Abstract
Objectives
To evaluate the long-term effects of two non-face-to-face treatment programmes for stress urinary incontinence (SUI) based on pelvic floor muscle training (PFMT).
Subjects and Methods
The present study was a randomized controlled trial with online recruitment of 250 community-dwelling women aged 18–70 years with SUI ≥ one time/week. Diagnosis was based on validated self-assessed questionnaires, 2-day bladder diary and telephone interview with a urotherapist. Consecutive computer-generated block randomization was carried out with allocation by an independent administrator to 3 months of treatment with either an internet-based treatment programme (n = 124) or a programme sent by post (n = 126). Both interventions focused mainly on PFMT. The internet group received continuous e-mail support from a urotherapist, whereas the postal group trained on their own. Follow-up was performed after 1 and 2 years via self-assessed postal questionnaires. The primary outcomes were symptom severity (International Consultation on Incontinence Questionnaire Short Form [ICIQ-UI SF]) and condition-specific quality of life (ICIQ-Lower Urinary Tract Symptoms Quality of Life [ICIQ-LUTSqol]). Secondary outcomes were the Patient Global Impression of Improvement, health-specific quality of life (EQ-visual analogue scale [EQ-VAS]), use of incontinence aids, and satisfaction with treatment. There was no face-to-face contact with the participants at any time. Analysis was based on intention-to-treat.
Results
We lost 32.4% (81/250) of participants to follow-up after 1 year and 38.0% (95/250) after 2 years. With both interventions, we observed highly significant (P < 0.001) improvements with large effect sizes (>0.8) for symptoms and condition-specific quality of life (QoL) after 1 and 2 years, respectively. No significant differences were found between the groups. The mean (sd) changes in symptom score were 3.7 (3.3) for the internet group and 3.2 (3.4) for the postal group (P = 0.47) after 1 year, and 3.6 (3.5) for the internet group and 3.4 (3.3) for the postal group (P = 0.79) after 2 years. The mean changes (sd) in condition-specific QoL were 5.5 (6.5) for the internet group and 4.7 the for postal group (6.5) (P = 0.55) after 1 year, and 6.4 (6.0) for the internet group and 4.8 (7.6) for the postal group (P = 0.28) after 2 years. The proportions of participants perceiving they were much or very much improved were similar in both intervention groups after 1 year (internet, 31.9% [28/88]; postal, 33.8% [27/80], P = 0.82), but after 2 years significantly more participants in the internet group reported this degree of improvement (39.2% [29/74] vs 23.8% [19/80], P = 0.03). Health-specific QoL improved significantly in the internet group after 2 years (mean change in EQ-VAS, 3.8 [11.4], P = 0.005). We found no other significant improvements in this measure. At 1 year after treatment, 69.8% (60/86) of participants in the internet group and 60.5% (46/76) of participants in the postal group reported that they were still satisfied with the treatment result. After 2 years, the proportions were 64.9% (48/74) and 58.2% (46/79), respectively.
Conclusion
Non-face-to-face treatment of SUI with PFMT provides significant and clinically relevant improvements in symptoms and condition-specific QoL at 1 and 2 years after treatment.
Keywords: stress urinary incontinence, randomized controlled trial, long-term, eHealth, pelvic floor muscle training, self-management
Introduction
Stress urinary incontinence (SUI) is the leakage of urine in association with laughing, coughing or exertion [1]. SUI affects 10–35% of women [2] and is the most common type of female incontinence [3]. First-line treatment can be provided in primary care and includes pelvic floor muscle training (PFMT), information and lifestyle advice [4–6]. A few small studies also suggest that cognitive behavioural therapy might improve symptoms and quality of life (QoL) in patients with urinary incontinence [7,8].
Although there is effective treatment available, only 10–20% of those who are affected seek care. Some women are not troubled enough by the leakage to seek treatment, and others avoid seeking care because of shame or embarrassment [2]. In addition, access to care could vary depending on location and the healthcare system. Furthermore, after having sought care, not all women receive the best treatment [9], due to symptoms not being taken seriously [10], a lack of knowledge among healthcare personnel [11] and low priority of the condition in times of financial constraint. Thus, there is a need for new and easily accessible ways to provide treatment.
Technological advances have brought about new possibilities for providing care. Although access to the internet is greater in high-income countries, it is increasing rapidly all over the world. In 2013, 94% of the Swedish population aged 16–74 years had access to a computer with an internet connection at home [12]. The corresponding proportions in the UK and US were 83% [13] and 76%, respectively [14]. The internet is an important source of health information, and 72% of American internet users go online for this purpose [15]. Women are more likely than men to use the internet for information on their health [15], especially for issues that are perceived as embarrassing [16]. Internet-based treatments have been developed and shown to be effective for numerous conditions, such as headaches, obesity, chronic pain and irritable bowel syndrome [17]. Many patients appreciate internet-based treatment and perceive it as time-sparing, flexible and convenient [18–20]. Moreover, the barrier to seeking care seems lower on the internet compared with ordinary care [19].
Our research group previously compared the short-term effects of an internet-based treatment programme for SUI based on PFMT and a treatment programme sent by post in a randomized controlled trial (RCT). After 4 months, both groups had achieved highly significant and clinically relevant improvements in symptoms and QoL, but with no significant differences between the groups. Compared with the postal group, women in the internet group reported greater subjective improvements, greater reduction in their use of incontinence aids and greater satisfaction with the treatment programme [21]. Although there was no face-to-face contact at any time during assessment or treatment, the participants reported that they felt acknowledged and supported in their situation [22]. The internet-based treatment was also found to be more cost-effective than the postal treatment [23].
Although the literature provides strong evidence of the short-term beneficial effects of PFMT for SUI [2,4,6,24], questions regarding the long-term outcome are still unanswered [24,25]. In a 2013 systematic review, Bo and Hilde [25] concluded that 41–85% of initial responders report long-term success, and ≈70% remain satisfied after 5 years. However, meta-analysis was not possible in the review, due to the high heterogeneity of the available data, and there is a need for more studies of the long-term effects.
The aim of the present study was to evaluate the long-term effects of two non-face-to-face treatment programmes for SUI based on PFMT: one internet-based and one sent by post.
Patients and Methods
The present study reports the long-term (1- and 2-year follow-up) results of an RCT comparing the effect of two different treatment programmes for SUI based on PFMT. The RCT was registered at http://www.clinicaltrials.gov, ID number NCT01032265. The recruitment of participants, assessment, interventions and short-term (4-month follow-up) results were reported previously [21].
Briefly, we recruited 250 women aged 18–70 years with SUI ≥ one time/week via our open access website. After self-assessment with validated questionnaires, 2-day bladder diaries and a telephone interview with a urotherapist to confirm the clinical diagnosis of SUI, we consecutively randomized eligible participants to one of the treatments (internet-based treatment programme, n = 124; postal treatment programme, n = 126). Exclusion criteria were ongoing pregnancy, previous incontinence surgery, difficulties passing urine, macroscopic haematuria, known malignancy in the lower abdomen, intermenstrual bleeding, severe psychiatric disorders and neurological disease with affection on sensibility in the legs or lower abdomen. The duration of the treatment programmes was 3 months. Both interventions were based on PFMT with an intensity of at least eight contractions three times per day and included information on SUI, lifestyle advice and training reports. Participants in the internet-based group received asynchronous, individually tailored e-mail support from a urotherapist during the treatment period, while participants in the postal group trained on their own. The internet programme contained eight escalating levels, and also included cognitive behavioural therapy assignments for lifestyle changes (if applicable) and for the identification and changes in behaviours of avoidance and/or redundant security measures (if applicable). At the end of the treatment period, we advised participants in the internet group to continue training two to three times per week at the highest level of the programme they had achieved. Participants in the postal group were advised to continue training but with no specification of frequency.
We collected follow-up data at 4 months (previously reported) [21], 1 year and 2 years after starting treatment. There was no face-to-face contact with the participants at any time.
Outcome Measures
Primary outcomes
Symptom severity was measured using the validated [26] and highly recommended [4–6] International Consultation on Incontinence Questionnaire Short Form (ICIQ-UI SF), which contains three scored items on the frequency, amount and overall bother of the leakage. The scoring is additive (0–21), and higher scores indicate greater severity. For additional analyses, the material was categorized into severity groups [27] according to the baseline score (overall score 1–5, slight; 6–12, moderate; 13–18, severe; 19–21, very severe).
Condition-specific QoL was measured using the validated [28–30] and highly recommended [4–6] International Consultation on Incontinence Questionnaire Lower Urinary Tract Symptoms Quality of Life (ICIQ-LUTSqol). This questionnaire contains 19 items on various aspects of QoL that might be affected by the leakage, such as the ability to work, travel, exercise, family life, sexuality, mood, energy and sleep. Each item is scored on a scale of 1–4 (not at all/never, slightly/sometimes, moderately/often, a lot/all the time), resulting in an additive score ranging from 19 to 76, with higher values indicating greater impact. Three items concerning personal relationships have an additional potential answer: ‘not applicable’.
Secondary outcomes
The Patient Global Impression of Improvement (PGI-I) is a validated [31], clinically relevant and simple question asking participants to rate their condition now compared with before treatment. The question has seven answer alternatives ranging from very much better to very much worse.
Health-specific QoL was measured with the Euroqol visual analogue scale (EQ-VAS) [32], a vertical scale from 0 (worst imaginable health state) to 100 (best imaginable health state). Use of incontinence aids was evaluated by determining the proportion of participants using any absorbent incontinence aid within the last 4 weeks.
Satisfaction with treatment was evaluated by asking the participants to rate how satisfied they were with the results of treatment. This question had four response options: very satisfied, quite satisfied, quite dissatisfied and very dissatisfied. Participants were also asked whether they wanted additional treatment or were satisfied with the treatment outcome.
Statistical Analysis
We saved overall scores in the ICIQ-UI SF and ICIQ-LUTSqol by replacing occasional missing answers in the 1-year and 2-year follow-up with the corresponding answer in the previously completed follow-up (i.e. the 4-month and 1-year follow-up, respectively). In the ICIQ-UI SF, three scores were saved in this manner (1-year follow up, n = 1; 2-year follow-up, n = 2). In the ICIQ-LUTSqol we saved five scores, all in the 1-year follow-up. When calculating the overall scores in the ICIQ-LUTSqol, we set the value of the answer option ‘not applicable’ in items on personal relationships to 1.
For the baseline comparison of the two intervention groups and analysis of the baseline characteristics of participants lost to follow-up, we used Student's t test for continuous variables and the chi-squared or Fischer's exact test for categorical variables. For the primary outcomes and EQ-VAS, we used paired t tests to evaluate treatment effects within the groups and a mixed model analysis to evaluate treatment effects between the groups. We also analysed the primary outcomes by age (<50 years: baseline [n = 140], 1 year [n = 83], 2 years [n = 75]; ≥50 years: baseline [n = 110], 1 year [n = 86], 2 years [n = 80]) and severity group at baseline (slight: baseline [n = 14]; 1 year [n = 11], 2 years [n = 11]; moderate: baseline [n = 170], 1 year [n = 119], 2 years [n = 110]; severe: baseline [n = 64], 1 year [n = 38], 2 years [n = 33]; very severe: baseline [n = 2], 1 year [n = 1], 2 years [n = 1]). In these statistical analyses, we combined the severe and very severe groups. The PGI-I and satisfaction with treatment are both questions with ranked answers, and we used the Wilcoxon/Mann–Whitney rank sum test to evaluate the differences between the treatment groups. For incontinence aids, we used McNemar's test to evaluate treatment effects within groups and the chi-squared test to evaluate differences between the groups.
We also calculated the effect sizes (mean standardized difference) for each continuous measure, and considered effect sizes >0.8 to be large.
The analysis was intention-to-treat and performed using all available data [33]. Participants who had surgery (n = 8) or sought other treatment (n = 11) during the follow-up period were included in the analysis. We used IBM-SPSS for Mac version 21.0 (IBM, Armonk, NY, USA) and considered P < 0.05 to be significant.
Ethics
We received ethical approval for the study from the Regional Ethical Review Board, Umeå University (number 08-124M). All participants provided informed consent for participation. No reimbursements were given.
Results
We conducted the study in Sweden from December 2009 to April 2013. The enrolment of study participants is shown in Fig.1.
Fig. 1.
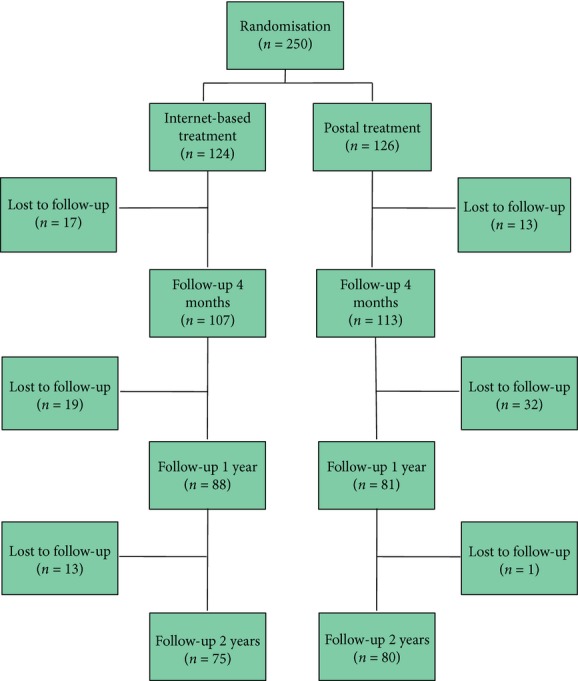
Study participant enrolment workflow.
We found no significant differences between the treatment groups at baseline with regard to age, parity, internet usage, education, menopausal status, smoking, use of incontinence aids or mean score on the ICIQ-UI SF and ICIQ-LUTS QoL (Table 1). We lost 32.4% (81/250) of participants to follow-up at 1 year, 29.0% (36/124) from the internet arm and 35.7% (45/126) from the postal arm. At 2 years we lost 38.0% (95/250) of participants to follow-up, 39.5% (49/124) from the internet arm and 36.5% (46/126) from the postal arm. Compared with those who completed the study, participants lost to follow-up after 1 and 2 years were significantly younger and reported larger impacts on their condition-specific QoL at baseline. Participants lost to follow-up after 2 years had more severe leakage at baseline than did completers, but this difference was not observed after 1 year. There were no differences regarding education or internet usage (Table 2).
Table 1.
Baseline demographics and incontinence severity by treatment group
| Variable | Internet-based treatment (n = 124) | Postal treatment (n = 126) | P value* |
|---|---|---|---|
| Baseline demographics | |||
| Mean (sd) | |||
| Age, years | 47.9 (10.6) | 49.4 (9.8) | NS |
| BMI, kg/m2 | 24.7 (4.2) | 24.5 (3.6) | NS |
| Parity | 2.2 (0.9) | 2.3 (0.8) | NS |
| EQ-VAS score | 79.1 (13.6) | 79.2 (14.0) | NS |
| Internet use, h/week | 13.5 (11.0) | 15.8 (13.1) | NS |
| Education, n (%) | |||
| Primary and lower secondary | 4 (3.2) | 1 (0.8) | NS |
| Upper secondary | 32 (25.8) | 25 (19.8) | |
| Post-secondary | 88 (71.0) | 100 (79.4) | |
| Postmenopausal, n (%) | 43 (35.8) | 48 (39.7) | NS |
| Daily smoker, n (%) | 4 (3.2) | 5 (4.0) | NS |
| Incontinence severity | |||
| Mean (sd) | |||
| Use of incontinence aids, per week | 6.8 (7.4) | 7.7 (8.2) | NS |
| ICIQ-UI SF score | 10.4 (3.1) | 10.3 (3.5) | NS |
| ICIQ-LUTSqol score | 33.6 (6.8) | 33.6 (8.2) | NS |
Based on Student's t test (means) or chi-squared/Fisher's exact test (numbers).
Table 2.
Comparison of baseline data between participants lost to follow-up and those who completed follow-up at 1 and 2 years
| Baseline data | Completed follow-up 1 year (n = 169) | Lost to follow-up 1 year (n = 81) | P value* | Completed follow-up 2 years (n = 155) | Lost to follow-up 2 years (n = 95) | P value* |
|---|---|---|---|---|---|---|
| Continuous variables, mean (sd) | ||||||
| Age, years | 50.3 (10.1) | 45.1 (9.5) | <0.001 | 50.4 (10.8) | 45.7 (8.5) | <0.001 |
| ICIQ-UI SF, overall score | 10.1 (3.2) | 10.9 (3.5) | NS | 10.0 (3.2) | 11.1 (3.4) | 0.008 |
| ICIQ-LUTSqol, overall score | 32.7 (6.8) | 35.5 (8.6) | <0.001 | 32.5 (6.8) | 35.5 (8.2) | 0.004 |
| Internet use, h/week | 14.3 (12.2) | 15.4 (12.0) | NS | 13.5 (11.4) | 16.6 (13.0) | NS |
| Categorical variable, n (%) | ||||||
| Education | ||||||
| Primary and lower secondary | 3 (1.8) | 2 (2.5) | NS | 3 (1.9) | 2 (2.1) | NS |
| Upper secondary | 38 (22.5) | 19 (23.4) | 32 (20.7) | 25 (26.3) | ||
| Post-secondary | 128 (75.7) | 60 (74.1) | 120 (77.4) | 68 (71.6) | ||
Based on Student's t test (means) or Fisher's exact test (numbers). NS, not significant (P > 0.05).
After 1 year, 9.6% (16/167) of the participants had sought other SUI care, 12.3% (19/154) after 2 years. The distributions per group and treatment received are reported in Table 3. The overall surgical rates were 3.0% (5/167) after 1 year and 5.2% (8/154) after 2 years of follow-up. There were no significant differences between the groups. At 1 and 2 years, 32.4% and 34.9% of the participants, respectively, reported that they performed PFMT regularly (≥one time/week). There were no differences between the groups.
Table 3.
Number of participants seeking other care and kind of care received after 1 and 2 years of follow-up
| 1-year follow-up |
2–year follow-up |
|||
|---|---|---|---|---|
| Internet (n = 87) | Postal (n = 80) | Internet (n = 75) | Postal (n = 79) | |
| Have sought other care since baseline* | 7 (8.0) | 9 (11.3) | 9 (12.0) | 10 (12.7) |
| Treatment† | ||||
| SUI surgery | 2 (2.3) | 3 (3.8) | 4 (5.3) | 4 (5.1) |
| Other PFMT regimen | 2 (2.3) | 1 (1.3) | – | – |
| Electrostimulation | – | – | 1 (1.3) | – |
| Medication | – | 3 (2.5) | – | 3 (3.8) |
| Incontinence aids | 1 (1.1) | 2 (2.5) | 1 (1.3) | 3 (3.8) |
| Waiting for treatment | 3 (3.4) | 1 (1.3) | 1 (1.3) | 2 (2.5) |
| None | 1 (1.1) | 1 (1.3) | 2 (2.7) | 1 (1.3) |
Data are presented as n (%).
No significant differences between the groups after 1 and 2 years of follow-up.
Some participants reported more than one treatment.
Primary Outcomes
Within both treatment groups, there were highly significant improvements in the primary outcomes, ICIQ-UI SF and ICIQ-LUTSqol, after 1 and 2 years compared with the baseline. The differences between the groups were not significant. In Table 4, we report the overall scores, mean differences and effect sizes for each measure. Improvements occurred mainly within the first 4 months and then persisted throughout the follow-up period (Fig.2).
Table 4.
Summary of continuous outcome measures by treatment group
| Outcome variable | Treatment group | Baseline (n = 250) | 1-year follow-up (n = 169) | Difference* | Within-group P† | Between-group P‡ | Effect size§ (95% CI) | 2-years follow-up (n = 155) | Difference* | Within-group P† | Between-group P‡ | Effect size§ (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary outcomes | ||||||||||||
| ICIQ-UI SF | Internet | 10.4 (3.1) | 6.6 (3.1) | 3.7 (3.3) | <0.001 | 0.47 | 1.22 (0.90–1.54) | 6.5 (3.0) | 3.6 (3.5) | <0.001 | 0.79 | 1.20 (0.86–1.55) |
| Postal | 10.3 (3.5) | 6.7 (3.2) | 3.2 (3.4) | <0.001 | 0.97 (0.64–1.30) | 6.4 (3.5) | 3.4 (3.3) | <0.001 | 0.99 (0.66–1.32) | |||
| ICIQ-LUTSqol | Internet | 33.6 (6.8) | 27.5 (6.1) | 5.5 (6.5) | <0.001 | 0.55 | 0.91 (0.60–1.22) | 26.5 (5.2) | 6.4 (6.0) | <0.001 | 0.28 | 1.13 (0.79–1.48) |
| Postal | 33.6 (8.2) | 27.8 (5.7) | 4.7 (6.5) | <0.001 | 0.70 (0.38–1.02) | 27.2 (6.4) | 4.8 (7.6) | <0.001 | 0.69 (0.38–1.01) | |||
| Secondary outcome | ||||||||||||
| EQ-VAS | Internet | 79.1 (13.6) | 80.4 (13.7) | 2.0 (13.3) | 0.17 | 0.56 | 0.14 (−0.16 to 0.45) | 83.3 (13.2) | 3.8 (11.4) | 0.005 | 0.81 | 0.29 (−0.03 to 0.61) |
| Postal | 79.2 (14.0) | 83.4 (12.3) | 1.7 (12.9) | 0.25 | 0.13 (−0.18 to 0.45) | 83.5 (12.2) | 2.8 (14.4) | 0.09 | 0.22 (−0.09 to 0.53) | |||
Values are means (sd) unless otherwise stated.
Based on participants with complete data on both occasions;
based on paired t tests;
based on a mixed model analysis;
mean standardized difference.
Fig. 2.
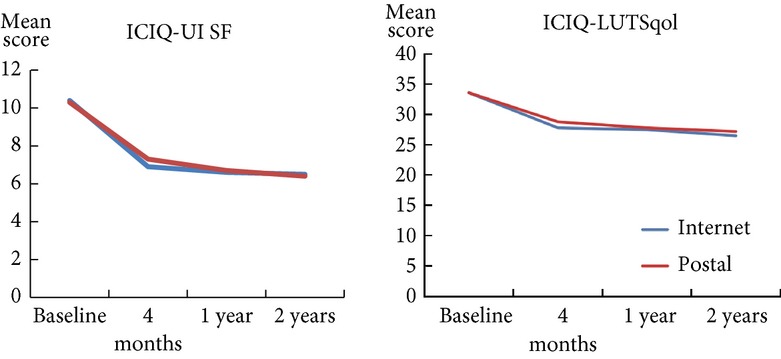
Improvement of primary outcomes during 2 years of follow-up.
Analysis by baseline age and severity (internet and postal groups combined) showed significant (P < 0.001) improvements in the symptom scores (ICIQ-UI SF) and condition-specific QoL (ICIQ-LUTSqol) in both age groups (<50 and ≥50 years of age) and in the groups with moderate and severe leakage. In the group with slight leakage at baseline, symptom scores improved significantly (P < 0.05) after 1 year, but not after 2 years.
Secondary Outcomes
The distribution of the responses in the PGI-I is shown in Fig.3. The difference between the groups was not significant after 1 year (P = 0.82). After 2 years, significantly more participants in the internet group rated their leakage as much or very much improved (39.2%, 29/74) than was the case in the postal group (23.8%, 19/80, P = 0.03).
Fig. 3.
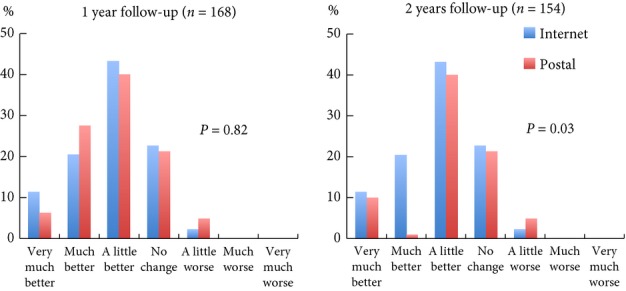
Distribution of responses on the PGI-I rating scale after 1 and 2 years of follow-up. P value is based on the Mann–Whitney rank sum test.
Health-specific QoL did not improve significantly in any of the treatment groups after 1 year. However, after 2 years there was significant improvement within the internet group, but not within the postal group. The differences between the groups were not significant (Table 4).
Among those who completed the 1-year follow-up, incontinence aids were used at baseline by 75.0% (63/84) in the internet group and 73.4% (58/79) in the postal group. After 1 year, the proportion using incontinence aids was significantly lower in both groups (internet group, 47.6% [40/84], P < 0.001; postal group, 57.0% [45/79], P = 0.001). Similarly, among those who completed the 2-year follow-up, 74.0% (54/73) in the internet group and 72.2% (57/79) in the postal group used incontinence aids at baseline, and the proportions were significantly lower after 2 years (internet group, 45.2% [33/73], P < 0.001; postal group, 53.2% [42/79], P < 0.001). The type of incontinence aid used (panty liner, small or large incontinence aid) did not change over time.
At 1 year after treatment, 69.8% (60/86) of the participants in the internet group and 60.5% (46/76) of the participants in the postal group reported that they were satisfied with the treatment results. In the internet group, 60.7% (51/84) of participants indicated that they did not want additional treatment, compared with 53.8% (42/78) in the postal group. After 2 years, the proportions of participants satisfied with treatment were 64.9% (48/74) and 58.2% (46/79) in the internet and postal groups, respectively. Further treatment was not considered necessary by 64.9% (48/74) of participants in the internet group and 59.5% (47/79) in the postal group. The differences between the groups were not significant.
Excluding participants who underwent surgery during the follow-up period did not affect the results.
Discussion
In the present study, we have presented the long-term results of two non-face-to-face treatment programmes for SUI based on PFMT, one internet-based and one sent by post. Two years after treatment, both groups showed highly significant improvements, with large effect sizes for symptom score and QoL, but we found no significant differences between the groups. However, compared with the postal group, significantly more participants in the internet group perceived that they were much or very much improved after treatment. In both groups, the proportion of women using incontinence aids was significantly reduced and, overall, almost two-thirds of the women were still satisfied with the treatment results after 2 years.
Strengths and Weaknesses of the Study
One strength of the present study is that it was conducted by an experienced research group consisting of GPs, urotherapists, psychologists and a statistician, all with broad knowledge of the topic. We adhered to existing guidelines, and for transparency we reported the study to http://www.clinicaltrials.gov. The study design is head-to-head, and we compared two active treatments developed by the research group according to the best available knowledge at the time. The outcomes were the same as in our short-term evaluation of the interventions, and most of the measures are highly recommended, validated and well established. An intention-to-treat analysis was possible because there were no differences between the groups with regard to surgical rates and other treatments received during the follow-up period. In addition, the long follow-up period contributes new knowledge.
The weaknesses of the study include not comparing the internet programme with a care-as-usual alternative, but for SUI no such standardized alternative exists. Also, handouts for the self-completion of PFMT are sometimes considered a sham treatment, but in our everyday practice, such handouts are used as an active treatment. Participants in the postal group were informed that they received active treatment, and the postal programme was extensive compared with other handouts. Furthermore, the loss to follow-up might have affected the results of the present study. Others have reported losses to follow-up of 0–39% at 1–15 years after SUI treatment [25]. The numbers in the present study are at the upper end of this range (38% after 2 years), most likely due to its non-face-to-face design. Participants lost to follow-up were younger and had a more severe leakage, but the loss to follow-up was similar in both treatment groups. Also, symptoms and QoL improved significantly in both age groups and in all severity groups except one (slight, n = 11). Therefore, we consider the risk of follow-up bias as little, and it should not have significantly affected the comparison between the groups.
Stress urinary incontinence is a dynamic condition and during the 2-year follow-up period some participants might have experienced spontaneous improvement, while others might have experienced a shift towards increased severity over time [34]. The distribution of such participants is likely to be equal in both groups and should not affect the comparison between the groups.
Strengths and Weaknesses Compared with the Literature
We think that our population represents a clinically relevant sample for a primary care setting, because all participants experienced leakage of such severity that they actively wanted treatment. A large proportion of our population was highly educated (75.2% had post-secondary education), but this may not contradict the applicability of the results to a more general population. Although some studies suggest that SUI could be more prevalent in women with a higher level of education [35,36], the online recruitment process probably contributed to the high education level of our participants. Women with a higher education level may be more active, more aware of their health status, have lower thresholds for reporting symptoms [36], have greater internet access [12] and use the internet more often to search for health information [15] compared with women with less education. However, Henderson et al. [37] previously concluded that education does not interfere with the ability to learn and perform PFMT, and others have suggested that socioeconomic status [38] and education level [39] do not affect adherence to treatment.
Both intervention arms were offered non-face-to-face treatment, and all participants completed the PFMT on their own without any previous examination or face-to-face supervision. The intensity of the training (≥eight contractions three times a day) followed the recommendations of the National Institute for Health and Clinical Excellence (NICE) guidelines [6]. However, the literature is not clear on whether PFMT should be supervised. The NICE guidelines [6] and the ICS [5] recommend supervised training. This approach is also supported by a 2011 Cochrane report [40], although it concluded that there is not enough evidence to make any strong recommendations. On the other hand, an American review from 2012 concluded that self-completed PFMT is as effective as supervised training with regard to the rates of treatment failure and discontinuation and the likelihood of improving SUI symptoms, improving QoL and achieving continence [4]. Moreover, clinical expertise assumes that digital assessment of pelvic floor contraction before starting treatment could aid the woman in performing future PFMT [6], but Henderson et al. [37] recently showed that 83.4% of women with SUI could contract their pelvic floor muscles correctly on the first attempt, and of those who could not, 88% learned after a short verbal cue.
We found no other studies reporting long-term (≥1 year) effects of PFMT measured with the ICIQ-UI SF; thus, relevant comparisons are difficult. However, our long-term (2 years follow-up) improvements in the ICIQ-UI SF (mean change, internet, 3.6; postal, 3.4) are of the same order of magnitude as short-term results from studies on supervised training. For example, Hirakawa et al. [41] reported an improvement of 3.4 and 3.7 in 46 women with SUI ≥ 1 week after 3 months of PFMT with and without biofeedback, respectively. The improvements we report (mean change in ICIQ-UI SF as mentioned earlier; mean change in ICIQ-LUTSqol, internet, 6.4; postal, 4.8) are likely to be detectable for individual women and considered clinically relevant. The minimum important differences in overall ICIQ-UI SF and ICIQ-LUTSqol scores in women treated with PFMT for SUI were previously determined to be 2.5 and 3.7, respectively [42]. The surgical rates in both intervention arms were low (internet, 5.3%; postal, 5.1%) compared with the literature, which has reported surgical rates of between 4.9% and 58% [25]. In addition, the proportion of women satisfied with treatment after 2 years corresponds well with previous reports in which ≈ two-thirds of patients are improved or cured by PFMT [4,24].
Clinical Implications and Future Research
We have shown that women with SUI treated based on PFMT and without face-to-face contact maintain the same amount of improvement after 2 years as they do directly after the cessation of active treatment. The degree of improvement was clinically relevant in both treatment groups and the overall surgery rates were low after 2 years. Although internet-based treatment seems to be more effective than postal treatment in some of the measures, no significant differences were found between the treatments for the main outcomes. For now, treatment choice is probably best based on the preference of each woman, but to enable individual treatment recommendations to be made, more research is needed on the factors that predict a successful outcome. More research is also needed on the kinds of women that choose this treatment approach and why they do so. Other potential developments include translation of the programmes into other languages for more widespread use and increased accessibility. The programmes could also be compared with PFMT supervised by an expert nurse or physiotherapist, and also developed to treat other kinds of urinary incontinence.
Healthcare systems face great challenges, and increased self-management using non-face-to-face treatment could be one way to meet future demands. In addition to adding value for the individual patient, this approach might reduce the need for support from the healthcare system, thereby saving its resources for those who prefer face-to-face contact or those with implicit needs. When implemented, the effects of the study treatments would need to be carefully followed because a clinical population is likely to be more diverse and the circumstances less controlled than in an RCT. However, if the treatment programmes can be successfully implemented in everyday practice, they have the potential to increase access to care and the quality of care given to women with SUI in a sustainable way.
Conclusion
Women with SUI achieved long-term, highly significant and clinically relevant improvements in symptoms and QoL with PFMT delivered without face-to-face contact as either an internet-based or postal programme.
Acknowledgments
We would like to thank the participating women for their time and engagement. Many thanks also to our urotherapists Eva Källström and Annika Andreasson and our coordinator Susanne Johansson for all their effort with this work. The present study was supported by the Swedish Council for Working Life and Social Research, Region Jämtland Härjedalen, The Västerbotten County Council (ALF) and Visare Norr, Northern County Councils, Sweden.
Glossary
- EQ-VAS
EQ-visual analogue scale
- ICIQ-LUTSqol
ICIQ-Lower Urinary Tract Symptoms Quality of Life
- ICIQ-UI SF
International Consultation on Incontinence Questionnaire Short Form
- NICE
National Institute for Health and Clinical Excellence
- PFMT
pelvic floor muscle training
- QoL
quality of life
- RCT
randomized controlled trial
- SUI
stress urinary incontinence
Conflict of Interest
None declared.
References
- 1.Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4–20. doi: 10.1002/nau.20798. [DOI] [PubMed] [Google Scholar]
- 2.Milsom I, Altman D, Lapitan MC, Nelson R, Sillén U, Thom D. Epidemiology of urinary (UI) and faecal (FI) incontinence and pelvic organ prolapse (POP) In: Paul Abrams LC, Saad K, Alan W, editors. Incontinence, 4th International Consultation on Incontinence, Paris July 5–8, 2008 4th Edition 2009. Paris: Health Publication Ltd; 2009. pp. 35–113. [Google Scholar]
- 3.Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of incontinence in the County of Nord-Trondelag. J Clin Epidemiol. 2000;53:1150–7. doi: 10.1016/s0895-4356(00)00232-8. [DOI] [PubMed] [Google Scholar]
- 4.Shamliyan T, Wyman J, Kane RL. Nonsurgical Treatments for Urinary Incontinence in Adult Women: Diagnosis and Comparative Effectiveness. Rockville: Agency for Heathcare Research and Quality (US); 2012. [Internet] (Comparative Effectiveness Review No. 36). Available at: http://www.effectivehealthcare.ahrq.gov/ehc/products/169/834/urinary-incontinence-treatment-report-130909.pdf. Accessed November 2014. [PubMed] [Google Scholar]
- 5.Abrams P, Andersson KE, Birder L, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29:213–40. doi: 10.1002/nau.20870. [DOI] [PubMed] [Google Scholar]
- 6.National Institute for Health and Clinical Excellence. Urinary Incontinence: The Management of Urinary Incontinence in Women. London: RCOG Press; 2013. [Internet]; Available at: http://www.nice.org.uk/guidance/cg171. Accessed November 2014. [Google Scholar]
- 7.Dowd T, Kolcaba K, Steiner R. Using cognitive strategies to enhance bladder control and comfort. Holist Nurs Pract. 2000;14:91–103. doi: 10.1097/00004650-200001000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Garley A, Unwin J. A case series to pilot cognitive behaviour therapy for women with urinary incontinence. Br J Health Psychol. 2006;11:373–86. doi: 10.1348/135910705X53876. [DOI] [PubMed] [Google Scholar]
- 9.Shaw C, Das Gupta R, Williams KS, Assassa RP, McGrother C. A survey of help-seeking and treatment provision in women with stress urinary incontinence. BJU Int. 2006;97:752–7. doi: 10.1111/j.1464-410X.2006.06071.x. [DOI] [PubMed] [Google Scholar]
- 10.St John W, James H, McKenzie S. “Oh, that's a bit of a nuisance”: community-dwelling clients perspectives of urinary continence health service provision. J Wound Ostomy Continence Nurs. 2002;29:312–9. doi: 10.1067/mjw.2002.129074. [DOI] [PubMed] [Google Scholar]
- 11.Teunissen D, van den Bosch W, van Weel C, Lagro-Janssen T. Urinary incontinence in the elderly: attitudes and experiences of general practitioners. A focus group study. Scand J Prim Health Care. 2006;24:56–61. doi: 10.1080/02813430500417920. [DOI] [PubMed] [Google Scholar]
- 12.Statistics Sweden. 2014. Use of computers and the Internet by private persons 2013. [Internet] Stockholm, Sweden, Available at: http://www.scb.se/sv_/Hitta-statistik/Publiceringskalender/Visa-detaljerad-information/?publobjid=19861+. Accessed August 2014.
- 13.Office for National Statistics. Part of Internet Access – Households and Individuals, 2013 Release. [Internet] Newport, South Wales, UK; Available at: http://www.ons.gov.uk/ons/rel/rdit2/internet-access-80-households-and-individuals/2013/stb-ia-2013.html. Accessed August 2014.
- 14.Zickuhr K. Who's not online and why. [Internet]: Pew Internet & American Life Project; Washington (DC): September 25, 2013; Available at: http://pewinternet.org/Reports/2013/Non-internet-users.aspx. Accessed November 2014.
- 15.Fox S, Duggan M. Health Online 2013 [Internet]. Pew Internet & American Life Project. Washington (DC): January 15, 2013. Available at: http://www.pewinternet.org/2013/01/15/health-online-2013/. Accessed November 2014.
- 16.Umefjord G, Petersson G, Hamberg K. Reasons for consulting a doctor on the internet: web survey of users of an ask the doctor service. J Med Internet Res. 2003;5:e26. doi: 10.2196/jmir.5.4.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andersson G. The Internet and CBT: A Clinical Guide. Boca Raton: CRC Press; 2014. [Google Scholar]
- 18.Beattie A, Shaw A, Kaur S, Kessler D. Primary-care patients' expectations and experiences of online cognitive behavioural therapy for depression: a qualitative study. Health Expect. 2009;12:45–59. doi: 10.1111/j.1369-7625.2008.00531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanchez-Ortiz VC, House J, Munro C, et al. “A computer isn't gonna judge you”: a qualitative study of users' views of an internet-based cognitive behavioural guided self-care treatment package for bulimia nervosa and related disorders. Eat Weight Disord. 2011;16:e93–101. doi: 10.1007/BF03325314. [DOI] [PubMed] [Google Scholar]
- 20.Ferwerda M, van Beugen S, van Burik A, et al. What patients think about E-health: patients' perspective on internet-based cognitive behavioral treatment for patients with rheumatoid arthritis and psoriasis. Clin Rheumatol. 2013;32:869–73. doi: 10.1007/s10067-013-2175-9. [DOI] [PubMed] [Google Scholar]
- 21.Sjostrom M, Umefjord G, Stenlund H, Carlbring P, Andersson G, Samuelsson E. Internet-based treatment of stress urinary incontinence: a randomised controlled study with focus on pelvic floor muscle training. BJU Int. 2013;112:362–72. doi: 10.1111/j.1464-410X.2012.11713.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bjork AB, Sjostrom M, Johansson EE, Samuelsson E, Umefjord G. Women's experiences of internet-based or postal treatment for stress urinary incontinence. Qual Health Res. 2014;24:484–93. doi: 10.1177/1049732314524486. [DOI] [PubMed] [Google Scholar]
- 23.Sjostrom M, Umefjord G, Lindholm L, Samuelsson E. Cost-effectiveness of an internet-based treatment program for stress urinary incontinence. Neurourol Urodyn. 2015;34:244–50. doi: 10.1002/nau.22540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dumoulin C, Hay-Smith EJ, Mac Habee-Seguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2014;5:CD005654. doi: 10.1002/14651858.CD005654.pub3. [DOI] [PubMed] [Google Scholar]
- 25.Bo K, Hilde G. Does it work in the long term? A systematic review on pelvic floor muscle training for female stress urinary incontinence. Neurourol Urodyn. 2013;32:215–23. doi: 10.1002/nau.22292. [DOI] [PubMed] [Google Scholar]
- 26.Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23:322–30. doi: 10.1002/nau.20041. [DOI] [PubMed] [Google Scholar]
- 27.Klovning A, Avery K, Sandvik H, Hunskaar S. Comparison of two questionnaires for assessing the severity of urinary incontinence: the ICIQ-UI SF versus the incontinence severity index. Neurourol Urodyn. 2009;28:411–5. doi: 10.1002/nau.20674. [DOI] [PubMed] [Google Scholar]
- 28.Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynaecol. 1997;104:1374–9. doi: 10.1111/j.1471-0528.1997.tb11006.x. [DOI] [PubMed] [Google Scholar]
- 29.Coyne K, Kelleher C. Patient reported outcomes: the ICIQ and the state of the art. Neurourol Urodyn. 2010;29:645–51. doi: 10.1002/nau.20911. [DOI] [PubMed] [Google Scholar]
- 30.Sjostrom M, Stenlund H, Johansson S, Umefjord G, Samuelsson E. Stress urinary incontinence and quality of life: a reliability study of a condition-specific instrument in paper and web-based versions. Neurourol Urodyn. 2012;31:1242–6. doi: 10.1002/nau.22240. [DOI] [PubMed] [Google Scholar]
- 31.Yalcin I, Bump RC. Validation of two global impression questionnaires for incontinence. Am J Obstet Gynecol. 2003;189:98–101. doi: 10.1067/mob.2003.379. [DOI] [PubMed] [Google Scholar]
- 32.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 33.Higgins JPT, Deeks JJ, Altman DG, Green S. 2011. Chapter 16: special topics in statistics. In Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0, [updated March 2011]. The Cochrane Collaboration,. Available at: http://www.cochrane-handbook.org/. Accessed November 2014.
- 34.Jahanlu D, Hunskaar S. Type and severity of new-onset urinary incontinence in middle-aged women: the Hordaland women's cohort. Neurourol Urodyn. 2011;30:87–92. doi: 10.1002/nau.20966. [DOI] [PubMed] [Google Scholar]
- 35.Waetjen LE, Liao S, Johnson WO, et al. Factors associated with prevalent and incident urinary incontinence in a cohort of midlife women: a longitudinal analysis of data: study of women's health across the nation. Am J Epidemiol. 2007;165:309–18. doi: 10.1093/aje/kwk018. [DOI] [PubMed] [Google Scholar]
- 36.Kuh D, Cardozo L, Hardy R. Urinary incontinence in middle aged women: childhood enuresis and other lifetime risk factors in a British prospective cohort. J Epidemiol Community Health. 1999;53:453–8. doi: 10.1136/jech.53.8.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Henderson JW, Wang S, Egger MJ, Masters M, Nygaard I. Can women correctly contract their pelvic floor muscles without formal instruction? Female Pelvic Med Reconstr Surg. 2013;19:8–12. doi: 10.1097/SPV.0b013e31827ab9d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Welch LC, Botelho EM, Joseph JJ, Tennstedt SL. A qualitative inquiry of patient-reported outcomes: the case of lower urinary tract symptoms. Nurs Res. 2012;61:283–90. doi: 10.1097/NNR.0b013e318251d8f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Borello-France D, Burgio KL, Goode PS, et al. Adherence to behavioral interventions for stress incontinence: rates, barriers, and predictors. Phys Ther. 2013;93:757–73. doi: 10.2522/ptj.20120072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hay-Smith EJ, Herderschee R, Dumoulin C, Herbison GP. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev. 2011:CD009508. doi: 10.1002/14651858.CD009508. [DOI] [PubMed] [Google Scholar]
- 41.Hirakawa T, Suzuki S, Kato K, Gotoh M, Yoshikawa Y. Randomized controlled trial of pelvic floor muscle training with or without biofeedback for urinary incontinence. Int Urogynecol J. 2013;24:1347–54. doi: 10.1007/s00192-012-2012-8. [DOI] [PubMed] [Google Scholar]
- 42.Nystrom E, Sjostrom M, Stenlund H, Samuelsson E. ICIQ symptom and quality of life instruments measure clinically relevant improvements in women with stress urinary incontinence. Neurourol Urodyn. 2014 doi: 10.1002/nau.22657. doi: 10.1002/nau.22657. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]


