted over conventional LC. SILC is considered a less invasive procedure with better aesthetic results. However, the safety of this procedure for acute cholecystitis has not yet been established.
Innovations and breakthroughs
In this study, the authors reviewed 100 consecutive cases of SILC for acute cholecystitis and reported their surgical outcomes. The authors focused on SILC as well as accumulated cases of acute cholecystitis. This study is based on single-institution and consecutive experiences.
Applications
The results of this study suggest the safety and difficulty of SILC for acute cholecystitis. SILC is feasible for acute cholecystitis. However, surgeons should not hesitate to convert to laparotomy when difficulties arise.
Terminology
SILC is also called single-port access surgery or laparo-endoscopic single-site surgery. It is a minimally invasive surgical procedure with a single skin incision. Scarless operations can be achieved by making a skin incision at the umbilicus. However, SILC is technically more difficult because of the limited maneuverability. Advanced laparoscopic surgical skills are required for SILC.
Peer-review
The authors retrospectively assessed the safety of SILC for acute cholecystitis. They concluded that SILC is feasible for acute cholecystitis and that early surgical intervention may reduce the risk of conversion to laparotomy. This article is of interest for further clinic practice.
Footnotes
P- Reviewer: Augustin G, Kim KH, Zhu YL S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
Institutional review board statement: The study was reviewed and approved by the Sano Hospital Institutional Review Board.
Informed consent statement: All study participants provided informed consent prior to study enrollment.
Conflict-of-interest statement: The authors have no conflict of interest directly relevant to the contents of this study.
Data sharing statement: No additional data are available.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: June 27, 2015
First decision: August 16, 2015
Article in press: November 4, 2015
References
- 1.Miura F, Takada T, Strasberg SM, Solomkin JS, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Yoshida M, Mayumi T, et al. TG13 flowchart for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:47–54. doi: 10.1007/s00534-012-0563-1. [DOI] [PubMed] [Google Scholar]
- 2.Kiviluoto T, Sirén J, Luukkonen P, Kivilaakso E. Randomised trial of laparoscopic versus open cholecystectomy for acute and gangrenous cholecystitis. Lancet. 1998;351:321–325. doi: 10.1016/S0140-6736(97)08447-X. [DOI] [PubMed] [Google Scholar]
- 3.Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy : scarless cholecystectomy. Surg Endosc. 2009;23:1393–1397. doi: 10.1007/s00464-008-0252-y. [DOI] [PubMed] [Google Scholar]
- 4.Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, Pitt HA, Garden OJ, Kiriyama S, Hata J, et al. TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos) J Hepatobiliary Pancreat Sci. 2013;20:35–46. doi: 10.1007/s00534-012-0568-9. [DOI] [PubMed] [Google Scholar]
- 5.Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–458. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:695. [PubMed] [Google Scholar]
- 7.Kroh M, Rosenblatt S. Single-port, laparoscopic cholecystectomy and inguinal hernia repair: first clinical report of a new device. J Laparoendosc Adv Surg Tech A. 2009;19:215–217. doi: 10.1089/lap.2008.0081. [DOI] [PubMed] [Google Scholar]
- 8.Langwieler TE, Nimmesgern T, Back M. Single-port access in laparoscopic cholecystectomy. Surg Endosc. 2009;23:1138–1141. doi: 10.1007/s00464-009-0389-3. [DOI] [PubMed] [Google Scholar]
- 9.Merchant AM, Cook MW, White BC, Davis SS, Sweeney JF, Lin E. Transumbilical Gelport access technique for performing single incision laparoscopic surgery (SILS) J Gastrointest Surg. 2009;13:159–162. doi: 10.1007/s11605-008-0737-y. [DOI] [PubMed] [Google Scholar]
- 10.Romanelli JR, Roshek TB, Lynn DC, Earle DB. Single-port laparoscopic cholecystectomy: initial experience. Surg Endosc. 2010;24:1374–1379. doi: 10.1007/s00464-009-0781-z. [DOI] [PubMed] [Google Scholar]
- 11.Ito M, Asano Y, Horiguchi A, Shimizu T, Yamamoto T, Uyama I, Miyakawa S. Cholecystectomy using single-incision laparoscopic surgery with a new SILS port. J Hepatobiliary Pancreat Sci. 2010;17:688–691. doi: 10.1007/s00534-010-0266-4. [DOI] [PubMed] [Google Scholar]
- 12.Zhou H, Jin K, Zhang J, Wang W, Sun Y, Ruan C, Hu Z. Single incision versus conventional multiport laparoscopic appendectomy: a systematic review and meta-analysis of randomized controlled trials. Dig Surg. 2014;31:384–391. doi: 10.1159/000369217. [DOI] [PubMed] [Google Scholar]
- 13.Ma CC, Li P, Wang LH, Xia ZY, Wu SW, Wang SJ, Lu CM. The value of single-incision laparoscopic surgery for colorectal cancer: a systematic literature review. Hepatogastroenterology. 2015;62:45–50. [PubMed] [Google Scholar]
- 14.Inaki N. Reduced port laparoscopic gastrectomy: a review, techniques, and perspective. Asian J Endosc Surg. 2015;8:1–10. doi: 10.1111/ases.12163. [DOI] [PubMed] [Google Scholar]
- 15.Tam YH, Pang KK, Tsui SY, Wong YS, Wong HY, Mou JW, Chan KW, Houben CH, Sihoe JD, Lee KH. Laparoendoscopic single-site nephrectomy and heminephroureterectomy in children using standard laparoscopic setup versus conventional laparoscopy. Urology. 2013;82:430–435. doi: 10.1016/j.urology.2013.02.057. [DOI] [PubMed] [Google Scholar]
- 16.Murji A, Patel VI, Leyland N, Choi M. Single-incision laparoscopy in gynecologic surgery: a systematic review and meta-analysis. Obstet Gynecol. 2013;121:819–828. doi: 10.1097/AOG.0b013e318288828c. [DOI] [PubMed] [Google Scholar]
- 17.Abe N, Takeuchi H, Ohki A, Aoki H, Masaki T, Mori T, Sugiyama M. Single-incision multiport laparoendoscopic surgery using a newly developed short-type flexible endoscope: a combined procedure of flexible endoscopic and laparoscopic surgery. J Hepatobiliary Pancreat Sci. 2012;19:426–430. doi: 10.1007/s00534-011-0454-x. [DOI] [PubMed] [Google Scholar]
- 18.Dominguez G, Durand L, De Rosa J, Danguise E, Arozamena C, Ferraina PA. Retraction and triangulation with neodymium magnetic forceps for single-port laparoscopic cholecystectomy. Surg Endosc. 2009;23:1660–1666. doi: 10.1007/s00464-009-0504-5. [DOI] [PubMed] [Google Scholar]
- 19.Idani H, Nakano K, Asami S, Kubota T, Komoto S, Kurose Y, Kubo S, Nojima H, Hioki K, Kin H, et al. “Hook and roll technique” using an articulating hook cautery to provide a critical view during single-incision laparoscopic cholecystectomy. Acta Med Okayama. 2013;67:259–263. doi: 10.18926/AMO/51071. [DOI] [PubMed] [Google Scholar]
- 20.Yin H, Wang Z, Xu J, Guan Y, Zhai B, Zhao L. A specific instrument to facilitate single-incision laparoscopic cholecystectomy: an initial experience. Surg Innov. 2011;18:289–293. doi: 10.1177/1553350611401428. [DOI] [PubMed] [Google Scholar]
- 21.Arezzo A, Scozzari G, Famiglietti F, Passera R, Morino M. Is single-incision laparoscopic cholecystectomy safe? Results of a systematic review and meta-analysis. Surg Endosc. 2013;27:2293–2304. doi: 10.1007/s00464-012-2763-9. [DOI] [PubMed] [Google Scholar]
- 22.Geng L, Sun C, Bai J. Single incision versus conventional laparoscopic cholecystectomy outcomes: a meta-analysis of randomized controlled trials. PLoS One. 2013;8:e76530. doi: 10.1371/journal.pone.0076530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.He GL, Jiang ZS, Cheng Y, Lai QB, Zhou CJ, Liu HY, Gao Y, Pan MX, Jian ZX. Tripartite comparison of single-incision and conventional laparoscopy in cholecystectomy: A multicenter trial. World J Gastrointest Endosc. 2015;7:540–546. doi: 10.4253/wjge.v7.i5.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lo CM, Liu CL, Fan ST, Lai EC, Wong J. Prospective randomized study of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Ann Surg. 1998;227:461–467. doi: 10.1097/00000658-199804000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yamashita Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Gomi H, Dervenis C, Windsor JA, et al. TG13 surgical management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:89–96. doi: 10.1007/s00534-012-0567-x. [DOI] [PubMed] [Google Scholar]


