Abstract
Background:
In selected inpatient settings, penicillin skin testing has been shown to affect antibiotic use. Routine penicillin skin testing has not been studied in hospitalized patients with a history of penicillin allergy.
Objectives:
To determine whether routine penicillin skin testing at a large regional hospital affected antibiotic use and/or antibiotic side effects in hospitalized persons with a history of penicillin allergy.
Methods:
A convenience sample of patients was penicillin skin tested from among those who had a history of penicillin allergy during any hospitalization from September 2002 through February 2003. Discharge coding was used to identify two age- and sex-matched control patients who had a history of penicillin allergy but who did not receive skin testing while hospitalized. All inpatient and outpatient antibiotic use, positive results of bacteriology culture obtained at any time from August 2002 through March 2003, and coded adverse reactions to medications were identified.
Results:
Of the 13,172 patients admitted to the hospital during the study period, 1627 (12.35%) had a history of penicillin allergy; of these 1627 patients, 141 (8.7%) received skin testing. Use of antibiotic agents was common: 79.4% of all study subjects received at least one antibiotic agent. Penicillins were used in substantially more cases than controls. Cephalosporins were the most widely used class of antibiotic agents, accounting for 26.8% of all antibiotic courses used. Of the six antibiotic-associated adverse drug reactions in five (1.2%) of the study subjects, one adverse reaction was associated with a penicillin, and one was associated with a cephalosporin.
Conclusions:
Routine penicillin skin testing in hospitalized patients is safe and allows more appropriate antibiotic use. To ensure that accurate information is available to support clinical care, hospitals should maintain a single centralized system for collecting data on drug allergy and testing.
Introduction
The effect of penicillin skin testing on antibiotic use in unselected hospitalized adults with a history of penicillin allergy has not been directly studied.
At Kaiser Permanente Medical Center in San Diego, we previously showed that penicillin skin testing among outpatients reduces both antibiotic use and costs in the year after testing compared with the year before testing.1 The present study was undertaken to determine whether routine penicillin skin testing at our large regional hospital affected use of antibiotic agents and/or side effects associated with antibiotic agents in hospitalized persons with a history of penicillin allergy.
Methods
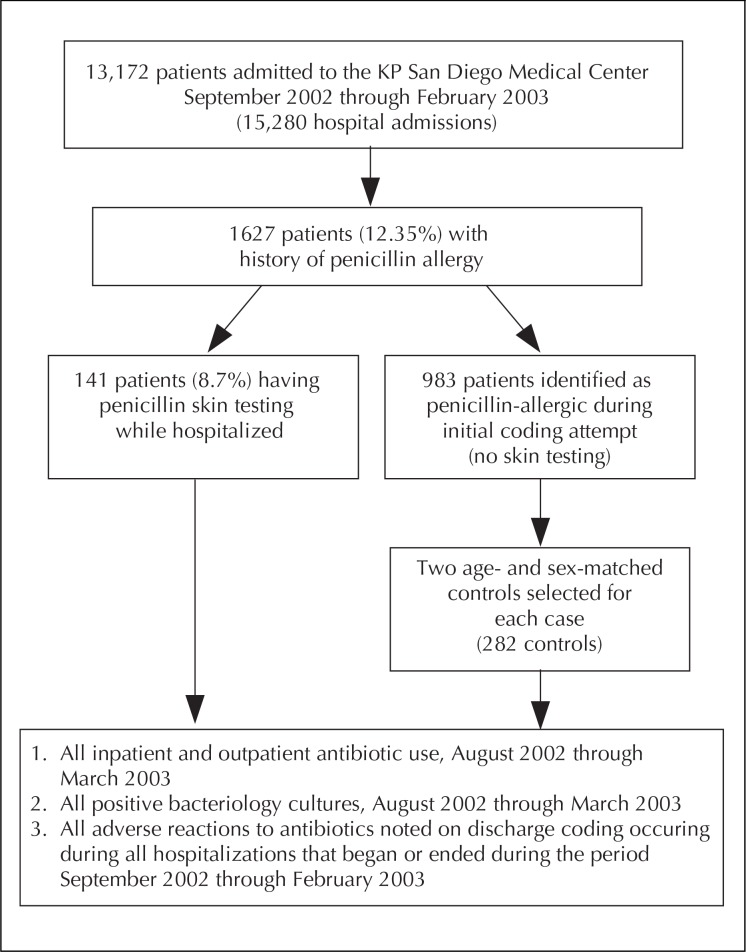
An overview of the study design is presented in Figure 1. Hospital personnel identified general medical and surgical adult patients who carried a history of penicillin allergy during the study period September 2002 through February 2003. A nurse from the allergy department regularly circulated throughout the hospital and administered penicillin skin testing. The nurse skin-tested as many patients as possible from among those who had a history of penicillin allergy, were available for testing, were not taking antihistamines or beta-blockers, and agreed to the testing. Penicillin skin testing was performed as previously described using a complete panel of reagents, including native penicillin, native amoxicillin, Pre-Pen®, penilloate, and penicilloate.2 A total 141 patients were tested. Pregnant women with a history of penicillin allergy and positive cultures for group B streptococcus or pediatric patients are commonly tested as outpatients in the allergy department and are tested as inpatients only if specifically requested by their attending physicians. Hospitalized pediatric patients and obstetric patients were not targeted as part of this program. Because of the theoretical risk of amplification of a rare systemic reaction from the penicillin skin test, patients taking beta-blockers were not tested in the hospital. However, patients receiving beta-blockers are routinely given penicillin skin tests as outpatients in the allergy department. Patients who were identified as potential candidates for skin testing were given an explanation of the risks and benefits of penicillin skin testing by the allergy department nurse and were allowed to refuse the test. All patients gave their written informed consent before they were tested. The study was reviewed and approved by the Kaiser Permanente Southern California Institutional Review Board.
Figure 1.
Flowchart illustrates study design for determining whether routine penicillin skin testing in hospitalized patients with history of penicillin allergy affected their use of antibiotic drugs, side effects of these drugs, or both
Initial discharge coding was used to identify a total 1041 control patients who had a history of penicillin allergy and who were not penicillin skin-tested during any hospitalization during the study period, September 2002 through February 2003. Discharge coders had been instructed to code for a history of penicillin allergy if present at discharge and to code for any penicillin skin testing that was done during any hospitalization while the study was in progress. Because only 7.9% of the 13,172 patients admitted to the hospital 15,280 times between September 1, 2002, and February 28, 2003, were initially coded for penicillin allergy, a random sample of 332 individuals was recoded. Of the 332 patients in this second sample, 41 (12.35%) had a history of penicillin allergy. Extrapolation based on this random sample led us to estimate that 1627 (12.35%) of the 13,172 hospitalized patients had a history of penicillin allergy. Of these 1627 patients, 141 (8.7%) were tested during at least one hospital stay during the study.
Accuracy of coding related to penicillin allergy among cases and controls was evaluated. Of the 1041 patients initially identified by discharge coding as having a history of being penicillin-allergic, 58 (5.6%) were erroneously coded. These 58 patients had a negative penicillin skin test during a hospital stay during the study and thus should not have been coded as penicillin-allergic. Two age- and sex-matched controls were selected for each of the 141 cases from the remaining 983. Further review determined that 10 (3.5%) of the control patients selected also had previous negative penicillin skin tests as outpatients between March 28, 1996 and June 21, 2002, although at their index admission, discharge coders still interpreted these patients as allergic to penicillin. As of September 8, 2003, 2099 San Diego area patients with a history of penicillin allergy had been tested since 1994; of these 2099 patients, 429 (20.4%) were tested while in the hospital.
All inpatient and outpatient antibiotic use and positive bacteriology cultures occurring between August 1, 2002, and March 31, 2003, were obtained from electronic databases for case and control patients. The follow-up period for antibiotic use and bacteriology cultures was extended one month on either side of the six-month in-hospital testing period to capture data from any prolonged hospital stay or from discharge therapy programs that extended into or beyond the testing period. Downloading usable sensitivity data on the positive bacteriology cultures was not possible.
Statistical comparison of two-way data was made by χ-square analysis. Summary measures of independent groups were evaluated by independent group t test. Significance was established at p < 0.05.
Results
Demographics of Matched Cases and Controls
The study population included more females than males (Table 1). A total 592 admissions of the 423 study subjects of one or more days accounted for 2645 total hospital days. Multiple admission frequency for study patients was significantly greater than among the remaining 12,749 patients admitted during this period (p = 0.0029).
Table 1.
Demographics of study subjects
| Cases (n = 141) | Controls (n = 282) | |
|---|---|---|
| Total (%) | 33.3% | 66.7% |
| Female sex (%) | 94 (66.7%) | 188 (66.7%) |
| Age (year) at index discharge or at penicillin skin test (mean – SD) | 63.7 – 16.1 | 62.3 – 16.5 |
| No. of years since index adverse reaction to penicillin (mean – SD) | 33.3 – 16.1 | Not available |
| Hospital stay >0 days during period September 2002 through February 2003 (percentage of total no. of admissions) | 214 (36.1%) | 378 (63.8%) |
| Mean hospital days during period September 2002 through February 2003 | 6.6 – 6.4 | 6.1 – 9.6 |
| Patients with any antibiotic use during period August 2002 through March 2003 (%) | 116 (82.2%) | 220 (78.0%) |
| Mean no. of antibiotic courses per study subject during period August 2002 through March 2003 | 5.16a | 3.87a |
p = 0.0112
Accuracy of Coding
Only 60 (42.5%) of the 141 cases were accurately coded as having had a penicillin skin test during any hospital stay. Twenty-three (16.3%) cases were not coded for either history of penicillin allergy or penicillin skin testing. Fifty control patients had at least two admissions of two or more days during the study period. With perfect coding, 105 of these admissions would have been coded for a history of penicillin allergy. Three of the control patients actually had previous negative penicillin skin tests as out-patients. These three patients accounted for six additional admissions and none of these six admissions should have been coded for penicillin allergy history. Thus, of 111 total multi-day admissions for these 50 control patients, 36 (32.4%) were miscoded. This value is close to the calculated error rate seen in initial control identification: 1627 calculated minus 1041 coded equals 586 (36%) missed.
Results of Penicillin Skin Testing
Only eight (5.5%) of the patients had skin tests positive for penicillin allergy. All ten of the controls who had previously tested negative for penicillin allergy had negative tests. Of the 141 patients tested in the hospital, no penicillin skin test was associated with adverse reactions.
Use of Antibiotic Agents
Antibiotic use was common in 116 (82.2%) of the case and 220 (78%) of the control patients receiving at least one antibiotic during the eight-month follow-up period (p = 0.3074). The entire cohort received 1820 courses of antibiotics: a mean 5.4 courses of antibiotics per subject who received any antibiotics, or a mean 4.3 courses for all subjects. Cases used significantly more courses of antibiotics than control patients: 728 (5.16 per case) versus 1092 (3.87 per control) (p = 0.0112).
Use of Penicillin
Penicillins were used by significantly more case than control patients: 24 (17.0%) of 141 case compared with 20 (7.1%) of 282 control patients (p = 0.0016). Fifty-seven courses of penicillin, representing 3.1% of all antibiotic courses used, were used by the entire cohort. Penicillins accounted for a significantly higher fraction of total antibiotic courses in cases than in control patients: 29 (4.0%) versus 28 (2.6%) (p < 0.0001). Specific penicillin exposures are shown in Table 2.
Table 2.
Type and extent of exposure to penicillin among cases and controlsa
| Exposed/courses | ||
|---|---|---|
| Cases | Controls | |
| Ampicillin, intravenous | 5/5 | 9/9 |
| Ampicillin, oral | 2/2 | |
| Amoxicillin, oral | 12/14 | 7/10 |
| Augmentin®, oral | 8/8 | 4/5 |
| Dicloxicillin, oral | 1/1 | |
| Oxacillin, intravenous | 1/1 | |
| Penicillin, intravenous | 1/1 | |
| Penicillin, oral | 1/1 | |
| Total cases exposed/total courses used | 24b/29c | 20a/28c |
Some case and control patients were exposed to more than one type of penicillin.
p = 0.0016
p < 0.0001
One penicillin-associated adverse drug reaction to ampicillin was reported in a control patient admitted to the hospital late in 2002. When the patient received ampicillin, she did not have a history of penicillin allergy but was readmitted early in 2003 and became a control based on that admission. One control patient who received both intravenous (IV) and oral ampicillin had skin testing negative to penicillin in late June 2002 as an outpatient but still carried a “history” of penicillin allergy as captured by the discharge coders.
Use of Cephalosporins
Cephalosporins were used by significantly more cases than control patients: 199 courses by 83 (58.9%) cases, and 288 courses by 136 (48.2%) control patients (p = 0.0390). As a fraction of total antibiotic courses used, we saw no significant difference: 199 (27.3%) of 728 compared with 288 (26.3%) of 1092 (p = 0.206).
One control patient had a reaction associated with ceftazidime, but this reaction occurred during the second course of ceftazidime received during the follow-up period. He also tolerated four other different cephalosporins during the follow-up period, was taking a quinoline at the same time as the ceftazidime-associated reaction, and was coded as reacting to both. Three cases positive to penicillin skin testing received nine courses of cephalosporins, and all received at least one IV course without any adverse reaction. Cephalosporins were the most commonly used antibiotic class in the cohort and accounted for 26.8% of all antibiotic courses used. Quinolones accounted for 25.3% of all antibiotic courses.
Use of Vancomycin
Sixty-three vancomycin courses were used in 48 (14.3%) patients. Vancomycin only accounted for 3.5% of all antibiotic courses used. The 19 cases received 24 courses, or a mean 6.68 days of vancomycin per patient exposed. The 29 control patients received 39 courses, or a mean 6.52 days of vancomycin per patient exposed. Penicillin skin testing had no discernible effect on vancomycin use, but vancomycin use was initially low.
Adverse Reactions to Antibiotics Based on Discharge Coding
One penicillin, one cephalosporin, one quinolone, two macrolides, and one unspecified antibiotic reaction were coded for five (1.2%) patients among 58 adverse drug reactions coded for 42 (9.9%) patients from the cohort of 423. One of the macrolide reactions occurred in one case. All other reactions occurred in control patients.
Results of Bacteriology Culture
Positive bacteriology cultures were obtained from 47 (33.1%) cases and 74 (26.2%) control patients, (p = 0.26, NS). Fourteen patients had MRSA-positive cultures. Five received vancomycin; one, linezolid and vancomycin; four, clindamycin; and four others, combinations of ciprofloxacin, metronidazole, sulfamethoxazole, gentamicin, ceftazidime, cefazolin, and cefizoxime. Of three patients who received vancomycin for MSRA and penicillin skin testing, one tested positive. Only four patients received any linezolid.
Discussion
To date, overall beneficial effects of routine penicillin skin testing on antibiotic use have not been determined directly among hospitalized patients with a history of penicillin allergy. In orthopedic patients at the Mayo Clinic, penicillin skin testing reduced vancomycin use from 30% of patients to 11%.3 At the Cleveland Clinic, a pilot study of prospective penicillin skin testing for patients with a history of penicillin allergy who were admitted to the medical ICU resulted in change in antibiotic use by ten (48%) of 21 patients tested.4 A study on antibiotic use and costs in patients with a history of penicillin allergy at the Tel Aviv Sourasky Medical Center showed that the mean antibiotic cost was 63% higher in the hospital and 38% higher for postdischarge therapy compared with controls who had no history of penicillin allergy;5 however, no penicillin skin testing was done in that study. A program to increase the use of penicillin skin testing at St Paul’s Hospital in British Columbia increased penicillin use without increase in total cost.6
A total of 18 (6.4%) control patients received an inappropriate penicillin based on medical history. Fortunately there were no significant adverse outcomes associated with errant penicillin exposure based on discharge coding. No patients with positive penicillin skin tests were re-exposed to penicillins.
Conclusions
Patients who carry a history of penicillin allergy are more likely to have multiple hospital admissions than randomly selected patients. Patients with a history of penicillin allergy are given numerous courses of antibiotics. Specific antibiotic use does not appear to be driven by positive bacteriology cultures but appears to be empirical. Patients with a history of penicillin allergy commonly receive multiple courses of similar antibiotics.
Penicillin skin testing of patients while they are in the hospital is associated with more penicillin and cephalosporin use. Continuing this penicillin skin testing program will enable more appropriate use of antibiotics in our hospitalized patients.
Cephalosporins are widely, safely, and appropriately used in patients with a history of penicillin allergy independent of penicillin skin test status.7 To date, we have identified nine patients with positive results of a penicillin skin test who have tolerated parenteral cephalosporins, including the three identified during this project.
Our analysis shows that drug allergy and intolerance information does not appear to be managed consistently in the currently used hospital medical record system. A history of penicillin allergy is often both erroneously coded or apparently ignored. Patients who prove not allergic to penicillin on the basis of recent negative results of penicillin skin testing are identified as allergic to penicillin. Patients identified as allergic to penicillin are given the penicillin class of antibiotics. Fortunately, only a fraction of people who carry a history of penicillin allergy have clinically significant penicillin allergy and few experience life-threatening reactions when re-exposed to penicillins.
A single centralized system of collecting drug allergy and intolerance data is needed and should be linked to drug distribution and allergy testing. The logical repository for this electronic database would be the pharmacy until the electronic hospital medical record becomes functional.
Acknowledgments
The research was funded by a Southern California Permanente Medical Group Innovation grant.
Elwyn A Garrard, PharmD, Gene Chiu, PharmD, Calvin T Togashi, PharmD, and Charles C Lino, PharmD, provided the antibiotic use data; Jose-Luis Romero, the bacteriology culture data; and Esther Straus, MLIS, RHIA, CCC, general medical record data. Raoul J Burchette, MA, MS, assisted with data analysis.
Biographies
Eric Macy, MD, works in the Department of Allergy in the San Diego Medical Center, as well as being a Partner Physician with the Southern California Permanente Medical Group, and an Assistant Clinical Professor of Medicine at the University of California, San Diego. E-mail: eric.m.macy@kp.org.

Linda B Roppe RN, BSN, is an Ambulatory Care Nursing Coordinator for the Allergy Department, SCPMG San Diego. E-mail: linda.b.roppe@kp.org.

Michael Schatz, MD, MS, has been at KP for 25 years and is Chief of the Department of Allergy in San Diego. He is also Clinical Professor in the Department of Medicine, University of California San Diego School of Medicine and President of the American Academy of Allergy Asthma and Immunology. E-mail: michael.x.schatz@kp.org.

The Giant Sequoia Tree
What is the purpose of the giant sequoia tree?
The purpose of the giant sequoia tree is to provide shade for the tiny titmouse.
— Edward Abbey, 1927–1989, naturalist and author
References
- 1.Macy E. Elective penicillin skin testing and amoxicillin challenge: effect on outpatient antibiotic use, cost, and clinical outcomes. J Allergy Clin Immunol. 1998 Aug;102(2):281–5. doi: 10.1016/s0091-6749(98)70097-1. [DOI] [PubMed] [Google Scholar]
- 2.Macy E, Richter PK, Falkoff R, Zeiger R. Skin testing with penicilloate and penilloate prepared by an improved method: amoxicillin oral challenge in patients with negative skin test responses to penicillin reagents. J Allergy Clin Immunol. 1997 Nov;100(5):586–91. doi: 10.1016/s0091-6749(97)70159-3. [DOI] [PubMed] [Google Scholar]
- 3.Li JT, Markus PJ, Osmon DR, Estes L, Gosselin VA, Hanssen AD. Reduction of vancomycin use in orthopedic patients with a history of antibiotic allergy. Mayo Clin Proc. 2000 Sep;75(9):902–6. doi: 10.4065/75.9.902. [DOI] [PubMed] [Google Scholar]
- 4.Arroliga ME, Wagner W, Bobek MB, Hoffman-Hogg L, Gordon SM, Arroliga AC. A pilot study of penicillin skin testing in patients with a history of penicillin allergy admitted to a medical ICU. Chest. 2000 Oct;118(4):1106–8. doi: 10.1378/chest.118.4.1106. [DOI] [PubMed] [Google Scholar]
- 5.Sade K, Holtzer I, Levo Y, Kivity S. The economic burden of antibiotic treatment of penicillin-allergic patients in internal medicine wards of a general tertiary care hospital. Clin Exp Allergy. 2003 Apr;33(4):501–6. doi: 10.1046/j.1365-2222.2003.01638.x. [DOI] [PubMed] [Google Scholar]
- 6.Forrest DM, Schellenberg RR, Thien VV, King S, Anis AH, Dodek PM. Introduction of a practice guideline for penicillin skin testing improves the appropriateness of antibiotic therapy. Clin Infect Dis. 2001 Jun 15;32(12):1685–90. doi: 10.1086/320752. Epub 2001 May 21. [DOI] [PubMed] [Google Scholar]
- 7.Novalbos A, Sastre J, Cuesta J, et al. Lack of allergic cross-reactivity to cephalosporins among patients allergic to penicillins. Clin Exp Allergy. 2001 Mar;31(3):438–43. doi: 10.1046/j.1365-2222.2001.00992.x. [DOI] [PubMed] [Google Scholar]