The ROM required for eight upper-extremity ADLs in healthy participants was quantified with a methodology that can be used in future studies to develop normative databases of upper-extremity motions and evaluate pathologic populations.
MeSH TERMS: activities of daily living; biomechanical phenomena; range of motion, articular; upper extremity
Abstract
OBJECTIVE. We quantified the range of motion (ROM) required for eight upper-extremity activities of daily living (ADLs) in healthy participants.
METHOD. Fifteen right-handed participants completed several bimanual and unilateral basic ADLs while joint kinematics were monitored using a motion capture system. Peak motions of the pelvis, trunk, shoulder, elbow, and wrist were quantified for each task.
RESULTS. To complete all activities tested, participants needed a minimum ROM of −65°/0°/105° for humeral plane angle (horizontal abduction–adduction), 0°–108° for humeral elevation, −55°/0°/79° for humeral rotation, 0°–121° for elbow flexion, −53°/0°/13° for forearm rotation, −40°/0°/38° for wrist flexion–extension, and −28°/0°/38° for wrist ulnar–radial deviation. Peak trunk ROM was 23° lean, 32° axial rotation, and 59° flexion–extension.
CONCLUSION. Full upper-limb kinematics were calculated for several ADLs. This methodology can be used in future studies as a basis for developing normative databases of upper-extremity motions and evaluating pathology in populations.
Analysis of three-dimensional upper-limb kinematics has the potential to be a useful tool in clinical decision making, similar to how gait analysis is commonly used today. However, determining the upper-limb motions required to complete key activities of daily living (ADLs) has proven difficult. The upper limb offers many degrees of freedom, coordinated movement across multiple joints, and a wide range of motion (ROM) at the joints. A range of different limb trajectories and associated movement patterns result in successful completion of a task. This complexity and associated variability make it difficult to define a clear optimal pattern of activity performance. In addition, unlike gait, the upper limb has no single, most relevant, or cyclic functional activity (van Andel, Wolterbeek, Doorenbosch, Veeger, & Harlaar, 2008). Therefore, it has been difficult to establish the same type of normative patterns for upper-limb motion.
Although many studies have quantified motion of the upper limb (Aizawa et al., 2010; Fitoussi, Diop, Maurel, Laassel, & Penneçot, 2006; Magermans, Chadwick, Veeger, & van der Helm, 2005; Petuskey, Bagley, Abdala, James, & Rab, 2007; Pieniazek, Chwała, Szczechowicz, & Pelczar-Pieniazek, 2007; Raiss, Rettig, Wolf, Loew, & Kasten, 2007; Sheikhzadeh, Yoon, Pinto, & Kwon, 2008; van Andel et al., 2008; Veeger, Magermans, Nagels, Chadwick, & van der Helm, 2006), they have varied significantly in their choice of tasks and in the methods used to measure joint angles, both in equipment used and in how the segments have been defined. This variation makes direct comparison among studies difficult. In addition, studies have typically focused on assessing a single joint or a few joints but have not quantified the three-dimensional ROM for all upper-body segments simultaneously. This component is important to better understand the upper-limb functional requirements necessary to complete ADLs as well as the impact that altered motion at a single joint has on proximal and distal joints during upper-limb ADLs after injury (i.e., compensatory motion patterns).
The appropriate assessment of three-dimensional ROM has important clinical implications. The ROM of upper-limb joints may be restricted by injury or disease; this restriction can have a serious impact on a person’s ability to perform ADLs. Clinically, decreased ROM is treated through stretching (Bonutti, Windau, Ables, & Miller, 1994), manual techniques, and strengthening (Kelley, McClure, & Leggin, 2009). To determine the success of such therapeutic interventions, occupational therapists must first be able to appropriately determine the patient’s ROM. In particular, the ROM for active movements has added value in allowing combined testing of joint range, control, strength, and the patient’s willingness to perform the movement (Aizawa et al., 2013).
The purpose of this study was to characterize and quantify the motions required by the trunk, pelvis, shoulder, elbow, and wrist to perform a select set of common ADLs. The secondary purpose was to develop an upper-limb model, using internationally accepted standards for motion tracking (Wu et al., 2005), to facilitate consistent assessment of clinical populations.
Method
Participants
Fifteen healthy young adults (8 men, 7 women) participated in this study (mean age = 26 yr, standard deviation [SD] = 6; mean height = 1.74 m, SD = 0.08; mean weight = 71.2 kg, SD = 9.0). All participants were right hand dominant as indicated by a score of ≥9 of 10 on the Edinburgh Handedness Inventory (Oldfield, 1971). All participants provided written informed consent before participating in this institutionally approved study.
Experimental Protocol
Thirty-eight reflective markers were placed on the arms, trunk, and pelvis to track the movements of eight body segments at 120 Hz using a motion capture system. Markers were placed on the trunk at the xiphoid process, sternal notch, eighth thoracic vertebra, and seventh cervical vertebra. The pelvis was tracked using markers placed bilaterally on the anterior and posterior superior iliac spines and iliac crests. Clusters of four markers each were placed on the upper arm and forearm to define the segments. The hand was defined by four markers placed at the radial and ulnar styloids and third and fifth metacarpal–phalangeal joints. Additional markers were placed on the medial and lateral humeral epicondyles and right and left acromion processes for a static calibration trial.
Participants completed a series of bimanual and unilateral ADLs. To ensure consistency across participants, a researcher read a description of the task and then demonstrated it for the participant before testing. Participants then completed the eight tasks five times at a comfortable pace. Unilateral tasks were completed first with the right arm and then with the left arm. Not all participants completed all tasks. In addition, data from several conditions were not analyzed because participants did not comply with instructions (e.g., transferred the object between hands rather than using a single hand) or because of technical issues (e.g., markers falling off or being obscured from the cameras) during collection. All tasks began with the participants standing upright with their arms relaxed at their sides (Figure 1C).
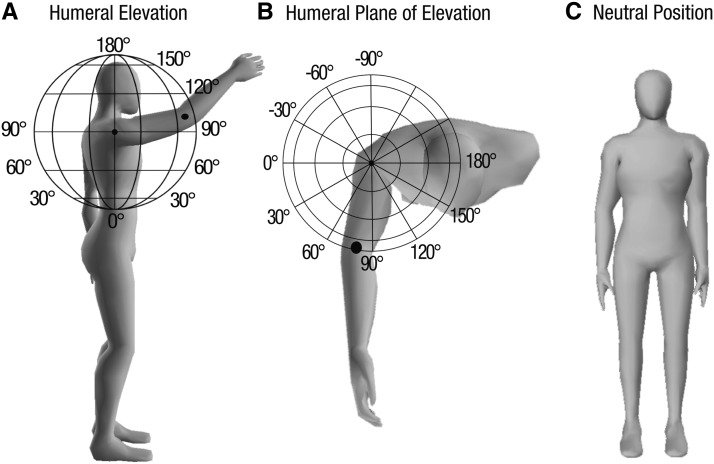
Figure 1.
Shoulder angle definition.
The globe coordinate system is illustrated for a sample movement of a participant reaching toward a can on a high shelf. The rotation axis of the shoulder is assumed to be the midpoint of the globe, and the elbow follows the surface of the globe (Doorenbosch et al., 2003). (A) Illustration of the humeral elevation angle. Latitudes correspond to elevation angle. When the elbow is raised to shoulder height in any plane, the humeral elevation angle is 90°. When the arm is at the side, the elevation angle is 0°. The depicted movement has an elevation of approximately 95°. (B) The humeral plane of elevation is indicated by the longitudes, viewed from the “North Pole.” The plane angle is functionally similar to horizontal adduction. When the humerus is elevated in the frontal plane (pure abduction), the plane angle is 0°. Pure shoulder flexion corresponds to humeral elevation at a plane angle of 90°, and in pure shoulder extension the plane angle is about −90°. The depicted movement has a plane of elevation of approximately 70°. (C) Movements for all joints and segments (shoulder, elbow, and wrist) are measured relative to the position displayed by the avatar, with the humerus in a neutral position by the side, elbow extended, and palm facing toward the midline.
The tasks and the number of participants who successfully completed each task were as follows:
Box off shelf (n = 9 fixed; n = 15 high): Participants stood an arm’s length from a tall shelving unit and were asked to move a shoe box from a higher shelf (fixed = 1.48 m vertical height; high = head height) to a lower shelf (0.96 m).
Can off shelf (n = 9 fixed; n = 15 high): Participants moved a commercially available full 15.5-oz (439-g) can from a high shelf to a low shelf with one arm.
Deodorant (n = 14): Participants reached toward a stick of deodorant that was placed on a 0.96-m-high shelf at the midline. They removed the lid from the deodorant, simulated swiping it three times on their contralateral axilla, then replaced the cap and set the deodorant back on the shelf.
Drinking from a cup (n = 9): Participants reached with one hand toward an empty paper cup that was placed on a 0.96-m-high shelf at the midline. They lifted the cup to or near their mouth, simulated drinking, and placed the cup back on the shelf.
Hand to back pocket (n = 9): Participants reached with one hand and simulated grasping an object in their back pocket on the ipsilateral side. They then extended the arm to simulate handing the object to another person. The task ended when the arm returned to the resting position.
Perineal care (n = 5): Participants began in a seated position on a 16-in. (40.6-cm) foldable commode chair with hands placed on their thighs. A commercially available weighted toilet tissue stand (53 cm tall) was placed 6 in. (15.2 cm) behind the front leg of the folding commode and 6 in. lateral to the commode on the side opposite the hand being tested. When instructed to begin, participants removed a few squares of toilet paper from the roll, simulated wiping from front to back, dropped the toilet paper into the toilet seat opening, and returned their hands to their thighs.
Donning and zipping pants (n = 15): Participants were instructed to don a pair of large elastic-waist pants to their knees, sit, and place their hands on their thighs. When instructed to begin, participants grasped the sides of the pants with both hands, stood, and pulled the pants up to their waist. They then zipped the pants and returned their hands to their side.
Box off ground (n = 15): Participants were instructed to squat down, keeping their back straight, and grasp the handles on both sides of a box placed on the ground. They then placed the box on a standard-height table (0.76 m). The box was 45 cm long, 29 cm wide, and 23 cm tall; weighed 20 lb (9.1 kg); and had handle holes on the sides.
Data Analysis
Marker position data were filtered using a fourth-order low-pass Butterworth filter with a 6-Hz cutoff frequency. Markers were used to create an eight-segment model consisting of hands, forearms, arms, trunk, and pelvis using Visual3D (CMotion, Germantown, MD). For each participant, the shoulder joint center was defined by first measuring the circumference of the shoulder around the acromion and axilla (Hingtgen, McGuire, Wang, & Harris, 2006). Using this approximately circular measurement, we estimated the radius of the shoulder. The joint center was then located inferiorly from the acromion by the measured joint radius (Hingtgen et al., 2006). The local coordinate system of the wrist was defined according to Rao, Bontrager, Gronley, Newsam, and Perry (1996). Joint centers and local coordinate systems for all other segments were defined using International Society of Biomechanics (ISB) recommendations (Wu et al., 2005). We defined the humerus according to the second option of the recommendations, which uses forearm position to determine the orientation of the humerus about its long axis (Wu et al., 2005).
Joint angles were defined as the three-dimensional motion of the distal segment relative to the proximal segment using Euler angle decomposition on the basis of ISB recommendations (Wu et al., 2005). Although using these recommendations should enable comparison across studies, they have several limitations. First, shoulder motion is described by the motion of the humerus with respect to the trunk according to a Y′–X–Y′′ Euler rotation sequence. In this definition, gimbal lock occurs when the elevation of the upper arm is close to 0° (Doorenbosch, Harlaar, & Veeger, 2003). In this position, both the axial rotation angle and the plane of elevation fluctuate greatly, giving rise to extreme values. In the chosen starting position for each movement, the gimbal lock effect occurs. For this reason, the shoulder angles in the first and last 10% of the movement were not included in analyses.
Shoulder angles (thoracohumeral) were described according to the globe system (Doorenbosch et al., 2003) in the following order: plane of elevation (Y′), elevation (X), and axial rotation (Y′′; Figure 1). Elbow angles were defined as motion of the forearm with respect to the upper arm in the following order: flexion (Z), carrying angle (X), and pronation–supination (Y), in which 0° corresponds to full extension and a neutral forearm. Wrist motion was defined as motion of the hand with respect to the radius in the following order: flexion–extension (Z), ulnar–radial deviation (X), and pronation–supination (Y). Motions of the thorax and pelvis relative to the globe coordinate system were lateral flexion, axial rotation, and flexion–extension for the trunk and rotation, obliquity, and pelvic tilt for the pelvis. Trunk motions relative to the pelvis were also calculated as lateral flexion, axial rotation, and flexion–extension. The full Visual3D model and description are included as Supplemental Appendix 1 (12.5MB, pdf) (available online at http://otjournal.net; navigate to this article, and click on “Supplemental”).
We calculated descriptive statistics for peak motion at each joint during each task. These statistics included means, medians, and 95% confidence intervals. Because participants performed every task with both arms, we compared right and left limb motions for all tasks using paired t tests to determine whether there were differences in the average peak values between the limbs. Statistical comparisons were made in IBM SPSS Statistics (Version 20; IBM Corporation, Armonk, NY) with a significance level of p < .05.
Results
We found several small but significant differences between the right and left limbs. In each case, the left limb had higher peak values. Because the objective of this study was to determine the minimal ROM necessary to complete the task, only data from the right arm are presented.
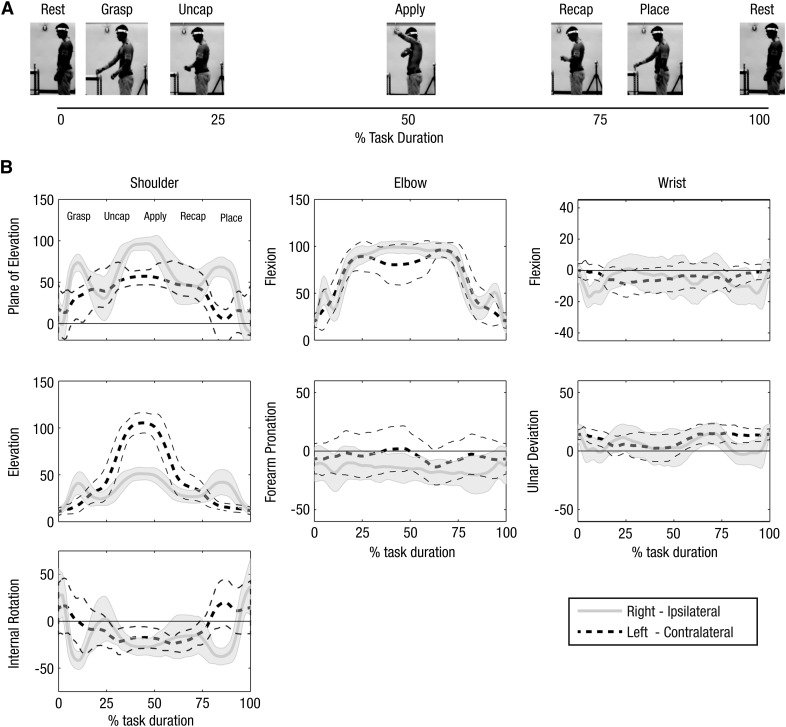
Shoulder (Thoracohumeral) Angles
The largest humeral plane of elevation occurred in the contralateral limb during the perineal care task (mean = 105°) when the person reached across the body to remove the toilet paper from the holder. Peak plane of elevation was also high (100°) for the ipsilateral limb during the deodorant application task when the arm crossed the body to apply deodorant to the contralateral axilla (Figure 2). Peak negative plane of elevation occurred when the arm was behind the body reaching to the back pocket (−65°) and as the participants donned pants (−57°). This task had the greatest elbow supination of the contralateral (left) limb (i.e., the arm that is lifted while deodorant is applied with the right arm). It also required high humeral elevation of the contralateral limb and high humeral plane angle for the ipsilateral limb.
Figure 2.
Kinematic patterns for deodorant application.
(A) Key components of the deodorant task; the x-axis shows the progression of the task as a percentage of completion from start (0%) to finish (100%). (B) The average (bold line) and standard deviation (shaded region or thin line) joint angles for the deodorant application task. Joint angles for shoulder (left), elbow (middle), and wrist (right) are shown for the right (solid) and left (dashed) arms. Labels on the y-axis describe the rotation angle shown and include only the positive motion for simplicity (i.e., ulnar deviation rather than ulnar–radial deviation).
Peak humeral elevation (>105°) was measured during tasks in which participants reached to objects (box, can) placed at head level (Table 1). Another task requiring high elevation was deodorant application (107°), in which the peak occurred when participants raised their contralateral limb so that deodorant could be applied under the axilla (Figure 2; Table 1).
Table 1.
Peak Shoulder (Thoracohumeral), Elbow, and Forearm Angles for Each Task
| Tasks | Angle, Degrees | ||
| Mean | Median | 95% CI | |
| Humeral Plane of Elevation | |||
| Peak motion in front of body | |||
| Perineal care—contralateral limb | 105 | 105 | [96, 115] |
| Deodorant—ipsilateral limb | 100 | 99 | [95, 104] |
| Box off shelf—fixed height | 90 | 88 | [86, 94] |
| Box off shelf—head height | 86 | 86 | [83, 89] |
| Donning and zipping pants | 84 | 85 | [79, 88] |
| Drinking from a cup | 81 | 79 | [74, 88] |
| Hand to back pocket | 80 | 79 | [73, 87] |
| Can off shelf—fixed height | 78 | 78 | [73, 83] |
| Box off ground | 75 | 76 | [72, 78] |
| Can off shelf—head height | 72 | 72 | [68, 77] |
| Deodorant—contralateral limb | 65 | 66 | [61, 70] |
| Perineal care—ipsilateral limb | 61 | 60 | [37, 84] |
| Peak motion behind body | |||
| Hand to back pocket | −65 | −64 | [−75, −55] |
| Donning and zipping pants | −57 | −55 | [−64, −50] |
| Perineal care—ipsilateral limb | −46 | −57 | [−79, −14] |
| Humeral Elevation | |||
| Peak elevation (measured as positive motion from arm at side) | |||
| Box off shelf—head height | 108 | 105 | [104, 111] |
| Deodorant—contralateral limb | 107 | 109 | [101, 113] |
| Can off shelf—head height | 105 | 104 | [102, 108] |
| Box off shelf—fixed height | 86 | 85 | [80, 92] |
| Can off shelf—fixed height | 86 | 84 | [78, 95] |
| Hand to back pocket | 80 | 80 | [74, 85] |
| Drinking from a cup | 71 | 71 | [67, 75] |
| Box off ground | 69 | 70 | [62, 75] |
| Perineal care—contralateral limb | 63 | 67 | [48, 77] |
| Perineal care—ipsilateral limb | 55 | 53 | [45, 65] |
| Deodorant—ipsilateral limb | 55 | 52 | [50, 60] |
| Donning and zipping pants | 51 | 51 | [49, 54] |
| Humeral Rotation | |||
| Peak internal rotation | |||
| Hand to back pocket | 79 | 83 | [63, 95] |
| Donning and zipping pants | 79 | 75 | [71, 86] |
| Perineal care—ipsilateral limb | 65 | 63 | [26, 104] |
| Box off shelf—fixed height | 23 | 21 | [13, 34] |
| Deodorant—ipsilateral limb | 13 | 8 | [2, 24] |
| Deodorant—contralateral limb | 12 | 7 | [0, 24] |
| Box off shelf—head height | 4 | 6 | [−6, 14] |
| Perineal care—contralateral limb | 3 | −3 | [−26, 32] |
| Box off ground | 3 | 1 | [−5, 10] |
| Peak external rotation | |||
| Box off shelf—fixed height | −55 | −53 | [−62, −47] |
| Drinking from a cup | −53 | −53 | [−60, −47] |
| Hand to back pocket | −53 | −51 | [−63, −43] |
| Can off shelf—fixed height | −51 | −51 | [−56, −46] |
| Box off shelf—head height | −48 | −47 | [−53, −44] |
| Can off shelf—head height | −46 | −45 | [−51, −42] |
| Box off ground | −45 | −46 | [−51, −39] |
| Deodorant—ipsilateral limb | −39 | −38 | [−45, −33] |
| Deodorant—contralateral limb | −37 | −35 | [−44, −30] |
| Perineal care—contralateral limb | −36 | −37 | [−42, −30] |
| Perineal care—ipsilateral limb | −25 | −28 | [−47, −4] |
| Donning and zipping pants | −20 | −18 | [−27, −13] |
| Forearm Pronation and Supination | |||
| Peak pronation | |||
| Donning and zipping pants | 13 | 15 | [4, 22] |
| Deodorant—contralateral limb | 8 | 5 | [−1, 18] |
| Drinking from a cup | 6 | 4 | [−3, 14] |
| Can off shelf—fixed height | 4 | 6 | [−5, 13] |
| Box off shelf—fixed height | 4 | 0 | [−7, 14] |
| Hand to back pocket | 3 | −4 | [−6, 13] |
| Peak supination | |||
| Perineal care—ipsilateral limb | −53 | −49 | [−70, −36] |
| Perineal care—contralateral limb | −40 | −33 | [−59, −22] |
| Box off shelf—head height | −38 | −41 | [−47, −30] |
| Box off ground | −36 | −39 | [−44, −29] |
| Hand to back pocket | −32 | −30 | [−40, −24] |
| Can off shelf—head height | −32 | −33 | [−37, −27] |
| Box off shelf—fixed height | −29 | −34 | [−40, −19] |
| Deodorant—ipsilateral limb | −28 | −27 | [−35, −22] |
| Can off shelf—fixed height | −27 | −27 | [−36, −19] |
| Donning and zipping pants | −24 | −24 | [−30, −18] |
| Drinking from a cup | −22 | −18 | [−31, −13] |
| Deodorant—contralateral limb | −20 | −17 | [−27, −13] |
| Elbow Flexion | |||
| Peak flexion | |||
| Drinking from a cup | 121 | 121 | [115, 126] |
| Box off shelf—head height | 120 | 120 | [115, 125] |
| Box off shelf—fixed height | 113 | 113 | [106, 119] |
| Perineal care—ipsilateral limb | 107 | 109 | [98, 116] |
| Can off shelf—head height | 105 | 105 | [98, 111] |
| Deodorant—ipsilateral limb | 104 | 101 | [100, 109] |
| Deodorant—contralateral limb | 103 | 104 | [98, 109] |
| Hand to back pocket | 101 | 106 | [91, 111] |
| Can off shelf—fixed height | 100 | 100 | [92, 107] |
| Donning and zipping pants | 98 | 98 | [92, 105] |
| Perineal care—contralateral limb | 90 | 91 | [74, 105] |
| Box off ground | 81 | 83 | [75, 87] |
Note. The mean, median, and 95% CI range across participants are provided for each peak value. Tasks are listed in order from the greatest motion to least motion for each angle. Not all tasks required motion of behind the body (negative plane angles), internal and external rotation, or pronation and supination of the forearm. CI = confidence interval.
Peak internal rotation of 79° occurred during the hand-to-back-pocket task when the hand was in the final position at the back pocket (Table 1). Peak external rotation (−55°) was measured when the participants took a box off a fixed-height shelf. This peak coincided with the hands grasping the box on the higher shelf.
Elbow–Forearm Angles
All tasks tested required 80° or more of elbow flexion. Peak flexion occurred when drinking from a cup (hand at mouth, 121°) and when moving a box from a high shelf to a low shelf (120°). In the latter task, participants performed the movement in different ways. Some participants moved the box around in a curved path, down and to the left, and others moved it in an arc, down and toward the body. Although both required large elbow flexion, the first resulted in an asymmetric motion in which flexion was greater at the left elbow.
Forearm pronation was generally small (<15°), and not all tasks required it. The largest pronation (13°) occurred as participants donned pants. A majority of the tasks did require supination, however. Peak forearm supination (−53°) occurred during perineal care when participants simulated wiping with their ipsilateral limb.
Wrist Angles
All tasks tested could be accomplished with 38° of wrist flexion and 40° of wrist extension (Table 2). The tasks requiring the greatest wrist motion were donning pants and perineal care. When donning pants, participants generally extended (−40°) and radially deviated (−25°) as they pulled up the pants and flexed (38°) and ulnarly deviated (35°) as they closed the zipper, although participants made numerous submovements of the wrist as they moved the pants forward and backward to pull them up. During perineal care, peak radial deviation (−28°) occurred on the ipsilateral limb during wiping, and peak ulnar deviation (38°) occurred on the contralateral limb when removing toilet paper from the holder.
Table 2.
Peak Wrist Angles for Each Task
| Task Name | Angle, Degrees | ||
| Mean | Median | 95% CI | |
| Wrist Flexion–Extension | |||
| Peak flexion | |||
| Donning and zipping pants | 38 | 37 | [31, 45] |
| Perineal care—ipsilateral limb | 34 | 32 | [19, 49] |
| Hand to back pocket | 28 | 30 | [15, 42] |
| Perineal care—contralateral limb | 16 | 14 | [4, 27] |
| Deodorant—ipsilateral limb | 11 | 11 | [7, 16] |
| Box off ground | 11 | 11 | [5, 17] |
| Box off shelf—head height | 11 | 10 | [7, 15] |
| Can off shelf—fixed height | 10 | 9 | [4, 16] |
| Box off shelf—fixed height | 10 | 11 | [5, 16] |
| Deodorant—contralateral limb | 9 | 8 | [5, 12] |
| Drinking from a cup | 8 | 6 | [3, 12] |
| Can off shelf—head height | 6 | 7 | [2, 10] |
| Peak extension | |||
| Donning and zipping pants | −40 | −37 | [−43, −36] |
| Perineal care—ipsilateral limb | −38 | −38 | [−42, −34] |
| Box off shelf—fixed height | −33 | −34 | [−43, −23] |
| Drinking from a cup | −33 | −30 | [−40, −26] |
| Perineal care—contralateral limb | −32 | −29 | [−43, −21] |
| Can off shelf—head height | −32 | −29 | [−35, −28] |
| Can off shelf—fixed height | −31 | −29 | [−36, −26] |
| Box off shelf—head height | −31 | −28 | [−35, −26] |
| Deodorant—ipsilateral limb | −27 | −25 | [−33, −21] |
| Deodorant—contralateral limb | −21 | −23 | [−25, −17] |
| Box off ground | −19 | −17 | [−27, −12] |
| Hand to back pocket | −15 | −14 | [−29, −1] |
| Ulnar–Radial Deviation | |||
| Peak ulnar deviation | |||
| Perineal care—contralateral limb | 38 | 41 | [30, 47] |
| Donning and zipping pants | 35 | 36 | [30, 39] |
| Hand to back pocket | 35 | 36 | [26, 44] |
| Box off shelf—head height | 34 | 34 | [30, 38] |
| Perineal care—ipsilateral limb | 34 | 39 | [19, 48] |
| Box off ground | 33 | 35 | [28, 39] |
| Box off shelf—fixed height | 32 | 34 | [24, 40] |
| Can off shelf—head height | 30 | 30 | [24, 34] |
| Can off shelf—fixed height | 29 | 30 | [23, 34] |
| Deodorant—contralateral limb | 24 | 24 | [19, 28] |
| Deodorant—ipsilateral limb | 23 | 21 | [19, 28] |
| Drinking from a cup | 23 | 24 | [19, 27] |
| Peak radial deviation | |||
| Perineal care—ipsilateral limb | −28 | −29 | [−43, −13] |
| Donning and zipping pants | −25 | −20 | [−34, −16] |
| Can off shelf—head height | −13 | −13 | [−19, −8] |
| Box off shelf—fixed height | −12 | −9 | [−20, −3] |
| Deodorant—ipsilateral limb | −12 | −10 | [−19, −4] |
| Perineal care—contralateral limb | −12 | −14 | [−31, 8] |
| Drinking from a cup | −11 | −12 | [−19, −3] |
| Box off shelf—head height | −10 | −10 | [−16, −5] |
| Can off shelf—fixed height | −10 | −12 | [−19, −1] |
| Deodorant—contralateral limb | −4 | −6 | [−9, 1] |
| Box off ground | 5 | 7 | [−2, 11] |
| Hand to back pocket | 7 | 10 | [−4, 17] |
Note. The mean, median, and 95% CI range across participants are provided for each peak value. Tasks are listed in order from the greatest motion to least motion for each angle. CI = confidence interval.
Trunk and Pelvic Angles
Trunk and pelvic angles were calculated as maximal excursion or ROM. A majority of the tasks required little to no trunk or pelvis motion (<10°; see Supplemental Appendixes 2–3 (12.5MB, pdf) ). The greatest trunk and pelvic lateral bending motions were found in the perineal care task, with a trunk (trunk relative to lab) ROM of 23°, a trunk–pelvis (trunk relative to pelvis) ROM of 27°, and a pelvis (pelvis relative to lab) obliquity ROM of 17°. This task also required the greatest axial rotation (trunk, 32°; trunk–pelvis, 21°; pelvis, 18°). Donning pants and picking a box up off the ground required the greatest trunk flexion–extension ROM (59° for the box lifting task, 50° for donning pants).
Discussion
This study quantified the motion requirements for the full upper limb and trunk during eight ADLs in healthy participants. The quantification of the three-dimensional motions needed for these tasks should enable clinicians to identify tasks that might be problematic for their patients or provide clinicians with a basis of comparison for evaluating impairments or the effects of interventions. ROMs for the shoulder, elbow, and wrist are similar to those published previously (Aizawa et al., 2010; Magermans et al., 2005; van Andel et al., 2008). In addition, we calculated average movement trajectories from start to finish for each task. Generally, these data show that healthy people made similar movements from trial to trial, and the trajectories were similar between participants for the five trials analyzed.
Shoulder Joint Angles
The model we developed uses ISB recommendations to define segmental coordinate systems and angular rotation sequences, where they are provided. As we have described, computation of three-dimensional rotation of the shoulder joint results in mathematical uncertainty of the joint position when the arm is at the side. Thus, the first and last 10% of shoulder movement were not included in analyses, and the corresponding area in the full joint angle trajectory curves should be viewed with caution. A second limitation is that forearm orientation was used to construct the coordinate system of the humerus. This method helped to reduce the soft tissue artifacts that are generated when movement of the body surface marker does not match that of the bone because of soft tissue movement (Cutti, Paolini, Troncossi, Cappello, & Davalli, 2005). However, it also introduced kinematic coupling with the elbow such that pure elbow flexion–extension or pure pronation–supination movement may generate apparent variation in humeral axial rotation (Cutti et al., 2005), which is particularly problematic when the elbow is near full extension (van Andel et al., 2008).
Another key challenge in presenting motion of the upper limb is that three-dimensional joint angles do not exactly match clinical definitions. For example, at the shoulder, clinicians typically measure shoulder motion in a single plane (sagittal, transverse, frontal) or around the longitudinal axis (rotation). These descriptions cannot be used to determine shoulder motion out of this plane (van Andel et al., 2008). We instead chose to define shoulder motion according to the globe definition of plane of elevation, elevation, and rotation (Figure 1), which allows for a visualization that is considered easily interpretable by clinicians (Doorenbosch et al., 2003).
In spite of these limitations, we determined shoulder joint angles for each task and found them to be consistent across participants. For the perineal care task, we obtained complete data for only 5 participants. Participants were not given specific instructions regarding how to perform wiping. They exhibited a variety of movement patterns, and the results for the perineal care task may not be representative of the general population. Peak humeral plane of elevation was 105° for the contralateral limb during the perineal care task and 100° for deodorant application. Similarly, Magermans et al. (2005) and Aizawa et al. (2010) measured peak humeral plane angles of 99.6° (SD = 8.9°) for washing the contralateral axilla and 109° (SD = 12°) for touching the contralateral axilla, respectively. Peak elevation (105°) occurred when participants reached to take a box off a high shelf. This elevation is significantly less than the 121° (SD = 6.5°) reported by Magermans et al. (2005) for reaching above shoulder level. In that study, shoulder angles were measured as glenohumeral motion (humerus relative to scapula) rather than thoracohumeral motion, as reported here.
Measurement of scapular motion using surface markers may not be reliable for all postures and movements (Sheikhzadeh et al., 2008). Thus, we opted to measure movement of the humerus relative to the trunk, and the reported shoulder angles represent combined scapular and humeral motion, not glenohumeral motion specifically. Although this choice may account for some of the differences seen, it is more likely that the difference is the result of task instructions because participants were reaching upward, but not toward any particular target. All of the tasks could be completed with 79° of internal rotation and 55° of external rotation. Peak internal rotation was significantly less than that measured previously for perineal care (105.4°, SD = 25.2°; Magermans et al., 2005), touching the perineum (135°, SD = 17°; Aizawa et al., 2010), and hand to back pocket (101.7°; van Andel et al., 2008). Peak external rotation for these tasks was similar to those reported previously (Aizawa et al., 2010; Magermans et al., 2005; van Andel et al., 2008; see Supplemental Appendix 1 (12.5MB, pdf) ).
Elbow Angles
All tasks in this study could be completed with 121° of elbow flexion, and all required ≥81° of flexion. Similarly, van Andel et al. (2008) found that a minimum elbow angle of ≥85° was used for all functional tasks they studied. Peak values were also similar across studies (see Supplemental Appendix 4 (12.5MB, pdf) ). Most tasks studied did not require forearm pronation (Table 1), and all could be performed with 53° of supination.
Wrist Angles
The activities tested in this study required a total wrist motion of 38° of flexion, 40° of extension, 38° of ulnar deviation, and 28° of radial deviation. The peak values for ulnar deviation were close to the maximal values (38°–40°) found in several other studies (Li, Kuxhaus, Fisk, & Christophel, 2005; Wigderowitz, Scott, Jariwala, Arnold, & Abboud, 2007). Peak radial deviation during ADLs (28°) was larger than the maximal deviation reported by Aizawa et al. (2013) of 12° but slightly less than the 30° reported by Wigderowitz et al. (2007). This finding suggests that several ADLs tested in this study required the full range of the wrist.
Trunk and Pelvic Angles
Trunk and pelvic angles are rarely reported for upper-limb motions but may contribute significantly when ROM of a joint is restricted (Carey, Jason Highsmith, Maitland, & Dubey, 2008). In the healthy participants tested in this study, motion of the trunk was minimal during most tasks. The largest motions occurred when performing a perineal care task and when donning and doffing pants.
Implications for Occupational Therapy Practice
This study provides a quantitative characterization of the motion required to complete activities of daily living. These data can be used in several important ways:
Occupational therapists can set treatment goals based on the motion used to complete specific tasks.
The patterns of motion can be used to identify activities that may be more difficult for patients with specific joint impairments, allowing training in compensatory approaches.
Conclusion
The results are presented as the entire movement to allow intersegmental comparison during the execution of the complete task. Investigators may use this methodology and preliminary data in future studies on people with upper-limb impairments. We suggest that this methodology be adopted as a standardized protocol to evaluate kinematic data of the upper extremity and trunk.
Supplementary Material
Acknowledgments
The views expressed herein are those of the authors and do not reflect the official policy or position of San Antonio Military Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, the U.S. Department of Defense, the U.S. Department of Veterans Affairs, or the U.S. government. This research was supported by Merit Review Award A9226-R from the U.S. Department of Veterans Affairs Rehabilitation Research and Development Service. Deanna H. Gates is supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K12HD073945).
Contributor Information
Deanna H. Gates, Deanna H. Gates, PhD, is Assistant Professor, School of Kinesiology, University of Michigan, Ann Arbor; gatesd@umich.edu
Lisa Smurr Walters, Lisa Smurr Walters, OTR, CHT, is Occupational Therapist, Center for the Intrepid, Department of Orthopaedics and Rehabilitation, San Antonio Military Medical Center, Ft. Sam Houston, TX.
Jeffrey Cowley, Jeffrey Cowley, MS, is Graduate Student, School of Kinesiology, University of Michigan, Ann Arbor.
Jason M. Wilken, Jason M. Wilken, PT, PhD, is Director, Military Performance Laboratory, Center for the Intrepid, Department of Orthopaedics and Rehabilitation, San Antonio Military Medical Center, Ft. Sam Houston, TX
Linda Resnik, Linda Resnik, PT, PhD, is Research Career Scientist, Providence VA, and Professor (Research), Health Services, Policy and Practice, Brown University, Providence, RI.
References
- Aizawa J., Masuda T., Hyodo K., Jinno T., Yagishita K., Nakamaru K., . . . Morita S. (2013). Ranges of active joint motion for the shoulder, elbow, and wrist in healthy adults. Disability and Rehabilitation, 35, 1342–1349. http://dx.doi.org/10.3109/09638288.2012.731133 [DOI] [PubMed] [Google Scholar]
- Aizawa J., Masuda T., Koyama T., Nakamaru K., Isozaki K., Okawa A., & Morita S. (2010). Three-dimensional motion of the upper extremity joints during various activities of daily living. Journal of Biomechanics, 43, 2915–2922. http://dx.doi.org/10.1016/j.jbiomech.2010.07.006 [DOI] [PubMed] [Google Scholar]
- Bonutti P. M., Windau J. E., Ables B. A., & Miller B. G. (1994). Static progressive stretch to reestablish elbow range of motion. Clinical Orthopaedics and Related Research, 303, 128–134. [PubMed] [Google Scholar]
- Carey S. L., Jason Highsmith M., Maitland M. E., & Dubey R. V. (2008). Compensatory movements of transradial prosthesis users during common tasks. Clinical Biomechanics, 23, 1128–1135. http://dx.doi.org/10.1016/j.clinbiomech.2008.05.008 [DOI] [PubMed] [Google Scholar]
- Cutti A. G., Paolini G., Troncossi M., Cappello A., & Davalli A. (2005). Soft tissue artefact assessment in humeral axial rotation. Gait and Posture, 21, 341–349. http://dx.doi.org/10.1016/j.gaitpost.2004.04.001 [DOI] [PubMed] [Google Scholar]
- Doorenbosch C. A., Harlaar J., & Veeger D. H. (2003). The globe system: An unambiguous description of shoulder positions in daily life movements. Journal of Rehabilitation Research and Development, 40, 147–155. http://dx.doi.org/10.1682/JRRD.2003.03.0149 [PubMed] [Google Scholar]
- Fitoussi F., Diop A., Maurel N., Laassel M., & Penneçot G. F. (2006). Kinematic analysis of the upper limb: A useful tool in children with cerebral palsy. Journal of Pediatric Orthopaedics, Part B, 15, 247–256. http://dx.doi.org/10.1097/01202412-200607000-00003 [DOI] [PubMed] [Google Scholar]
- Hingtgen B., McGuire J. R., Wang M., & Harris G. F. (2006). An upper extremity kinematic model for evaluation of hemiparetic stroke. Journal of Biomechanics, 39, 681–688. http://dx.doi.org/10.1016/j.jbiomech.2005.01.008 [DOI] [PubMed] [Google Scholar]
- Kelley M. J., McClure P. W., & Leggin B. G. (2009). Frozen shoulder: Evidence and a proposed model guiding rehabilitation. Journal of Orthopaedic and Sports Physical Therapy, 39, 135–148. http://dx.doi.org/10.2519/jospt.2009.2916 [DOI] [PubMed] [Google Scholar]
- Li Z. M., Kuxhaus L., Fisk J. A., & Christophel T. H. (2005). Coupling between wrist flexion–extension and radial–ulnar deviation. Clinical Biomechanics, 20, 177–183. http://dx.doi.org/10.1016/j.clinbiomech.2004.10.002 [DOI] [PubMed] [Google Scholar]
- Magermans D. J., Chadwick E. K., Veeger H. E., & van der Helm F. C. (2005). Requirements for upper extremity motions during activities of daily living. Clinical Biomechanics, 20, 591–599. http://dx.doi.org/10.1016/j.clinbiomech.2005.02.006 [DOI] [PubMed] [Google Scholar]
- Oldfield R. C. (1971). The assessment and analysis of handedness: The Edinburgh inventory. Neuropsychologia, 9, 97–113. http://dx.doi.org/10.1016/0028-3932(71)90067-4 [DOI] [PubMed] [Google Scholar]
- Petuskey K., Bagley A., Abdala E., James M. A., & Rab G. (2007). Upper extremity kinematics during functional activities: Three-dimensional studies in a normal pediatric population. Gait and Posture, 25, 573–579. http://dx.doi.org/10.1016/j.gaitpost.2006.06.006 [DOI] [PubMed] [Google Scholar]
- Pieniazek M., Chwała W., Szczechowicz J., & Pelczar-Pieniazek M. (2007). Upper limb joint mobility ranges during activities of daily living determined by three-dimensional motion analysis—Preliminary report. Ortopedia, Traumatologia, Rehabilitacja, 9, 413–422. [PubMed] [Google Scholar]
- Raiss P., Rettig O., Wolf S., Loew M., & Kasten P. (2007). Das Bewegungsausmass der Schulter und des Ellenbogens bei Alltagsbewegungen in der 3D-Bewegungsanalyse [Range of motion of shoulder and elbow in activities of daily life in 3D motion analysis]. Zeitschrift fur Orthopadie und Unfallchirurgie, 145, 493–498. http://dx.doi.org/10.1055/s-2007-965468 [DOI] [PubMed] [Google Scholar]
- Rao S. S., Bontrager E. L., Gronley J. K., Newsam C. J., & Perry J. (1996). Three-dimensional kinematics of wheelchair propulsion. IEEE Transactions on Rehabilitation Engineering, 4, 152–160. http://dx.doi.org/10.1109/86.536770 [DOI] [PubMed] [Google Scholar]
- Sheikhzadeh A., Yoon J., Pinto V. J., & Kwon Y. W. (2008). Three-dimensional motion of the scapula and shoulder during activities of daily living. Journal of Shoulder and Elbow Surgery, 17, 936–942. http://dx.doi.org/10.1016/j.jse.2008.04.008 [DOI] [PubMed] [Google Scholar]
- van Andel C. J., Wolterbeek N., Doorenbosch C. A., Veeger D. H., & Harlaar J. (2008). Complete 3D kinematics of upper extremity functional tasks. Gait and Posture, 27, 120–127. http://dx.doi.org/10.1016/j.gaitpost.2007.03.002 [DOI] [PubMed] [Google Scholar]
- Veeger H. E., Magermans D. J., Nagels J., Chadwick E. K., & van der Helm F. C. (2006). A kinematical analysis of the shoulder after arthroplasty during a hair combing task. Clinical Biomechanics, 21(Suppl. 1), S39–S44. http://dx.doi.org/10.1016/j.clinbiomech.2005.09.012 [DOI] [PubMed] [Google Scholar]
- Wigderowitz C. A., Scott I., Jariwala A., Arnold G. P., & Abboud R. J. (2007). Adapting the Fastrak system for three-dimensional measurement of the motion of the wrist. Journal of Hand Surgery, European Volume, 32, 700–704. http://dx.doi.org/10.1016/j.jhse.2007.06.019 [DOI] [PubMed] [Google Scholar]
- Wu G., van der Helm F. C., Veeger H. E., Makhsous M., Van Roy P., Anglin C., . . . Buchholz B.; International Society of Biomechanics. (2005). ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—Part II: Shoulder, elbow, wrist and hand. Journal of Biomechanics, 38, 981–992. http://dx.doi.org/10.1016/j.jbiomech.2004.05.042 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.