Abstract
Lung herniation has been defined as a protrusion of lung tissue through its bounding structure. We present a case of spontaneous intercostal lung herniation following bouts of cough, which was complicated by multiple rib fractures, in which we had to adopt a non-surgical approach due to the clinical circumstance. Its understanding in the field of internal medicine is important as appropriate therapeutic judgment, and long-term follow-up is essential for full recovery.
INTRODUCTION
Lung herniation was defined as a protrusion of lung tissue through its bounding structure by Roland in 1499 [1]. Classification is based on the location (cervical, intercostal and diaphragmatic) and the cause (congenital and acquired). Herniations are further classified as traumatic, post-thoracotomy and spontaneous [2]. Spontaneous lung herniation accounts for 30% of the total cases [3, 4]. Most of the spontaneous lung hernias are uncomplicated, but some of them can complicate by rib fractures, lung incarcerations and infections. We present a case of spontaneous intercostal lung herniation following bouts of cough, which was complicated by multiple rib fractures, in which we had to adopt a non-surgical approach due to the clinical circumstance.
CASE REPORT
A 65 years old man presented to the emergency department with left-sided flank pain that started after a popping sound was heard following a cough spell. There was no history of trauma. He is an active smoker, and his past medical history includes congestive heart failure, hypertension, coronary artery disease, diabetes mellitus, chronic pain secondary to lumbar disc disease requiring multiple epidural injections and multiple orthopedic procedures including knee replacement and rotator cuff repair. He did not have any history of surgical procedures on his chest wall. His medications included hydrochlorothiazide, lisinopril, metoprolol, metformin, aspirin, clopidogrel and diclofenac. Examination was negative for any tenderness or deformity on the left flank. Electrocardiogram was unremarkable, and chest X-ray was negative for any acute pathology. He was discharged home on pain medications with a diagnosis of muscular spasm. A few days later, he represented with non-resolution of symptoms. This time on examination he was found to have a large hematoma of the left flank tracking inferiorly to the left gluteus. There was no fullness, tenderness or crepitus on palpation. Computed tomography (CT) thorax revealed a chest wall defect on the left side between eighth and ninth ribs with herniation of lung tissue (Fig. 1, red arrow) and a 5 cm × 3 cm hematoma but did not reveal any fractures. He was managed conservatively with pain medications as there was no evidence of vascular compromise to the lung tissue. A month later, he presented again with poorly controlled chest pain and shortness of breath. Chest X-Ray showed stable herniation of lung tissue with widening of eighth intercostal space (Fig. 2). Subsequent CT thorax revealed progression of lung herniation (Fig. 3, red arrow) associated with left lower lobe atelectasis, alongside acute, displaced fractures of left eighth and ninth ribs (Fig. 3, green arrow). No surgical repair was performed based on a recent positive stress test and his elevated perioperative risk of cardiovascular events. He was discharged on opioid pain medications. At the follow-up visit, he still continues to have pain in the left lower chest, even though he is on a high dose of pain medications. We also tried intercostal nerve blocks, which seems to be ineffective in his case. There appears to be some respiratory compromise unsure whether secondary to chronic heart failure or ‘lung herniation fracture’.
Figure 1:
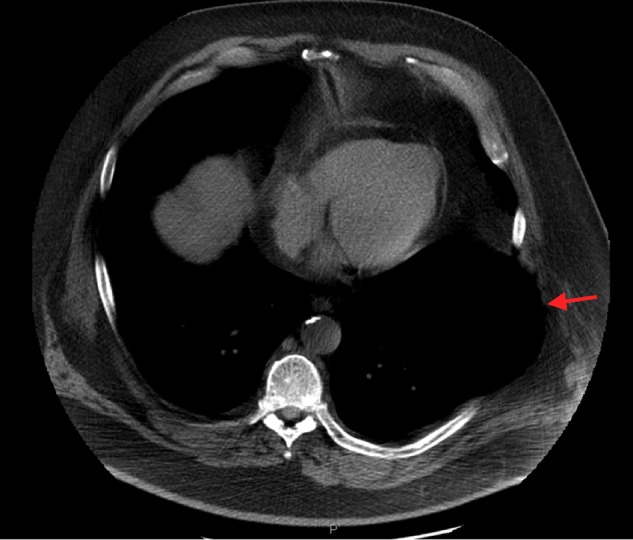
CT thorax: transverse view on initial presentation showing the presence of lung herniation (red arrow) without any rib fracture.
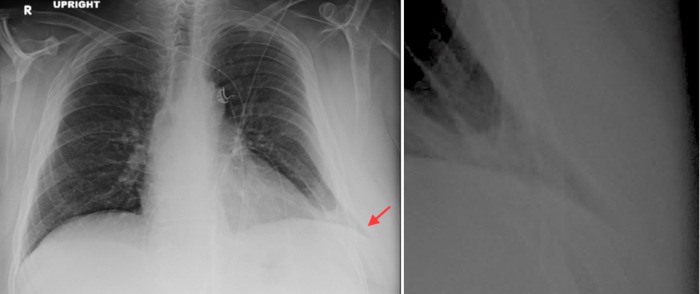
Figure 2:
Chest radiograph posterior–anterior view showing lung field extending outside the rib cage demonstrated by the red arrow (left) with a magnified image (right). This finding is well known as ‘lung beyond rib sign’.
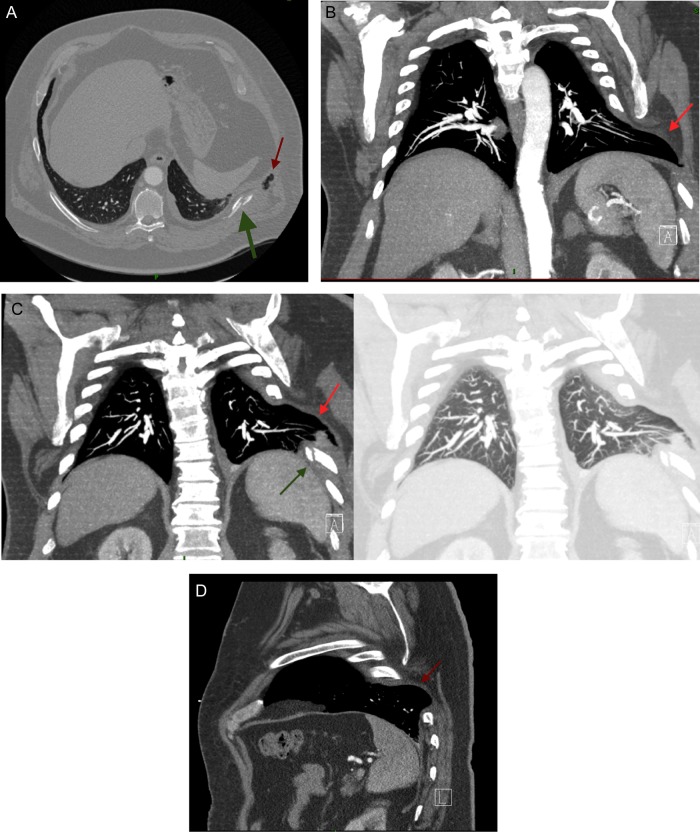
Figure 3:
(A) CT thorax: transverse plane. Showing the displaced fracture of ninth rib (green arrow) with a small amount of lung tissue seen outside the rib cage (red arrow). (B) CT thorax: coronal view better demonstrating the extent of herniation (red arrow). (C) CT thorax coronal plane: (left) regular window showing a displaced ninth rib fracture (green arrow) and lung tissue outside the rib cage (red arrow); (right) lung window confirming the lung tissue outside the rib cage. (D) CT thorax: sagittal view demonstrating lung herniating through the posterior intercostal space (red arrow), most common site being the region between the vertebrae and the costal angle.
DISCUSSION
The basic mechanics of lung herniation includes protrusion of lung tissue through a defect in the chest wall caused by (i) sudden increase in the intrathoracic pressure superimposed on a (ii) weakness or opening in the chest wall. Weak areas in the chest wall could be congenital or acquired. Congenital weakness in the thoracic wall occurs due to disruption in endo-thoracic fascia. Acquired defects in the chest wall occur usually due to trauma or a prior thoracic surgery. Some other causes of acquired defect on the basis of predisposition have been combined together in a single entity and named ‘pathologic hernias’. These include chest wall abscess, empyema, osteomyelitis, malignancy or tuberculosis [5]. Several causes of sudden increase in intrathoracic pressure have been reported including coughing fits mostly seen in patients with chronic obstructive airway disease especially with long-term steroid use, sneezing, playing a musical instrument or lifting heavy weight [6, 7]. Uncomplicated spontaneous lungs hernias are usually asymptomatic. However, they could present as palpable, soft mass that enlarge with coughing or Valsalva. A chest radiograph is used for initial evaluation. Positive findings include the presence of lung field outside the rib cage also known as ‘lung beyond rib sign’ (Fig. 2) or a focal lucent area on the lung field called ‘lucent lung sign’. It is important to note that the chest radiograph might be completely normal even in the presence of hernia. A CT scan of the thorax provides valuable information regarding the extent of the hernia and the presence of associated complications (Fig. 3). A common site of predilection in the anterior thoracic wall is the area between the eighth and ninth ribs because of the absence of external intercostal muscle in that region, whereas in the posterior thoracic wall, the area from vertebrae to the costal angle is more prone to a hernia due to the absence of internal intercostal muscle in that region (Fig. 3D). Management of these hernias in the past used to be conservative with thoracic strapping; however, this method has been abandoned due to the risk of impaired thoracic wall motion, which reduces the pulmonary compliance and increases the incidence of atelectasis and infection. Early surgical repair has shown the best results with low morbidity and excellent long-term prognosis [5]. Several methods of surgical repair have been described either with or without the use of prosthetic patch [6]. A video thoracoscopic repair was suggested by Reardon et al. for traumatic hernia repair [8]. However, no one method is applicable for every single hernia, and the approach is individualized [7]. The basic concept of surgical repair includes approximation of ribs and stabilization of intercostal space. Rib fractures have been reported several times in association with lung herniation especially in traumatic injuries [9]. The presence of these fractures increases the risk of other complications including incarceration due to entrapment of lung tissue in the broken rib spicules [5]. In such cases, repair of lung parenchyma or even resection of lung tissue has been described [10]. Several methods for the repair of rib fractures have been described in the literature; but because of the rarity of a rib fracture associated with a spontaneous lung hernia, there lacks a common consensus on the best approach for management, and hence most clinicians continue to rely on case reports and expert opinion when encountered with this condition. In our case, the ideal approach would have been a surgical repair; but due to the cardiovascular perioperative risk, any surgical intervention was disregarded. Although uncomplicated small hernias have shown to have a fair prognosis with a conservative approach, the presence of rib fractures creates a therapeutic dilemma in old patients with high perioperative risk.
Fewer than 300 cases of lung hernia have been reported, most of them being case reports in the surgical and radiology journals. Its understanding in the field of internal medicine is important as appropriate therapeutic judgment, and long-term follow-up is essential for full recovery. For the best clinical outcome in terms of decreased morbidity or mortality, an early surgical intervention may be adopted irrespective of the severity of the hernia. But if encountered by an increased surgical risk, a conservative approach is acceptable, although it does significantly affect the quality of life even after maximal therapy especially in the presence of a complication.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Montgomery JG, Lutz H. Hernia of the lung. Ann Surg 1925;82:220–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sulaiman A, Cottin V, De Souza Neto EP, Orsini A, Cordier J-F, Gamondes J-P et al. Cough-induced intercostals lung herniation requiring surgery: report of a case. Surg Today 2006;36:978–980. [DOI] [PubMed] [Google Scholar]
- 3.Hiscoe DB, Digman GJ. Types and incidence of lung hernias. J Thorac Cardiovasc Surg 1955;30:335–342. [PubMed] [Google Scholar]
- 4.Moncada R, Vade A, Gimenez C, Rosado W, Demos TC, Turbin R et al. Congenital and acquired lung hernias. J Thorac Imag 1996;11:75–82. [DOI] [PubMed] [Google Scholar]
- 5.Scullion DA, Negus R, Al-Kutoubi A. Case report: extrathoracic herniation of the lung with a review of the literature. Br J Radio 1994;67:94–96. [DOI] [PubMed] [Google Scholar]
- 6.Brock MV, Heitmiller RF. Spontaneous anterior lung hernias. J Thorac Cardiovasc Surg 2000;119:1046–1047. [DOI] [PubMed] [Google Scholar]
- 7.Weissberg D, Refaely Y. Hernia of the lung. Ann Thorac Surg 2002;74:1963–1966. [DOI] [PubMed] [Google Scholar]
- 8.Reardon MJ, Fabre J, Reardon PR, Baldwin JC. Video-assisted repair of a traumatic intercostal pulmonary hernia. Ann Thorac Surg 1998;65:1155–1157. [DOI] [PubMed] [Google Scholar]
- 9.May AK, Chan B, Daniel TM, Young JS. Anterior lung herniation: another aspect of the seatbelt syndrome. J Trauma 1995;38:587–589. [DOI] [PubMed] [Google Scholar]
- 10.Allen GS, Fischer RP. Traumatic lung herniation. Ann Thorac Surg 1997;63:1455–1456. [DOI] [PubMed] [Google Scholar]