Abstract
OBJECTIVE
In the post-sternotomy mediastinitis patients, Staphylococcus aureus is the pathogenic microorganism encountered most often. In our study, we aimed to determine the efficacy of antibiotic treatment with vancomycin and tigecycline, alone or in combination with hyperbaric oxygen treatment, on bacterial elimination in experimental S. aureus mediastinitis.
METHODS
Forty-nine adult female Wistar rats were used. They were randomly divided into seven groups, as follows: non-contaminated, contaminated control, vancomycin, tigecycline, hyperbaric oxygen, hyperbaric oxygen + vancomycin and hyperbaric oxygen + tigecycline. The vancomycin rat group received 10 mg/kg/day of vancomycin twice a day through intramuscular injection. The tigecycline group rats received 7 mg/kg/day of tigecycline twice a day through intraperitoneal injection. The hyperbaric oxygen group underwent 90 min sessions of 100% oxygen at 2.5 atm pressure. Treatment continued for 7 days. Twelve hours after the end of treatment, tissue samples were obtained from the upper part of the sternum for bacterial count assessment.
RESULTS
When the quantitative bacterial counts of the untreated contaminated group were compared with those of the treated groups, a significant decrease was observed. However, comparing the antibiotic groups with the same antibiotic combined with hyperbaric oxygen, there was a significant reduction in microorganisms identified (P<0.05). Comparing hyperbaric oxygen used alone with the vancomycin and tigecycline groups, it was seen that the effect was not significant (P<0.05).
CONCLUSION
We believe that the combination of hyperbaric oxygen with antibiotics had a significant effect on mediastinitis resulting from methicillin-resistant Staphylococcus aureus. Methicillin-resistant Staphylococcus aureus mediastinitis can be treated without requiring a multidrug combination, thereby reducing the medication dose and concomitantly decreasing the side effects.
Keywords: Mediastinitis, Hyperbaric Oxygenation, Vancomycin
| Abbreviations, acronyms & symbols | |
|---|---|
| HBO | = Hyperbaric oxygen |
| MIC | = Minimum inhibitory concentrations |
| MRSA | = Methicillin-resistant Staphylococcus aureus |
| PBS | = Phosphate-buffered saline |
| SD | = Standard deviation |
INTRODUCTION
While mediastinitis developing on the median sternotomy incision after heart surgery is rarely seen (0.5-8%), it is a complication with serious results the majority of the time[1]. Hospital stays related to mediastinitis increase hospital costs[2,3]. It frequently occurs due to the endogenous flora of the patient inoculating the surgical mediastinal cavity. After cardiac surgery with median sternotomy, the most frequently observed pathogen is methicillin-resistant Staphylococcus aureus (MRSA), which is also the bacterium isolated in most blood cultures[4,5].
After diagnosis of mediastinitis, in addition to serious antibiotic treatment, surgical interventions such as primary closure after sternum debridement using vancomycine paste instead of bone vax, closing with a muscle flap after total removal of the sternum using skeletonised left internal thoracic artery and closing the skin completely for closed drainage may be used[6-8]. Due to the bactericidal properties of vancomycin on methicillin-resistant staphylococcal infections, systemic vancomycin is the most frequently chosen antibiotic for severe infections like mediastinitis after surgery linked to MRSA[9]. However, side effects such as renal failure and hearing loss may be observed to be linked to vancomycin use[10]. To protect against these unwanted side effects there is a need to use additional treatments. Adjuvant treatments like hyperbaric oxygen (HBO) treatment are required, but there are insufficient data n this topic in the current literature[11].
Tigecycline is a broad-spectrum glycylcycline effective against Gram-positive and Gram-negative pathogens in soft tissue infections. Between 2004 and 2009, no resistance to tigecycline was observed in soft tissue infections with MRSA, and all the minimum inhibitory concentrations (MIC) were at or below susceptibility break points[12,13].
Studies comparing new antibiotics like tigecycline with vancomycin have shown that tigecycline is more effective against MRSA[14]. An experimental rat model found that tigecycline was significantly superior to vancomycin in this application[15]. HBO has become a focus of interest for mediastinitis treatment in recent years; however, the patient numbers in both experimental and prospective randomised studies are insufficient[16].
The main aim of our study was to compare the efficacy of HBO alone and combined with tigecycline and vancomycin in an experimental model of mediastinitis. In addition, we aimed to compare the proven therapeutic effectiveness of vancomycin against MRSA with the newer antibiotic tigecycline in an experimental mediastinitis model.
METHODS
The study was performed at the Canakkale Onsekiz Mart University Experimental Research Application and Research Centre. It was approved by the Canakkale Onsekiz Mart University Animal Research Ethics Committee, Canakkale, Turkey. All animals received human care in compliance with the principles of laboratory animal care developed by the National Academy of Sciences[17]. During the study, the animals were housed in Canakkale Onsekiz Mart University Experimental Research Application and Research Centre under veterinary control in rooms with a temperature of 25ºC and humidity of 52%, and given free access to standard feed and water.
Organisms and susceptibility testing
This study used the ATCC 43300 strain of MRSA. The antibiotic susceptibility was assessed with a Vitek 2 (BioMérieux, Marcy l'Etoile, France) in the Microbiology Laboratory of Canakkale Onsekiz Mart University.
In vivo rat model and drugs
This study used 49 female adult Wistar rats weighting 250-300 g, with each group comprising 7 rats. The rats were randomly divided into seven groups, as follows: uncontaminated control (group 1), contaminated control (group 2), vancomycin (group 3), tigecycline (group 4), HBO (group 5), vancomycin+HBO (group 6) and tigecycline+HBO (group 7). To anaesthetise the rats, ketamine hydrochloride (90 mg/kg of body weight; Pfizer, Luleburgaz, Turkey) and xylazine hydrochloride (3 mg/kg of body weight; Bayer AG, Leverkusen, Germany) were used. Each animal was laid securely in supine position for the operation. After, the chest wall was cleaned with 10% povidone-iodine, a sterile towel was used to cover the sternum (Figure 1), and then a central line skin incision was completed. Both major pectoral muscles were divided along the central line and the sternal bone was exposed well. The mid-sternal incision was completed using a no. 15 blade; after, haemostasis was provided by sterile sponges, the mediastinum was entered behind the sternum and a pocket was formed. In the sham group rats, non-contaminated sterile physiological serum was injected into the mediasternal pocket. In all other groups a concentration of 2x107 colony-forming units (CFU)/ml of MRSA strain ATCC 43300 in 1 ml of physiological serum solution was injected into the mediastinum with an insulin injector and the mediastinum was filled with fluid. Later, the sternum and subdermis were sutured with 5/0 polypropylene suture material.
Fig. 1.
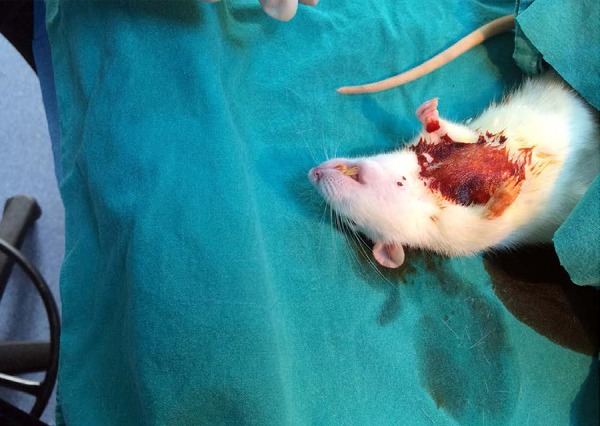
Mediastinal appearance before sternotomy.
After the surgical procedure, the rats were placed in cages and monitored for hyperaemia, oedema, fever and purulent discharge for seven days. During this time, the rats had free access to standard feed and water. Treatment began 2 days later. In groups 1 and 2, no medication was administered. Postoperatively, in Groups 3, 4, 6 and 7, antibiotic treatment was given twice a day for 7 days. In Groups 5, 6 and 7, HBO with 100% oxygen at a pressure of 2.5 atm was administered once a day for 7 days (Table 1). To identify the microbial load in rats in the non-contaminated and contaminated control groups, at the start of treatment, the non-contaminated animals were sacrificed and equal size thin sections of the upper sternum were removed (Figure 2). The rats in all of the other groups had sternotomy applied 12 h after the end of the 7 day treatment. Equal-sized tissue pieces and the upper section of the contaminated part of the sternum were removed by sternotomy under aseptic conditions. Later, the animals were given a high dose of anaesthetic and sacrificed.
Table 1.
The results of experimental rat mediastinitis after treatment.
| Groups | Therapy | Number of culture negative/ total | Bacterial count: Mean±S.D. log10CFU/g |
|---|---|---|---|
| Group 1 n=7 | No therapy (Uncontaminated) | 10/10 | 0.0 |
| Group 2 n=7 | No therapy (Contaminated) | 0/10 | 3.96±0.56 |
| Group 3 n=7 | Vancomycin | 0/10 | 1.90±0.27 |
| Group 4 n=7 | Tigesiklin | 0/10 | 2.05±0.32 |
| Group 5 n=7 | HBO | 0/10 | 3.11±0.54 |
| Group 6 n=7 | Vancomycin+HBO | 0/10 | 1.52±0.95 |
| Group 7 n=7 | Tigesiklin+HBO | 0/10 | 1.79±0.98 |
Mean±S.D. log10 CFU/g
Fig. 2.
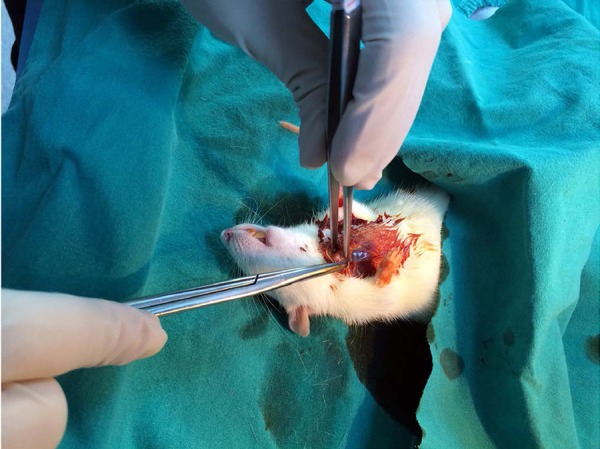
Removing of the upper sternum.
Treatment protocols
Group I (sham group; n=7): Uncontaminated control group, no contamination or antibiotic therapy.
Group II (control group; n=7): Untreated contaminated control group, local contamination with MRSA, no antibiotic therapy.
Group III (vancomycin group; n=7): Vancomycin (Edicine, Sandoz, Istanbul, Turkey) intramuscular injections at 10 mg/kg/ day, twice a day for 7 days.
Group IV (tigecycline group; n=7): Tigecycline (Tygacil, Wyeth Pharmaceuticals, Havant, UK) intraperitoneal injections at 7 mg/kg/day, twice a day for 7 days.
Group V (HBO group; n=7): HBO with 100% oxygen at a pressure of 2.5 atm for 90 min, once a day for 7 days.
Group VI (vancomycin + HBO group; n=7): Vancomycin intramuscular injections at 10 mg/kg/day, twice a day for 7 days, and HBO with 100% oxygen at a pressure of 2.5 atm once a day.
Group VII (tigecycline + HBO group; n=7): Tigecycline intraperitoneal injections at 7 mg/kg/day, twice a day for 7 days, and HBO with 100% oxygen at a pressure of 2.5 atm once a day.
Assessment of the infection
The explanted sternal upper portion and surrounding tissue samples were placed in sterile tubes and washed in sterile saline solution. Following this, they were placed in tubes containing 10 ml of phosphate-buffered saline (PBS) solution, and vortexed for 1 min to remove the adhering bacteria from the tissue and sternum. Quantification of viable bacteria was performed by culturing serial 10-fold dilutions (0.1 ml) of the bacterial suspension on blood agar plates. All plates were incubated at 37ºC for 48 h and evaluated for the presence of MRSA. The organisms were quantitated by counting the number of CFU/g per tissue. The results were converted to log form.
Statistical analysis
Quantitative culture results are presented as arithmetic mean±standard deviation (SD) CFU/ml. Differences among the groups were evaluated using Kruskal-Wallis analysis and multiple comparisons between the groups were performed using the Mann-Whitney test. Differences were considered statistically significant when P<0.05. Data were analysed by statistical software (SPSS for Windows 17.0; SPSS, Chicago, IL).
RESULTS
In this study, we aimed to assess the efficacy of vancomycin, which has been proven for the treatment of mediastinitis, in comparison with the relatively newly used tigecycline, HBO and combinations of these. In all contaminated rats, macroscopic mediastinitis findings were observed (tissue oedema). Especially in the untreated contaminated group, advanced-degree infected tissues with purulent fibrin adhesions were present. With the exception of group 1, comprising non-contaminated rats which were not given antibiotherapy, macroscopic mediastinitis findings in the groups were compared. The culture-negative rates and bacterial counts linked to mediastinitis in each group are shown in Table 1. The mean growth sizes of microorganisms in the mediastinal areas within the sternum were compared. When the quantitative bacterial counts in the mediastinal region within the sternum in the contaminated non-treated group (group 2) were compared with the treated groups (group 3-7), a significant reduction was observed (P<0.05). Comparing groups with vancomycin and tigecycline administered as prophylactics, there was no statistically significant difference observed (P>0.05). However, comparing the antibiotic groups with the same antibiotic combined with HBO, there was a significant reduction in the number of microorganisms (P<0.05). In addition, when the vancomycin+HBO (group 6) and tigecycline+HBO (group 7) were compared, there was a significant reduction in the amount of microorganisms in the group treated with combined vancomycin (P<0.05).
Comparing the use of HBO alone with the untreated contaminated group, a significant reduction in bacteria counts was observed (P<0.05); however, comparing HBO alone with the vancomycin and tigecycline groups, the effect was observed not to be significant (P>0.05).
DISCUSSION
In this experimental mediastinitis model, we aimed to compare tigecycline with vancomycin, which is classically used to treat mediastinitis linked to MRSA. In addition, we aimed to compare the treatment efficacy of both antibiotics combined with HBO. We proved that there was no statistical superiority of either antibiotic when used alone.
In this study, we used previously applied experimental rat mediastinitis models[18,19]. When the literature was examined, we found several animal models using tigecycline, vancomycin and HBO against MRSA, so we aimed to use these antibiotics and HBO. However, we did not discover any rat model involving the combined use of tigecycline and HBO[15,20-22]. Tigecycline was first derived from minocycline, and is a broad spectrum antibiotic of the glycylcycline class with broad in vitro activity[23,24].
There is no requirement to regulate the dose of tigecycline for patients with renal failure or even those with mild to moderate hepatic dysfunction; moreover, it is not induced or inhibited by cytochrome p450[23,25]. In addition, studies of medication interactions have shown that when tigecycline is used with medications like warfarin and digoxin, no side effects were observed in healthy individuals[26,27]. The most frequently observed side effects are mild to moderate nausea and vomiting in the early stages, mainly the first 1-2 days[28].
Tigecycline has been used successfully in the treatment of many severe and mortally progressing types of mediastinitis, such as Mycobacterium chelonae, pan-resistant Acinetobacter baumannii mediastinitis and multidrug-resistant Klebsiella pneumoniae mediastinitis[29-31].
Vancomycin is an antibiotic frequently chosen for the treatment of severe MRSA infections like mediastinitis. As this has a slow killing effect on glycopeptide bacteria, it should be used for treatment of long-term diseases and this may cause a risk of severe kidney failure for patients[32-34]. Although vancomycin is not routinely recommended for use in cardiac surgery, it is important to use it in patients with an increased risk or cases with a high incidence of MRSA[35]. However, there has been no study on the role of tigecycline in a rat model or in combination with HBO.
Another aim of our study was to compare the efficacy of HBO combined with antibiotic treatment or used alone for MRSA mediastinitis. HBO therapy involves the treatment of patients with 100% oxygen at higher than atmospheric pressure within a hyperbaric chamber[36]. HBO causes increased dissolved oxygen levels in blood; this in turn causes hyperoxia in tissues. It restores the bactericidal capacity of leukocytes in hypoxic wounds by increasing tissue oxygen tensions[37]. Moreover, it has been used to treat difficult cases for many years. Although the effective mechanism of HBO is not fully understood, it has been observed to activate many mechanisms, including collagen synthesis[38], accelerated macrophage infiltration[39], fibroblast proliferation[40,41], growth factor proliferation[42,43], modulation of hypoxia-inducible factor 1 alpha[44], improved antibactericidal capacity[45], bacteriostatic effects[46,47] and stimulation of angiogenesis[48]. In this study, when the use of HBO alone was compared with the untreated group with MRSA mediastinitis, a reduction in the number of bacteria was found; however, when HBO alone was compared with vancomycin and tigecycline, the effect was not observed to be significant.
HBO (100% oxygen once per day for 90-120 min at 2-3 atm) can generally be combined with antibiotics like penicillins, beta-lactamase inhibitors, cephalosporins, aztreonam, imipenem, vancomycin, clindamycin, rifampin, aminoglycosides, fluoroquinolones, trimethoprim/sulphamethoxazole, metronidazole, teicoplanin, quinupristin and dalfopristin, and is used to treat osteomyelitis. Thus, the efficacy of an antibiotic is increased in hypoxic tissues[49]. It has been observed that HBO increases the effectiveness of debridement and antibiotic treatment. Topuz et al.[50] observed heightened efficacy when HBO was combined with antibiotics and surgery for spinal tuberculosis patients.
In our study, similar to other research using HBO and combinations of a classic and new antibiotic like vancomycin and teicoplanin, we researched the efficacy of these treatments in rats with MRSA mediastinitis. While HBO alone resulted in a significant drop in the number of bacteria, its combination with either antibiotic significantly increased the efficacy of the medication.
When this study is evaluated, there are some limitations to consider. The pathogenic bacteria were directly inoculated to the sternal and mediasternal layers, and this situation is not appropriate for clinical comparison. For ethical reasons, the treatment continued for 7 days, but longer duration of treatment may produce better results. For technical reasons, we did not obtain sufficient data on systemic infection (direct histological examination, white blood cells). Moreover, we did not obtain sufficient data on the serum antibiotic concentrations. In spite of these limitations, this is the only study to compare the effects of HBO with new generation antibiotics like tigecycline in the in vivo environment.
CONCLUSION
We conclude that the combination of HBO with antibiotics shows a significant effect on MRSA mediastinitis. HBO can also reinforce antibacterial therapy and speed up healing. MRSA mediastinitis can be treated without requiring multidrug combinations, thereby decreasing the required dose of medication, and as a result, reducing its side effects. In the future, ethical permission for human studies will determine the efficacy of HBO in the treatment of MRSA mediastinitis.
| Authors' roles & responsibilities | |
|---|---|
| TK | Final manuscript approval |
| AV | Study conception and design; final manuscript approval |
| AT | Manuscript writing and critical review of its content; final manuscript approval |
| EO | Analysis/interpretation of data; statistical analysis; final manuscript approval; manuscript writing or critical review of its content |
| AUY | Conduct of operations/experiments; final manuscript approval |
| SS | Manuscript writing and critical review of its contents; final manuscript approval |
| MS | Study conception and design; final manuscript approval |
Footnotes
This study was carried out at the Department of Cardiovascular Surgery, Canakkale Onsekiz Mart University, School of Medicine Canakkale, Turkey.
No financial support.
REFERENCES
- 1.Milano CA, Kesler K, Archibald N, Sexton DJ, Jones RH. Mediastinitis after coronary artery bypass graft surgery. Risk factors and long-term survival. Circulation. 1995;92(8):2245–2251. doi: 10.1161/01.cir.92.8.2245. [DOI] [PubMed] [Google Scholar]
- 2.Loop FD, Lytle BW, Cosgrove DM, Mahfood S, McHenry MC, Goormastic M, et al. Sternal wound complications after isolated coronary artery bypass grafting: early and late mortality, morbidity, and cost of care. Ann Thorac Surg. 1990;49:179–187. doi: 10.1016/0003-4975(90)90136-t. [DOI] [PubMed] [Google Scholar]
- 3.Kappstein I, Schulgen G, Fraedrich G, Schlosser V, Schumacher M, Daschner FD. Added hospital stay due to wound infections following cardiac surgery. Thorac Cardiovasc Surg. 1992;40(3):148–151. doi: 10.1055/s-2007-1020134. [DOI] [PubMed] [Google Scholar]
- 4.Sá MP, Silva DO, Lima EN, Lima RC, Silva FP, Rueda FG, et al. Postoperative mediastinitis in cardiovascular surgery postoperations. Analysis of 1038 consecutive surgeries. Rev Bras Cir Cardiovasc. 2010;25(1):19–24. [PubMed] [Google Scholar]
- 5.Gardlund B, Bitkover CY, Vaage J. Postoperative mediastinitis in cardiac surgery: microbiology and pathogenesis. Eur J Cardiothorac Surg. 2002;21(5):825–830. doi: 10.1016/s1010-7940(02)00084-2. [DOI] [PubMed] [Google Scholar]
- 6.Arruda MV, Braile DM, Joaquim MR, Suzuki FA, Alves RH. The use of the vancomycin paste for sternal hemostasis and mediastinitis prophylaxis. Rev Bras Cir Cardiovasc. 2008;23(1):35–39. doi: 10.1590/s0102-76382008000100007. [DOI] [PubMed] [Google Scholar]
- 7.Sá MP, Soares EF, Santos CA, Figueiredo OJ, Lima RO, Escobar RR, et al. Skelotenized left internal thoracic artery is associated with lower rates of mediastinitis in diabetic patients. Rev Bras Cir Cardiovasc. 2011;26(2):183–189. doi: 10.1590/s0102-76382011000200007. [DOI] [PubMed] [Google Scholar]
- 8.Calvat S, Trouillet JL, Nataf P, Vuagnat A, Chastre J, Gibert C. Closed drainage using Redon catheters for local treatment of poststernotomy mediastinitis. Ann Thorac Surg. 1996;61(1):195–201. doi: 10.1016/0003-4975(95)00921-3. [DOI] [PubMed] [Google Scholar]
- 9.Rupp ME. Mediastinitis. In: Mandell GL, Bennet JE, Dolin R, editors. Principles and practice of infectious diseases. 6th ed. Philadelphia: Elsevier Churchill Livingstone; 2005. pp. 1070–1078. [Google Scholar]
- 10.Traber PG, Levine DP. Vancomycin ototoxicity in patient with normal renal function. Ann Intern Med. 1981;95(4):458–460. doi: 10.7326/0003-4819-95-4-458. [DOI] [PubMed] [Google Scholar]
- 11.Turhan V, Sacar S, Uzun G, Sacar M, Yildiz S, Ceran N, et al. Hyperbaric oxygen as adjunctive therapy in experimental mediastinitis. J Surg Res. 2009;155(1):111–115. doi: 10.1016/j.jss.2008.08.031. [DOI] [PubMed] [Google Scholar]
- 12.Namdari H, Tan T, Dowzicky Y. Activity of tigecycline and comparators against skin and skin structure pathogens: global results of the Tigecycline Evaluation and Surveillance Trial, 20042009. Int J Infect Dis. 2012;16(1):e60–e66. doi: 10.1016/j.ijid.2011.09.021. [DOI] [PubMed] [Google Scholar]
- 13.Puzniak LA, Quintana A, Wible M, Babinchak T, McGovern PC. Methicillin-resistant Staphylococcus aureus infection epidemiology and clinical response from tigecycline soft tissue infection trials. Diagn Microbiol Infect Dis. 2014;79(2):261–265. doi: 10.1016/j.diagmicrobio.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 14.Tarai B, Das P, Kumar D. Recurrent challenges for clinicians: emergence of methicillin-resistant Staphylococcus aureus, vancomycin resistance, and current treatment options. J Lab Physicians. 2013;5(2):71–78. doi: 10.4103/0974-2727.119843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Antonopoulou A, Tsaganos T, Tzepi IM, Giamarellou H, Giamarellos-Bourboulis EJ. Comparative efficacy of tigecycline VERSUS vancomycin in an experimental model of soft tissue infection by methicillin-resistant Staphylococcus aureus producing Panton-Valentine leukocidin. J Chemother. 2015;27(2):80–86. doi: 10.1179/1973947814Y.0000000171. [DOI] [PubMed] [Google Scholar]
- 16.Egito JG, Abboud CS, Oliveira AP, Máximo CA, Montenegro CM, Amato VL, et al. Clinical evolution of mediastinitis in patients undergoing adjuvant hyperbaric oxygen therapy after coronary artery bypass surgery. Einstein. 2013;11(3):345–349. doi: 10.1590/S1679-45082013000300014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Institute of Laboratory Animal Resources National Research Council: Guide for the care and use of laboratory animals. Washington: National Academy Press; 1996. [Google Scholar]
- 18.Ersoz G, Aytacoglu BN, Sucu N, Tamer L, Bayindir I, Kose N, et al. Comparison and evaluation of experimental mediastinitis models: precolonized foreign body implants and bacterial suspension inoculation seems promising. BMC Infect Dis. 2006;6:76–76. doi: 10.1186/1471-2334-6-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sacar M, Sacar S, Kaleli I, Cevahir N, Teke Z, Kavas ST, et al. Efficacy of linezolid in the treatment of mediastinitis due to methicillinresistant Staphylococcus aureus: an experimental study. Int J Infect Dis. 2008;12(4):396–401. doi: 10.1016/j.ijid.2007.09.017. [DOI] [PubMed] [Google Scholar]
- 20.Oguz E, Ekinci S, Eroglu M, Bilgic S, Koca K, Durusu M, et al. Evaluation and comparison of the effects of hyperbaric oxygen and ozonized oxygen as adjuvant treatments in an experimental osteomyelitis model. J Surg Res. 2011;171(1):e61–e68. doi: 10.1016/j.jss.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 21.Turhan V, Sacar S, Uzun G. Hyperbaric oxygen as adjunctive therapy in experimental mediastinitis. J Surg Res. 2009;155(1):111–115. doi: 10.1016/j.jss.2008.08.031. [DOI] [PubMed] [Google Scholar]
- 22.Ozcan AV, Demir M, Onem G, Goksin I, Baltalarli A, Topkara VK, et al. Topical versus systemic vancomycin for deep sternal wound infection caused by methicillin-resistant Staphylococcus aureus in a rodent experimental model. Tex Heart Inst J. 2006;33(2):107–110. [PMC free article] [PubMed] [Google Scholar]
- 23.Peterson LR. A review of tigecycline-the first glycylcycline. Int J Antimicrob Agents. 2008;32(Suppl 4):S215–S222. doi: 10.1016/S0924-8579(09)70005-6. [DOI] [PubMed] [Google Scholar]
- 24.Livermore DM. Tigecycline: what is it, and where should it be used? J Antimicrob Chemother. 2005;56(4):611–614. doi: 10.1093/jac/dki291. [DOI] [PubMed] [Google Scholar]
- 25.MacGowan AP. Tigecycline pharmacokinetic/pharmacodynamic update. J Antimicrob Chemother. 2008;62(Suppl 1):i11–i16. doi: 10.1093/jac/dkn242. [DOI] [PubMed] [Google Scholar]
- 26.Zimmerman JJ, Harper DM, Matschke K, Speth JL, Raible DG, Fruncillo RJ. Absence of an interaction between tigecycline and digoxin in healthy men. Pharmacotherapy. 2007;27(6):835–844. doi: 10.1592/phco.27.6.835. [DOI] [PubMed] [Google Scholar]
- 27.Zimmerman JJ, Raible DG, Harper DM, Matschke K, Speth JL. Evaluation of a potential tigecycline warfarin drug interaction. Pharmacotherapy. 2008;28(7):895–905. doi: 10.1592/phco.28.7.895. [DOI] [PubMed] [Google Scholar]
- 28.Ellis-Grosse EJ, Babinchak T, Dartois N, Rose G, Loh E, Tigecycline 300 cSSSI Study Group. Tigecycline 305 cSSSI Study Group The efficacy and safety of tigecycline in the treatment of skin and skin-structure infections: results of 2 double-blind phase 3 comparison studies with vancomycin-aztreonam. Clin Infect Dis. 2005;41(Suppl 5):S341–S353. doi: 10.1086/431675. [DOI] [PubMed] [Google Scholar]
- 29.Unai S, Miessau J, Karbowski P, Bajwa G, Hirose H. Sternal wound infection caused by Mycobacterium chelonae. J Card Surg. 2013;28(6):687–692. doi: 10.1111/jocs.12194. [DOI] [PubMed] [Google Scholar]
- 30.Tekçe AY, Erbay A, Çabadak H, Yagci S, Karabiber N, Sen S. Pan-resistant Acinetobacter baumannii mediastinitis treated successfully with tigecycline: a case report. Surg Infect (Larchmt) 2011;12(2):141–143. doi: 10.1089/sur.2009.063. [DOI] [PubMed] [Google Scholar]
- 31.Evagelopoulou P, Myrianthefs P, Markogiannakis A, Baltopoulos G, Tsakris A. Multidrug-resistant Klebsiella pneumoniae mediastinitis safely and effectively treated with prolonged administration of tigecycline. Clin Infect Dis. 2008;46(12):1932–1933. doi: 10.1086/588557. [DOI] [PubMed] [Google Scholar]
- 32.Mangin O, Urien S, Mainardi JL, Fagon JY, Faisy C. Vancomycin pharmacokinetic and pharmacodynamic models for critically ill patients with post-sternotomy mediastinitis. Clin Pharmacokinet. 2014;53(9):849–861. doi: 10.1007/s40262-014-0164-z. [DOI] [PubMed] [Google Scholar]
- 33.Contreiras C, Legal M, Lau TT, Thalakada R, Shalansky S, Ensom MH. Identification of risk factors for nephrotoxicity in patients receiving extended-duration, high-trough vancomycin therapy. Can J Hosp Pharm. 2014;67(2):126–132. doi: 10.4212/cjhp.v67i2.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barnea Y, Navon-Venezia S, Kuzmenko B, Artzi N, Carmeli Y. Ceftobiprole medocaril is an effective treatment against methicillinresistant Staphylococcus aureus (MRSA) mediastinitis in a rat model. Eur J Clin Microbiol Infect Dis. 2014;33(3):325–329. doi: 10.1007/s10096-013-1959-9. [DOI] [PubMed] [Google Scholar]
- 35.Yokoe DS, Mermel LA, Anderson DJ, Arias KM, Burstin H, Calfee DP, et al. A compendium of strategies to prevent healthcare-associated infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29(Suppl 1):S12–S21. doi: 10.1086/591060. [DOI] [PubMed] [Google Scholar]
- 36.Tibbles PM, Edelsberg JS. Hyperbaric-oxygen therapy. N Engl J Med. 1996;334(25):1642–1648. doi: 10.1056/NEJM199606203342506. [DOI] [PubMed] [Google Scholar]
- 37.Cimsit M, Uzun G, Yildiz S. Hyperbaric oxygen therapy as an anti-infective agent. Expert Rev Anti Infect Ther. 2009;7(8):1015–1026. doi: 10.1586/eri.09.76. [DOI] [PubMed] [Google Scholar]
- 38.Hunt TK, Pai MP. The effect of varying ambient oxygen tensions on wound metabolism and collagen synthesis. Surg Gynecol Obstet. 1972;135(4):561–567. [PubMed] [Google Scholar]
- 39.Fujita N, Ono M, Tomioka T, Deie M. Effects of hyperbaric oxygen at 1.25 atmospheres absolute with normal air on macrophage number and infiltration during rat skeletal muscle regeneration. PLoS One. 2014;9(12): doi: 10.1371/journal.pone.0115685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brismar K, Lind F, Kratz G. Dose-dependent hyperbaric oxygen stimulation of human fibroblast proliferation. Wound Repair Regen. 1997;5(2):147–150. doi: 10.1046/j.1524-475X.1997.50206.x. [DOI] [PubMed] [Google Scholar]
- 41.Kang TS, Gorti GK, Quan SY, Ho M, Koch RJ. Effect of hyperbaric oxygen on the growth factor profile of fibroblasts. Arch Facial Plast Surg. 2004;6(1):31–35. doi: 10.1001/archfaci.6.1.31. [DOI] [PubMed] [Google Scholar]
- 42.Zhao LL, Davidson JD, Wee SC, Roth SI, Mustoe TA. Effect of hyperbaric oxygen and growth factors on rabbit ear ischemic ulcers. Arch Surg. 1994;129(10):1043–1049. doi: 10.1001/archsurg.1994.01420340057010. [DOI] [PubMed] [Google Scholar]
- 43.Sheikh AY, Gibson JJ, Rollins MD, Hopf HW, Hussain Z, Hunt TK. Effect of hyperoxia on vascular endothelial growth factor levels in a wound model. Arch Surg. 2000;135(11):1293–1297. doi: 10.1001/archsurg.135.11.1293. [DOI] [PubMed] [Google Scholar]
- 44.Sunkari VG, Lind F, Botusan IR, Kashif A, Liu ZJ, Ylä-Herttuala S, et al. Hyperbaric oxygen therapy activates hypoxia-inducible factor 1 (HIF-1), which contributes to improved wound healing in diabetic mice. Wound Repair Regen. 2015;23(1):98–103. doi: 10.1111/wrr.12253. [DOI] [PubMed] [Google Scholar]
- 45.Hopf HW, Holm J. Hyperoxia and infection. Best Pract Res Clin Anaesthesiol. 2008;22(3):553–569. doi: 10.1016/j.bpa.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 46.Park MK, Muhvich KH, Myers RA, Marzella L. Hyperoxia prolongs the aminoglycoside-induced postantibiotic effect in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1991;35(4):691–695. doi: 10.1128/aac.35.4.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hassan HM, Fridovich I. Superoxide radical and the oxygen enhancement of the toxicity of paraquat in Escherichia coli. J Biol Chem. 1978;253(22):8143–8148. [PubMed] [Google Scholar]
- 48.Knighton DR, Silver IA, Hunt TK. Regulation of wound-healing angiogenesis-effect of oxygen gradients and inspired oxygen concentration. Surgery. 1981;90(2):262–270. [PubMed] [Google Scholar]
- 49.Mader JT, Shirtliff ME, Bergquist SC, Calhoun J. Antimicrobial treatment of chronic osteomyelitis. Clin Orthop Relat Res. 1999;(360):47–65. doi: 10.1097/00003086-199903000-00008. [DOI] [PubMed] [Google Scholar]
- 50.Topuz K, Kutlay AM, Simsek H, Colak A, Kaya S, Demircan MN. Effect of hyperbaric oxygen therapy on the duration of treatment of spinal tuberculosis. J Clin Neurosci. 2009;16(12):1572–1577. doi: 10.1016/j.jocn.2009.02.040. [DOI] [PubMed] [Google Scholar]


