Abstract
Background and Objectives
This trial explores whether intravenous iron isomaltoside 1000 (Monofer®) results in a better regeneration of haemoglobin levels and prevents anaemia compared to placebo in preoperative non-anaemic patients undergoing cardiac surgery.
Study Design and Methods
The trial is a prospective, double-blind, comparative, placebo-controlled trial of 60 non-anaemic patients undergoing cardiac surgery. The patients were randomized 1:1 to either 1000 mg intravenous iron isomaltoside 1000 administered perioperatively by infusion or placebo.
Results
Mean preoperative haemoglobin in the active treatment group was 14·3 g/dl vs. 14·0 g/dl in the placebo group. At discharge 5 days after surgery, haemoglobin levels were reduced to 10·7 and 10·5 g/dl, respectively. One month after surgery, haemoglobin concentration had increased to an average of 12·6 g/dl vs. 11·8 g/dl (p = 0·012) and significantly more patients were non-anaemic in the intravenous iron isomaltoside 1000-treated group compared to the placebo group (38·5% vs. 8·0%; p = 0·019). There were no differences in side-effects between the groups.
Conclusion
A single perioperative 1000 mg dose of intravenous iron isomaltoside 1000 significantly increased the haemoglobin level and prevented anaemia 4 weeks after surgery, with a short-term safety profile similar to placebo. Future trials on potential clinical benefits of preoperative treatment with intravenous iron in non-anaemic patients are needed.
Keywords: anaemia, iron, coronary artery bypass surgery
Introduction
Coronary artery diseases are highly frequent causes of morbidity and mortality in the developed and developing countries 1. More than 800 000 patients undergo coronary artery bypass graft (CABG) surgery worldwide each year 2. Perioperative anaemia in surgical patients is well documented and has been associated with decreased quality of life and increased risk of postoperative morbidity and mortality 3. Perioperative blood loss and low erythropoiesis commonly increase the risk of postoperative anaemia and the risk of blood transfusion 4. Though blood transfusion helps to increase the haemoglobin (Hb) levels and avoid the deleterious effects of acute anaemia, several studies have suggested that blood transfusions may increase the risk of postoperative morbidity and mortality following cardiac surgery 5–8. Oral iron does not seem to be effective as demonstrated in a recent study 9. This has prompted a need for a safe alternative treatment 10–12.
Besides the fact that preoperative anaemia is associated with a worse outcome for the patients, it has also been found that patients with a normal Hb level may become anaemic during the surgery. A recent evaluation of patients undergoing cardiac surgery at the Department of Thoracic Surgery at Copenhagen University Hospital, Rigshospitalet, Denmark, showed that there was a decrease in mean ± standard deviation (SD) Hb level presurgery of 14·3 ± 1·3 g/dl to 10·6 ± 1·3 g/dl 2 days after surgery and 9·8 ± 1·3 g/dl 4 days after surgery. To date, no prospective randomized clinical study in cardiac surgery assessing the effect of iron supplementation in patients undergoing cardiac surgery has been reported.
This placebo-controlled trial was designed to evaluate the effect of perioperative administration of intravenous (IV) iron isomaltoside 1000 (Monofer®; Pharmacosmos, Holbaek, Denmark) in preoperative non-anaemic patients undergoing elective or subacute CABG, valve replacement or a combination thereof.
Materials and methods
Study design
This prospective, double-blind, placebo-controlled, randomized comparative, single-centre trial was conducted in Denmark from December 2012 to August 2013 in non-anaemic patients undergoing elective or subacute CABG, valve replacement or a combination thereof. The trial protocol and other related documents were approved by competent authorities and the local ethics committee (The Committees on Health Research Ethics for the Capital Region of Denmark, approval date: 15 March 2011, approval number: H-4-2011-010). The trial was conducted in accordance with good clinical practice and the Declaration of Helsinki. Informed consent was obtained in writing prior to any trial-related activities.
The study is registered at ClinicalTrials.gov (identifier: NCT01563367).
The patients attended 4 visits: screening visit (visit 1), baseline visit/start of therapy (day before surgery or same day) (visit 2), day 5 postoperative (±1 day) (visit 3) and week 4 postoperative (±4 days) (visit 4) during the 4-week trial period. The assessments performed at each trial visit included physical examination, adverse events and laboratory assessments. All assessments performed are shown in Table S1. All the enrolled patients were randomized 1:1 to receive either iron isomaltoside 1000 as an IV infusion of 1000 mg (treatment group A) or placebo (0·9% saline) as IV infusions (treatment group B).
Permuted block randomization with a block size of 4 was used to randomize the patients. The randomization list was prepared centrally by a contract research organization, Max Neeman International Data Management Centre, using a validated computer program (Statistical Analysis Software [SAS] 9.1.3; SAS Institute Inc., Cary, NC) PROC PLAN procedure. An interactive web response system method was used to randomize the eligible patient to the treatment groups. When the patient data had been entered into the interactive web response system, a unique randomization number was generated for the patient, identifying which treatment the patient was allocated to. The screening and enrolment of the patients were performed by the investigator at the site, whereas the entering of the patient data into the interactive web response system generating the randomization number was typically performed by the trial nurse or trial co-ordinator.
Participants
Patients ≥18 years of age undergoing elective or subacute CABG, valve replacement or a combination thereof, with a Hb ≥12·0 g/dl (7·45 mmol/L) for women and a Hb ≥13·0 g/dl (8·1 mmol/L) for men, and who were willing to provide written informed consent were considered eligible to participate in the trial. The exclusion criteria were iron overload or disturbances in utilization of iron (e.g. haemochromatosis and haemosiderosis), s-ferritin >800 ng/ml, known hypersensitivity to any excipients in the investigational drug products, history of multiple allergies, decompensated liver cirrhosis and hepatitis, alanine aminotransferase >3 times normal upper value, acute infections, rheumatoid arthritis with symptoms or signs of active joint inflammation, pregnant or nursing women, participation in any other clinical trial where the trial drug had not passed five half-lives prior to screening, untreated vitamin B12 or folate deficiency, other IV or oral iron treatment within 4 weeks prior to screening visit, erythropoietin treatment within 4 weeks prior to screening visit, and impaired renal function defined by s-creatinine >150 μmol/L. Patients who received blood transfusion <30 days before screening and/or during the elective or subacute CABG, valve replacement or a combination thereof were excluded from participation in the trial.
Any concomitant medication or treatment deemed necessary to provide adequate supportive care was allowed throughout the trial except the erythropoiesis-stimulating agent treatment and any iron supplementation other than investigational drug as this would influence the outcome measures of the trial. All the blood samples were analysed at one central laboratory.
Interventions
Patients in the iron isomaltoside 1000 group received iron isomaltoside 1000 as a single-dose infusion of 1000 mg over 15 min with a maximum single dose of 20 mg/kg. Patients in the placebo group received saline (Natriumklorid 9 mg/ml; Fresenius Kabi, Copenhagen, Denmark) as a single-dose infusion of 100 ml over 15 min.
Objectives and outcomes
The primary efficacy objective of the trial was to demonstrate that IV iron isomaltoside 1000 is superior compared to placebo in leading to a less decrease in the Hb level in non-anaemic patients undergoing cardiac surgery. The secondary efficacy objectives were to compare the effect of iron isomaltoside 1000 and placebo on the need of blood transfusion, iron-related parameters, and safety.
The primary end-point was to assess the change in Hb concentrations from baseline to 4 weeks postoperatively. The secondary end-points were to determine the proportion of patients who were anaemic (women Hb <12 g/dl and men Hb <13 g/dl) at day 5 and week 4, proportion of patients who were able to maintain a Hb between 9·5 and 12·5 g/dl (both values included) at day 5 and week 4, number of patients in each treatment group who needed blood transfusion and number of transfusions administered, change from baseline in concentrations of s-ferritin, s-iron, transferrin saturation (TSAT) and reticulocytes at day 5 and week 4, and safety (adverse events, vital signs, electrocardiogram (ECG), s-phosphate, and haematology and biochemistry parameters). The baseline was defined as the day before surgery or the same day of surgery.
Sample size
The sample size calculation was based on superiority analysis, normally distributed data, type I error = 5 %, 2-sided test, and a power of 80 %. With a sample size of 30 patients/treatment group and an assumed standard deviation of 1·50, the trial was able to detect a difference of 1·1 g/dl in change in Hb concentration from baseline to 4 weeks postoperatively between the treatment groups.
Statistical methods
The following data sets were used in the analysis (Fig.1):
Figure 1.
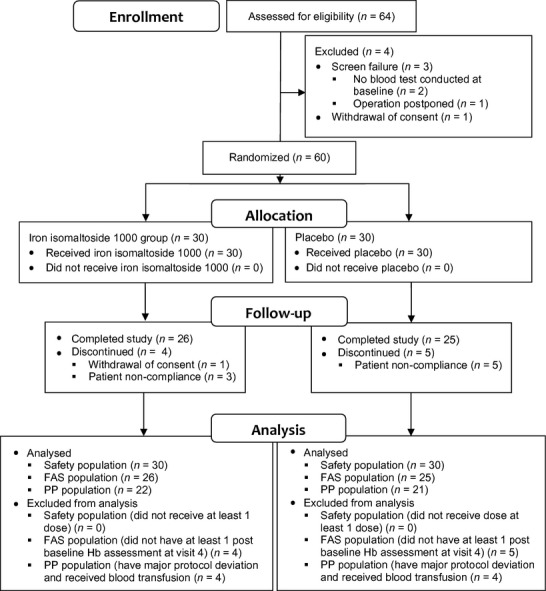
Patient disposition.
Safety analysis set (N = 60): The safety analysis set consisted of all patients who were randomized and received at least one dose of the trial drug. The patients were included as treated.
Full analysis set (FAS, N = 51): The FAS consisted of all patients who were randomized into the trial, received at least one dose of the trial drug and had a Hb assessment at visit 4. Patients were included as randomized, regardless of which treatment they actually received.
Per protocol (PP, N = 43): The PP analysis set consisted of all patients in the FAS who did not have any major protocol deviation and had not received blood transfusion during the trial.
The primary analyses were conducted on FAS and PP analysis sets. The secondary analyses were conducted on the FAS. Number of blood transfusions and the safety analyses were conducted on the safety population.
The primary end-point and the average change in s-ferritin, s-iron, TSAT and reticulocytes from baseline to day 5 and week 4 were summarized descriptively and further analysed by analysis of covariance (ANCOVA) with diagnostic group (defined as elective CABG, subacute CABG, valve replacement or a combination of them) and treatment as factor and baseline Hb value as covariate using Proc Mixed procedure of SAS software. The least square mean and estimate statements were used for treatment estimates and contrasts between the treatments, respectively.
Proportion of patients who were anaemic, who were able to maintain Hb between 9·5 and 12·5 g/dl (both values inclusive), number of patients who needed blood transfusion, and the number of blood transfusion were summarized by frequency and percentage; changes between the treatment groups were compared by Fisher’s exact test.
The adverse events were coded by system organ class and preferred term using Medical Dictionary for Regulatory Activities body system version 16·1. All the safety data were summarized descriptively.
All the statistical tests were two-tailed, and the significance level was 0·05.
Results
Patients
A total of 64 patients were screened from December 2012 to July 2013 of whom 60 (38 underwent CABG where 18 had elective CABG and 20 had subacute CABG, 20 patients had valve replacement, and 2 patients had a combination thereof) were randomized into the trial (30 patients each in the iron isomaltoside 1000 group (treatment group A) and the placebo group (treatment group B)). Overall, patient discontinuation was comparable between the two treatment groups (group A: 13·3% (4/30); group B: 16·7% (5/30)). Details of patient disposition are summarized in Fig.1. Subject demographics and baseline characteristics are summarized in Table1. Overall, more men (87%) than women (13%) were included in the trial. Majority of the patients were Caucasian (95%) and non-smokers (75%).
Table 1.
Patient demographics and baseline characteristics
| Statistics/Category | Treatment group | Overall (N = 60) | |
|---|---|---|---|
| Iron isomaltoside 1000 (n = 30) | Placebo (n = 30) | ||
| Age (years) | |||
| Mean | 65 | 65 | 65 |
| SD | 8 | 11 | 9 |
| Median | 67 | 67 | 67 |
| Range (Min.: Max.) | (47:79) | (45:80) | (45:80) |
| Gender, n (%) | |||
| Men | 26 (87) | 26 (87) | 52 (87) |
| Women | 4 (13) | 4 (13) | 8 (13) |
| Ethnic origin, n (%) | |||
| Caucasian | 29 (96·7) | 28 (93·3) | 57 (95·0) |
| Other | 1 (3·3) | 2 (6·7) | 3 (5·0) |
| Current smoker, n (%) | |||
| Yes | 7 (23·3) | 8 (26·7) | 15 (25·0) |
| No | 23 (76·7) | 22 (73·3) | 45 (75·0) |
| Weight (kg) | |||
| Mean | 88 | 87 | 88 |
| SD | 21 | 19 | 20 |
| Median | 89 | 85 | 88 |
| Range (Min.: Max.) | (55:165) | (57:130) | (55:165) |
| Body mass index (kg/m2) | |||
| Mean | 28 | 28 | 28 |
| SD | 6 | 5 | 5 |
| Median | 28 | 27 | 27 |
| Range (Min.: Max.) | (20:49) | (18:44) | (18:49) |
| Type of surgery | |||
| CABG | 17 | 21 | 38 |
| Valve replacement | 11 | 9 | 20 |
| Combination | 2 | 0 | 2 |
| Biochemistry at baseline | |||
| Haemoglobin (g/dl) | 14·25 | 13·98 | |
| Transferrin saturation (%) | 19 | 21 | |
| Ferritin (ng/ml) | 254 | 286 | |
Exposure to iron
All 60 patients were administered the trial drug at baseline. The duration of infusion was 15 min for 59 patients and 27 min for 1 patient in the iron isomaltoside 1000 group.
Efficacy results
Primary end-point
The primary efficacy analysis on change in Hb concentration from baseline to 4 weeks postoperatively was conducted on the FAS (N = 51) and PP (N = 43) analysis sets.
There was a decrease in mean Hb concentration from baseline to week 4 in both treatment groups in the FAS; however, this decrease was significantly less in the iron isomaltoside 1000 group (treatment group A) as compared to the placebo group (treatment group B) (p = 0·0124) (Fig.2). Similar results were observed in the PP analysis set (Fig.2). Four patients in the iron isomaltoside 1000 group and three patients in the placebo group were included in the FAS and received blood transfusion. Due to the fact that blood transfusions influence the primary end-point and for medical reasons need to be allowed and anticipated to occur in some of the patients, the primary end-point ‘change in Hb concentration from baseline to 4 weeks postoperatively’ was conducted on the FAS (N = 51) as well as on the PP (N = 43) analysis set (the PP analysis set included all patients in the FAS who did not have any major protocol deviation and had not received blood transfusion during the study). Since similar results were shown in both the FAS (including the blood-transfused patients) and PP (excluding the blood-transfused patients) populations, it seems reasonable to presume that the transfused patients included in the FAS did not have a substantial impact on the results.
Figure 2.
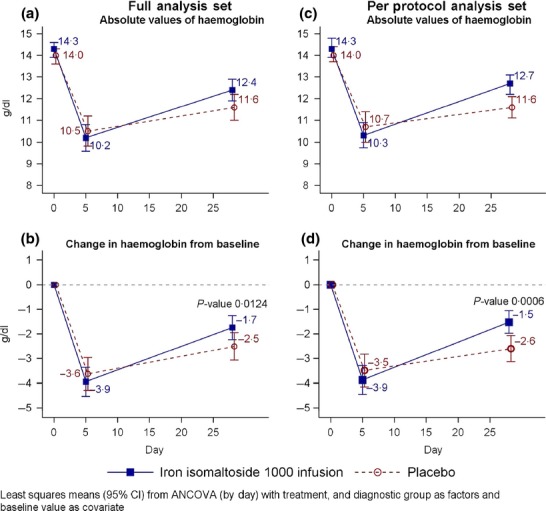
Response profile of the change in haemoglobin (g/dl) concentration from baseline to 4 weeks with respect to LS mean estimate by treatment group and absolute values (a) Full analysis set, absolute values of haemoglobin. (b) Full analysis set, change in haemoglobin from baseline. (c) Per protocol, absolute values of haemoglobin. (d) Per protocol, change in haemoglobin from baseline.
Secondary end-points
There was statistically significant less decrease in s-iron concentration from baseline to day 5 and week 4 in the iron isomaltoside 1000 group as compared to the placebo group (day 5: p < 0·0001; week 4: p < 0·05) (Table S2), an increase in s-ferritin and TSAT concentration from baseline to day 5 and week 4 in the iron isomaltoside 1000 group compared to the placebo group (s-ferritin: day 5 and week 4: p < 0·0001; TSAT: day 5: p < 0·0001, week 4: p = 0·0015), and an increase in reticulocyte counts from baseline to day 5 in the iron isomaltoside 1000 group compared to the placebo group (p = 0·0157) (Fig.3 and Table S2).
Figure 3.
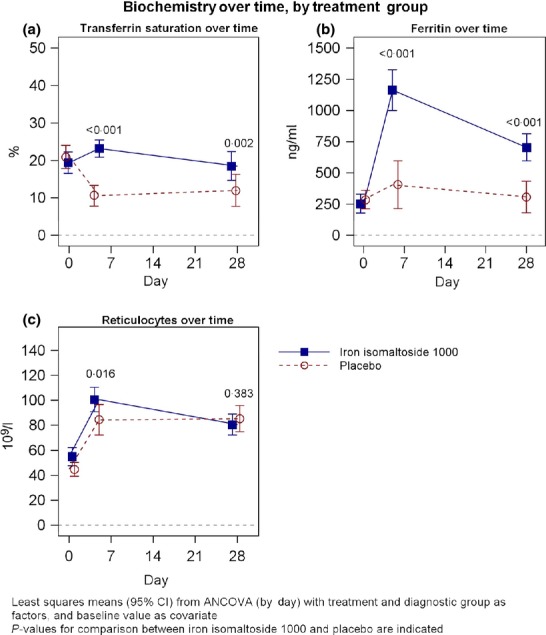
Transferrin saturation (a), serum ferritin (b) and reticulocyte counts (c) over time by treatment group.
No statistically significant difference in the proportion of anaemic patients was observed at day 5 between the two treatment groups (92·3% vs. 100%; p = 0·4902); however, the proportion of non-anaemic patients at week 4 was significantly higher in the iron isomaltoside 1000 group as compared to the placebo group (38·5% vs. 8%; p < 0·05) (Fig.4 and Table S3).
Figure 4.
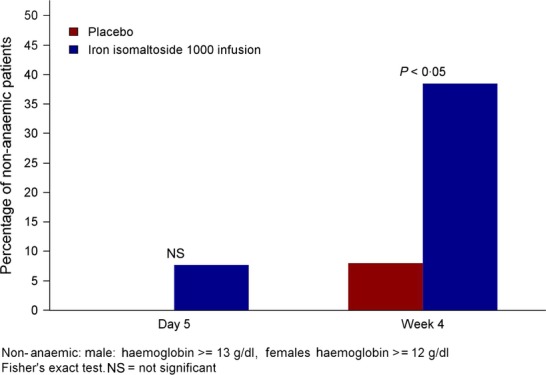
Proportion of non-anaemic patients – full analysis set.
There was no statistically significant difference in the proportion of patients who were able to maintain Hb between 9·5 and 12·5 g/dl at day 5 between the treatment groups (65·4% vs. 88·0%; p = 0·1181). However, a significant lower proportion of patients in the iron isomaltoside 1000 group were able to maintain Hb between 9·5 and 12·5 g/dl as compared to the placebo group at week 4 (46·2% vs. 76·0%; p = 0·0291); this was due to a significant higher proportion of patients reaching a Hb >12·5 g/dl in the iron isomaltoside 1000 group than in the placebo group (53·8% vs. 24·0 %; p = 0·0291) (Table S4).
The proportion of patients who needed blood transfusion postoperatively to day 5 or after day 5 to week 4 postoperatively is given in Table2. There was no statistically significant difference in the number of transfusions.
Table 2.
Summary of required blood transfusions – safety analysis set
| Visit/Category, n (%)a | Treatment group | |
|---|---|---|
| Monofer (n = 30) | Placebo (n = 30) | |
| Postoperative visit | ||
| Total blood transfusion done | ||
| Yes | 4 (13·3) | 6 (20·0) |
| No | 26 (86·7) | 24 (80·0) |
| P-valueb | 0·5273 | |
| Summary for number of blood transfusion | ||
| N | 4 | 5c |
| Mean | 1·25 | 2·20 |
| SD | 0·50 | 1·64 |
| Median | 1·00 | 2·00 |
| Range (Min.: Max.) | (1:2) | (1:5) |
| Postoperative to day 5 | ||
| Total blood transfusion done | ||
| Yes | 4 (13·3) | 5 (16·7) |
| No | 26 (86·7) | 25 (83·3) |
| P-valuea | >0·9999 | |
| Summary for number of blood transfusion | ||
| N | 4 | 5 |
| Mean | 1·25 | 2·20 |
| SD | 0·50 | 1·64 |
| Median | 1·00 | 2·00 |
| Range (Min.: Max.) | (1:2) | (1:5) |
| After day 5 to week 4 | ||
| Total blood transfusion done | ||
| Yes | – | 1 (3·3) |
| No | 26 (86·7) | 24 (80·0) |
| P-valueb | 0·4902 | |
| Summary for number of blood transfusion | ||
| N | – | –c |
| Mean | – | – |
| SD | – | – |
| Median | – | – |
| Range (Min.: Max.) | – | – |
Percentages were calculated by taking corresponding column count N as denominator.
P-value was calculated using Fisher’s exact test.
Data for one transfused patient were missing.
Safety
All (N = 139) the observed treatment-emergent adverse events (TEAEs) were considered as not related to the trial drug (Table3).Of TEAEs, 94% were mild or moderate and 87% were either recovered or recovering. The most frequent TEAE reported for 3 or more patients was atrial fibrillation (group A: 13 events in 12 patients; group B: 12 events in 10 patients) followed by pleural effusion (group A: 3 events in three patients; group B: 6 events in six patients), decreased Hb (group A and group B: 4 events in four patients), oral candidiasis (group A: 3 events in three patients; group B: 4 events in four patients), pneumonia (group A: 5 events in four patients; group B: 2 events in two patients) and infection (group A: 4 events in four patients; group B: 1 event in one patient).
Table 3.
Treatment-emergent adverse events – safety analysis set
| Category, n (%) | Treatment group | |
|---|---|---|
| Monofer (n = 30) | Placebo (n = 30) | |
| Total number of treatment-emergent adverse events reported | 73 | 66 |
| Number of treatment-emergent adverse events by seriousness | ||
| Non-serious | 64 (87·7) | 56 (84·8) |
| Serious | 9 (12·3) | 10 (15·2) |
| Number of treatment-emergent adverse events with relationship of | ||
| Probable | – | – |
| Possible | – | – |
| Unlikely | – | – |
| Not related | 73 (100·0) | 66 (100·0) |
| Number of treatment-emergent adverse events by outcome | ||
| Recovered | 60 (82·2) | 54 (81·8) |
| Recovering | 6 (8·2) | 5 (7·6) |
| Recovered with sequelae | – | – |
| Not Recovered | 6 (8·2) | 4 (6·1) |
| Unknown | 1 (1·4) | 3 (4·5) |
| Number of treatment-emergent adverse events by action taken | ||
| None | 72 (98·6) | 66 (100·0) |
| Drug stopped temporarily | – | – |
| Drug stopped permanently | – | – |
| Unknown | 1 (1·4) | – |
| Patients reporting treatment-emergent adverse events leading to withdraw | – | – |
| Patients reporting serious treatment-emergent adverse events | 8 (26·7) | 9 (30·0) |
| Patients reporting death | – | – |
There was no statistically significant difference in the number of patients with at least 1 TEAE or serious adverse events (SAE) between the treatment groups. Of patients, 28·3% (17/60) reported 19 SAEs, and none of the SAEs was fatal. None of the SAEs was related to the trial drug and was recovered except 1 SAE (cerebrovascular accident) in the placebo group which did not recover. Out of 19 SAEs, 4 in three patients were considered as mild, 11 in 10 patients as moderate, and 4 SAEs in four patients as severe. The most frequent SAE reported for 2 or more patients was atrial fibrillation (group A: 2 events in two patients; group B: 2 events in two patients) followed by pericardial effusion (group A: 2 events in two patients; group B: 1 events in one patient) and post-procedural haemorrhage (group B: 2 events in two patients).
The haematological and biochemistry parameters and vital signs at each trial visit were comparable between the two treatment groups. No cases of hypophosphataemia were observed in any of the patients.
Two patients, one each in the treatment group, had abnormal clinically significant physical observations (group A: atrial fibrillation; group B: left-hand distensibility) at week 4 which were not present at the screening visit. The outcome of atrial fibrillation was recovered, and left-hand distensibility was recovering. Three patients in the iron isomaltoside 1000 group reported abnormal clinically significant ECG at week 4 and not at the screening visit. All the abnormal clinically significant physical observations and ECG findings were captured as not treatment-related adverse events. The change in mean body weight from screening to week 4 was comparable between the two treatment groups.
Discussion
It has also been found that patients with a normal Hb level may become anaemic during the surgery. A recent evaluation of patients undergoing cardiac surgery at the Department of Thoracic Surgery at Copenhagen University Hospital, Rigshospitalet, Denmark, showed that there was a decrease in Hb level presurgery of 14·3 ± 1·3 g/dl to 10·6 ± 1·3 g/dl two days after surgery and 9·8 ± 1·3 g/dl 4 days after surgery. To date, no prospective randomized clinical study in cardiac surgery assessing the effect of iron supplementation in patients undergoing cardiac surgery has been reported. This placebo-controlled, randomized trial evaluated the effect of perioperative IV iron isomaltoside 1000 in non-anaemic patients undergoing elective or subacute CABG, valve replacement or a combination thereof.
Post-cardiac surgery, patients tend to experience a downward drift in Hb and anaemia which often leads to a need for blood transfusion 8. In this trial, we also observed a decline in Hb concentration from baseline to week 4 in both treatment groups; however, this decline was significantly less in the iron isomaltoside 1000-treated group compared to the placebo group. The proportion of anaemic patients was significantly lower in the iron isomaltoside 1000 group compared to the placebo group at week 4 (92% of the placebo group patients were anaemic vs. 61·5% in the iron isomaltoside 1000 group). In the study by Garrido-Martin and colleagues, they concluded that the use of IV or oral iron supplementation proved ineffective in correcting anaemia after cardiopulmonary bypass and did not reduce blood transfusion requirements 13. One possible reason for this finding is that the patient might have received a lower dose of IV iron compared to our study. The patients received 3 doses of 100 mg IV iron (III)–hydroxide sucrose complex per 24 h during pre- and postoperative hospitalization (the cumulative doses are not mentioned), whereas the patients in our study received 1000 mg IV iron isomaltoside 1000.
The significant increase in reticulocyte count with iron isomaltoside 1000 vs. placebo at day 5 shows that the erythropoietic effect of iron isomaltoside 1000 has a rapid onset. Our results on Hb were in line with a previous trial where oral iron supplementation as a four-week course of ferrous sulphate prior to surgery in patients undergoing total hip or knee replacement protected the patients against a fall in Hb during the immediate postoperative period 14. On the other hand, oral iron did not increase preoperative Hb in patients scheduled for hip or knee arthroplasty 9 and often a 4-week preoperative course is not achievable or tolerated in surgery patients. In another trial, preoperative IV iron administration in anaemic patients undergoing major elective surgery also resulted in significant increase in Hb levels and a high rate of anaemia correction 15.
The present trial demonstrated a statistically significant higher increase in s-ferritin and TSAT concentration from baseline to week 4 in the iron isomaltoside 1000 group as compared to the placebo group, suggesting that perioperative IV iron supplementation maintains iron store after cardiac surgery. Similar results were reported in a previous trial where perioperative IV iron with or without erythropoietin preserved the iron stores after knee replacement surgery 16.
There was no statistically significant difference in the number of transfusions between the two treatment groups. This pilot trial was not powered for this, and the numerical differences indicate that such eventual clinical effects may take a larger trial powered for such outcomes and other clinical outcomes. Iron isomaltoside 1000 showed a good safety profile in non-anaemic patients undergoing elective or subacute CABG, valve replacement or a combination thereof. All the TEAEs reported in this trial were not related to the trial drug, and the majority (87%) was either recovered or recovering. SAEs were reported in 26·7% of the patients in the iron isomaltoside 1000 group and in 30% in the placebo group. The majority of the SAEs were mild or moderate and were recovered.
No patient reported hypophosphataemia (defined as a phosphate level <2 mg/dl), which is consistent with two interim analyses of other studies where no clinically significant hypophosphataemia was observed in 25 patients with cancer (ClinicalTrial.gov ID: NCT 01145638) and in 50 patients with non-dialysis-dependent chronic kidney disease (ClinicalTrial.gov ID: NCT 01102413) 17.
The present trial was an exploratory trial with the sample size of 60 patients. Hence, clinical studies of a larger scale would be of interest to further investigate whether the demonstrated treatment effect on Hb results in a possible beneficial clinical effect of iron isomaltoside 1000 administration to non-anaemic patients undergoing elective or subacute CABG, valve replacement or a combination thereof.
In conclusion, the present trial demonstrated that iron isomaltoside 1000 can be used safely and effectively to prevent anaemia after open-heart surgery. The haemopoietic response is already evident at day 5. The safety profile of iron isomaltoside is very favourable. In the present trial, no adverse drug reactions were reported and the number of adverse events reported was at placebo level.
Acknowledgments
The authors gratefully acknowledge all the investigators and trial personnel for their contribution to the trial, the statistical support from Jens-Kristian Slott Jensen, Slott Stat, and the medical writing assistance of Eva-Maria Damsgaard Nielsen in editing the manuscript. Eva-Maria Damsgaard Nielsen is employed by Pharmacosmos A/S. LLT is employed by Pharmacosmos A/S, and the institution (Department of Clinical Immunology, Copenhagen University Hospital, Rigshospitalet) received a fee per patient. PIJ and ASR did not have further conflict of interest. The study was funded by Pharmacosmos A/S (Holbaek, Denmark).
Source of funding
The study was funded by Pharmacosmos A/S (Holbaek, Denmark).
Author contributions
P.I.J and L.L.T. involved in research and trial design; P.I.J, A.S.R and L.L.T. performed data acquisition, data analysis and interpretation. All authors reviewed the manuscript, contributed each with important intellectual content during the manuscript writing and approved the final version.
Supporting Information
Table S1Study flow chart (word file).
Table S2 Changes in s-iron, s-ferritin, transferrin saturation and reticulocyte counts from baseline to day 5 and 4 weeks postoperatively – full analysis set (word file).
Table S3 Summary of proportion of patients who are anaemic at day 5 and week 4 – full analysis set (word file).
Table S4 Proportion of patients able to maintain haemoglobin between 9·5 and 12·5 g/dl at day 5 and week 4 – full analysis set (word file).
References
- WHO. Global Atlas on Cardiovascular Disease Prevention and Control. Geneva: World Health Organization; 2011. http://www.who.int/mediacentre/factsheets/fs317/en/ [Google Scholar]
- Nalysnyk L, Fahrbach K, Reynolds MW, et al. Adverse events in coronary artery bypass graft (CABG) trials: a systematic review and analysis. Heart. 2003;89:767–772. doi: 10.1136/heart.89.7.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munoz M, Gomez-Ramirez S, Martin-Montanez E, et al. Perioperative intravenous iron: an upfront therapy for treating anaemia and reducing transfusion requirements. Nutr Hosp. 2012;27:1817–1836. doi: 10.3305/nh.2012.27.6.6087. [DOI] [PubMed] [Google Scholar]
- Beris P, Munoz M, Garcia-Erce JA, et al. Perioperative anaemia management: consensus statement on the role of intravenous iron. Br J Anaesth. 2008;100:599–604. doi: 10.1093/bja/aen054. [DOI] [PubMed] [Google Scholar]
- Koch CG, Li L, Duncan AI, et al. Transfusion in coronary artery bypass grafting is associated with reduced long-term survival. Ann Thorac Surg. 2006;81:1650–1657. doi: 10.1016/j.athoracsur.2005.12.037. [DOI] [PubMed] [Google Scholar]
- Murphy GJ, Reeves BC, Rogers CA, et al. Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation. 2007;116:2544–2552. doi: 10.1161/CIRCULATIONAHA.107.698977. [DOI] [PubMed] [Google Scholar]
- Surgenor SD, Kramer RS, Olmstead EM, et al. The association of perioperative red blood cell transfusions and decreased long-term survival after cardiac surgery. Anesth Analg. 2009;108:1741–1746. doi: 10.1213/ane.0b013e3181a2a696. [DOI] [PubMed] [Google Scholar]
- George TJ, Beaty CA, Kilic A, et al. Hemoglobin drift after cardiac surgery. Ann Thorac Surg. 2012;94:703–709. doi: 10.1016/j.athoracsur.2012.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachance K, Savoie M, Bernard M, et al. Oral ferrous sulfate does not increase preoperative hemoglobin in patients scheduled for hip or knee arthroplasty. Ann Pharmacother. 2011;45:764–770. doi: 10.1345/aph.1P757. [DOI] [PubMed] [Google Scholar]
- Leal-Noval SR, Munoz M, Paramo JA, et al. Spanish consensus statement on alternatives to allogeneic transfusions: the “Seville document”. TATM. 2006;8:178–202. doi: 10.2450/2013.0029-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lidder PG, Sanders G, Whitehead E, et al. Pre-operative oral iron supplementation reduces blood transfusion in colorectal surgery - a prospective, randomised, controlled trial. Ann R Coll Surg Engl. 2007;89:418–421. doi: 10.1308/003588407X183364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leal-Noval SR, Munoz M, Asuero M, et al. Spanish consensus statement on alternatives to allogeneic blood transfusion: the 2013 update of the “Seville Document”. Blood Transfus. 2013;11:585–610. doi: 10.2450/2013.0029-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrido-Martín P, Nassar-Mansur MI, de la Llana-Ducrós R, et al. The effect of intravenous and oral iron administration on perioperative anaemia and transfusion requirements in patients undergoing elective cardiac surgery: a randomized clinical trial. Interact Cardiovasc Thorac Surg. 2012;15:1013–1018. doi: 10.1093/icvts/ivs344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews CM, Lane DW, Bradley JG. Iron pre-load for major joint replacement. Transfus Med. 1997;7:281–286. doi: 10.1046/j.1365-3148.1997.d01-42.x. [DOI] [PubMed] [Google Scholar]
- Bisbe E, Garcia-Erce JA, Diez-Lobo AI, et al. A multicentre comparative study on the efficacy of intravenous ferric carboxymaltose and iron sucrose for correcting preoperative anaemia in patients undergoing major elective surgery. Br J Anaesth. 2011;107:477–478. doi: 10.1093/bja/aer242. [DOI] [PubMed] [Google Scholar]
- Garcia-Erce JA, Cuenca J, Martinez F, et al. Perioperative intravenous iron preserves iron stores and may hasten the recovery from post-operative anaemia after knee replacement surgery. Transfus Med. 2006;16:335–341. doi: 10.1111/j.1365-3148.2006.00682.x. [DOI] [PubMed] [Google Scholar]
- Kalra PA, Bock K, Meldal M. Iron isomaltoside 1000: a new high dose option for parenteral iron therapy. Port J Nephrol Hypert. 2012;26:13–24. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1Study flow chart (word file).
Table S2 Changes in s-iron, s-ferritin, transferrin saturation and reticulocyte counts from baseline to day 5 and 4 weeks postoperatively – full analysis set (word file).
Table S3 Summary of proportion of patients who are anaemic at day 5 and week 4 – full analysis set (word file).
Table S4 Proportion of patients able to maintain haemoglobin between 9·5 and 12·5 g/dl at day 5 and week 4 – full analysis set (word file).


