Abstract
High-sensitivity C-reactive protein (hs-CRP) has been associated with coronary heart disease (CHD) in numerous but not all observational studies, and whether low levels of low-density lipoprotein cholesterol (LDL-C) alter this association is unknown. In the Multi-Ethnic Study of Atherosclerosis (2000–2012), we prospectively assessed the association of hs-CRP concentrations with incident CHD in participants who did not receive lipid-lowering therapy, as well as in those with LDL-C concentrations less than 130 mg/dL (n = 3,106) and those with LDL-C concentrations of 130 mg/dL or greater (n = 1,716) at baseline (2000–2002). Cox proportional hazard analyses were used to assess the associations after adjustment for socioeconomic status, traditional risk factors, body mass index, diabetes, aspirin use, kidney function, and coronary artery calcium score. Loge hs-CRP was associated with incident CHD in participants with LDL-C concentrations of 130 mg/dL or higher (hazard ratio (HR) = 1.29, 95% confidence interval (CI): 1.05, 1.60) but not in those with LDL-C concentrations less than 130 mg/dL (HR = 0.88, 95% CI: 0.74, 1.05; P for interaction = 0.003). As a whole, loge hs-CRP was not associated with incident CHD in participants who had not received lipid-lowering therapy at baseline (HR = 1.05, 95% CI: 0.92, 1.20) and who had mean LDL-C concentrations less than 130 mg/dL. These findings suggest that LDL-C concentrations might be a moderator of the contribution of hs-CRP to CHD.
Keywords: coronary heart disease, high-sensitivity C-reactive protein, low-density lipoprotein cholesterol
C-reactive protein (CRP), which is a member of the pentraxin protein family, is mainly synthesized in the liver after stimulation by proinflammatory cytokines (1). Additionally, CRP is also produced by extra-hepatic cells, such as aortic endothelial cells, under oxidative stress or inflammatory stimulation (2–4). CRP is present in atherosclerotic lesions and has been found to interact with some modified low-density lipoproteins, possibly leading to progression of atherosclerotic plaque (4, 5).
In the past 15 years, higher concentrations of high-sensitivity CRP (hs-CRP) within the normal range have been associated with a higher risk of future coronary heart disease (CHD) in multiple observational studies and clinical trials (6–9). Measurement of hs-CRP has become a part of prevention guidelines in the United States, particularly for persons at intermediate risk of cardiovascular disease (CVD) (10).
Notably, the association between hs-CRP concentration and CHD risk was mainly observed in community-based cohort studies before 2000, when the general population had higher mean concentrations of low-density lipoprotein cholesterol (LDL-C) (7, 8). In contrast, hs-CRP concentrations were not associated with incident CHD in the Multi-Ethnic Study of Atherosclerosis (MESA) (11, 12). Whether the low baseline LDL-C concentrations in MESA participants altered the association with hs-CRP is not known. Therefore, we aimed to study in greater depth the association between hs-CRP concentrations and CHD events in MESA participants with lower LDL-C concentrations and in those with higher LDL-C concentrations.
METHODS
Study population and data collection
The study design for MESA has previously been published elsewhere (13). In brief, MESA is a longitudinal cohort study designed to investigate the prevalence, correlates, and progression of subclinical CVD in individuals without clinical CVD at baseline. The cohort includes 6,814 women and men recruited from 6 US communities (Baltimore, Maryland; Chicago, Illinois; Forsyth County, North Carolina; Los Angeles County, California; northern Manhattan, New York; and St. Paul, Minneapolis) who were 45–84 years of age at the baseline examination (July 2000 to August 2002). Thirty-eight percent of the participants were white, 28% were black, 22% were Hispanic, and 12% were Chinese. The study was approved by the institutional review boards of each study site, and written informed consent was obtained from all participants.
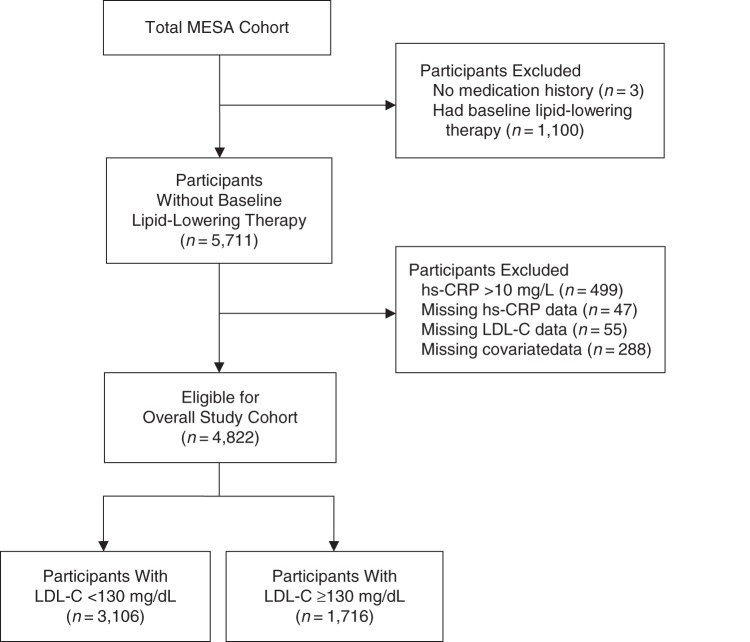
Of the 6,814 participants, 3 had missing medication histories and 1,100 had received lipid-lowering therapy at baseline. We excluded those with a hs-CRP concentration higher than 10 mg/L to avoid confounders such as occult infectious disease and those with missing data about hs-CRP and LDL-C concentrations and relevant covariates, leaving a sample of 4,822 participants for analysis. Of these, 3,106 had an LDL-C concentration lower than 130 mg/dL and 1,716 had an LDL-C concentration of 130 mg/dL or higher. Figure 1 shows the criteria used to select study participants.
Figure 1.
Flow chart of the selection criteria for the eligible overall study cohort, the subcohort with low-density lipoprotein cholesterol (LDL-C) concentrations less than 130 mg/dL, and the subcohort with LDL-C concentrations of 130 mg/dL or higher for the analysis of the association between high-sensitivity C-reactive protein (hs-CRP) concentrations and incident coronary heart disease, Multi-Ethnic Study of Atherosclerosis (MESA), 2000–2012.
Demographic, medical history, anthropometric, and laboratory data for the present analysis were obtained from the first examination of MESA. Body mass index was calculated as weight in kilograms divided by height in meters squared. Smoking status was defined as current, former, or never smoker from self-report. Resting blood pressure was measured 3 times at 1-minute intervals while participants were seated, and the mean of the second and third measurements was recorded. Diabetes mellitus was defined as having a fasting glucose level of 126 mg/dL or higher or using hypoglycemic medications. Glomerular filtration rate was estimated according to the Chronic Kidney Disease Epidemiology Collaboration equation (14). Total cholesterol and high-density lipoprotein cholesterol levels were measured from blood samples obtained after a 12-hour fast. LDL-C concentration was estimated using the Friedewald equation in participants with a triglyceride concentration less than 400 mg/dL (15).
We assessed medication use at clinic visits by reviewing participants' medication containers. The Laboratory for Clinical Biochemistry Research (University of Vermont, Burlington, Vermont) measured serum hs-CRP concentrations using the BN II nephelometer (Dade Behring Inc., Deerfield, Illinois) and urinary albumin/creatinine ratio (mg of albumin/g of creatinine) on a single spot morning collection using nephelometry and the rate-Jaffe reaction. Analytical intra-assay coefficients of variation of hs-CRP ranged from 2.1% to 5.7%, with a detection concentration of 0.18 mg/L. Microalbuminuria and macroalbuminuria were defined as having urinary albumin/creatinine ratios of 30–299 mg/g and ≥300 mg/g, respectively. Family history of CHD was defined as self-report of any immediate family member (parents or siblings) with fatal or nonfatal myocardial infarction at any age.
Coronary artery calcium was measured using either electron beam computed tomography or multidetector computed tomography. Participants were scanned twice at a single examination, and images were interpreted at a centralized reading center (Harbor–UCLA Medical Center, Los Angeles, California). The coronary artery calcium scores from the 2 scans were averaged (16).
Ascertainment of incident CHD
Incident CHD events were defined as myocardial infarction, CHD death, resuscitated cardiac arrest, or definite or probable angina if followed by coronary revascularization. CHD events were adjudicated by a committee that included cardiologists, physician epidemiologists, and neurologists. A description of the adjudication process has been reported previously (17).
Statistical analysis
In the primary analysis, we examined the association of hs-CRP concentrations with incident CHD in participants with LDL-C concentrations less than 130 mg/dL and in those with LDL-C concentrations of 130 mg/dL or higher. We also investigated the association of hs-CRP concentrations with incident CHD in participants who had received lipid-lowering therapy at baseline.
In the analysis, we used the follow-up time from the first MESA examination with censoring at the first occurrence of incident CHD, loss to follow-up, or end of follow-up (December 31, 2012). hs-CRP concentrations were treated as continuous variables by loge transformation. Cox proportional hazard regression analyses were used to assess the multivariable associations of loge hs-CRP with incident CHD in the groups, with adjustment for potential confounders.
In model 1, we adjusted for age, sex, race/ethnicity, study site, educational level, and total family income. In model 2, we additionally adjusted for body mass index, diabetes, smoking status, family history of CHD, systolic blood pressure, total cholesterol level, high-density lipoprotein cholesterol level, aspirin use, and antihypertensive therapy. In model 3, we adjusted for the variables in models 1 and 2 and estimated glomerular filtration rate, microalbuminuria, macroalbuminuria, and coronary artery calcium score (log2 transformation). Finally, in model 4, we adjusted for the variables in all previous models and the interim use of lipid-lowering medications. Formal testing for interaction for the hs-CRP association between the subcohorts defined by LDL-C concentration were performed by pooling the 2 subcohorts and introducing into the statistical model an indicator variable for 1 subcohort together with the product of that indicator variable with loge hs-CRP. A 2-tailed P value <0.017 was considered significant. All statistical analyses were performed using SAS, version 9.4 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
Table 1 shows the baseline characteristics of the study participants. As shown in Table 2, over an average of 10.3 years of follow-up, there were 299 (6.2%) CHD events in the overall cohort, 168 (5.4%) in the subcohort with LDL-C concentrations less than 130 mg/dL, and 131 (7.6%) in the subcohort with LDL-C concentrations of 130 mg/dL or higher. In the subcohort with LDL-C concentrations of 130 mg/dL or higher, loge hs-CRP was associated with incident CHD independent of traditional risk factors, body mass index, diabetes, renal function, coronary artery calcium score, and interim use of lipid-lowering medication in the multivariable analyses.
Table 1.
Baseline Characteristics of Participants Who Did Not Receive Lipid-Lowering Therapy Stratified by Low-Density Lipoprotein and High-Sensitivity C-Reactive Protein Concentrations, Multi-Ethnic Study of Atherosclerosis, 2000–2012
| Characteristic | Overall (n = 4,822) |
LDL-C <130 mg/dL (n = 3,106) |
LDL-C ≥130 mg/dL (n = 1,716) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| hs-CRP ≥3 mg/L (n = 1,461) |
hs-CRP <3 mg/L (n = 3,361) |
hs-CRP ≥3 mg/L (n = 892) |
hs-CRP <3 mg/L (n = 2,214) |
hs-CRP ≥3 mg/L (n = 569) |
hs-CRP <3 mg/L (n = 1,147) |
|||||||
| Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | |
| Age, years | 61.5 (9.8) | 61.2 (10.5) | 61.6 (10.0) | 61.3 (10.7) | 61.1 (9.5) | 61.0 (10.1) | ||||||
| Sex, female | 62.3 | 45.9 | 60.2 | 45.9 | 65.6 | 45.8 | ||||||
| Race | ||||||||||||
| White | 36.6 | 39.2 | 36.4 | 38.0 | 36.9 | 41.6 | ||||||
| Black | 30.3 | 22.9 | 31.1 | 23.5 | 29.0 | 21.7 | ||||||
| Hispanic | 28.5 | 20.5 | 28.4 | 19.5 | 28.8 | 22.3 | ||||||
| Chinese | 4.6 | 17.4 | 4.2 | 19.0 | 5.3 | 14.4 | ||||||
| Cigarette smoking | ||||||||||||
| Current | 17.5 | 11.3 | 17.0 | 12.3 | 18.3 | 9.2 | ||||||
| Former | 35.9 | 35.4 | 38.1 | 35.3 | 32.5 | 35.6 | ||||||
| Never | 46.5 | 53.3 | 44.8 | 52.4 | 49.2 | 55.2 | ||||||
| Body mass indexa | 30.2 (5.6) | 26.7 (4.5) | 30.2 (5.7) | 26.5 (4.6) | 30.1 (5.4) | 26.9 (4.3) | ||||||
| Diabetes | 12.2 | 8.8 | 13.7 | 9.4 | 9.8 | 7.7 | ||||||
| SBP, mm Hg | 128.8 (21.5) | 123.3 (20.9) | 128.5 (21.8) | 123.3 (21.1) | 129.4 (21.2) | 124.1 (20.5) | ||||||
| Antihypertensive therapy | 37.7 | 27.9 | 40.5 | 29.5 | 33.4 | 24.9 | ||||||
| Aspirin therapy | 20.4 | 20.7 | 20.6 | 21.6 | 20.0 | 19.0 | ||||||
| Total cholesterol, mg/dL | 198.1 (36.4) | 195.3 (34.1) | 177.5 (25.4) | 178.3 (24.0) | 230.5 (25.9) | 228.1 (25.6) | ||||||
| LDL-C level, mg/dL | 121.5 (33.1) | 119.4 (30.8) | 101.0 (20.6) | 102.4 (19.2) | 153.6 (21.4) | 152.3 (20.8) | ||||||
| HDL-C level, mg/dL | 50.0 (14.5) | 51.8 (15.1) | 50.6 (15.8) | 52.3 (16.2) | 49.1 (12.1) | 50.7 (12.5) | ||||||
| Triglycerides, mg/dL | 132.9 (64.7) | 120.4 (64.6) | 129.1 (66.3) | 117.6 (66.9) | 138.9 (61.9) | 125.8 (59.5) | ||||||
| eGFR, mL/min/1.73 m2 | 81.3 (17.8) | 82.2 (18.6) | 81.2 (18.2) | 83.1 (17.2) | 81.5 (17.2) | 80.5 (21.0) | ||||||
| Albuminuria | 10.8 | 7.6 | 11.2 | 7.8 | 10.2 | 7.1 | ||||||
| CAC score, Agatstonb | 0 (0, 64.5) | 0 (0, 65.4) | 0 (0, 62.5) | 0 (0, 61.5) | 1.9 (0, 68.0) | 0 (0, 73.6) | ||||||
| Interleukin-6 level, pg/mL | 1.9 (1.2) | 1.2 (0.9) | 2.0 (1.3) | 1.2 (0.9) | 1.8 (1.1) | 1.1 (0.9) | ||||||
| hs-CRP level, mg/L | 5.2 (1.9) | 1.2 (0.8) | 5.2 (1.9) | 1.2 (0.8) | 5.3 (1.9) | 1.3 (0.8) | ||||||
Abbreviations: CAC, coronary artery calcium; CHD, coronary heart disease; eGFR, estimated glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; hs-CRP, high-sensitivity C-reactive protein; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure.
a Weight (kg)/height (m)2.
b CAC score was presented as median (25th percentile, 75th percentile).
Table 2.
Association of Loge High-Sensitivity C-Reactive Protein With Incident Coronary Heart Disease, Multi-Ethnic Study of Atherosclerosis, 2000–2012
| Study Group | CHD Events |
Model 1a |
Model 2b |
Model 3c |
Model 4d |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | HR | 95% CI | P for Interactione | HR | 95% CI | P for Interactione | HR | 95% CI | P for Interactione | HR | 95% CI | P for Interactione | |
| Overall | 299 | 6.2 | 1.13 | 1.00, 1.28 | 1.04 | 0.91, 1.19 | 1.05 | 0.92, 1.20 | 1.06 | 0.93, 1.21 | ||||
| LDL-C <130 mg/dL | 168 | 5.4 | 0.94 | 0.79, 1.10 | 0.002 | 0.88 | 0.74, 1.05 | 0.007 | 0.88 | 0.74, 1.05 | 0.003 | 0.89 | 0.75, 1.06 | 0.003 |
| LDL-C ≥130 mg/dL | 131 | 7.6 | 1.43 | 1.17, 1.75 | 1.25 | 1.02, 1.55 | 1.29 | 1.05, 1.60 | 1.29 | 1.05, 1.60 | ||||
Abbreviations: CHD, coronary heart disease; CI, confidence interval; HR, hazard ratio; LDL-C, low-density lipoprotein cholesterol.
a Adjusted for age, sex, race, site, total family income, and educational level.
b Adjusted for the variables in model 1 and body mass index, diabetes, smoking status, family history of coronary heart disease, systolic blood pressure, total cholesterol, high-density lipoprotein cholesterol level, aspirin use, and antihypertensive therapy.
c Adjusted for the variables in models 1 and 2 and estimated glomerular filtration rate, macroalbuminuria, microalbuminuria, and coronary artery calcium score.
d Adjusted for the variables in models 1–3 and interim use of lipid-lowering medication.
e P value for interaction was examined for the difference in the associations with high-sensitivity C-reactive protein between the LDL-C <130 mg/dL subcohort and the LDL-C ≥130 mg/dL subcohort.
In the subcohort with LDL-C concentrations less than 130 mg/dL, all associations were nonsignificant. In addition, the associations with risk of incident CHD differed significantly between the subcohorts in the multivariable analyses (P value for interaction from model 1 to model 4: 0.002, 0.007, 0.003, and 0.003, respectively). In the overall cohort in which mean LDL-C concentration was less than 130 mg/dL, loge hs-CRP was not associated with incident CHD in the multivariable analyses.
As shown in Appendix Table 1, loge hs-CRP was associated with incident CHD in the model 1 analysis (HR = 1.34, 95% confidence interval (CI): 1.08, 1.66). Associations were slightly attenuated in the model 2 and model 3 analyses (in both, HR = 1.22, 95% CI: 0.96, 1.55). As compared with having a hs-CRP concentration less than 3 mg/L, having a concentration of 3 mg/L or higher was associated with higher risk of incident CHD in model 1 (HR = 2.21, 95% CI: 1.46, 3.36), model 2 (HR = 2.00, 95% CI: 1.28, 3.12), and model 3 (HR = 1.93, 95% CI: 1.24, 3.02).
DISCUSSION
In MESA participants who were had not received lipid-lowering therapy at baseline, higher hs-CRP concentrations were associated with a higher risk of CHD only if their LDL-C concentration was at least 130 mg/dL. Higher hs-CRP concentrations while receiving treatment were associated with higher risk of incident CHD in those who had received lipid-lowering therapy at baseline, 94% of whom used statins.
On the basis of current evidence, some modified low-density lipoproteins (LDLs), such as oxidized LDLs, which are generally correlated with plasma concentrations of LDL-C, could initiate vascular inflammation by stimulating endothelial cells to secrete CRP (5, 18). CRP in turn increases the release of lectin-like oxidized LDL receptor 1 from macrophages, which can increase uptake of these modified LDLs (19). As a mediator of vascular inflammation, CRP might induce complement activation via lectin-like oxidized LDL receptor 1 (20). Activation of lectin-like oxidized LDL receptor 1 contributes to endothelial exudation, vasomotor dysfunction, and proatherogenic actions of CRP (21, 22). In clinical observations, hs-CRP concentrations were correlated with oxidized LDL concentrations in the general population (23) and had additive value to predict myocardial infarction and death in patients with acute coronary syndrome (24).
Previous studies of the associations of hs-CRP concentrations with vascular events have been done in populations with low LDL-C concentrations (8, 9, 25). In the Women's Health Study (8), they did not control for lipid-lowering therapy at baseline in their subgroup with a lower LDL-C concentration. In the Air Force/Texas Coronary Atherosclerosis Prevention Study (9), the subgroup with lower LDL-C concentrations included participants with LDL-C concentrations less than the median of 150 mg/dL, many of whom had LDL-C concentrations of 130 mg/dL or higher. In the Justification for Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) (25), even though hs-CRP concentrations were associated with CVD events in the subcohort comprising men who received the placebo, the association was not seen in the subcohort of women who received the placebo.
The strengths of the present study include the large array of covariates for which we adjusted and the carefully conducted adjudications for incident CHD. In contrast, our study had a relatively short follow-up period. In addition, residual confounding might have contributed to the inconsistent results for the hs-CRP association in our subgroup analyses despite the large array of covariates in the multivariable adjustment models.
In conclusion, these data suggest that LDL-C concentrations might be a moderator of the contribution of hs-CRP to vascular events. Whether the hs-CRP association in individuals with higher LDL-C concentrations is mediated by modified LDL or some factors that are correlated closely with LDL-C concentrations needs further investigation in the general population, including people who are and people who are not using lipid-lowering therapy.
ACKNOWLEDGMENTS
Author affiliations: Department of Preventive Medicine, Feinberg School of Medicine, Northwestern University, Chicago, Illinois (Gen-Min Lin, Kiang Liu, Laura A. Colangelo, Philip Greenland); Department of Medicine, Hualien Armed Forces General Hospital, Hualien, Taiwan (Gen-Min Lin); Division of Cardiology, Department of Medicine, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan (Gen-Min Lin); Department of Internal Medicine, College of Medicine, University of Vermont, Burlington, Vermont (Susan G. Lakoski); Department of Pathology and Laboratory Medicine, College of Medicine, University of Vermont, Burlington, Vermont (Russell P. Tracy); and Department of Biochemistry, College of Medicine, University of Vermont, Burlington, Vermont (Russell P. Tracy).
This research was supported by National Institutes of Health contracts N01-HC-95159 through N01-HC-95169. G.-M.L. was supported by a scholarship grant from the Ministry of Defense, Taiwan.
Conflict of interest: none declared.
APPENDIX
Appendix Table 1.
Association of High-Sensitivity C-Reactive Protein Concentrations With Incident Coronary Heart Disease in Participants Receiving Lipid-Lowering Therapy (n = 963), Multi-Ethnic Study of Atherosclerosis, 2000–2012
| hs-CRP Variable | Model 1a |
Model 2b |
Model 3c |
|||
|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Loge hs-CRP | 1.34 | 1.08, 1.66 | 1.22 | 0.96, 1.55 | 1.22 | 0.96, 1.55 |
| hs-CRP ≥3 mg/L vs. hs-CRP <3 mg/L | 2.21 | 1.46, 3.36 | 2.00 | 1.28, 3.12 | 1.93 | 1.24, 3.02 |
Abbreviations: CI, confidence interval; HR, hazard ratio; hs-CRP, high-sensitivity C-reactive protein.
a Adjusted for age, sex, race, site, total family income, and educational level.
b Adjusted for the variables in model 1 and body mass index, diabetes, smoking status, family history of coronary heart disease, systolic blood pressure, total cholesterol, high-density lipoprotein cholesterol level, aspirin use, and antihypertensive therapy.
c Adjusted for the variables in models 1 and 2 and estimated glomerular filtration rate, macroalbuminuria, microalbuminuria, and coronary artery calcium score.
REFERENCES
- 1.Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;11112:1805–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Calabro P, Chang DW, Willerson JT et al. . Release of C-reactive protein in response to inflammatory cytokines by human adipocytes: linking obesity to vascular inflammation. J Am Coll Cardiol. 2005;466:1112–1113. [DOI] [PubMed] [Google Scholar]
- 3.Calabró P, Willerson JT, Yeh ET. Inflammatory cytokines stimulated C-reactive protein production by human coronary artery smooth muscle cells. Circulation. 2003;10816:1930–1932. [DOI] [PubMed] [Google Scholar]
- 4.Tsai MH, Chang CL, Yu YS et al. . Chemical analysis of C-reactive protein synthesized by human aortic endothelial cells under oxidative stress. Anal Chem. 2012;8421:9646–9654. [DOI] [PubMed] [Google Scholar]
- 5.Hulthe J, Wikstrand J, Fagerberg B. Relationship between C-reactive protein and intima-media thickness in the carotid and femoral arteries and to antibodies against oxidized low-density lipoprotein in healthy men: the Atherosclerosis and Insulin Resistance (AIR) study. Clin Sci (Lond). 2001;1004:371–378. [DOI] [PubMed] [Google Scholar]
- 6.Koenig W, Khuseyinova N, Baumert J et al. . Increased concentrations of C-reactive protein and IL-6 but not IL-18 are independently associated with incident coronary events in middle-aged men and women: results from the MONICA/KORA Augsburg case-cohort study, 1984–2002. Arterioscler Thromb Vasc Biol. 2006;2612:2745–2751. [DOI] [PubMed] [Google Scholar]
- 7.Danesh J, Whincup P, Walker M et al. . Low grade inflammation and coronary heart disease: prospective study and updated meta-analyses. BMJ. 2000;3217255:199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ridker PM, Rifai N, Rose L et al. . Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002;34720:1557–1565. [DOI] [PubMed] [Google Scholar]
- 9.Ridker PM, Rifai N, Clearfield M et al. . Measurement of C-reactive protein for the targeting of statin therapy in the primary prevention of acute coronary events. N Engl J Med. 2001;34426:1959–1965. [DOI] [PubMed] [Google Scholar]
- 10.Greenland P, Alpert JS, Beller GA et al. . 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2010;12225:e584–e636. [DOI] [PubMed] [Google Scholar]
- 11.Blaha MJ, Budoff MJ, DeFilippis AP et al. . Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet. 2011;3789792:684–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blankstein R, Budoff MJ, Shaw LJ et al. . Predictors of coronary heart disease events among asymptomatic persons with low low-density lipoprotein cholesterol MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2011;584:364–374. [DOI] [PubMed] [Google Scholar]
- 13.Bild DE, Bluemke DA, Burke GL et al. . Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;1569:871–881. [DOI] [PubMed] [Google Scholar]
- 14.Levey AS, Stevens LA. Estimating GFR using the CKD Epidemiology Collaboration (CKD-EPI) creatinine equation: more accurate GFR estimates, lower CKD prevalence estimates, and better risk predictions. Am J Kidney Dis. 2010;554:622–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;186:499–502. [PubMed] [Google Scholar]
- 16.Carr JJ, Nelson JC, Wong ND et al. . Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;2341:35–43. [DOI] [PubMed] [Google Scholar]
- 17.Yeboah J, Folsom AR, Burke GL et al. . Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the Multi-Ethnic Study of Atherosclerosis. Circulation. 2009;1206:502–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chu CS, Wang YC, Lu LS et al. . Electronegative low-density lipoprotein increases C-reactive protein expression in vascular endothelial cells through the LOX-1 receptor. PLoS One. 2013;88:e70533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao XQ, Zhang MW, Wang F et al. . CRP enhances soluble LOX-1 release from macrophages by activating TNF-α converting enzyme. J Lipid Res. 2011;525:923–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fujita Y, Yamaguchi S, Kakino A et al. . Lectin-like oxidized LDL receptor 1 is involved in CRP-mediated complement activation. Clin Chem. 2011;5710:1398–1405. [DOI] [PubMed] [Google Scholar]
- 21.Fujita Y, Kakino A, Nishimichi N et al. . Oxidized LDL receptor LOX-1 binds to C-reactive protein and mediates its vascular effects. Clin Chem. 2009;552:285–294. [DOI] [PubMed] [Google Scholar]
- 22.Hein TW, Qamirani E, Ren Y et al. . Selective activation of lectin-like oxidized low-density lipoprotein receptor-1 mediates C-reactive protein-evoked endothelial vasodilator dysfunction in coronary arterioles. Circ Res. 2014;1141:92–100. [DOI] [PubMed] [Google Scholar]
- 23.Holvoet P, Jenny NS, Schreiner PJ et al. . The relationship between oxidized LDL and other cardiovascular risk factors and subclinical CVD in different ethnic groups: the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis. 2007;1941:245–252. [DOI] [PubMed] [Google Scholar]
- 24.Zhang YC, Tang Y, Chen Y et al. . Oxidized low-density lipoprotein and C-reactive protein have combined utility for better predicting prognosis after acute coronary syndrome. Cell Biochem Biophys. 2014;682:379–385. [DOI] [PubMed] [Google Scholar]
- 25.Ridker PM, MacFadyen J, Libby P et al. . Relation of baseline high-sensitivity C-reactive protein level to cardiovascular outcomes with rosuvastatin in the Justification for Use of statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER). Am J Cardiol. 2010;1062:204–209. [DOI] [PubMed] [Google Scholar]