Abstract
Objective:
We examined the relation between eight types of adverse childhood experience (ACE) and three indicators of impaired worker performance (serious job problems, financial problems, and absenteeism).
Methods:
We analyzed data collected for the Adverse Childhood Experiences Study from 9633 currently employed adult members of the Kaiser Foundation Health Plan in San Diego.
Results:
Strong graded relations were found between the ACE Score (total number of ACE categories experienced) and each measure of impaired worker performance (p < .001). We found strong evidence that the relation between ACE Score and worker performance was mediated by interpersonal relationship problems, emotional distress, somatic symptoms, and substance abuse.
Conclusions:
The long-term effects of adverse childhood experiences on the workforce impose major human and economic costs that are preventable. These costs merit attention from the business community in conjunction with specialists in occupational medicine and public health.
The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition.
—Constitution of the World Health Organization1
Job performance can be affected by personal factors other than knowledge and skills. Indeed, the complexity and team interaction inherent in many current jobs have increased the importance of personal and interpersonal factors in the workplace. For this reason, modern employee assistance programs offer help for emotional, family, and marital problems as well as for substance abuse and financial stress.2,3 Poor interpersonal skills, emotional distress, frequent somatic symptoms, and substance abuse all can reduce worker performance.
In addition to being intrinsically related to individual and public health, these factors affect business profitability and even national productivity.4 Chronic back pain in the workforce is estimated to cost US businesses as much as $28 billion per year;5 depression and its work-related outcomes—absenteeism, reduced productivity, and medical expenses—are estimated to cost as much as $44 billion per year;6 and chemical dependency is estimated to cost $246 billion per year.7 These massive losses occur despite existence of workplace safety programs and the most expensive system of medical care in the world.8
In this article, we analyze the ways in which adverse childhood experiences affect several indicators of job performance during adult life. Specifically, we tested the hypothesis that childhood abuse and household dysfunction exert negative long-term effects on three broad-based indicators of worker performance: serious job problems, serious financial problems, and absenteeism. We then assessed how interpersonal relationship problems, emotional distress, somatic symptoms, and substance abuse may act as mediating variables in the relation between adverse childhood experiences and indicators of occupational performance.
Methods
Study Population
To test our hypothesis, we used data from the Adverse Childhood Experiences (ACE) Study, which was designed to assess the effect of adverse childhood experiences on later (adult) health behavior and health outcomes as these types of behavior and outcomes relate to the leading causes of morbidity and mortality in the United States.9–16 The ACE Study is being conducted among adult members of the Kaiser Foundation Health Plan in San Diego, California, which administers standardized biopsychosocial medical evaluation to more than 55,000 adult Health Plan members annually at a specialized clinic, the Health Appraisal Center. Review of medical records showed that 81% of adults who were continuously enrolled in the Health Plan between 1992 and 1995 had visited this clinic. All 13,494 Health Plan members who completed the standardized evaluation at the Health Appraisal Center in August 1995 or in March 1996 were eligible to participate in the ACE Study.9 The ACE Study was approved by the Institutional Review Boards of the Southern California Permanente Medical Group, Emory University, and the National Institutes of Health Office of Protection from Research Risks.
Each Health Plan member who completed the standardized evaluation at the Health Appraisal Center was mailed a study questionnaire. This survey instrument was administered in two rounds (“Waves”). Of the 13,494 adult Health Plan members surveyed in Wave 1, 9508 (70%) responded and were discussed in initial ACE publications.10–13 In Wave 2,9,16 questionnaires were administered to 13,330 adult Health Plan members who completed the standardized evaluation between June 1997 and October 1997; of these 13,330 adults, 8667 (65%) responded. The final ACE Study cohort included 18,175 persons: 9508 questionnaire respondents from Wave 1 and 8667 questionnaire respondents from Wave 2. Thus, the overall response rate was 68% for the 26,824 adult Health Plan members surveyed. We excluded from analysis all 754 respondents who coincidentally underwent standardized evaluation during both survey waves; all 7761 respondents who were unemployed (ie, had neither fulltime nor part-time employment); four respondents who provided incomplete information about their race; and 23 respondents who provided incomplete information about their educational attainment. Thus, the final study cohort included 9633 persons who were employed at the time of the ACE Survey.
Because the ACE Study questionnaire addressed sensitive topics, we compared respondents and nonrespondents to assess possible study bias introduced by nonresponse. For this assessment, we abstracted medical evaluation data for respondents as well as for nonrespondents to the Wave I questionnaire. We found no important differences between respondents and nonrespondents, either in type of health risk behavior (eg, smoking, obesity, substance abuse) or disease history (eg, diabetes, hyper-tension, heart disease, or cancer).17
Defining Adverse Childhood Experiences
All questions about adverse childhood experiences pertained to eight phenomena experienced by respondents during their first 18 years of life. These phenomena included emotional (verbal), physical, and sexual abuse; having a mother or stepmother who was battered at home; having parents who were either separated or divorced from each other during the respondent’s childhood or adolescence; living with a problem drinker, a drug user, or a mentally ill person; having a household member who was imprisoned. Questions for emotional (verbal) and physical abuse and for having a battered mother were obtained from the Conflict Tactics Scales.18 Questions about contact sexual abuse were adapted from the work of Wyatt.19
Emotional Abuse
Respondents were characterized as emotionally abused if they answered “often” or “very often” to either (or both) of the following questions:
“How often did a parent, step-parent, or adult living in your home swear at you, insult you, or put you down?”
“How often did a parent, step-parent, or adult living in your home act in a way that made you afraid that you might be physically hurt?”
Physical Abuse
Respondents were characterized as physically abused if they answered “often” or “very often” to the following question:
“While you were growing up, that is, in your first 18 years of life, how often did a parent, stepparent, or adult living in your home push, grab, slap, or throw something at you?”
An alternative criterion for being defined as physically abused was an answer of “sometimes,” “often,” or “very often” to the following question:
“While you were growing up, that is, in your first 18 years of life, how often did a parent, step-parent, or adult living in your home hit you so hard that you had marks or were injured?”
Sexual Abuse
A respondent was identified as having experienced contact sexual abuse if he or she answered “yes” to any part of the following four-part question:
- During your first 18 years of life, did an adult, relative, family friend, or stranger ever:
- touch or fondle your body in a sexual way?
- have you touch their body in a sexual way?
- attempt to have any type of sexual intercourse with you (oral, anal, or vaginal)? or
- actually have any type of sexual intercourse with you (oral, anal, or vaginal)?
Battered Mother
A respondent was identified as having a battered mother or stepmother if the respondent answered “sometimes,” “often,” or “very often” to one or both parts of the following two-part question:
- While you were growing up in your first 18 years of life, how often did your father (or a step-father) or mother’s boyfriend do any of these things to your mother (or a stepmother):
- push, grab, slap, or throw something at her?
- kick, bite, hit her with a fist, or hit her with something hard?
Alternatively, a respondent was identified as having a battered mother or stepmother if the respondent answered in any way other than “never” to one or both parts of the following two-part question:
- While you were growing up in your first 18 years of life, how often did your father (or a step-father) or mother’s boyfriend do any of these things to your mother (or a stepmother):
- repeatedly hit her over at least a few minutes?
- threaten her with a knife or gun or use a knife or gun to hurt her?
Household Substance Abuse
Respondents were identified as having been exposed to household substance abuse if they responded affirmatively when asked whether they grew up with a problem drinker or alcoholic20 or with anyone who used street drugs.
Mental Illness in Household
Respondents were identified as having been exposed to mental illness if they responded affirmatively to being asked whether anyone in their household had been depressed, mentally ill, or attempted suicide.
Parental Separation or Divorce
A respondent was characterized as having parents who were separated or divorced if the respondent answered “yes” to the question, “Were your parents ever separated or divorced?”
Incarcerated Household Member
A respondent met this criterion if anyone in the respondent’s household had been imprisoned during the respondent’s childhood.
ACE Score
To assess the cumulative effect of adverse childhood experiences, we calculated for each respondent a score ranging from 0 to 8 (the ACE Score), which represented the total number of categories to which the respondent had been exposed.
Indicators of Impaired Worker Performance
The three indicators of impaired worker performance were job problems, financial problems, and absenteeism. Respondents were identified as having impaired worker performance if they answered “yes” to any of the following questions:
Are you currently having serious problems with your job?
Are you currently having serious problems with your finances?
Respondents were also asked how many days of work they missed in the past 30 days because of poor physical health, stress, or feeling depressed. Respondents were characterized as having a problem with absenteeism if they reported having missed two or more days of work during the past 30 days.
Areas of Health and Well-Being
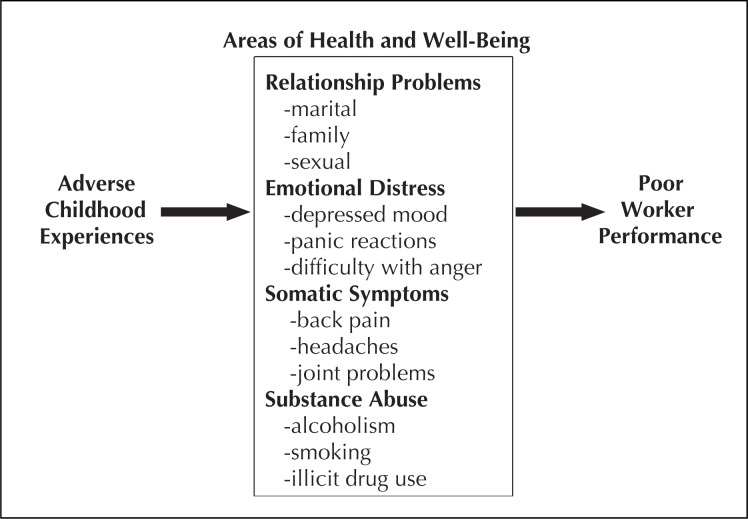
We hypothesized that four selected areas of health and well-being may be intermediate variables that relate adverse childhood experiences to worker performance (Figure 1). We used our clinical judgment on an a priori basis to select three representative problems from each of these four areas of health and well-being. We used factor analysis with orthogonal transformation and a minimal factor loading of 0.4 to determine whether our a priori reasoning about the grouping of the problems was statistically robust. This analysis showed that the four areas of health and well-being that emerged as factors for men matched exactly our a priori areas (eigenvalues >1). The factor structure for women was similar except that among women, depressed mood was a factor associated with relationship problems (eigenvalues >1). Table 1 lists the questions used to define each of the four areas of health and well-being and shows the criteria for a positive response in each area. Respondents who met the criteria for any of the three questions were considered to have a problem in that area of health and well-being.
Figure 1.
Adverse childhood experiences and areas of health and well-being that may affect worker performance
Table 1.
Questions and criteria used to identify Health Plan members with problems in any of four areas of health and well-being
| Problem type | Question | Criterion |
|---|---|---|
| Relationship problems | ||
| Marital problems | “How many times have you been married?” | ≥3 times |
| Family problems | “Are you currently having serious problems with your family?” | Yes |
| Sexual relationships | “Are you currently satisfied with your sex life?” | No |
| Emotional distress | ||
| Depressed affect | “Are you currently having problems with depression or feeling ‘down in the dumps?’ ” | Yes |
| Panic reaction | “In the past year, have you had special circumstances in which you found yourself panicked?” | Yes |
| Anger | “Have you had reason to fear your anger getting out of control?” | Yes |
| Somatic symptoms | ||
| Back pain | “Have you had frequent back pain?” | Yes |
| Headaches | “Have you had frequent headaches?” | Yes |
| Joint pain | “Have you had pain or swelling in your joints?” | Yes |
| Substance abuse | ||
| Alcoholism | “Have you ever considered yourself to be an alcoholic?” | Yes |
| Current Smoker | “Do you currently smoke cigarettes?” | Yes |
| Drug use | “Have you ever used street drugs?” | Yes |
Statistical Analysis
For purposes of analysis, persons for whom incomplete information was available about childhood exposure were considered not to have had that experience. This decision probably biased our results toward the null hypothesis, because persons who might have been exposed to an experience would always be misclassified as unexposed.21 To assess the effect of this decision, we repeated our analyses after excluding respondents with missing information on any exposure. The results of these analyses were nearly identical to those presented herein.
We used logistic regression22 to estimate odds ratios (OR) for the association between three items: childhood exposure to adverse experiences, indicators of impaired worker performance, and response to each question about health and well-being. All models included the respondent’s age, sex, race, and educational attainment.
Assessment of Mediating Effects on Health and Well-Being
We compared the strength of the relation between adverse childhood experiences and indicators of impaired worker performance by using logistic models with and without controlling for potential mediation (ie, by problems in the four areas of health and well-being). To do this comparison, we used an ordinal variable to designate total number of problems from the four areas of health and well-being (range 0–12). We used the term “mediation” in the same way as some researchers use the term “intermediate”; we consider these terms to have the same meaning and to be interchangeable.
Our analyses used the following principle:
A confounding variable must not be an intermediate step in the causal path between the exposure and the disease.
This criterion requires information outside the data. The investigator must decide whether the causal mechanism that might follow from exposure to disease would include the potentially confounding factor as an intermediate step. If so, the variable is not a confounder.21:p94
Figure 1 presents a proposed causal pathway in which four areas of health and well-being are mediating variables. Our analyses treated these areas as potential mediating (or intermediate) variables, as recommended by Rothman.21
Results
Characteristics of Study Population
Mean age of the cohort was 47.9 years (SD +11.7), 51.9% were women, and 68% of the population were white. Forty-six percent were college graduates, 37% had some college, and 4% did not graduate from high school.
Prevalence of Adverse Childhood Experiences
Prevalence of the eight categories of adverse childhood experience is shown in Table 1. Thirty-two percent of respondents reported no exposure to adverse childhood experiences, and 25% of respondents reported exposure to only one category of adverse childhood experience. More than two thirds of respondents were exposed to at least one category of adverse childhood experience; and 43% of respondents reported exposure to two or more categories of adverse childhood experience. Exposure to two categories of adverse childhood experience was reported by 17% of respondents; exposure to three categories, by 11% of respondents; and exposure to four categories, by 15% of respondents.
Childhood Exposure and Indicators of Worker Performance
Job-related problems were reported by 11.5% of the study cohort; financial problems were reported by 15.5%; and absenteeism, by 8.7%. Each of the eight adverse childhood experiences was associated with an increased likelihood of job problems, financial problems, and absenteeism (Table 2).
Table 2.
Relation between adverse childhood experiences and indicators of worker performance
| Category of ACE (%) | (N) | Job problems | Financial problems | Absenteeism | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| % | ORa (95%CI) | % | ORa (95%CI) | % | ORa (95%CI) | ||
|
|
|
|
|
||||
| Abuse during childhood: | |||||||
| Emotional | |||||||
| No (87%) | 8413 | 10.3 | 1.0 (referent) | 14.2 | 1.0 (referent) | 7.8 | 1.0 (referent) |
| Yes (13%) | 1220 | 19.6 | 2.1 (1.8–2.4) | 24.3 | 1.8 (1.6–2.1) | 14.9 | 1.9 (1.6–2.3) |
|
|
|
|
|
||||
| Physical | |||||||
| No (68%) | 6581 | 9.6 | 1.0 (referent) | 13.6 | 1.0 (referent) | 7.3 | 1.0 (referent) |
| Yes (32%) | 3052 | 15.6 | 1.7 (1.5–1.9) | 19.5 | 1.5 (1.3–1.7) | 11.9 | 1.7 (1.5–2.0) |
|
|
|
|
|
||||
| Sexual | |||||||
| No (78%) | 7480 | 10.6 | 1.0 (referent) | 14.0 | 1.0 (referent) | 8.1 | 1.0 (referent) |
| Yes (22%) | 2153 | 14.4 | 1.4 (1.2–1.6) | 20.6 | 1.5 (1.3–1.7) | 10.9 | 1.3 (1.1–1.5) |
|
|
|
|
|
||||
| Household dysfunction: | |||||||
| Battered mother? | |||||||
| No (86%) | 8243 | 11.1 | 1.0 (referent) | 14.8 | 1.0 (referent) | 8.2 | 1.0 (referent) |
| Yes (14%) | 1390 | 14.0 | 1.3 (1.1–1.5) | 19.6 | 1.3 (1.1–1.5) | 11.9 | 1.4 (1.2–1.7) |
|
|
|
|
|
||||
| Substance abuse? | |||||||
| No (68%) | 6562 | 10.3 | 1.0 (referent) | 13.4 | 1.0 (referent) | 7.7 | 1.0 (referent) |
| Yes (32%) | 3071 | 14.1 | 1.4 (1.2–1.6) | 20.0 | 1.5 (1.3–1.6) | 10.9 | 1.4 (1.2–1.6) |
|
|
|
|
|
||||
| Mental illness? | |||||||
| No (78%) | 7491 | 10.0 | 1.0 (referent) | 14.2 | 1.0 (referent) | 7.6 | 1.0 (referent) |
| Yes (22%) | 2142 | 16.6 | 1.7 (1.5–2.0) | 20.0 | 1.4 (1.3–1.6) | 12.7 | 1.7 (1.4–2.0) |
|
|
|
|
|
||||
| Parental separation or divorce? | |||||||
| No (74%) | 7135 | 11.0 | 1.0 (referent) | 14.5 | 1.0 (referent) | 7.8 | 1.0 (referent) |
| Yes (26%) | 2498 | 12.8 | 1.1 (1.0–1.3) | 18.2 | 1.2 (1.0–1.3) | 11.2 | 1.4 (1.2–1.6) |
|
|
|
|
|
||||
| Incarcerated household member? | |||||||
| No (94%) | 9085 | 11.3 | 1.0 (referent) | 15.1 | 1.0 (referent) | 8.3 | 1.0 (referent) |
| Yes (6%) | 548 | 14.2 | 1.2 (1.0–1.6) | 21.2 | 1.3 (1.1–1.7) | 15.3 | 1.8 (1.4–2.3) |
|
|
|
|
|
||||
| Total (100%) | 9663 | 11.5 | -------- | 15.5 | -------- | 8.7 | -------- |
Odds ratios are adjusted for age at time of survey and for sex, race, and educational attainment..
Adverse Childhood Experiences and Measures of Health and Well-Being
The ACE Score had a strong, graded relation to the four areas of health and well-being (p < 0.0001) (Table 3). Compared with workers who had an ACE Score of 0, workers with an ACE Score of 4 or higher had a 1.8-fold (somatic symptoms) to 3.5-fold (substance abuse) increased risk of problems in the four areas of health and well-being.
Table 3.
Relation between ACE Score and problems related to health and well-being
| ACE Score | (N) | Relationship problems | Emotional distress | Somatic symptoms | Substance abuse | ||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||
| % | ORa (95% CI) | % | ORa (95% CI) | % | ORa (95% CI) | % | ORa (95%CI) | ||
|
|
|
|
|
|
|||||
| 0 | 3019 | 36.6 | 1.0 (referent) | 21.0 | 1.0 (referent) | 44.4 | 1.0 (referent) | 22.2 | 1.0 (referent) |
| 1 | 2440 | 44.0 | 1.3 (1.2–1.5) | 27.9 | 1.4 (1.3–1.6) | 48.4 | 1.2 (1.1–1.3) | 30.0 | 1.4 (1.2–1.6) |
| 2 | 1642 | 47.8 | 1.6 (1.4–1.8) | 35.0 | 1.9 (1.7–2.2) | 53.7 | 1.4 (1.3–1.6) | 36.9 | 1.8 (1.6–2.1) |
| 3 | 1041 | 52.3 | 1.9 (1.6–2.2) | 40.8 | 2.4 (2.0–2.8) | 58.3 | 1.7 (1.5–2.0) | 44.0 | 2.5 (2.2–3.0) |
| ≥4 | 1491 | 57.4 | 2.3 (2.1–2.7) | 49.0 | 3.1 (2.7–3.6) | 60.8 | 1.8 (1.6–2.1) | 52.1 | 3.5 (3.1–4.1) |
|
|
|
|
|
|
|||||
| Total | 9633 | 45.3 | -- | 31.6 | -- | 51.0 | -- | 33.7 | -- |
Odds ratios were adjusted for age at time of survey and for sex, race, and educational attainment. Trend for increasing likelihood (OR) of each indicator or worker performance as ACE Score increases was statistically significant (p < 0.0001) for each logistic regression model
We observed a graded relation between ACE Score and mean number of positive responses to the component questions (range 0–12) (Table 4). The ACE Score also had a graded relation to each of the three component questions in each of the four areas of health and well-being (p < 0.001) (data not shown).
Table 4.
Relation between ACE Score and mean number of workforce problems related to health and well-beinga
| ACE Score | (N) | Mean number of problems related to health and well-beingb |
|---|---|---|
| 0 | 3019 | 1.72 (.06) |
| 1 | 2440 | 2.07 (.06) |
| 2 | 1642 | 2.44 (.07) |
| 3 | 1041 | 2.73 (.07) |
| ≥4 | 1491 | 3.22 (.07) |
Means were adjusted for age, sex, race, and educational attainment. Differences in mean between all groups were statistically significant (p < .0001).
Trend for increasing means was statistically significant (p < .0001) in the multiple linear regression model.
ACE Score, Indicators of Worker Performance, and Assessment for Mediation
The relation observed between ACE Score and each indicator of impaired worker performance was strong and graded (Table 5). Compared with workers who had an ACE Score of 0, workers with an ACE Score of 4 or higher were more than twice as likely to report each of the three indicators of impaired performance (Model 1; p < .0001). In logistic models that adjusted simultaneously for total number of positive responses to component questions for the measures of health and well-being, the strength of this relation between ACE Score and indicators of performance was reduced by an amount ranging from 50% to 100% (Model 2; p < .001), indicating a high degree of medication.
Table 5.
Relation between ACE Score and indicators of worker performance with and without adjustment for total number of problems related to health and well-being
| ACE Scorea | % | Job problems | % Risk reductionc | |
| Model 1b | Model 2b | |||
| OR (95% CI) | OR (95% CI) | |||
| 0 | 8.3 | 1.0 (referent) | 1.0 (referent) | -- |
| 1 | 9.6 | 1.2 (1.0–1.4) | 1.0 (0.8–1.2) | 100 |
| 2 | 12.0 | 1.5 (1.2–1.8) | 1.1 (0.9–1.3) | 80 |
| 3 | 14.1 | 1.8 (1.4–2.2) | 1.2 (0.9–1.5) | 75 |
| >4 | 18.5 | 2.4 (2.0–2.9) | 1.3 (1.1–1.6) | 79 |
| Total | 11.5 | -- | -- | -- |
| ACE Scorea | % | Financial problems | % Risk reductionc | |
| 0 | 10.5 | 1.0 (referent) | 1.0 (referent) | -- |
| 1 | 13.5 | 1.3 (1.1–1.5) | 1.1 (0.9–1.3) | 67 |
| 2 | 18.5 | 1.8 (1.5–2.2) | 1.4 (1.1–1.6) | 50 |
| 3 | 19.7 | 1.9 (1.6–2.3) | 1.3 (1.1–1.6) | 67 |
| >4 | 22.4 | 2.2 (1.8–2.6) | 1.2 (1.0–1.4) | 83 |
| Total | 15.5 | -- | -- | -- |
| ACE Scorea | % | Absenteeism | % Risk Reductionc | |
| OR (95% CI) | OR (95% CI) | |||
| 0 | 6.0 | 1.0 (referent) | 1.0 (referent) | -- |
| 1 | 7.5 | 1.3 (1.1–1.6) | 1.1 (1.1–1.6) | 67 |
| 2 | 8.5 | 1.4 (1.1–1.8) | 1.1 (0.9–1.4) | 75 |
| 3 | 11.1 | 1.8 (1.4–2.3) | 1.4 (1.0–1.7) | 50 |
| >4 | 14.8 | 2.4 (2.0–3.0) | 1.6 (1.2–1.9) | 57 |
| Total | 8.7 | -- | -- | -- |
Sample sizes for each ACE Score are the same for each model: 0 = 3019, 1 = 2440, 2 = 1642, 3 = 1041, >4 = 1491; increasing likelihood (OR) of each indicator or worker performance as the ACE Score increases is significant (p < 0.001).
Both Model 1 and Model 2 adjust for age, sex, race, and education; Model 2 also includes number of problems in the areas of health and well-being (range: 0–12).
Change in relative risk (OR) between Model 1 and Model 2.
The overall fit of the logistic regression model for job problems was statistically significantly improved when both the number of positive responses to questions about health and well-being and the ACE Score were added to the model simultaneously (χ2 = 425, 1 degree of freedom; p < .0001). When the number of problems in the areas of health and well-being were entered into the models for financial problems and absenteeism, the χ2 values for the overall fit of the models were 117 and 177, respectively (1 degree of freedom, p < .00001 for each). The substantial differences between the unadjusted and adjusted models suggest that problems in the areas of health and well-being play a substantial role mediating the relation between ACE Score and indicators of worker performance.
Discussion
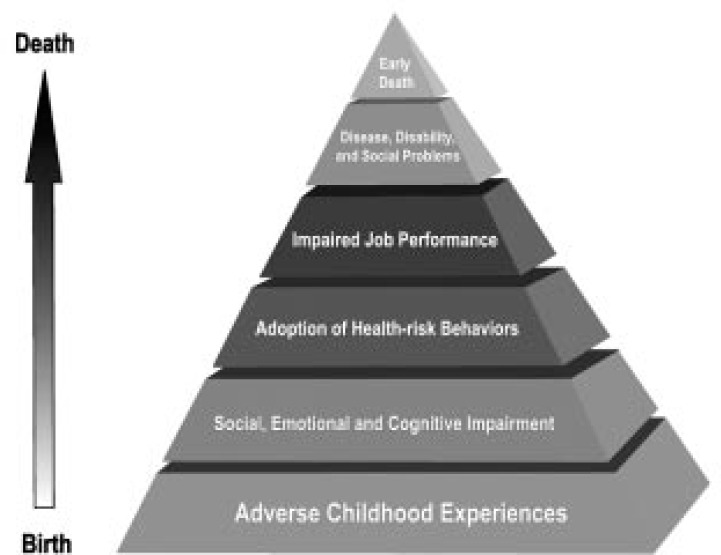
The ACE Study showed that adverse childhood experiences bear a strong, graded relation to many adult health problems and to many leading causes of death.9–16 Using data from the ACE Study, we showed a strong, graded relation between eight categories of adverse childhood experience and three indicators of worker performance. Moreover, four areas of health and well-being that employers and medical practitioners have difficulty managing (relationship problems, emotional distress, somatic symptoms, substance abuse)2,3 appear to be intermediate variables. Because child abuse and household dysfunction are common and have long-term effects that are highly disruptive to workers’ health and well-being, these adverse childhood experiences merit serious attention from the business community, labor leaders, the everyday practitioners of medicine, and government agencies.
Traditionally, maintaining a healthy and productive workforce has centered on job training, technologic improvement in production, and medical care for injury.23–25 Instead, however, our data indicate the need to adopt the World Health Organization (WHO) definition of health.1 To do so would necessitate a paradigm shift, in which the disease-oriented biomedical approach is replaced by a biopsychosocial approach in which child abuse and household dysfunction are understood in terms of their long-term effects on worker health and well-being.9–16 In this approach, a person’s life experiences, well-being (emotional, social, and financial), and risk-related behavior would be assessed according to Engel’s concept of biopsychosocial evaluation.26 The result of this assessment might be a healthier, more productive workforce that would, in turn, produce greater benefits not only for individual persons but also for families, communities, and the nation.
A major obstacle to implementing this paradigm shift is that medical practitioners,27 corporate managers, and labor leaders are unlikely to fully understand that impaired worker performance may be a long-term effect of childhood abuse and household dysfunction. This lack of understanding may be expected for three reasons: Reports of this long-term cause-and-effect relation9–16 are too new to have been disseminated as widely as necessary; the interval between cause and effect is long, and thus the etiology is easily overlooked; and the adverse childhood experiences that led to worker impairment are well shielded by shame, secrecy, and social taboo. In this context, many workers become involved in an expensive,28 lengthy, and frequently unproductive search for an “organic” or biomedical explanation for worker performance and occupational medicine problems.
The adverse childhood experiences we studied do not occur in isolation from each other. We previously reported that people who report having one category of exposure have an 85% chance of experiencing a second category and have a 70% chance of experiencing a third.9,11 Thus, we view this set of childhood exposures as a constellation of interrelated problems. In this and other published studies,9–16 the ACE Score has proved useful as a summary device for assessing the cumulative negative effects of adverse childhood experiences. Further, the biologic plausibility of using the ACE Score as a cumulative stressor model is supported by recent neuroscientific information.29 Specifically, exposure of children to stressful events such as recurrent abuse or witnessing domestic violence can negatively disrupt early development of the central nervous system and can adversely affect brain functioning later in life.30 These developmental effects might account both for some health problems and for treatment for failures later in life.
Our findings may be limited by the general nature of our indicators of worker performance; however, their lack of specificity probably leads to underestimating the strength of the relation between adverse childhood experiences and worker performance. Had we used more detailed measures of performance, we might have observed an even stronger relation to adverse childhood experiences. Because the sensitive nature of our questions probably led study participants to underreport problems in health and well-being, we probably tended to be conservative in estimating mediating influence of these areas on workers’ job performance. Moreover, the finding that our general indicators of worker performance are strongly associated with four areas of health and well-being known to affect worker performance2,3,5 supports the external validity of our findings.
Because our study participants were enrolled in a large HMO and were currently employed, we can reasonably expect our findings to apply to a wide population of employers and HMOs. That the prevalence of these exposures in our study is similar to the prevalence in other population-based studies of childhood abuse, household dysfunction, and alcoholism in the home20,31,32 suggests that our study population reflects the general population.
Our findings suggest that employers and HMOs have both the need and the opportunity to work together against the long-term effects of childhood abuse and household dysfunction. Exposure to such adverse circumstances is likely to lead to massive financial expenditures for health care as well as to economic losses attributable to poor work performance. Adverse childhood experiences are a source of many problems—somatic manifestations of health and social problems—treated by occupational medicine specialists. The traditional search for organic causes of illness and injury among workers is expensive for employers, who must pay higher insurance premiums for their workers. In addition, this traditional process is expensive for health care organizations, because much of such medical care is ineffective or inefficient: diagnostic procedures are used without sufficient understanding of the common psychosocial origins of symptoms, multiple office visits and specialty referrals are used in repeated efforts to resolve the same problem, and drugs are prescribed to little or no effect. Most important, workers suffer when their health problems and health-related social problems remain unresolved. If even a small fraction of the economic and human resources currently spent on these conventional approaches was used to identify and address the root origins of these problems in the workforce, we could reasonably expect to find more effective ways to improve worker health, well-being, and performance.
Acknowledgments
We gratefully acknowledge technical assistance provided by Naomi (Howard) Jensen, BA, Study Coordinator. The Adverse Childhood Experiences (ACE) Study was funded by cooperative agreement #TS-44-10/11 by the Centers for Disease Control and Prevention with the Association of Teachers of Preventive Medicine and currently by a grant from the Kaiser Permanente Garfield Memorial Fund.
Biographies
Robert F Anda, MD, MS, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA.
Vladimir I Fleisher, MD, PhD, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA.
Vincent J Felitti, MD, FACP, Department of Preventive Medicine, Southern California Permanente Medical Group, Kaiser Permanente, San Diego, CA.
Valerie J Edwards, PhD, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA.
Charles L Whitfield, MD, Private Practice of Trauma Psychology and Addiction Medicine, Atlanta, GA.
Shanta R Dube, MPH, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA.
David F Williamson, MS, PhD, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA.
| Practice tips |
|---|
| 1. Consider a biopsychosocial approach when you encounter: relationship problems, emotional distress, somatic symptoms, substance abuse. |
| 2. Specifically consider adverse childhood event if: work problems, financial problems, or absenteeism. |
| 3. Assess problems using the questions in Table 1. |
The Relatioinship of Adverse Childhood Experiences to Job Performance and Occupational Health
References
- 1.World Health Organization Constitution of the World Health Organization. Available from: http://opbw.org/int_inst/health_docs/WHO-CONSTITUTION.pdf (accessed November 26, 2003).
- 2.Cohen GS, Gard LH, Heffernan WR. Employee assistance programs: a preventive, cost-effective benefit. J Health Care Finance. 1998 Spring;24(3):45–53. [PubMed] [Google Scholar]
- 3.Turpin SC. Employee assistance programs pay off. Warehousing Management. 1998 Jun 1; Available from: www.manufacturing.net/ctl/index.asp?layout=article&articleid=CA149037 (accessed November 20, 2003. [Google Scholar]
- 4.Board of Governors of the Federal Reserve System Monetary policy report to the Congress pursuant to the Full Employment and Balanced Growth Act of 1978, July 22, 1999. Available from: www.federalreserve.gov/boarddocs/hh/1999/July/FullReport.pdf (accessed November 20, 2003). [Google Scholar]
- 5.Rizzo JA, Abbott TA, 3rd, Berger ML. The labor productivity effects of chronic backache in the United States. Med Care. 1998 Oct;36(10):1471–88. doi: 10.1097/00005650-199810000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of lost productive work time among US workers with depression. JAMA. 2003 Jun 18;289(23):3135–44. doi: 10.1001/jama.289.23.3135. [DOI] [PubMed] [Google Scholar]
- 7.National Institute on Drug Abuse, National Institute on Alcohol Abuse and Alcoholism . The economic costs of alcohol and drug abuse in the United States, 1992. Rockville (MD): US Department of Health and Human Services; 1998. Available from: www.nida.nih.gov/economiccosts/index.html (accessed December 18, 2003). [Google Scholar]
- 8.Smith S, Freeland M, Heffler S, McKusick D. The next ten years of health spending: what does the future hold? The Health Expenditures Projection Team. Health Aff (Millwood) 1998 Sep-Oct;17(5):128–40. doi: 10.1377/hlthaff.17.5.128. [DOI] [PubMed] [Google Scholar]
- 9.Felitti VJ, Anda RF, Nordenberg D, et al. The relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998 May;14(4):245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 10.Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999 Nov 3;282(17):1652–8. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 11.Dietz PM, Spitz AM, Anda RF, et al. Unintended pregnancy among adult women exposed to abuse or household dysfunction during their childhood. JAMA. 1999 Oct 13;282(14):1359–64. doi: 10.1001/jama.282.14.1359. [DOI] [PubMed] [Google Scholar]
- 12.Hillis SD, Anda RF, Felitti VJ, Nordenberg D, Marchbanks PA. Adverse childhood experiences and sexually transmitted diseases in men and women: a retrospective study. Pediatrics. 2000 Jul;106(1):E11. doi: 10.1542/peds.106.1.e11. [DOI] [PubMed] [Google Scholar]
- 13.Anda RF, Felitti VJ, Chapman DP, et al. Abused boys, battered mothers, and male involvement in teen pregnancy. Pediatrics. 2001 Feb;107(2):E19. doi: 10.1542/peds.107.2.e19. [DOI] [PubMed] [Google Scholar]
- 14.Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB. Adverse childhood experiences and personal alcohol abuse as an adult. Addict Behav. 2002 Sep-Oct;27(5):713–25. doi: 10.1016/s0306-4603(01)00204-0. [DOI] [PubMed] [Google Scholar]
- 15.Hillis SD, Anda RF, Felitti VJ, Marchbanks PA. Adverse childhood experiences and sexual risk behaviors in women: a retrospective cohort study. Fam Planning Perspectives. 2001 Sep-Oct;33(5):206–11. [PubMed] [Google Scholar]
- 16.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001 Dec 26;286(24):3089–96. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 17.Edwards VJ, Anda RF, Nordenberg DF, Felitti VJ, Williamson DF, Wright JA. Bias assessment for child abuse survey: factors affecting probability of response to a survey about childhood abuse. Child Abuse Negl. 2001 Feb;25(2):307–12. doi: 10.1016/s0145-2134(00)00238-6. [DOI] [PubMed] [Google Scholar]
- 18.Straus M, Gelles RJ. Physical violence in American families: risk factors and adaptations to violence in 8145 families. New Brunswick (NJ): Transaction; 1990. [Google Scholar]
- 19.Wyatt GE. The sexual abuse of Afro-American and white-American women in childhood. Child Abuse Negl. 1985;9(4):507–19. doi: 10.1016/0145-2134(85)90060-2. [DOI] [PubMed] [Google Scholar]
- 20.Schoenborn CA. Exposure to alcoholism in the family: United States, 1988. Advance Data. 1991 Sep 30;205:1–13. [PubMed] [Google Scholar]
- 21.Rothman KJ. Modern epidemiology. Boston: Little, Brown; 1986. [Google Scholar]
- 22.SAS Institute . SAS procedures guide, version 6. 3rd ed. Cary (NC): SAS Institute; 1990. [Google Scholar]
- 23.Green GM, Baker F, editors. Work, health, and productivity. New York: Oxford University Press; 1991. [Google Scholar]
- 24.Leclaire R, Esdaile JM, Suissa S, Rossignol M, Proulx R, Dupuis M. Back school in a first episode of compensated acute low back pain: a clinical trial to assess efficacy and prevent relapse. Arch Phys Med Rehabil. 1996 Jul;77(7):673–9. doi: 10.1016/s0003-9993(96)90007-6. [DOI] [PubMed] [Google Scholar]
- 25.Weidner BL, Gotsch AR, Delnevo CD, Newman JB, McDonald B. Worker health and safety training: assessing impact among responders. Am J Indus Med. 1998 Mar;33(3):241–6. doi: 10.1002/(sici)1097-0274(199803)33:3<241::aid-ajim5>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 26.Engel G. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980 May;137(5):535–44. doi: 10.1176/ajp.137.5.535. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez MA, Bauer HM, McLoughlin E, Grumbach K. Screening and intervention for intimate partner abuse: practices and attitudes of primary care physicians. JAMA. 1999 Aug 4;282(5):468–74. doi: 10.1001/jama.282.5.468. [DOI] [PubMed] [Google Scholar]
- 28.Doyle R. Health care costs. Sci Am. 1999 Apr;280(4):36. [Google Scholar]
- 29.Weiss MJ, Wagner SH. What explains the negative consequences of adverse childhood experiences on adult health? Insights from cognitive and neuroscience research. Am J Prev Med. 1998 May;14(4):356–60. doi: 10.1016/s0749-3797(98)00011-7. [DOI] [PubMed] [Google Scholar]
- 30.Perry BD, Pollard R. Homeostasis, stress, trauma, and adaptation. A neurodevelopmental view of childhood trauma. Child Adolesc Psychiatr Clin N Am. 1998 Jan;7(1):33–51. [PubMed] [Google Scholar]
- 31.Finkelhor D, Hotaling G, Lewis IA, Smith C. Sexual abuse in a national survey of adult men and women: prevalence, characteristics, and risk factors. Child Abuse Negl. 1990;14(1):19–28. doi: 10.1016/0145-2134(90)90077-7. [DOI] [PubMed] [Google Scholar]
- 32.MacMillan HL, Fleming JE, Trocme N, et al. Prevalence of child physical and sexual abuse in the community. Results from the Ontario Health Supplement. JAMA. 1997 Jul 9;278(2):131–5. [PubMed] [Google Scholar]