CONSPECTUS
Carbon nanotubes (CNTs) are carbon atoms arranged in a crystalline graphene lattice with a tubular morphology. CNTs exhibit high tensile strength, possess unique electrical properties, are durable, and can be functionalized. These properties allow applications as structural materials, in electronics, as heating elements, in batteries, in the production of stain-resistant fabric, for bone grafting and dental implants, and for targeted drug delivery. Carbon nanofibers (CNFs) are strong, flexible fibers that are currently used to produce composite materials.
Agitation can lead to aerosolized CNTs and CNFs, and peak airborne particulate concentrations are associated with workplace activities such as weighing, transferring, mixing, blending, or sonication. Most airborne CNTs or CNFs found in workplaces are loose agglomerates of micrometer diameter. However, due to their low density, they linger in workplace air for a considerable time, and a large fraction of these structures are respirable.
In rat and mouse models, pulmonary exposure to single-walled carbon nanotubes (SWCNTs), multi-walled carbon nanotubes (MWCNTs), or CNFs causes the following pulmonary reactions: acute pulmonary inflammation and injury, rapid and persistent formation of granulomatous lesions at deposition sites of large CNT agglomerates, and rapid and progressive alveolar interstitial fibrosis at deposition sites of more dispersed CNT or CNF structures.
Pulmonary exposure to SWCNTs can induce oxidant stress in aortic tissue and increases plaque formation in an atherosclerotic mouse model. Pulmonary exposure to MWCNTs depresses the ability of coronary arterioles to respond to dilators. These cardiovascular effects may result from neurogenic signals from sensory irritant receptors in the lung. Pulmonary exposure to MWCNTs also upregulates mRNA for inflammatory mediators in selected brain regions, and pulmonary exposure to SWCNTs upregulates the baroreceptor reflex. In addition, pulmonary exposure to MWCNTs may induce levels of inflammatory mediators in the blood, which may affect the cardiovascular system.
Intraperitoneal instillation of MWCNTs in mice has been associated with abdominal mesothelioma. MWCNTs deposited in the distal alveoli can migrate to the intrapleural space, and MWCNTs injected in the intrapleural space can cause lesions at the parietal pleura. However, further studies are required to determine whether pulmonary exposure to MWCNTs can induce pleural lesions or mesothelioma.
In light of the anticipated growth in the production and use of CNTs and CNFs, worker exposure is possible. Because pulmonary exposure to CNTs and CNFs causes inflammatory and fibrotic reactions in the rodent lung, adverse health effects in workers represent a concern. NIOSH has conducted a risk assessment using available animal exposure–response data and is developing a recommended exposure limit for CNTs and CNFs.
Evidence indicates that engineering controls and personal protective equipment can significantly decrease workplace exposure to CNTs and CNFs. Considering the available data on health risks, it appears prudent to develop prevention strategies to minimize workplace exposure. These strategies would include engineering controls (enclosure, exhaust ventilation), worker training, administrative controls, implementation of good handling practices, and the use of personal protective equipment (such as respirators) when necessary. NIOSH has published a document containing recommendations for the safe handling of nanomaterials.
Graphical abstract
I. Introduction
Methods have been perfected to arrange carbon atoms in a crystalline graphene lattice with a tubular morphology. A single-walled carbon nanotube (SWCNT) is composed of a single cylindrical sheet of graphene and has a diameter of 0.5–2 nm. Multiwalled carbon nanotubes (MWCNTs) consist of multiple tubes within a tube and have diameters of 10–150 μm, depending on the number of concentric tubes forming the structure. Carbon nanotubes (CNTs) can range in length from 0.5 to 30 μm.1 Carbon nanofibers (CNFs) are composed of graphene layers arranged at an angle to the fiber axis. CNFs range from 70 to 200 nm in diameter and 10–100 μm in length.2 CNTs exhibit high tensile strength, possess unique electrical properties, are resistant to acid or high temperature, and can be easily functionalized. Therefore, application as structural materials, in electronics, as heating elements, in batteries, in production of conductive and stain-resistant fabric, for bone grafting and dental implants, and in targeted drug delivery are being developed. CNFs are strong, flexible fibers that are currently being used to produce strong but lightweight composite materials.
II. Workplace Exposures to CNTs or CNFs
Occupational exposure to CNTs and CNFs can occur during laboratory research, product development (synthesis), downstream use, and waste recycling/disposal. Maynard et al.3 were the first to report aerosolization of CNTs in a laboratory setting upon agitation of SWCNTs during removal of material from the synthesis furnace, transfer of the SWCNTs, or cleaning. Respirable dust concentrations ranged from 0.7 to 53 μg/m3, with most airborne particles being agglomerates. Aerosolization of MWCNTs during weighing, transfer, and sonication was also reported in a laboratory setting.4 Han et al.5 reported that total particle concentration in a MWCNT production laboratory could be as high as 430 μg/m3 during weighing, blending, and spraying. MWCNTs (agglomerates and more dispersed structures) represented only a fraction of this total dust. Lee et al.6 reported particle generation in seven MWCNT facilities. Peak total particle concentrations were as high as 320 μg/m3 during oven opening, catalyst preparation, gel spraying, and transfer or sonication of MWCNTs. Only a fraction of these particles were MWCNTs, with most being metal nano-particles. Sawing, drilling, and sanding of composite materials containing CNTs can release both fine and nanoscale particles with peak concentrations as high as 8380 μg/m3 being reported during the dry cutting of composites in the absence of exposure controls.7,8 Methner et al.9 measured peak airborne particle concentrations 2–64 times higher than office area levels during weighing and mixing of CNFs. These airborne particles included loosely agglomerated CNFs. Significant particulate generation was also reported during bagging (peak 500 μg/m3) and transfer (peak 1100 μg/m3) of dried CNFs. These aerosolized particles contained fiber agglomerates.10 A more complete review of workplace exposure to CNTs and of CNFs is available elsewhere.11
III. Animal Model Responses to CNTs
A. Pulmonary Responses
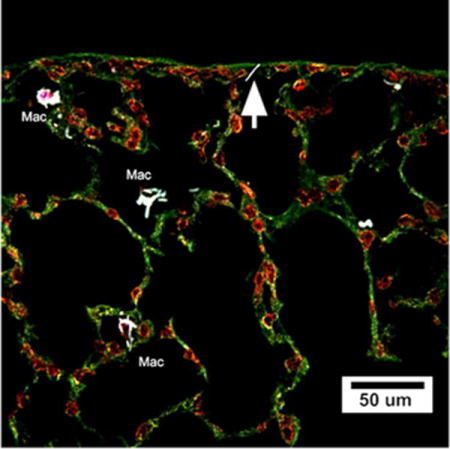
The literature base documenting pulmonary responses (dose and time dependence) following intratracheal instillation (IT), pharyngeal aspiration, or inhalation of SWCNTs or MWCNTs in rat or mouse models has grown significantly over the past few years. These studies have been reviewed in greater detail elsewhere, and commonalities in responses have been identified.1,11,12 For example, pharyngeal aspiration of purified SWCNTs (10–40 μg/mouse) resulted in (1) a dose-dependent and rapid but transient inflammatory and injury response, (2) a rapid and persistent granulomatous response, and (3) alveolar interstitial fibrosis of rapid onset and progressive nature.13 Short-term (4 days) inhalation exposure to SWCNTs induced a similar spectrum of pulmonary reactions.14 On an equal mass lung burden basis, the fibrotic response following inhalation was 4-fold greater than after aspiration of SWCNTs.13,14 This was because SWCNTs were more dispersed in the dry aerosol (inhalation exposure) than in an aqueous suspension (pharyngeal aspiration). Aspiration of a well-dispersed suspension of SWCNTs resulted in a less severe granulomatous response and a 4-fold greater interstitial fibrotic response than a poorly dispersed SWCNT suspension.15 Furthermore, aspiration of gold-labeled SWCNTs demonstrated that agglomerates induced granulomatous lesions in the terminal bronchioles and proximal alveoli, while more dispersed SWCNT structures deposited in the distal lung, rapidly entered the alveolar interstitium, and caused progressive fibrosis.15 Aspiration of purified MWCNTs in mice caused a similar spectrum of pulmonary responses as SWCNTs, that is, rapid but transient damage and inflammation, granulomatous lesions, and interstitial fibrosis.16 Short-term inhalation (4 days) of MWCNTs induced pulmonary responses in mice similar to those reported after aspiration.17 Morphometric analysis indicates that a greater fraction of alveolar MWCNTs are phagocytized than SWCNTs, while a greater fraction of SWCNTs enter the alveolar interstitium.18 This results in a greater fibrotic reaction to an equal lung burden of SWCNTs compared with MWCNTs.18 Recently, Murray et al.19 reported that aspiration of CNFs in a mouse model also resulted in transient inflammation and damage and persistent fibrosis. The fibrotic potency (on a mass lung burden basis) was SWCNTs > CNFs = asbestos. These inflammatory and fibrotic pulmonary responses to CNTs have also been associated with measurable alterations of pulmonary function, that is, an increase in expiratory time with SWCNTs and decreased compliance with increased resistance with aspiration of MWCNTs.13,20 Evidence also indicates that SWCNT exposure also decreases the ability of the lung to resist infection.21
Recent studies indicate that functionalization of MWCNTs with −COOH groups significantly decreases the inflammatory and fibrotic response after aspiration in a mouse model.22,23 These studies open the possibility that adverse bioactivity of CNTs may be mitigated through “safety by design”.
B. Pleural Responses
Takayi et al.24 reported induction of mesothelioma after intraperitoneal injection of high doses (3 μg/mouse) of MWCNTs. Recently, Kanno et al.25 reported similar responses to abdominal exposure to a much lower MWCNT dose (50 μg/mouse). Murphy et al.26 reported persistent (24 weeks post) inflammation and fibrosis of the parietal pleural surface after intrapleural injection of long (>15 μm) but not short (<4 μm) MWCNTs (5 μg/mouse). Pulmonary exposure of mice to MWCNTs has been shown to result in the migration of CNTs to subpleural tissue and from the subpleural tissue to the intrapleural space with time postexposure.27,28 Mercer et al.28 have reported 12000 MWCNT penetrations into the intrapleural space 56 days following aspiration of 80 μg of MWCNTs/mouse. Therefore, studies are needed to determine whether pulmonary exposure to MWCNTs would result in mesotheliomia. Such studies are in progress at NIOSH.
C. Cardiovascular Responses
Inhalation of MWCNTs in rats results in significant impairment of the ability of coronary arterioles to respond to dilatory stimuli 24 h post-exposure.29 Similar microvascular dysfunction has been reported after inhalation of nano-titanium dioxide and has been associated with stimulation of sensory neurons from the lung and enhanced sympathetic input at the systemic arterioles.30,31 Aspiration of MWCNTs has also been reported to increase baroreflex activity in rats.32,33 In addition, Erdely et al.34 reported transient elevation of blood inflammatory mediators after aspiration of MWCNTs, which may mediate this systemic microvascular response. Multiple exposures (aspiration of 20 μg/mouse, every 2 weeks for 2 months) to SWCNTs also resulted in elevation of inflammation and oxidant stress markers in aortic tissue and augmentation of aortic plaques in atherosclerotic sensitive ApoE −/− mice.35
D. Central Nervous System Responses
As described above, cardiovascular responses to pulmonary exposure to MWCNTs have been attributed to a neurogenic mechanism involving sensor nerve input from the lung to brain and resultant sympathetic input to the cardiovascular tissue. Studies by Sriram et al.36 demonstrate significant induction of inflammatory mRNA and blood/brain damage markers in selected regions of the brain 24 h after aspiration of MWCNTs. The direct relationship between these central nervous system changes and cardiovascular effects following pulmonary exposure to CNTs requires further investigation.
IV. In Vitro Responses to CNTs
The effects of CNTs on various cell types was extensively reviewed previously.1 Many in vitro CNT studies are characterized by three issues: (1) the use of doses per cell that are much higher than those achieved in animal models of pulmonary exposure, (2) CNT agglomeration, and (3) adsorption of assay indicator dyes by CNTs. Therefore, care must be taken in analyzing in vitro results. SWCNTs have been reported to be toxic to cells; however, much of this cytotoxicity is due to oxidants generated by contaminating metal catalysts on the CNTs.37,38 Purified CNTs have been reported to generate low levels of reactive species in a cellular system yet remain bioactive in vivo.16,39 Low doses of SWCNTs, representative of CNT lung burdens and alveolar epithelial cell surface area achieved after aspiration of 40 μg/mouse, exhibit low cytotoxicity. Rather, low dose SWCNT exposure of lung fibroblasts increases proliferation rate and collagen production.40 Therefore, the rapid onset of an interstitial fibrotic response to pulmonary CNT exposure may be a direct scaffolding and matrix effect of CNTs resulting in fibroblast activation. This scaffolding and matrix effect of CNTs is dependent on dispersed fibrous structures rather than CNT agglomerates.41,42
Purified SWCNTs do not generate radicals yet cause a measurable level of genotoxicity to fibroblasts in the comet and micronucleus assay.39 However, CNFs generate significant radicals and are more genotoxic than SWCNTs.43 Sargent et al.44 reported that SWCNTs disrupt centrosomes in dividing lung epithelial cells resulting in multipolar mitosis and aneuploidy. MWCNTs have also been shown to interact with centrosomes preventing normal migration to mitotic poles and resulting in monopolar mitosis.45
V. Physicochemical Properties and Bioactivity
There is great interest in elucidation of relationships between given physical or chemical properties of CNTs and their bioactivity. Knowledge of such relationships would impact prediction of relative hazard in the absence of biological data and allow “safety by design”.
A. Contaminating Metals
As discussed above, contaminating catalytic metals appear to play an important role in radical generation by CNTs and their in vitro cytotoxicity. However, metal contaminants do not appear to drive pulmonary responses to in vivo CNT exposure. Lam et al.46 reported rapid and persistent granulomas in mice after intratracheal instillation of SWCNTs. However, the degree of this granulomatous reaction was not dependent on metal contamination when responses of raw (25% metal catalyst by weight) and purified (2% iron by weight) SWCNTs were compared. Similarly, the inflammatory response to aspiration of raw (17.7% iron) vs purified (0.23% iron) SWCNTs was not significantly different.13,14
B. Agglomerates versus Dispersed Structures
As discussed above, well-dispersed SWCNTs and MWCNTs are more fibrogenic in vitro than agglomerated CNTs, causing greater proliferation and collagen formation with fibroblasts and greater TGF-β1 production by lung epithelial cells.40–42 Aspiration of a well-dispersed SWCNT preparation also caused more transient inflammation and persistent interstitial fibrosis than poorly dispersed SWCNTs.15 In contrast, poorly dispersed SWCNTs caused a greater granulomatous response. Similarly, Li et al.47 reported a greater degree of inflammation following intratracheal instillation of agglomerated MWCNTs and greater alveolar wall thickening after inhalation of more dispersed MWCNTs. A strong granulomatous response with low interstitial fibrosis was also reported after inhalation of a highly agglomerated MWCNT preparation.48
C. Functionalization of CNTs
Functionalization of MWCNTs with COOH groups decreased in vitro MWCNT stimulation of TGF-β1 production by bronchial epithelial cells and decreased stimulation of IL-1β in THP-1 cells.22 COOH functionalization of MWCNTs mitigated pulmonary inflammation, lung damage, and IL-1β production after aspiration.23 In addition, COOH functionalization significantly decreased the fibrogenic response in the alveolar septa.22,23 The depression of bioactivity achieved by COOH functionalized of MWCNTs was only partial and did not result in a nonfibrogenic CNTs.
D. Relative potency of SWCNTs, MWCNTs, and CNFs
Murray et al.19 compared the potencies on an equal mass basis of SWCNTs, CNFs, and asbestos to induce pulmonary inflammation, lung injury, and fibrosis from 1 to 28 days after pharyngeal aspiration in mice. At 1 day postexposure, potency for acute inflammation and damage was SWCNTs > CNFs > asbestos, while at 7 days postexposure the potency sequence was SWCNTs > CNFs = asbestos. At 7 days post-exposure, SWCNTs > CNFs = asbestos in the induction of the fibrogenic factor, TGF-β. At 28 day postexposure, the potency sequence for induction of alveolar wall thickening and lung collagen was SWCNTs > CNFs = asbestos. Mercer et al.15,18 conducted quantitative microscopy of mouse lungs after aspiration of SWCNTs and MWCNTs. Only 10% of deposited SWCNTs were found in alveolar macrophages, while 90% rapidly crossed the alveolar epithelium and entered the alveolar wall interstitium. In contrast, 70% of MWCNTs deposited in the alveolar region were found in macrophages, while only 8% entered the alveolar septa. As a result, on an equal deposited mass basis, SWCNTs were more fibrogenic than MWCNTs. This greater potency of SWCNTs remained even when corrected for the difference in alveolar wall burden.
Kisin et al.39 reported that CNFs induced a more potent genotoxic response than SWCNTs in vitro. In contrast, the potency of SWCNTs and MWCNTs to transform lung epithelial cells in a long-term culture system was similar.49
E. The Effect of Fiber Length on CNT Potency
Muller et al.50 reported that grinding a MWCNT sample decreased fiber length from 6 to 0.7 μm. At 60 day post-exposure, 81% of unground MWCNTs were retained in the lung compared with 30% of the ground sample. The authors concluded that this would affect long-term pulmonary responses.
Takagi et al.24 reported that intra-abdominal injection of MWCNTs (28% >5 μm in length) caused mesothelioma. In contrast, Muller et al.51 reported no mesothelioma over a 2 year observation period following intraperitoneal injection of short MWCNTs (0.7 μm in length). Poland et al.52 demonstrated that intraperitoneal injection of long MWCNTs but not short MWCNTs were inflammatory and induced granulomatous lesions on the diaphragm 2 week postexposure. This length-dependent effect was confirmed with MWCNT-induced lesions on the inner lining of the chest wall 28 days after intrapleural exposure to MWCNTs.26 The authors suggested that two length-dependent mechanisms are involved: (1) frustrated phagocytosis of long fibers by macrophages and (2) failure of long fibers to be cleared from the intrapleural space via stomata in the parietal pleura.53
VI. Relationships between Bolus Pulmonary Exposure (IT or Aspiration) and Inhalation
It has been argued that bolus particle exposure (intratracheal instillation or pharyngeal aspiration) would result in a greater pulmonary reaction than inhalation exposure due to nonuniform deposition creating hot spots and the greater time-dependent lung burden.
Shvedova et al.14 compared pulmonary responses of mice to pharyngeal aspiration vs a short-term inhalation (4 days) of SWCNTs. In this investigation, the SWCNT dry aerosol preparation for inhalation was more dispersed than the CNT suspension used for aspiration exposure. Results indicate that inhalation exposure resulted in 4-fold greater inflammation and fibrosis than aspiration of the same mass lung burden. Li et al.47 reported similar findings, that is, inhalation of a more dispersed MWCNT preparation caused greater interstitial fibrosis and cell proliferation than aspiration of a less dispersed preparation. Mercer et al.15 found that when efforts were made to improve the dispersion of aspirated SWCNT suspensions, fibrotic potency was similar between aspiration and a 4 day inhalation exposure. Porter and colleagues compared the inflammatory response to aspiration of a well-dispersed MWCNT suspension and to short-term inhalation (4 days) of a dry MWCNT aerosol. They found that the levels of pulmonary inflammation and damage were not significantly different between these two modes of pulmonary exposure.16,17 In addition, NIOSH11 conducted a risk analysis to compare benchmark human exposure concentration for MWCNTs using data from a mouse aspiration16 vs a 3 month inhalation54 study. Benchmark exposure concentrations for MWCNT-induced pulmonary granulomatous inflammation or fibrosis were 0.61 μg/m3 vs 0.51 μg/m3 for the aspiration vs inhalation study, respectively. Therefore, evidence indicates that when CNT samples of similar dispersion are used, aspiration studies can predict a pulmonary response that is consistent with short-term inhalation studies when dosed at an equal mass lung burden.
VII. Relationship between in Vivo and in Vitro Responses to CNTs
Many in vitro studies with CNTs have employed tissue culture doses in the range of 10–100 μg/mL and have reported cytotoxicity.1 However, on a per cell basis, such doses are orders of magnitude higher than those achieved in pulmonary exposure studies with rats or mice and may not be relevant to workplace exposure. NIOSH researchers have employed micrograms of CNTs per alveolar epithelial cell surface area as a dose metric to compare lung burdens in rodents to projected burdens in workers. Stone et al.55 reported alveolar epithelial surface areas determined by morphometric analysis as 102 m2, 0.4 m2, and 0.05 m2 per human, rat, and mouse lungs, respectively. NIOSH researchers have employed similar doses (CNT mass/surface area of cells) for in vitro studies. When such low exposure doses are employed, stimulation of lung fibroblast proliferation and collagen production rather than cytotoxicity were found, which mimic the fibrogenic effects of CNTs observed after pulmonary exposure. Such low doses also reveal CNT-induced cell transformation and aneuploidy instead of cell death.44,49
VIII. Effectiveness of Controls
The discussion above indicates that CNTs and CNFs can be aerosolized as respirable particles during synthesis and processing activities in the workplace. Since pulmonary exposure to CNTs and CNFs in rodent models consistently results in acute pulmonary inflammation and persistent fibrosis, worker exposure is considered a respiratory health risk. Therefore, it would be prudent to minimize inhalation exposure to workers. Han et al.5 have reported that the use of engineering controls can effectively decrease airborne MWCNT concentrations during laboratory synthesis and processing. Similarly, Methner56 reported that local exhaust ventilation decreased airborne nanoparticle concentrations during reactor clean out by 88%. In addition, Regasamy et al.57 have shown that filtering facepiece respirators equipped with a 95 or 100 series filter will effectively capture more than 95% of nanoparticles in the size range of 4–30 nm. NIOSH has published a document containing recommendations for engineering controls, administrative controls, worker training, use of personal protective equipment, and implementation of safe handling practices for nanomaterials, which would significantly decrease worker exposure.58
IX. Interim Recommendation for Implementation of Prevention Strategies
Use of animal model data and risk assessment indicates that at current workplace CNT and CNF respirable mass concentrations, a risk to workers for adverse respiratory effects may exist over a working lifetime.11 As noted above, engineering controls (containment, exhaust ventilation) and personal protective equipment (e.g., respirators) appear effective for significantly reducing airborne CNT and CNF concentrations. Therefore, it appears prudent, based on available data, to implement prevention strategies. Therefore, a combination of engineering controls, worker training, administrative controls and good handling practices, and personal protective equipment have been recommended to protect worker health.11
X. Conclusions
Available information indicates that CNTs and CNFs can be aerosolized in the workplace. Animal model studies report that pulmonary exposure to CNTs or CNFs can cause persistent granulomatous lesions and alveolar interstitial fibrosis. In addition, pulmonary exposure to CNTs has been shown to cause cardiovascular effects. In light of these potential health effects, control of exposure is a prudent course of action.
To support more definitive risk assessment and development of exposure standards, several knowledge gaps must be addressed. First, more workplace exposure data are required, and more precise measurement methods are needed. Such exposure data would guide long-term animal studies to determine the time course and dose response for possible development of fibrosis, lung cancer, or mesothelioma. Elucidation of mechanisms of action could identify biomarkers, which would be useful in worker surveillance. Lastly, elucidation of relationships between physicochemical properties and bioactivity would assist in progress toward “safety by design”.
Biographies
Vincent Castranova was born on March 18, 1949, in Trenton, New Jersey. He is Chief of the Pathology and Physiology Research Branch at the National Institute for Occupational Safety and Health (NIOSH). He holds the grade of a CDC Distinguished Consultant. He received the Shepard Lifetime Scientific Achievement Award from CDC in 2008 and the Stokinger Outstanding Achievement in Industrial Toxicology Award from ACGIH in 2009. He is also an adjunct professor at West Virginia University (WVU) and the University of Pittsburgh. Dr. Castranova received a B.S. in biology from Mount Saint Mary’s College in 1970 and a Ph.D. in physiology and biophysics in 1974 from WVU. He was a NIH fellow and research faculty member at Yale University before accepting a research position at NIOSH and an adjunct faculty position at WVU in 1977. He has served at these institutions since that time. Dr. Castranova’s research interests are pulmonary toxicology and occupational lung disease. He has been coordinator of the NIOSH Nanotoxicology Program since 2005. He has coedited of four books and has coauthored over 470 manuscripts and book chapters.
Ralph Zumwalde is a senior research scientist with the Education and Information Division (EID) at the National Institute for Occupational Safety and Health (NIOSH). He is currently assigned to the NIOSH Nanotechnology Research Center (NTRC) to assist in the evaluation of the potential health risks to engineered nanomaterials and development of risk management practices for preventing occupational exposure to nanoparticles. Mr. Zumwalde has also held several management positions at NIOSH including the Chief of the Document Development Branch, EID. Mr. Zumwalde was born on April 15, 1947, in Cincinnati, OH. He attended the University of Cincinnati where he received a B.S. in biology/horticulture/physical sciences in 1975 and a M.S. in industrial hygiene/environmental health in 1981. He has over 40 years in conducting occupational safety and health research at NIOSH with specific research interests in the characterization of occupational exposures to mineral and synthetic fibers and engineered nanoparticles. Mr. Zumwalde has coauthored over 100 manuscripts and NIOSH publications, which have received several NIOSH Alice Hamilton and Bullard-Sherwood Awards for excellence in the field of occupational safety and health research.
Paul A. Schulte, Ph.D., was born on August 14, 1946, in Pittsburgh, PA. He received a B.A. from the University of Toronto and a M.S. and Ph.D. from the University of Cincinnati. He is the Director of the Education and Information Division and Manager of the Nanotechnology Research Center and the Prevention through Design programs, National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention. Dr. Schulte has extensive experience in conducting research and developing guidance on occupational cancer, nanomaterials, risk communication, and genetics. He is the coeditor of the textbook entitled “Molecular Epidemiology: Principles and Practices.” He has served as guest editor of the Journal of Occupational Medicine and the American Journal of Industrial Medicine and was on the initial editorial board of Cancer Epidemiology, Biomarkers and Prevention. He currently is on the editorial board of the Scandinavian Journal of Work and Environmental Health and the International Advisory Board of the Annals of Occupational Hygiene.
Footnotes
The authors declare no competing financial interest.
The findings and conclusions in this article are those of the author and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
References
- 1.Shvedova AA, Kisin ER, Porter D, Schulte P, Kagan VE, Fadeel B, Castranova V. Mechanisms of toxicity and medical application of carbon nanotubes: Two faces of Janus? J Pharmacol Ther. 2009;121:192–204. doi: 10.1016/j.pharmthera.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 2.De Jong K, Geus J. Carbon nanofibers: Catalytic synthesis and applications. Catal Rev Sci Eng. 2000;42:481–510. [Google Scholar]
- 3.Maynard AD, Baron PA, Foley M, Shvedova AA, Kisin ER, Castranova V. Exposure to carbon nanotube material during the handling of unrefined single walled carbon nanotube material. J Toxicol Environ Health, Part A. 2004;67:87–107. doi: 10.1080/15287390490253688. [DOI] [PubMed] [Google Scholar]
- 4.Johnson DR, Methner MM, Kennedy AJ, Steevens JA. Potential for occupational exposure to engineered carbon-based nanomaterial in environmental laboratory studies. Environ Health Perspect. 2010;118:44–54. doi: 10.1289/ehp.0901076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Han JR, Lee EJ, Lee JH, So KP, Lee YH, Bae GN, Lee S, Ji JH, Cho MH, Yu IJ. Monitoring multiwalled carbon nanotube research facility. Inhalation Toxicol. 2008;20:741–749. doi: 10.1080/08958370801942238. [DOI] [PubMed] [Google Scholar]
- 6.Lee JR, Lee S-B, Bae GN, Jean KS, Yoon JU, Ji JH, Sun JH, Lee BG, Lee JH, Yang JS, Kim HY, Kang CS, Yu IJ. Exposure assessment of carbon nanotube manufacturing workplaces. Inhalation Toxicol. 2010;22:369–381. doi: 10.3109/08958370903367359. [DOI] [PubMed] [Google Scholar]
- 7.Bello D, Wardle BL, Yamamoto N, de Villora RG, Garcia EJ, Hart AJ, Ahn K, Ellenbecker MJ, Hallock M. Exposure to nanoscale particles and fibers during machining of hybrid advanced composites containing carbon nanotubes. J Nanopart Res. 2009;11:231–249. [Google Scholar]
- 8.Bello D, Wardle BL, Zhang J, Yamamoto N, Santeufernio C, Hallock M, Virji MA. Characterization of exposures to nanoscale particles and fibers during solid core drilling of hybrid carbon nanotubes advanced composites. Int J Occup Environ Health. 2010;16:434–450. doi: 10.1179/107735210799159996. [DOI] [PubMed] [Google Scholar]
- 9.Methner MM, Birch ME, Evans DE, Ku BK, Crouch KG, Hoover MD. Identification and characterization of potential sources of worker exposure to carbon nanofibers during polymer composite laboratory operations. J Occup Environ Hyg. 2007;4:D125–D120. doi: 10.1080/15459620701683871. [DOI] [PubMed] [Google Scholar]
- 10.Birch ME, Ku B-K, Evans DE, Ruda-Eberenz T. Exposure and emissions monitoring during carbon and iron-soot aerosols. Ann Occup Hyg. 2011;55:1016–1036. doi: 10.1093/annhyg/mer073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NIOSH. Current Intelligence Bulletin: Occupational Exposure to Carbon Nanotubes. 2010 www.cdc.gov/niosh/docket/review/docket161A/
- 12.Castranova V, Mercer RR. Responses to Pulmonary Exposure to Carbon Nanotubes. In: Donaldson K, Duffin R, Bonner J, Poland C, editors. The Nanotoxicology of Carbon Nanotubes. Cambridge University Press; Cambridge: 2012. pp. 134–149. Chapter 8. [Google Scholar]
- 13.Shvedova AA, Kisin ER, Mercer R, Murray AR, Johnson VJ, Potapovich AI, Tyurina YY, Gorelik O, Arepulli S, Schwegler-Berry D, Hubbs AF, Antonini J, Evans DE, Ku B-K, Ramsey D, Maynard A, Kagan VE, Castranova V, Baron P. Unusual inflammatory and fibrogenic pulmonary responses to single walled carbon nanotubes in mice. Am J Physiol: Lung Cell Mol Physiol. 2005;289:L698–L 708. doi: 10.1152/ajplung.00084.2005. [DOI] [PubMed] [Google Scholar]
- 14.Shvedova AA, Kisin E, Murray AR, Johnson VJ, Gorelik O, Arepali S, Hubbs AF, Mercer RR, Keohavong P, Sussman N, Jin J, Stone S, Chen BT, Deye G, Maynard A, Castranova V, Baron PA, Kagan VE. Inhalation versus aspiration of single walled carbon nanotubes in C57BL/6 mice: inflammation, fibrosis, oxidative stress and mutagenesis. Am J Physiol: Lung Cell Mol Physiol. 2008;295:L552–565. doi: 10.1152/ajplung.90287.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mercer RR, Scabilloni J, Wang L, Kisin E, Murray AR, Schwegler-Berry D, Shvedova AA, Castranova V. Alteration of deposition pattern and pulmonary response as a result of improved dispersion of aspirated single walled carbon nanotubes in a mouse model. Am J Physiol: Lung Cell Mol Physiol. 2008;294:L87–L97. doi: 10.1152/ajplung.00186.2007. [DOI] [PubMed] [Google Scholar]
- 16.Porter DW, Hubbs A, Mercer R, Wu N, Wolfarth MG, Sriram K, Leonard S, Battelli L, Schwegler-Berry D, Friend S, Andrew M, Chen BT, Tsuruoka S, Endo M, Castranova V. Mouse pulmonary dose- and time course-responses induced by exposure to multi-walled carbon nanotubes. Toxicology. 2010;269:136–147. doi: 10.1016/j.tox.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Porter D, Wolfarth MG, Chen BT, McKinney W, Hubbs AF, Battelli LA, Andrew M, Frazier DG, Castranova V. Pulmonary toxicity of inhaled multi-walled carbon nanotubes. The Toxicologist. 2009;108(A2193) [Google Scholar]
- 18.Mercer RR, Hubbs AF, Scabilloni JF, Wang L, Battelli LA, Friend S, Castranova V, Porter DW. Pulmonary fibrotic response to aspiration of multi-walled carbon nanotubes. Part Fibre Toxicol. 2011;8:21. doi: 10.1186/1743-8977-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murray AR, Kisin ER, Tkach AV, Yanamala N, Mercer R, Young S-H, Fadeel B, Kagan VE, Shvedova AA. Factoring in agglomeration of carbon nanotubes and nanofibers for better prediction of their toxicity versus asbestos. Part Fibre Toxicol. 2012;9(10) doi: 10.1186/1743-8977-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang X, Katwa P, Podilla R, Chen P, Kep C, Rao AM, Walters DM, Wingard CJ, Brown JM. Multi-walled carbon nanotube instillation impairs pulmonary function in C57BL/6 mice. Part Fibre Toxicol. 2011;8:24. doi: 10.1186/1743-8977-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shvedova AA, Fabisiak JP, Kisin ER, Murray AR, Roberts JR, Antonini JA, Kommineni C, Reynolds J, Barchowsky A, Castranova V, Kagan V. Sequential exposure to carbon nanotubes and bacteria enhances pulmonary inflammation and infectivity. Am J Respir Cell Mol Biol. 2008;38:579–590. doi: 10.1165/rcmb.2007-0255OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang X, Xia T, Ntim SA, Ji Z, Lim S, Meng H, Chung C-M, George S, Zhang H, Wang M, Li N, Yang Y, Castranova V, Mitra S, Bonner JC, Nel AE. The dispersal state of multi-walled carbon nanotubes elicits pro-fibrogenic cellular responses that correlate with fibrogenesis biomarkers and fibrosis in the murine lung. ACS Nano. 2012;5:9772–9787. doi: 10.1021/nn2033055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sager TM, Wolfarth M, Porter D, Castranova V, Wu N, Holian A. Effect of surface modification on the bioavailability and inflammatory potential of multi-walled carbon nanotubes. The Toxicologist. 2011;120(A1178) [Google Scholar]
- 24.Takagi A, Hirose A, Nishimura T, Fukumori W, Ogata A, Ohashi N. Induction of mesothelioma in p53 ( mouse by intraperitoneal application of multi-walled carbon nanotube. J Toxicol Sci. 2008;33:105–116. doi: 10.2131/jts.33.105. [DOI] [PubMed] [Google Scholar]
- 25.Kanno J, Takagi A, Nishimura T, Fukumori W, Ogata A, Ohashi N. Mesothelioma induction by micrometer-sized multi-walled carbon nanotube intraperitoneally inject to p53 heterozygous mice. The Toxicologist. 2010;114(A1397) [Google Scholar]
- 26.Murphy FA, Poland CA, Duffin R, AI-Jamal KT, Ali-Boucetta H, Nunes A, Byrna F, Prina-Mello A, Volkov Y, Li S, Mathor SJ, Bianco A, Prato M, MacNea A, Wallace WA, Kosturelos K, Donaldson K. Length-dependent retention of carbon nanotubes in the pleural space of mice initiates sustained inflammation and progressive fibrosis on the parietal pleura. Am J Pathol. 2011;78:2587–2600. doi: 10.1016/j.ajpath.2011.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ryman-Rasmussen JP, Cesta MF, Brody AR, Shipley-Phillips JK, Everitt JI, Tewksbury EW, Moss OR, Wang BA, Dodd DE, Anderson ME, Bonner JC. Inhaled carbon nanotubes reach the subpleural tissue in mice. Nat Nanotechnol. 2009;4:747–751. doi: 10.1038/nnano.2009.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mercer RR, Hubbs AF, Scabilloni JF, Wang L, Battelli L, Schwegler-Berry D, Castranova V, Porter DW. Distribution and persistence of pleural penetrations by multi-walled carbon nanotubes. Part Fibre Toxicol. 2010;7:28. doi: 10.1186/1743-8977-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stapleton PA, Minarchick V, Cumpston A, McKinney W, Chen BT, Frazer D, Castranova V, Nurkiewicz TR. Time-course of improved coronary arteriolar endothelium-dependent dilation after multi-walled carbon nanotube inhalation. The Toxicologist. 2011;120(A194) [Google Scholar]
- 30.Kan H, Wu ZX, Young SH, Chen BT, Cumpston JL, Chen F, Castranova V. Pulmonary exposure of rats to ultrafine titanium dioxide enhances cardiac protein phosphorylation and substance P synthesis in nodose ganglia. Nanotoxicology. 2012;6:736–745. doi: 10.3109/17435390.2011.611915. [DOI] [PubMed] [Google Scholar]
- 31.Knuckles TL, Yi J, Frazer DG, Leonard HD, Chen BT, Castranova V, Nurkiewicz TR. Nanoparticle inhalation alters systemic arteriolar vasoreactivity through sympathetic and cyclooxygenase-mediated pathways. Nanotoxicology. 2012;6:724–735. doi: 10.3109/17435390.2011.606926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Legramante JM, Valentini F, Magrini A, Palleschi G, Iavicoli L, Pallante M, Moscone D, Galante A, Bergamashi E, Bergamashi A, Pietroiusti A. Cardiac autonomic regulation after lung exposure to carbon nanotubes. Hum Exp Toxicol. 2009;28:369–375. doi: 10.1177/0960327109105150. [DOI] [PubMed] [Google Scholar]
- 33.Coppeta L, Legramante J, Galante A, Bergamashi AJ, Bergamashi E, Margrini A, Pietroiusti A. Interaction between carbon nanotubes and cardiovascular autonomic nervous system regulation: Proposal of an animal model and preliminary findings. G Ital Med Lav Ergon. 2007;29:465–467. [PubMed] [Google Scholar]
- 34.Erdely A, Hulderman T, Salmen R, Liston A, Zeidler-Erdely PC, Schwegler-Berry D, Castranova V, Koyama S, Kim Y-A, Endo M, Simeonova PP. Cross-talk between lung and systemic circulation during carbon nanotube respiratory exposure. Potential biomarkers. Nano Lett. 2009;9:36–43. doi: 10.1021/nl801828z. [DOI] [PubMed] [Google Scholar]
- 35.Li Z, Hulderman T, Salmen R, Chapman R, Leonard SS, Shvedova A, Luster MI, Simeonova PP. Cardiovascular effects of pulmonary exposure to single-wall carbon nanotubes. Environ Health Perspect. 2007;115:377–382. doi: 10.1289/ehp.9688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sriram K, Porter DW, Jefferson AM, Lin GX, Wolfarth MG, Chen BT, McKinney W, Frazer DG, Castranova V. Neuro inflammation and blood-brain barrier changes following exposure to engineered nanomaterials. The Toxicologist. 2009;108(A2197) [Google Scholar]
- 37.Shvedova AA, Kisin ER, Murray AR, Schwegler-Berry D, Gandelsman VZ, Maynard A, Baron P, Castranova V. Exposure to carbon nanotube material: Assessment of the biological effects of nanotube materials using human keratinocytes. J Toxicol Environ Health, Part A. 2003;66:1901–1926. doi: 10.1080/713853956. [DOI] [PubMed] [Google Scholar]
- 38.Kagan VE, Tyurina YY, Tyurin VA, Konduru NV, Potapovich AI, Osipov AN, Kisin ER, Schwegler-Berry D, Mercer R, Castranova V, Shvedova AA. Direct and indirect effects of single walled carbon nanotubes on RAW 264.7 macrophages: Role of iron. Toxicol Lett. 2006;165:88–100. doi: 10.1016/j.toxlet.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 39.Kisin E, Murray AR, Sargent L, Lowry D, Chirila M, Siegrist KJ, Schwegler-Berry D, Leonard S, Castranova V, Fadeel B, Kagan VE, Shvedova AA. Genotoxicity of carbon nanofibers: are they potentially more or less dangerous than carbon nanotubes of asbestos? Toxicol Appl Pharmacol. 2011;252:1–10. doi: 10.1016/j.taap.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang L, Mercer RR, Rojanasakul Y, Qiu A, Lu Y, Scabilloni JF, Wu N, Castranova V. Direct fibrogenic effects of dispersed single-walled carbon nanotubes on human lung fibroblasts. J Toxicol Environ Health, Part A. 2010;73:410–422. doi: 10.1080/15287390903486550. [DOI] [PubMed] [Google Scholar]
- 41.Wang L, Castranova V, Mishra A, Chen B, Mercer RR, Schwegler-Berry D, Rojanasakul Y. Dispersion of single-walled carbon nanotubes by a natural lung surfactant for pulmonary in vitro and in vivo toxicity studies. Part Fibre Toxicol. 2010;7:31. doi: 10.1186/1743-8977-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang X, Xia T, Ntim SA, Ji Z, George S, Meng H, Zhang H, Castranova V, Mitra S, Nel AE. Quantitative techniques for assessing and controlling the dispersion state and biological effects of multi-walled carbon nanotubes in mammalian tissue culture cells. ACS Nano. 2010;4:7241–7252. doi: 10.1021/nn102112b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kisin ER, Murray AR, Keane MJ, Shi X-C, Gorelik O, Arepalli S, Castranova V, Wallace WE, Kagan VE, Shvedova AA. Single-walled carbon nanotubes: Geno- and cytotoxic effects in lung fibroblast V79 cells. J Toxicol Environ Health, Part A. 2007;70:2071–2079. doi: 10.1080/15287390701601251. [DOI] [PubMed] [Google Scholar]
- 44.Sargent L, Reynolds SH, Castranova V. Potential pulmonary effects of engineered carbon nanotubes: in vitro genotoxic effects. Nanotoxicology. 2010;4:396–408. doi: 10.3109/17435390.2010.500444. [DOI] [PubMed] [Google Scholar]
- 45.Sargent LM, Reynolds SH, Hubbs AF, Benkovic SA, Lowry DT, Kashon ML, Siegrist KJ, Mastovich J, Sturgeon JL, Bunker KL, Dinu CZ. Understanding carbon nanotube genotoxicity. The Toxicologist. 2011;120(A58) [Google Scholar]
- 46.Lam G-W, James JT, McCluskey R, Hunter RL. Pulmonary toxicity of single-wall carbon nanotubes in mice 7 and 90 days after intratracheal instillation. Toxicol Sci. 2004;77:125–134. doi: 10.1093/toxsci/kfg243. [DOI] [PubMed] [Google Scholar]
- 47.Li J-G, Li W-X, Xu J-Y, Cai X-Q, Liu R-L, Li Y-J, Zhao Q-F, Li Q-N. Comparative study of pathological lesions induced by multiwalled carbon nanotubes in lungs of mice by intratracheal instillation and inhalation. Environ Toxicol. 2007;22:415–421. doi: 10.1002/tox.20270. [DOI] [PubMed] [Google Scholar]
- 48.Pauluhn J. Subchronic 13-week inhalation exposure of rats to multiwalled carbon nanotubes: Toxic effects are determined by density of agglomerate structures, not fibrillar structure. Toxicol Sci. 2010;113:226–242. doi: 10.1093/toxsci/kfp247. [DOI] [PubMed] [Google Scholar]
- 49.Stueckle TA, Mishra A, Derk R, Rojanasakul Y, Castranova Y, Wang L. In vitro assessment of potential tumorgenicity of chronic SWCNT and MWCNT exposure to lung epithelium. The Toxicologist. 2011;120(A1182) [Google Scholar]
- 50.Muller J, Huaux F, Moreau N, Mission P, Heilier J-F, Delos M, Arras M, Fonseca A, Nagy JB, Lison D. Respiratory toxicity of multi-wall carbon nanotubes. Toxicol Appl Pharmacol. 2005;207:221–231. doi: 10.1016/j.taap.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 51.Muller J, Delos M, Panin N, Rabolli V, Huaux F, Lison D. Absence of carcinogenic response to multi wall carbon nanotubes in a 2-year bioassay in the peritoneal cavity of the rat. Toxicol Sci. 2009;110:442–447. doi: 10.1093/toxsci/kfp100. [DOI] [PubMed] [Google Scholar]
- 52.Poland CA, Duffin R, Kinloch I, Maynard A, Wallace WA, Seaton A, Stone Y, Brown S, MacNee W, Donaldson K. Carbon nanotubes introduced into the abdominal cavity of mice show asbestos-like pathogenicity in a pilot study. Nat Nanotechnol. 2008;3:423–428. doi: 10.1038/nnano.2008.111. [DOI] [PubMed] [Google Scholar]
- 53.Donaldson K, Murphy FA, Duffin R, Poland CA. Asbestos, carbon nanotubes and the pleural mesotheliomia review of the hypothesis regarding the role of long fibre retention in the parietal pleura, inflammation and mesothelioma. Part Fibre Toxicol. 2010;7:5. doi: 10.1186/1743-8977-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ma-Hock L, Trenmann S, Strauss V, Brill S, Luizi F, Mertler M, Wiench K, Gamer AO, van Ravenzwaay B, Landsiedel R. Inhalation toxicity of multiwall carbon nanotubes in rats exposed for 3 months. Toxicol Sci. 2009;112:468–481. doi: 10.1093/toxsci/kfp146. [DOI] [PubMed] [Google Scholar]
- 55.Stone K, Mercer RR, Gehr P, Stockstill B, Crapo JD. Allometric relationships of cell numbers and size in the mammalian lung. Am J Respir Cell Mol Biol. 1992;6:235–243. doi: 10.1165/ajrcmb/6.2.235. [DOI] [PubMed] [Google Scholar]
- 56.Methner MM. Effectiveness of local exhaust ventilation (LEV) in controlling engineered nanomaterial emissions during rector clean out operations. J Occup Environ Hyg. 2008;5:D63–D69. doi: 10.1080/15459620802059393. [DOI] [PubMed] [Google Scholar]
- 57.Regasamy S, King W, Eimer B, Shaffer R. Filtration performance of NIOSH-approved N95 and PI00 filtering facemasks respirators against 4 30 nm-size nanoparticles. J Occup Environ Hyg. 2008;5:556–564. doi: 10.1080/15459620802275387. [DOI] [PubMed] [Google Scholar]
- 58.NIOSH. (DHHS (NIOSH) Publication No. 2009-15).Approaches to Safe Nanotechnology: Managing the Health and Safety Concerns Associated with Engineered Nanomaterials. 2009 [Google Scholar]


