Editor,
A 66-year-old peritoneal dialysis (PD) patient presented with new-onset edema, weight gain, hypotension, and oliguria 5 weeks after influenza vaccination (Vaxigrip; Sanofi Pasteur MSD, Gouda, The Netherlands). Her medical history included end-stage renal disease (ESRD) due to IgA nephropathy, and breast cancer treated in 2009 with no evidence of recurrence on mammography 6 weeks before presentation. One year ago, she had similar but milder symptoms 1 week after the same type of influenza vaccination, which responded well to conservative treatment without hospitalization.
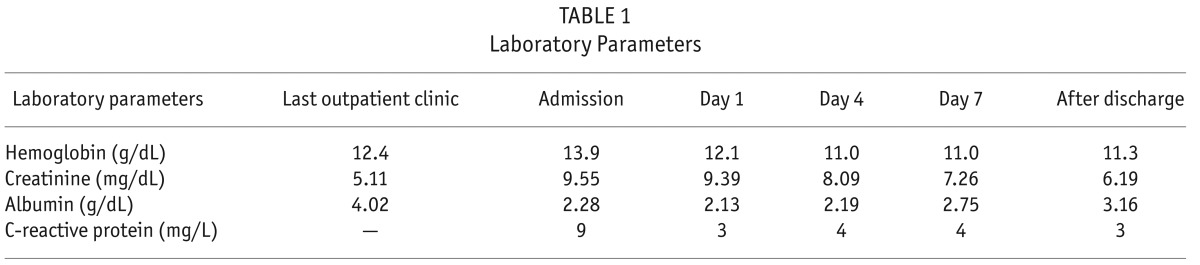
The patient did well on her PD regimen, which consisted of 3 nocturnal cycles of biocompatible dialysate solution, icodextrin during the day, and an extra manual exchange with amino-acid based solution in the evening. She had a residual diuresis of 1,700 mL per day, and there was zero net ultrafiltration. Hypertension was controlled with telmisartan and lercanidipine. She presented to the dialysis unit with hypotension (blood pressure 80/60 mmHg), complete anuria for the previous 2 days, weight gain of 4 kg, and peripheral edema without elevated jugular venous pressure. Accompanying symptoms were a non-productive cough for 1 week, diffuse myalgia, and loss of appetite. Laboratory analysis revealed hypoalbuminemia, increased hemoglobin, and increased serum creatinine (Table 1). Chest X ray was unremarkable. Apart from flu-like symptoms, there were no clinical signs of infection and/or sepsis, and C-reactive protein was not elevated (Table 1). Transthoracic echocardiography revealed a marked inspiratory collapse of the inferior vena cava as well as a normal left ventricular ejection fraction. Serology was negative for influenza, parainfluenza, echovirus, Coxsackievirus, respiratory syncytial virus, adenovirus, mycoplasma pneumoniae, chlamydia pneumoniae, legionella pneumophila, and Coxiella burnettii. There was no monoclonal gammopathy. Serum tryptase and complement C4 and C1 esterase activity were normal.
TABLE 1.
Laboratory Parameters
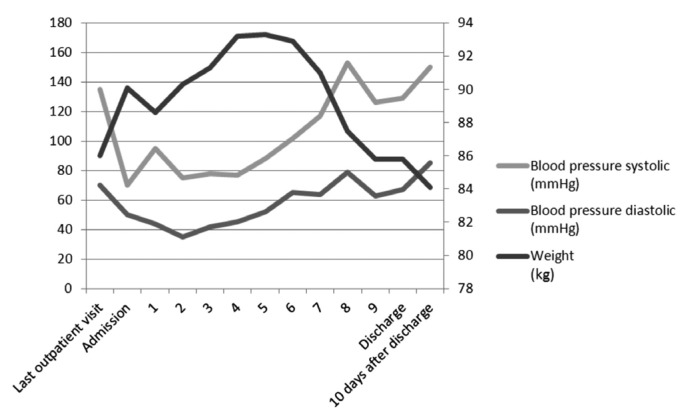
The patient was diagnosed with systemic capillary leak syndrome (SCLS) (1). Supportive therapy was initiated with judicious fluid administration under frequent monitoring of blood pressure, body weight, and diuresis. Dialysate glucose concentrations were altered in order to adjust ultrafiltration according to volume status assessment. Additional treatment with intravenous immunoglobulin appeared unnecessary since blood pressure and diuresis started to improve from day 4. Ten days after presentation, body weight, blood pressure (as illustrated in Figure 1), residual diuresis, and serum albumin normalized. Although a relationship between the influenza vaccination and SCLS could not be proven, we reported this possible side effect of the influenza vaccination to the Netherlands Pharmacovigilance Center (Lareb).
Figure 1 —
Evolution of blood pressure and body weight.
To our knowledge, this is the first report of SCLS in a patient on PD. Fluid management in patients with SCLS is challenging, and acute kidney injury frequently develops. After an initial phase of intravascular volume depletion with anuria and shock, the recovery phase results in rapid fluid redistribution, with the risk of volume overload and pulmonary edema. In this setting, PD seems to be the optimal dialysis method because it allows tight correction of fluid balances by adjusting ultrafiltration. Also, more gradual and continuous fluid removal by PD, compared with intermittent hemodialysis (HD), results in optimization of hemodynamic stability (2,3). Because our patient was on PD, initiation of continuous venovenous HD with HD catheter placement could be avoided.
We hypothesize that, in the absence of an alternative explanation, the immunologic response to the influenza vaccination played an important role in the development of SCLS in this patient. Although we were unable to prove this hypothesis, there is a temporal relationship between the vaccination and the reaction, and the patient had a similar episode following a previous vaccination. Previously, 1 report of SCLS following influenza A virus infection was published (4), but we did not find an association between SCLS and influenza vaccination in the literature. When assessed using the Naranjo adverse drug reaction (ADR) probability scale, a score of 5 assigned this as a probable ADR (5 – 8 points) (5). The score was based on: there are no previous reports on this ADR (0); the ADR appeared after administration of the vaccine (+2); the ADR improved when the drug was discontinued (0); the ADR reappeared when an influenza vaccine was readministered (0); there were no alternative causes that could have caused the ADR (+2); a placebo was not given (0); drug detection in the blood was not done (0); there were no different doses administered (0); the patient had a similar reaction with an influenza vaccination the year before (+1); the event could not be confirmed by objective evidence (0).
In conclusion, this is the first case report of SCLS in a patient on PD, and we suggest that this episode was probably caused by influenza vaccination.
Disclosures
The authors have no financial conflicts of interest to declare.
REFERENCES
- 1. Druey KM, Greipp PR. Narrative review: the systemic capillary leak syndrome. Ann Intern Med 2010; 153:90–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nakayama M. Nonuremic indication for peritoneal dialysis for refractory heart failure in cardiorenal syndrome type II: review and perspective. Perit Dial Int 2013; 33(1):8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Selby NM, McIntyre CW. Peritoneal dialysis is not associated with myocardial stunning. Perit Dial Int 2011; 31(1):27–33. [DOI] [PubMed] [Google Scholar]
- 4. Perme T, Pokorn M, Markelj G, Avčin T, Battelino T, Uršič T, et al. Two episodes of systemic capillary leak syndrome in an 8-year-old boy, following influenza A virus infection. Pediatr Infect Dis J 2014; 33(2):222–4. [DOI] [PubMed] [Google Scholar]
- 5. Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981; 30:239–45. [DOI] [PubMed] [Google Scholar]