Abstract
Objectives:
To evaluate social and program factors associated with the one-year smoking cessation rate among participants of a smoking cessation program at a managed care organization (MCO).
Methods:
As implemented at this MCO, the Quit Smart™ program incorporated group sessions taught by health educators, discount vouchers for nicotine replacement patches, self-help manuals, and a relaxation audiotape. A survey of 97 patients who participated in the program during 1999 or 2000 or both was administered one year after these participants completed the program.
Results:
Of the 97 participants, 58 responded to the survey. Nineteen (33%) reported not smoking at one year after completing the program; and 11 (19%) reported that they were smoking-abstinent for 12 months after completing the program. Compared with patients who did not use the nicotine patch, respondents who used the nicotine patch were significantly more likely (OR = 4.42 [1.12, 17.35]) to report not smoking at 12 months after completing the program and to be smoking-abstinent for 12 months after completing the program (OR = 8.31 [1.15–60.22]). Respondents who were exposed to smoking in two or three settings (ie, at home, with friends, at work) were significantly less likely to report smoking cessation at 12 months (OR = 0.12 [0.02, 0.70]) and to have abstained from smoking for 12 months (OR = 0.04 [0.01, 0.42]) than were respondents who were not exposed to smoking in these settings.
Conclusions:
The Quit Smart™ program achieved 12-month smoking cessation and abstinence rates comparable with those achieved by other multifactorial programs to promote smoking cessation. Subsidized therapy using the nicotine patch was effective for promoting smoking cessation. However, program success was inhibited by exposure to smoking in domestic and social situations.
Introduction
Population-based studies of smoking cessation programs indicate that, although initial quit rates are high, quit rates decline to approximately 15%–25% at one year.1,2 Community- and workplace-based interventions generally report quit rates of a similar magnitude,3,4 and some report rates as high as 36%.5 For comparison, the background rate of unassisted smoking cessation is estimated at approximately 7%–8%.2,6 Physician interventions that use nicotine gum as an aid to smoking cessation produce one-year quit rates of about 10%.7,8 Within managed care organizations, one-year smoking cessation rates as high as 30%–40% have been reported.9–11 One of several interventions used in multifactorial health education programs to promote smoking cessation, nicotine replacement therapy is efficacious for promoting and sustaining smoking cessation7 and is also a cost-effective method of treatment.9,12 Controlled studies have shown that quit rates for users of the nicotine patch are approximately double the quit rates for users of placebo.13,14
The Quit Smart™ smoking cessation program, developed by Robert H Shipley, PhD (founding director of the Duke Medical Center Stop Smoking Clinic), is a multifactorial health education program designed to promote smoking cessation among tobacco users. Quit Smart™ was implemented in 1998 as part of the health education program of the Kaiser Permanente Georgia Region (KPG). A pilot evaluation of the Quit Smart™ program was conducted for KPG’s quality improvement initiatives and addressed three questions:
How many participants were smoking when surveyed at 12 months after completing the program?
How many participants abstained from tobacco use for the entire 12-month period after completing the program?
What behavioral and environmental factors promoted or inhibited the likelihood of attaining these two endpoints?
This article presents results of the pilot evaluation.
Methods
Intervention Used in the Quit Smart™ Program
As implemented at KPG, the Quit Smart™ program combines features of aided smoking cessation programs (eg, programs using nicotine gum) and programs that use group support and behavioral intervention. The goal of this combined approach is to maximize the number of smokers who can abstain from cigarettes permanently. The Quit Smart™ program consists of six interactive group sessions directed by trained health educators and offered quarterly during evenings and weekends. During the course of the program, participants wean themselves from nicotine by switching to cigarette brands that deliver successively lower levels of nicotine. Participants also receive a $5 discount voucher (redeemable at any KPG pharmacy) for a two-week supply of nicotine patches every two weeks for the duration of the program. Additional materials provided to participants for use during the program include brochures and guides for adopting a smokefree lifestyle; an audiotape designed to promote relaxation; and a patented, realistic cigarette substitute. The fee for the program is $20. Key components of the Quit Smart™ intervention are summarized in Figure 1.
Figure 1.
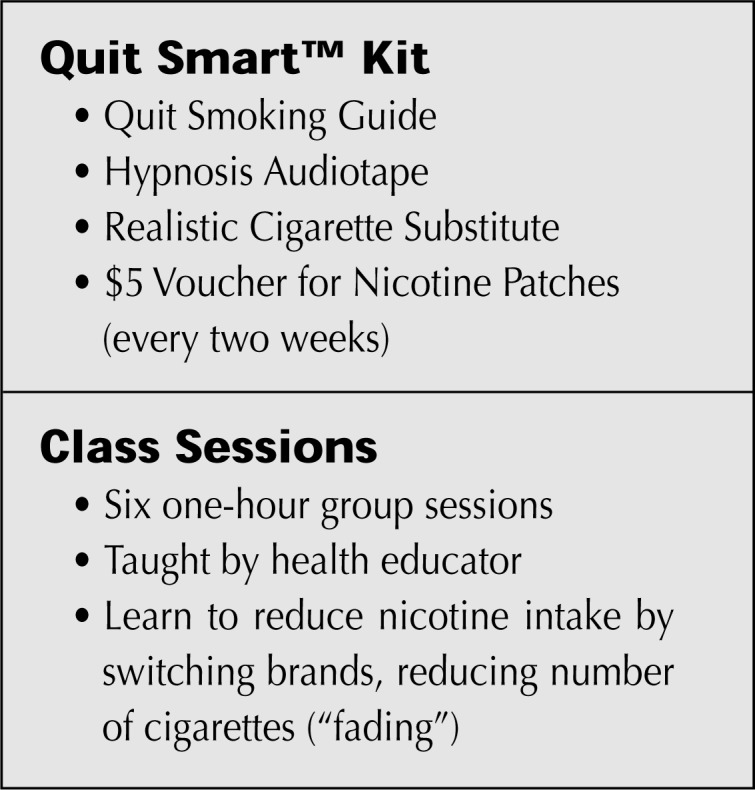
Diagram summarizes Quit SmartTM Program components.
Study Population
The study population consisted of all participants in the Quit Smart™ program during the Fall 1998 (n = 62) and Spring 1999 (n = 35) sessions who remained enrolled with KPG at 12 months after attending the last program session.
Participant Survey
A short survey of the study population was administered by telephone to ascertain one-year smoking cessation status and to identify factors promoting or inhibiting smoking cessation in the 12 months after completing the Quit Smart™ program.
Instrument items and scales were developed through an iterative process. We initially reviewed the smoking cessation literature for sample items and for factors associated with promoting or inhibiting smoking cessation. The survey instrument included items about the following topics:
Tobacco smoking in the 12 months after completing the Quit Smart™ program;
Motivation for enrolling in the program;
Aids for smoking cessation, whether used in the Quit Smart™ program or otherwise known to be effective (eg, nicotine patches);
Other behavioral and environmental factors associated with promoting smoking cessation (eg, regular physical exercise) or inhibiting smoking cessation (eg, smoking by other family members);
Symptoms experienced by program participants after completing the program and which are typically associated with newly begun abstinence from tobacco; and
Basic demographic and socioeconomic characteristics of program participants.
The survey instrument was designed to be completed within 10–15 minutes. A draft instrument was administered to a small convenience sample of colleagues (smokers and former smokers) for assessing flow and clarity of the instrument. The final survey instrument included revisions suggested by the preliminary survey results. The final survey instrument and the protocol for its administration were reviewed, approved, and monitored by the KPG Institutional Review Board.
For the Fall 1998 group, the survey was administered during December 1999; for the Spring 1999 group, the survey was administered during May 2000. Approximately two weeks before receiving the initial telephone call, each potential respondent was mailed a letter containing information about the survey. As many as five attempts were made to contact each potential respondent. A total of 58 participants completed most of the survey (response rate of 60%).
Measures
The study had two principal dependent variables: smoking cessation status at 12-month follow-up and smoking cessation status for the entire 12 months after participating in the program. Smoking cessation at 12 months after last attending the Quit Smart™ program was assessed by response to the following item: “Do you currently smoke cigarettes?” A negative response was interpreted as indicating nonsmoking at 12 months. The second dependent variable—ie, whether or not the respondent was smokefree for the entire 12-month period—was ascertained for respondents who responded negatively both to the initial item and to another item: “Did you smoke cigarettes at any time following the Quit Smart™ program?” Respondents who answered “no” to smoking at 12 months and respondents who answered “no” to smoking at any time were considered to be smokefree for 12 months. Both dependent variables were coded as binary (1 = not smoking at 12 months or 1 = 12 months smokefree, 0 = otherwise).
The study had three principal independent variables: use of aids to quit smoking, cumulative number of settings with smoking exposure, and level of physical activity. Use of aids to quit smoking was assessed among all respondents by asking, “What techniques did you use to quit smoking?” Responses included: “Cold turkey, will power” and “Nicotine patch.” Both variables were coded as binary (1 = used the technique). Smoking exposure at home, among friends, and at work was ascertained. Exposure at home was measured by asking if the respondent lived in a house with others and whether or not any of these persons smoked. Exposure among friends was assessed by asking how many of the respondent’s five closest friends smoked. Exposure at work was ascertained by asking if the respondent was employed and whether or not any of the respondent’s five closest colleagues smoked. Each of these three variables was coded as binary (1 = exposed). A cumulative measure of smoking exposure was also computed as the sum of the settings with exposure (0, 1, 2, or 3). Level of physical activity was ascertained from a 5-level response (“Rarely or not at all” through “Every day”) to the question “How often do you exercise?” We recoded this item into a binary variable of “Every day” versus “Less than every day.”
Patient demographic and socioeconomic measures included age (below median age 48 years vs at or above median age); gender; race/ethnicity (white or African American); level of education; and household income.
Statistical methods
The 12-month quit rate was calculated as the number of respondents who were not smoking at the time of interview divided by the total number of respondents who completed the survey. The 12-month abstinence rate was calculated as the number of respondents who remained smokefree for the entire 12 months after completing the program divided by the total number of respondents.
Association of the independent variables with respondent status as a 12-month quitter or with respondent status as a 12- month abstainer or not was evaluated by using a χ2 test of significance (α = 0.05). Because the sample size was small, we considered any association with an α-level of 0.15 to be marginally significant.
Logistic regression for each of the two dependent variables was estimated to assess competing effects of factors that help smoking cessation and factors that inhibit smoking cessation.
Analyses were performed using SAS (Statistical Analysis Software) Version 6.12 (SAS Institute, Cary NC).
Results
Respondent characteristics
Median age of respondents was 48 years (Table 1). The population of respondents was predominantly (nearly 75%) female and consisted of approximately equal percentages of whites and African Americans. Most respondents had some college education, reported an annual household income of at least $50,000, and were married. Overall, respondents resembled the KPG adult membership except for the distribution by gender, which in the general KPG adult membership is approximately equal.
Table 1.
Characteristics of 58 participants in smoking cessation program
| Number (%) of respondents | ||||
|---|---|---|---|---|
| Not smoking at 12 months | P | Smokefree for 12 months | P | |
| Overall | 19 (32.8) | -- | 11 (19.0) | -- |
| Age: | 0.78 | 0.50 | ||
| 25–47 years (50.0%) | 10 (35.7) | 7 (25.0) | ||
| 48 years and older (50.0%) | 9 (32.1) | 4 (14.2) | ||
| Gender: | 0.49 | 0.91 | ||
| Male (25.9%) | 6 (40.0) | 3 (20.0) | ||
| Female (74.1%) | 13 (30.2) | 8 (18.6) | ||
| Race/ethnicity: | 0.35 | 0.94 | ||
| White (53.6%) | 8 (26.7) | 6 (20.0) | ||
| Black (46.4%) | 10 (38.5) | 5 (19.2) | ||
| Education: | 0.23 | 0.03 | ||
| High school or less (25.9%) | 3 (20.0) | 0 (0.0) | ||
| Some college, college graduate, or postgraduate (74.1%) | 16 (37.3) | 11 (25.6) | ||
| Household income (1998): | 0.39 | 0.89 | ||
| Less than $50,000 (47.3%) | 7 (26.9) | 5 (19.2) | ||
| $50,000 or more (52.7%) | 11 (37.9) | 6 (20.7) | ||
| Marital status: | 0.77 | 0.38 | ||
| Married (70.9%) | 13 (33.3) | 9 (23.1) | ||
| Single (29.1%) | 6 (37.5) | 2 (12.5) | ||
Probabilities derived from a χ2 (1 df) test of two levels of the patient characteristic with smoking cessation status.
Note: Numbers of respondents by characteristic may be less than overall number because of missing values for the characteristic.
Personal choice was indicated by 71% of respondents as the principal reason for enrolling in the Quit Smart™ program (data not shown in tables). Physician recommendation to enroll was the principal reason given by 21% of respondents. Only 7% indicated that availability of the nicotine patch was their principal reason for enrollment. Neither the 12-month quit rate nor the 12-month abstinence rate was significantly associated with respondents’ reasons for enrolling in the Quit Smart™ program.
Smoking Cessation
The 12-month quit rate was 32.8% (95% CI≈21.4%–46.5%; Table 1). The 12-month smoking abstinence rate was 19.0% (95% CI≈10.3%–31.8%). The 12-month quit rate was not significantly associated with any of the demographic, racial or socioeconomic characteristics of respondents. The 12-month abstinence rate differed significantly only by level of education of respondents (p = 0.03). None of the respondents with a high school education or less abstained from tobacco use for the entire 12 months after enrollment in the Quit Smart™ program.
Of the 39 respondents who indicated that they were smoking at 12 months after last attending the Quit Smart™ program, 67% indicated that they had quit smoking for a limited time after completing the Quit Smart™ program (data not shown in tables). At the time of survey, current smokers were, on average, smoking 13 cigarettes (half a pack) per day. Mean duration of abstaining from smoking was 2.6 months.
Factors Promoting or Inhibiting Smoking Cessation
The 12-month quit rate was marginally associated with several environmental factors reported by respondents (Table 2). The 12-month quit rate among respondents who reported exposure to smoking in two or more settings was 18.2%, lower than the 46.7% rate for respondents who were not exposed to smoking in any setting (p = 0.06). The 15.4% quit rate for respondents who were exposed to smoking at home was lower than the 37.8% quit rate for respondents who were not exposed to smoking at home (p = 0.13). The 22.6% quit rate for respondents who were exposed to smoking among friends was lower than the 44.4% quit rate for respondents who were not exposed to smoking among friends (p = 0.08). Among respondents who reported using the nicotine patch as an aid for quitting smoking, the 12-month quit rate (41.9%) was greater than the 12-month quit rate (22.2%) among respondents who did not use the nicotine patch (p = 0.11).
Table 2.
Behavior reported by 58 participants in a smoking cessation program
| Number (%) of respondents | ||||
|---|---|---|---|---|
| Not smoking at 12 months | P | Smokefree for 12 months | P | |
| Overall: | 19 (32.8) | -- | 11 (19.0) | -- |
| Use of aids to quit smoking: | ||||
| Nicotine patch (53.5%) | 13 (41.9) | 0.11a | 8 (25.8) | 0.16a |
| Willpower (25.9%) | 6 (40.0) | 0.49a | 2 (13.3) | 0.52a |
| Exercise daily (22.4%) | 6 (46.2) | 0.25a | 5 (38.5) | 0.04a |
| Number of settings exposed to smoking: | 0.06b | 0.03b | ||
| 0 (25.9%) | 7 (46.7) | 6 (40.0) | ||
| 1 (36.2%) | 8 (38.1) | 3 (14.3) | ||
| 2 (37.9%) | 4 (18.2) | 2 (9.1) | ||
| Exposed to smoking at home (22.4%) | 2 (15.4) | 0.13a | 2 (15.4) | 0.71a |
| Exposed to smoking among friends (53.5%) | 7 (22.6) | 0.08a | 2 (6.5) | 0.01a |
| Exposed to smoking at work (41.4%) | 7 (29.2) | 0.63a | 3 (12.5) | 0.30 a |
Probability for a χ2 (1 df) test of the behavior and its counterfactual (eg, doctor did not recommend, nicotine patch was not used, patient was not exposed to smoking at home) with smoking cessation status.
Probability for a χ2 (2 df) test of the three levels of the behavior with smoking cessation status.
Note: Numbers of respondents by behavior may be less than overall number because of missing values for the behavior.
The 12-month abstinence rate was significantly associated with exercise frequency, number of settings exposed to smoking, and exposure to smoking among friends (p < 0.950 (Table 2). The 12-month abstinence rate among respondents who reported exercising daily (38.5%) was higher than the abstinence rate among respondents who exercised less frequently (13.3%) (p = 0.04). For respondents who were exposed to smoking in at least two settings, the 12-month abstinence rate (9.1%) was lower than the abstinence rate for respondents who were not exposed to smoking in any setting (40.0%) (p = 0.03). The 12-month abstinence rate was most adversely associated with exposure to smoking among friends (6.5%) of any setting in which respondents were exposed to smoking (33.3%) (p = 0.01).
For exercise frequency, use of the nicotine patch, and settings in which respondents were exposed to smoking, we obtained adjusted odds ratios for 12-month smoking cessation status (Table 3). Compared with respondents who did not use the nicotine patch, respondents who used the nicotine patch were significantly more likely (OR = 4.42 [1.12, 17.35]) to report not smoking at 12 months and to abstain from smoking for 12 months (OR = 8.31 [1.15–60.22]). Compared with respondents who were not exposed to smoking at home, among friends, or at work, respondents who were exposed to smoking in two or three settings were significantly less likely to report smoking cessation at 12 months (OR = 0.12 [0.02, 0.70]). Similarly, respondents who were exposed to smoking in either one, two, or three settings were significantly less likely (OR = 0.09 [0.01, 0.42] and 0.04 [0.01, 0.42], respectively) to abstain from smoking for 12 months than were participants who were not exposed to smoking in these three settings.
Table 3.
Adjusted odds ratios obtained from logistic regression analysis of smoking cessation
| Not smoking at 12 months | Smokefree for 12 months | |||||
|---|---|---|---|---|---|---|
| Adjusted odds ratio | Lower 95% CI | Upper 95% CI | Adjusted odds ratio | Lower 95% CI | Upper 95% CI | |
| Used nicotine patch as aid to quit smoking | 4.42a | 1.12 | 17.35 | 8.31a | 1.15 | 60.22 |
| Exposed to smoking in only one setting | 0.47 | 0.11 | 2.13 | 0.09a | 0.01 | 0.76 |
| Exposed to smoking in two or three settings | 0.12a | 0.02 | 0.70 | 0.04a | 0.01 | 0.42 |
| Exercise daily | 2.19 | 0.55 | 8.75 | 6.11a | 1.11 | 33.51 |
| Model goodness of fit: | ||||||
| χ2 (4 df) | 10.46b | 15.69b | ||||
| Mallows c | 0.73 | 0.87 | ||||
Indicates that adjusted odds ratio is significantly different from 1.00 for p < 0.05.
Indicates that the model goodness-of-fit estimate is significant for p < 0.05.
Reference group: did not use nicotine patch; not exposed to smoking at home, among friends, or at work; and exercise less than daily.
Discussion
As implemented at KPG, the Quit Smart™ program yielded a 12-month quit rate of 33% and a 12-month abstinence rate of 19%. These rates resemble those achieved in other multi-factorial health education programs promoting smoking cessation at other MCOs. Use of the nicotine patch promoted both smoking cessation and smoking abstinence at 12 months, whereas continued exposure to smoking—whether at home, among friends, or at work—inhibited both smoking cessation and smoking abstinence at 12 months. This importance of the nicotine patch (and other forms of nicotine replacement) for facilitating smoking cessation is consistent with results reported for clinical trials as well as for other observational studies of smoking cessation techniques.7,9,12–15 Other studies have affirmed the association between exposure to smoking and temptation to smoke, failure to quit smoking, and smoking relapse among former smokers.16–22
The main strength of the Quit Smart™ smoking cessation program is its combination of proven methods for aiding smoking cessation. Comments solicited from survey respondents indicated that the program was well received by those who attended it. Even respondents who continued to smoke indicated that they were very satisfied with the program overall.
That smoking cessation programs are cost-effective—both in general and with regard to specific strategies—is widely accepted.9,12,23–25 The cost of an entire smoking cessation program may be justified even if only a low percentage of program participants achieve abstinence.24 Of KPG participants in the Quit Smart™ program, 19% abstained from tobacco use for 12 months after completing the program. Although we did not calculate a final cost-benefit analysis, the quit rate as calculated would suggest that the Quit Smart™ program is a success from a cost-benefit standpoint as well as from a health education standpoint.
Although encouraging, the results of our evaluation of the Quit Smart™ program should be interpreted as preliminary. Although the response rate to the survey was relatively high (60%), the number of respondents was small. This small sample size limited power to detect statistically significant differences (for p < 0.05) in factors promoting or inhibiting smoking cessation and resulted in wide confidence intervals even when a difference was significant (p < 0.05). Moreover, the study sample included only KPG members who completed the Quit Smart™ program and remained KPG members at 12 months after completing the program. If smoking cessation or abstinence rates differ between survey respondents and nonrespondents, between study participants who remained KP members and study participants who disenrolled from KPG, or between participants who completed the Quit Smart™ program and those who did not, then our current estimates of the Quit Smart™ program could overestimate or underestimate the true intervention effects. In addition, we used patient-reported measures for estimating 12-month quit and abstinence rates. Although self-reported measures are generally consistent with biochemical measures of smoking status, self-reported measures may tend to overstate the socially desirable response (ie, smoking cessation).26–30 Because this study was conducted as part of a quality improvement initiative, we did not include a control group (eg, patients randomly assigned at entry to the Quit Smart™ program or no intervention).
In summary, the Quit Smart™ program was easily incorporated into the prevention and health promotion objectives of the Kaiser Permanente Georgia Region. Of program participants responding to a survey at 12 months after completing the program, 33% had quit smoking; and 19% reported that they had abstained from smoking for the entire 12 months. Use of the nicotine patch significantly promoted smoking cessation, whereas exposure to smokers in multiple settings significantly inhibited smoking cessation.
Biographies
Karen M Polizzi, MPH, Doctoral Student, Research Department, KP Atlanta, GA. E-mail: Karen.Polizzi@gatech.edu.
Douglas W Roblin, PhD, Research Scientist, Research Department, KP Atlanta, GA. E-mail: douglas.robin@kp.org.
Adrienne D Mims, MD, MPH, Chief of Prevention and Health Promotion, KP Atlanta, GA. E-mail: adrienne.mims@kp.org.
Dianne Harris, BS, CHES, Member Education Coordinator, KP Atlanta, GA. E-mail: dianne.harris@kp.org.
Dennis D Tolsma, MPH, Director of Research for KP Atlanta, GA. E-mail: dennis.tolsma@kp.org.
To Choose an Action
His mother often said, When you choose an action, you choose the consequences of that action. She had emphasized the corollary of this axiom even more vehemently: when you desired a consequence you had damned well better take the action that would create it.
—Lois McMaster Bujold, b 1949, Science Fiction and Fantasy writer
References
- 1.Bains N, Pickett W, Hoey J. The use and impact of incentives in population-based smoking cessation programs: a review. Am J Health Promot. 1998 May-Jun;12(5):307–20. doi: 10.4278/0890-1171-12.5.307. [DOI] [PubMed] [Google Scholar]
- 2.Zhu S, Melcer T, Sun J, Rosbrook B, Pierce JP. Smoking cessation with and without assistance: a population-based analysis. Am J Prev Med. 2000 May;18(4):305–11. doi: 10.1016/s0749-3797(00)00124-0. [DOI] [PubMed] [Google Scholar]
- 3.Klesges RC, Brown K, Pascale RW, Murphy M, Williams E, Cigrang JA. Factors associated with participation, attrition, and outcome in a smoking cessation program at the workplace. Health Psychol. 1988;7(6):575–89. doi: 10.1037//0278-6133.7.6.575. [DOI] [PubMed] [Google Scholar]
- 4.Carlson LE, Taenzer P, Koopmans J, Bultz BD. Eight-year follow-up of a community-based large group behavioral smoking cessation intervention. Addict Behav. 2000 Sep-Oct;25(5):725–41. doi: 10.1016/s0306-4603(00)00081-2. [DOI] [PubMed] [Google Scholar]
- 5.Becona E, Vazquez FL. The course of relapse across 36 months for smokers from a smoking-cessation program. Psychol Rep. 1998 Feb;8(1):143–6. doi: 10.2466/pr0.1998.82.1.143. [DOI] [PubMed] [Google Scholar]
- 6.Baillie AJ, Mattick RP, Hall W. Quitting smoking: estimation by meta-analysis of the rate of unaided smoking cessation. Aust J Public Health. 1995 Apr;19(2):129–31. doi: 10.1111/j.1753-6405.1995.tb00361.x. [DOI] [PubMed] [Google Scholar]
- 7.Richmond RL, Makinson RJ, Kehoe LA, Guigni AA, Webster IW. One-year evaluation of three smoking cessation interventions administered by general practitioners. Addict Behav. 1993 Mar-Apr;18(2):187–99. doi: 10.1016/0306-4603(93)90049-f. [DOI] [PubMed] [Google Scholar]
- 8.Ockene JK, Kristeller J, Pbert L, et al. The physician-delivered smoking intervention project: can short-term interventions produce long-term effects for a general outpatient population? Health Psychol. 1994 May;13(3):278–81. doi: 10.1037//0278-6133.13.3.278. [DOI] [PubMed] [Google Scholar]
- 9.Curry SJ, Grothaus LC, McAfee T, Pabiniak C. Use and cost effectiveness of smoking-cessation services under four insurance plans in a health maintenance organization. N Engl J Med. 1998 Sep 3;339(10):673–9. doi: 10.1056/NEJM199809033391006. [DOI] [PubMed] [Google Scholar]
- 10.Sidorov J, Christianson M, Girolami S, Wydra C. A successful tobacco cessation program led by primary care nurses in a managed care setting. Am J Manag Care. 1997 Feb;3(2):207–14. [PubMed] [Google Scholar]
- 11.Joslin KA, Fleszar GJ, Malone NT, Owens SK. Report of two smoking cessation programs: telephone intervention and group sessions. HMO Pract. 1995 Sep;9(3):134–7. [PubMed] [Google Scholar]
- 12.Fiscella K, Franks P. Cost-effectiveness of the transdermal nicotine patch as an adjunct to physicians’ smoking cessation counseling. JAMA. 1996 Apr 24;275(16):1247–51. [PubMed] [Google Scholar]
- 13.Hurt RD, Dale LC, Fredrickson PA, et al. Nicotine patch therapy for smoking cessation combined with physician advice and nurse follow-up. One-year outcome and percentage of nicotine replacement. JAMA. 1994 Feb 23;271(8):595–600. [PubMed] [Google Scholar]
- 14.Daughton D, Susman J, Sitorius M, et al. Transdermal nicotine therapy and primary care. Importance of counseling, demographic, and participant selection factors on 1-year quit rates. The Nebraska Primary Practice Smoking Cessation Trial Group. Arch Fam Med. 1998 Sep-Oct;7(5):425–30. doi: 10.1001/archfami.7.5.425. [DOI] [PubMed] [Google Scholar]
- 15.Silagy C, Lancaster T, Stead L, Mant D, Fowler G. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2003;(3):CD000146. doi: 10.1002/14651858.CD000146.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Brownson RC, Hopkins DP, Wakefield MA. Effects of smoking restrictions in the workplace. Annu Rev Public Health. 2002;23:333–48. doi: 10.1146/annurev.publhealth.23.100901.140551. Epub 2001 Oct 25. [DOI] [PubMed] [Google Scholar]
- 17.Cummings KM, Jaen CR, Giovino G. Circumstances surrounding relapse in a group of recent exsmokers. Prev Med. 1985 Mar;14(2):195–202. doi: 10.1016/0091-7435(85)90035-0. [DOI] [PubMed] [Google Scholar]
- 18.Derby CA, Lasater TM, Vass K, Gonzalez S, Carleton RA. Characteristics of smokers who attempt to quit and of those who recently succeeded. Am J Prev Med. 1994 Nov-Dec;10(6):327–34. [PubMed] [Google Scholar]
- 19.Gilpin EA, White MM, Farkas AJ, Pierce JP. Home smoking restrictions: which smokers have them and how they are associated with smoking behavior. Nicotine Tob Res. 1999 Jun;1(2):153–62. doi: 10.1080/14622299050011261. [DOI] [PubMed] [Google Scholar]
- 20.Hymowitz N, Sexton M, Ockene J, Grandits G. Baseline factors associated with smoking cessation and relapse. MRFIT Research Group. Prev Med. 1991 Sep;20(5):590–601. doi: 10.1016/0091-7435(91)90057-b. [DOI] [PubMed] [Google Scholar]
- 21.Hymowitz N, Cummings KM, Hyland A, Lynn WR, Pechacek TF, Hartwell TD. Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tob Control. 1997;6(Suppl 2):S57–S62. doi: 10.1136/tc.6.suppl_2.s57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schiffman S, Gnys M, Richards TJ, Paty JA, Hickcox M, Kassel JD. Temptations to smoke after quitting: a comparison of lapsers and maintainers. Health Psychol. 1996 Nov;15(6):455–61. doi: 10.1037//0278-6133.15.6.455. [DOI] [PubMed] [Google Scholar]
- 23.Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V, Baker T. Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. Agency for Health Care Policy and Research. JAMA. 1997 Dec 3;278(21):1759–66. [PubMed] [Google Scholar]
- 24.Warner KE. Cost effectiveness of smoking-cessation therapies. Interpretation of the evidence and implications for coverage. Pharmacoeconomics. 1997 Jun;11(6):538–49. doi: 10.2165/00019053-199711060-00003. [DOI] [PubMed] [Google Scholar]
- 25.Weiss SJ, Jurs S, Lesage JP, Iverson DC. A cost-benefit analysis of a smoking cessation program. Eval Program Plann. 1984;7(4):337–46. doi: 10.1016/0149-7189(84)90058-2. [DOI] [PubMed] [Google Scholar]
- 26.Gariti P, Alterman AI, Ehrman R, Mulvaney FD, O’Brien CP. Detecting smoking following smoking cessation treatment. Drug Alcohol Depend. 2002 Jan 1;65(2):191–6. doi: 10.1016/s0376-8716(01)00162-4. [DOI] [PubMed] [Google Scholar]
- 27.Murray RP, Connett JE, Lauger GG, Voelker HT. Error in smoking measures: effects of intervention on relations of cotinine and carbon monoxide to self-reported smoking. The Lung Health Study Research Group. Am J Public Health. 1993 Sep;83(9):1251–7. doi: 10.2105/ajph.83.9.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murray RP, Connett JE, Istvan JA, Nides MA, Rempel-Rossum S. Relations of cotinine and carbon monoxide to self-reported smoking in a cohort of smokers and ex-smokers followed over 5 years. Nicotine Tob Res. 2002 Aug;4(3):287–94. doi: 10.1080/14622200210141266. [DOI] [PubMed] [Google Scholar]
- 29.Perez-Stable EJ, Marin G, Marin BV, Benowitz NL. Misclassification of smoking status by self-reported cigarette consumption. Am Rev Respir Dis. 1992 Jan;145(1):53–7. doi: 10.1164/ajrccm/145.1.53. [DOI] [PubMed] [Google Scholar]
- 30.Wagenknecht LE, Burke GL, Perkins LL, Haley NJ, Friedman GD. Misclassification of smoking status in the CARDIA study: a comparison of self-report with serum cotinine levels. Am J Public Health. 1992 Jan;82(1):33–6. doi: 10.2105/ajph.82.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]


