Abstract
Cardiovascular rehabilitation (CR) has been designed to decrease the burden of cardiovascular disease. This study described (1) patient-healthcare provider (HCP) interactions regarding CR, and (2) which discussion elements were related to patient referral. This was a prospective study of cardiovascular patients and their HCPs. Discussion utterances were coded using the Roter Interaction Analysis System. Discussion between 26 HCPs and 50 patients were recorded. CR referral was related to greater HCP interactivity (Odds Ratio [OR]=2.82, 95% CI 1.01–7.86), and less patient concern and worry (OR=0.64, 95% CI 0.45–0.89). Taking time for reciprocal discussion and allaying patient anxiety may promote greater referral.
Introduction
Cardiovascular disease, including coronary artery disease (CAD) and stroke, are among the leading causes of morbidity and mortality globally (World Health Organization, 2011). CAD and transient ischemic attack or mild, non-disabling stroke have similar atherosclerotic etiology and modifiable risk factors. As such, similar to secondary prevention for CAD, recurrent vascular events in stroke patients can be prevented with an exercise-based, lifestyle intervention in combination with medication therapies (Prior et al., 2011; Sacco et al., 2006).
Comprehensive chronic disease management programs, such as outpatient cardiovascular rehabilitation (CR), play an integral role in augmenting recovery. CR involves structured exercise training, education, risk factor reduction and behavior change counseling. Participation in CR programs have been shown to reduce mortality by about 25%–30% and to have favorable effects on re-hospitalization and functional capacity (Grace et al., 2008). Emerging evidence supports the feasibility, safety and benefits of CR for transient ischemic attack/mild non-disabling stroke patients as well (Lennon et al., 2008; Prior et al., 2011; Tang et al., 2010).
However, despite the evidence of CR benefit (Heran et al., 2011) in multiple domains and clinical guideline recommendations to refer patients (Thomas et al., 2010), only 15–30% of CAD patients access CR (Grace et al., 2002). Referral to CR, involving form completion and submission by a healthcare provider (HCP), is required to initiate patient access (Arena et al., 2012; Balady et al., 2011; Grace et al., 2011). The patient should be informed that the referral is being submitted (i.e., CR referral discussion), and to expect a phone call at home from the program in the week or so post-discharge. Moreover, the strength of physician endorsement of CR when patients are being informed of the referral has long been known to be related to greater use (Ades et al., 1992; Tsui et al., 2012). However, to date, the verbal and non-verbal aspects of these discussions have not been characterized, and thus it is unknown how the nature of these discussions may influence patient referral (McCorry et al., 2009). Accordingly, the objectives of this study were to: (1) describe patient-HCP discussions regarding CR from multiple perspectives (i.e., patient, HCP, and researcher), and (2) identify elements of the patient-HCP interaction which distinguished between patients who were referred to CR versus those who were not.
Methods
Design and procedure
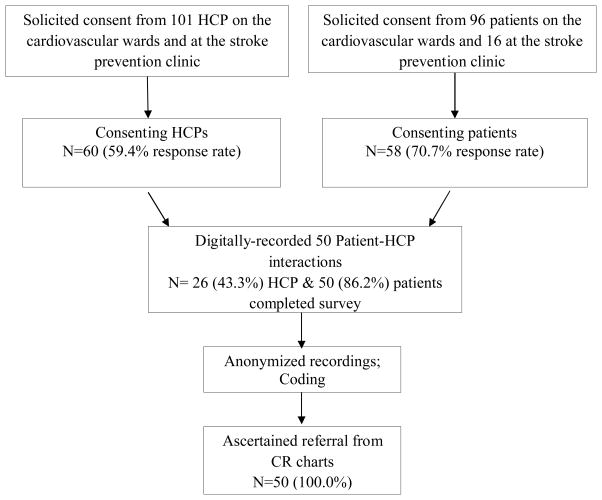
This was an observational, prospective study of cardiovascular patients and their HCPs recruited between September 2011 to November 2012 from three hospitals (two academic) in Southern Ontario. Ethics approval was granted by all participating organizations’ research ethics boards. A diagram depicting study flow is shown in Figure 1.
Figure 1.
Study Flow Diagram
The setting consisted of the non-intensive cardiovascular care units at all 3 institutions and at the Stroke Prevention Clinic at the community hospital. The academic hospitals had separate wards for surgical patients and those undergoing percutaneous coronary interventions. There was some variation in referral strategies between the units, with one unit having electronic referral through inclusion dictation on the discharge summary which is then made accessible to the CR staff. Another unit had a liaison nurse from the CR program who would meet with inpatients several days a week to discuss CR. Most used fax of a written referral form. As part of CR practice, program staff intermittently offer education sessions to the inpatient HCPs on these units regarding the referral process to the affiliated CR program, and Canadian policy recommending inpatient rather than outpatient CR referral (Grace et al., 2011). One academic centre was a quaternary facility. Given the geographic distribution of the patients treated, inpatient HCPs were directed to refer all patients to the affiliated CR program, who would then triage referrals to the site closest to their home.
HCPs were approached via email and in-services to solicit informed consent to participate. Upon HCP consent, a research assistant approached cardiovascular patients inviting them to participate in the study on the days a consenting HCP was working. Once both a provider and corresponding patient was consented, a coloured poster was mounted on the wall of the patient’s room. Willing HCPs and/or patients were asked to carry a numbered digital recorder throughout the day, and to turn it on and off at the beginning and end of their interaction, respectively. Therefore when the HCP next entered the patients room, were alerted to audio-record their interaction. For those patients undergoing intervention, discussions were only recorded post-procedure.
After the patient-HCP dialogue had been recorded, patients were asked to complete a self-report survey. It assessed sociodemographic characteristics, as well as attitudes and perceptions towards their HCP and their CR conversation. Clinical characteristics were extracted from patient charts. The participating HCPs were similarly asked to complete a self-report survey, assessing their perceptions of the specific medical encounter.
All audio-recordings of the HCP-patient discussions were anonymized. These were then emailed through a secure file portal for external coding based on the Roter Interaction Analysis System (RIAS) (Roter and Larson, 2002; RIASWorks, 2012). One RIAS coder categorized interactions according to the 41 standard RIAS categories. A second RIAS coder audited the coding trail on a random subset of audio-recordings, to ensure data quality and to establish the RIAS’ reliability in this setting.
Finally, CR charts were audited at the institutional programs 2 months later. Where a patient was not referred, patients were telephoned at home to ascertain whether they had been referred to another CR program.
Participants
Participants and HCPs were approached on the cardiovascular units and at the Stroke Prevention Clinic to participate. HCP participants included all those working on the cardiac inpatient units, including surgical and interventional wards, as well as the outpatient Stroke Prevention Clinic. This included physicians, nurse-practitioners, nurses, and allied healthcare professionals (e.g., physiotherapists). In addition, peer mentors from the surgical ward who were registered with volunteer services were approached, given recent evidence that they can have a positive effect on CR use (Scott et al., 2013). While CR referral is only in the scope of physician and nurse-practitioner practice in Ontario, it is generally nurses or allied health professionals who discuss CR with patients and draft CR referral forms for their signature (Grace et al., 2004). The exclusion criterion was that the HCPs were not involved in direct patient care (i.e., nurse managers).
Patient inclusion criteria were: age 18 years or older, and having a clinical indication for CR based on clinical practice guidelines (e.g., acute coronary syndrome, post-procedure such as percutaneous coronary intervention or coronary artery bypass grafting surgery) (Stone et al., 2009). In the case of stroke patients, those with transient ischemic attacks and mild non-disabling strokes were eligible. Exclusion criteria were: (1) patients who were not eligible for CR due to comorbid musculoskeletal, neuromuscular, visual, cognitive or non-dysphoric psychiatric conditions (i.e., schizophrenia, advanced dementia), (2) being discharged to long-term care, (3) any serious or terminal illness not otherwise specified which would preclude CR participation (Stone et al., 2009), and (4) limited English-language proficiency. In addition, stroke patients who were unable to ambulate, and hence participate fully in CR, were excluded.
Measures
HCP characteristics
HCPs were asked to report their profession, highest degree obtained, year they graduated from their most advanced degree, sex, and estimated average number of patients seen in person daily.
Patient sociodemographic and clinical characteristics
On the survey, patients were asked to report their age, sex, marital status, racial/ethnic background, work status, and highest level of education. The survey also included the MacArthur Scale of Subjective Socioeconomic Status (John and MacArthur, 2000), where participants were asked to demarcate their perceived status compared to others in Canada. Scale scores ranged from 1 to 10, with higher scores indicating greater subjective socioeconomic status (SES). A median split was computed, to categorize participants as high versus low subjective SES.
With regard to clinical characteristics, the survey also included the Duke Activity Status Index (DASI) (Hlatky et al., 1989), a brief 12-item self-administered survey used to determine functional capacity. The DASI inquires about a patient’s ability to perform common activities of daily living, such as personal care, ambulation, household tasks, sexual function, and recreational activities, which are each associated with specific metabolic equivalents. This valid and common tool correlates highly with peak oxygen uptake (Nelson et al., 1991). Finally, clinical variables abstracted from patient medical charts included: index cardiovascular condition, risk factors, and previous history of cardiovascular disease.
HCP and patient perceptions of audio-recorded discussions
The HCP self-report survey assessed their perception of the quality of the audio-recorded interaction with their cardiovascular patient through investigator-generated items. This was measured on a 5-point Likert scale, from “poor” to “excellent”, with higher scores indicating greater perceived quality. Additionally, HCP were asked whether the patient with whom they interacted will be referred to CR (yes/no).
The patient self-report surveys included items assessing their: (a) perceptions of HCP endorsement of CR, (b) awareness of CR, (c) perception of degree of patient-centeredness of the interaction, (d) perception of the likelihood they will be referred to CR, and (e) intentions to enroll in a CR program. These investigator-generated items were assessed on a 5-point Likert scale, with greater scores indicating higher endorsement of the given construct. In order to further assess patient perception of their interaction, the following 4 items were administered: To what extent did your HCP (a) ‘involve you as an equal partner in making decisions about illness management strategies and goals?’; (b) ‘Did your HCP listen carefully to what you had to say about your illness?’; (c) ‘Did your HCP encourage you to go to a specific group or class to help you manage your health condition?’; and (d) ‘Did your HCP convey that what you do to take care of yourself, influences your health condition?’. These were measured on a 5-point Likert scale, from “not at all” to “a great deal”. Finally, patients were asked if any family members were present during the audio-recorded interaction (yes/no).
Interaction analysis
To quantify the dialogue between patients and HCPs, RIAS-trained coders analyzed audio-recordings externally. RIAS is a standardized method of coding medical dialogue. It has been validated in several countries and healthcare settings (Roter and Larson, 2002), including in cardiac surgery patients. (Van Weert et al., 2003) The RIAS has been shown to be both reliable and valid (Roter and Larson, 2002).
The unit of analysis was an utterance, defined as the smallest discriminable speech segment to which a coder could assign a classification, and which expressed or implied a complete thought. This could vary from a single word, to a phrase, or a complete sentence. All utterances were assigned to 1 of the 29 mutually-exclusive and exhaustive categories for the patient, and 1 of 41 categories for the HCP. The broad categories are: data gathering, patient education and counselling, facilitation and patient activation, rapport building and procedural.
Firstly, with regard to data gathering, these were utterances where patients described their condition in their own words, allowing HCPs to understand and ask the appropriate questions regarding their concerns. Data gathering questions were categorized as open or closed-ended. These utterances were also categorized as medical (e.g., “What can you tell me about the pain?”), therapeutic (e.g., “How are you doing with the pain medication?”), lifestyle (e.g., “Who’s living at home with you now?), or psychosocial (e.g., “Are you anxious about leaving the hospital”).
Second, patient education and counseling statements refer to utterances to facilitate patient’s understanding about their illness, and to motivate them to follow treatment recommendations. These utterances were also grouped into biomedical (i.e., medical condition, or therapeutic regimen) and psychosocial (i.e., lifestyle, or psychosocial issues) subcategories (e.g., “Getting exercise now is a good idea, especially now”- psychosocial counseling; “I’ve been working out in the yard most days” – lifestyle counseling; “My grandfather died of heart disease”- medical).
Third, facilitation and patient activation and partnership-building include participatory facilitators (i.e., asking for patient opinion, asking for understanding, paraphrases, back-channels) and procedural talk (i.e., orientation, transitions) to improve the patients’ ability to connect in an affective partnership with their HCP (e.g., “What do you think?” – asks for opinion; “Do you follow me?”- asks for understanding; “Mmm-huh, right, go on. “- back-channels; “Ah…wait a minute now…”- transitions). Lastly, rapport-building, fell within the scope of social talk (e.g., “How about the weather the past few days”- non-medical topic), positive talk (e.g., “I might get blown away in a strong wind”-laughter; “You look fantastic, you are doing great”- approvals), negative talk (e.g., “I think you are wrong, you were not being careful”- criticism; “Don’t say I didn’t warn you” –disagreement) and emotional talk (i.e., “I just want to know if I’m heading for the hospital again”- concern, worry; “I wouldn’t worry about it, you’ll be feeling better before you know it”- reassurance).
Finally, RIAS coders rated the global affect (i.e., the tonal qualities of the interaction) of each audio-recording. These tonal qualities transmit the emotional context of the audio-recording beyond the significance of the words spoken. Coders rated both the patient and HCP on a range of global affective dimensions including anger, anxiety, dominance, interest, friendliness, and interactivity. These were rated on a 5-point Likert scale from “low” to “high”.
Dependent variable
CR charts were audited at the institutions’ programs, to ascertain whether a referral to the program was received or not (yes/no). For the academic hospitals, the source of the referral was also noted, to ascertain whether the referral had been generated during the inpatient stay (yes/no). Where there was no documentation of referral, patients were telephoned at home to ascertain whether they had been referred to another CR program.
Statistical analyses
SPSS version 20.0 was used for all analyses (IBM Corp., 2011). Data were summarized with percentages for categorical variables, and by mean with standard deviation for continuous variables. Since the assumption of homogeneity of variance could not be assumed, non-parametric tests were applied (i.e., Mann-Whitney U or chi-square, as appropriate). P< 0.05 was used for all tests to indicate statistical significance. An initial descriptive analysis of HCP and patient characteristics was performed.
To test the first objective, a descriptive examination of patient and HCP perceptions of the interaction, and RIAS coding categories was performed. Cohen’s kappa was computed to ascertain the degree of concordance between HCP perception of patient referral and CR chart-reported referral.
To test the final objective, first, the CR referral rate was described. Next, HCP characteristics and perceptions were compared by the referral status of their patient (yes/no). Patient characteristics, attitudes and perceptions were similarly compared by CR referral. Moreover, RIAS coding was compared by CR referral. Finally, binary logistic regression analysis was used to examine the association of patient and RIAS factors identified as significantly related with CR referral (dependent variable) through the previous analysis. Any HCP characteristics significantly related to CR referral were excluded from the model, as there was insufficient power to compute generalized estimating equations, which would be required to take into consideration of the nesting of patients by HCPs. Odds ratios (OR) with 95% confidence intervals (CI) were reported.
Results
Respondent characteristics
A diagram of study flow is shown in Figure 1. Of the 101 HCPs approached, 60 consented to participate in the study (59.4% response rate). Of these, valid audio-recordings were obtained with 26 (43.3%) HCPs. Their sociodemographic and work-related characteristics are summarized in Table 1. The primary healthcare professional audio-recorded was nurses (n=13, 50.0%). Other professions represented in the sample were: nurse-practitioners (n=5, 19.2%), cardiologists (n=2, 7.7%), physiotherapists (n=2, 7.7%), peer mentors (n=2, 7.7%), a dietitian (n=1, 3.8%), and a pharmacist (n=1, 3.8%). Thus, 7 (26.9%) HCPs had CR referral within their scope of practice.
Table 1.
Participating Healthcare Provider Characteristics, as well as Attitudes and Perceptions Related to CR
| Patient CR Referral | ||||
|---|---|---|---|---|
|
| ||||
| Characteristics | Total N=26 |
Yes n=35 (70.0%) |
No n=15 (30.0%) |
p |
| Sex (% female) | 19 (73.1) | 11 (78.6) | 8 (66.7) | 0.50 |
| Highest Degree Obtained (% undergraduate degree) | 9 (34.6) | 4 (28.6) | 5 (41.7) | 0.19 |
| Year obtained highest academic qualification | 1992±15 | 1993±14 | 1990±16 | 0.66 |
| Profession (% nurse) | 13 (50.0) | 8 (57.1) | 5 (41.7) | 0.45 |
| Estimated number of patients seen/day | 8.19±5.48 | 5.50±1.61 | 11.33±6.72 | <.05 |
| Mean % of eligible patients referred or recommended to CR | 77.83±29.25 | 81.08±27.89 | 74.58±31.44 | 0.77 |
| CR awarenessa (mean ± SD) | 3.96±0.77 | 4.00±0.78 | 3.92±0.79 | 0.78 |
Note: CR: Cardiac Rehabilitation;
Evaluated on a 5-point Likert scale from “poor” to “excellent”
Of these referring HCP, 10 (66.7%) of the patients with whom they interacted were referred to CR. For non-referring HCPs, 25 (71.4%) of the patients were referred to CR (p=0.74). When asked what percentage of their eligible patients do they refer or recommend for referral, referring HCPs reported 75.71±31.01 and non-referring HCPs reported 78.71±29.44 (p=0.60). When asked to rate their perceptions of the interaction quality from 1 “poor” to 5 “excellent”, referring HCPs reported 3.00±1.00 and non-referring HCPs reported 3.37±0.96 (p=0.40). When asked whether the patient with whom they interacted will be referred to CR, 11 (28.2%) referring HCPs responded affirmatively, and 28 (71.8%) non-referring HCPs responded affirmatively (p=0.24).
One hundred and twelve patients were approached, of whom 58 (70.7% response rate) were considered eligible, and consented. Twenty-four (21.4%) patients declined to participate, and 30 (26.8%) were considered ineligible, for the following reasons: insufficient English-language proficiency (n=21, 70.0%), imminent discharge (n=1, 3.3%), patient already referred to CR (n=1, 3.3%), vision problems (n=1, 3.3%), and patient not cognitively-oriented to time and place (n=1, 3.3%). Of the participating patients, for two (6.7%) the tape quality was insufficient for coding both speakers, one (3.3%) patient’s HCP changed, one (3.3%) patient was transferred to another hospital, and one (3.3%) patient did not have an interaction with a consenting HCP before discharge, and thus these 5 patients were subsequently excluded. The resultant sample size is 50 patients. Their sociodemographic and clinical characteristics are summarized in Table 2.
Table 2.
Sociodemographic and Clinical Characteristics of Patients
| Characteristics | Patient CR Referral | |||
|---|---|---|---|---|
|
| ||||
| Total N=50 |
Yes n=35 (70.0%) |
No n=15 (30.0%) |
p | |
| Sociodemographic | ||||
| Age, years (mean ± SD) | 65.48±12.95 | 66.37±10.36 | 63.40±17.87 | 0.88 |
| Sex (% female) | 14(28.0) | 8 (22.9) | 6 (40.0) | 0.22 |
| Marital Status (% married) | 33 (66.0) | 24 (68.6) | 9 (60.0) | 0.56 |
| Ethnicity (% white/Caucasian) | 27 (54.0) | 19 (54.3) | 8 (53.3) | 0.95 |
| Work Status (% retired) | 35 (70.0) | 22 (62.9) | 13 (86.7) | 0.09 |
| Education (% post-secondary) | 17 (34.0) | 9 (25.7) | 8 (53.3) | 0.06 |
| Subjective SES/10 (mean ± SD) | 6.55±1.31 | 6.65±1.32 | 6.33±1.29 | 0.22 |
| Clinical | ||||
| CR Indication | ||||
| PCI (%) | 23 (46.0) | 19 (54.3) | 4 (26.7) | 0.07 |
| Stroke (%) | 8 (19.5) | 5 (17.2) | 3 (25.0) | 0.57 |
| HF (%) | 7 (14.0) | 5 (14.3) | 2 (13.3) | 0.93 |
| MI (%) | 4 (8.2) | 2 (5.9) | 2 (13.3) | 0.38 |
| BMI (mean ± SD) | 27.36±5.35 | 28.04±5.62 | 25.81±4.45 | 0.16 |
| Diabetes (%) | 15 (30.6) | 132 (35.3) | 2 (20.0) | 0.28 |
| Hypertension (%) | 33 (66.0) | 26 (74.3) | 7 (46.7) | 0.06 |
| Dyslipidemia (%) | 32 (64.0) | 25 (71.4) | 7 (46.7) | 0.10 |
| Previous CAD (%) | 24 (48.0) | 19 (54.3) | 5 (33.3) | 0.17 |
| DASI (mean ± SD) | 29.58±15.56 | 29.68±15.67 | 29.34±15.83 | 0.76 |
| Patient Perception of CR | ||||
| Perceived strength of CR endorsement/5, (mean ± SD) | 4.07±0.72 | 4.00±0.78 | 4.27±0.47 | 0.34 |
| Perceives they will be referred (%yes) | 38 (86.4) | 30 (88.2) | 8 (80.0) | 0.51 |
| Intention to enroll /5, (mean ± SD) | 3.49±1.44 | 3.61±1.34 | 3.21±1.67 | 0.53 |
| CR awareness /5, (mean ± SD) | 3.22±1.34 | 3.15±1.33 | 3.40±1.40 | 0.52 |
| HCP- Patient Audio-recoding Experience | ||||
| Involve you as an equal partner in making decisions about illness management strategies and goals?b | 4.04±1.00 | 4.20±0.90 | 3.64±1.15 | 0.11 |
| Listen carefully to what you had to say about your illness?b | 4.29±0.91 | 4.40±0.77 | 4.00±1.18 | 0.33 |
| Encourage you to go to a specific group or class to help you manage your health condition?b | 4.12±1.13 | 4.40±0.74 | 3.43±1.60 | <.05 |
| Convey that what you should do to take care of yourself influences your health condition?b | 4.27±0.91 | 4.46±0.74 | 3.79±1.12 | <.05 |
| Patient-centeredness of interaction c, (mean ± SD) /5 | 4.29±0.94 | 4.44±0.75 | 3.93±1.27 | 0.20 |
| Family present during audio-recorded discussion (% yes) | 26 (53.1) | 18 (51.4) | 8 (57.1) | 0.72 |
Note: SES: Socioeconomic Status; PCI: Percutaneous Coronary Intervention; HF: Heart Failure; MI: Myocardial Infarction; BMI: Body mass index; CAD: Coronary Artery Disease; DASI: Duke Activity Status Index; CR: Cardiac Rehabilitation; HCP: Healthcare provider; SD: Standard Deviation;
Chi-square test for categorical variables and Man-Whitney U were performed for continuous variables by CR referral
Participants were asked “To what extent did your healthcare provider involve you as an equal partner in making decision about illness management strategies and goals? To what extent did your healthcare provider listen carefully to what you had to say about your illness? To what extent did you healthcare provider encourage you to go to a specific group or class to help you manage your heart condition? Did you healthcare provider convey that what you do to take care of yourself, influences your heart condition?” Scores ranged from 1 “not at all” to 5 “a great deal”
Participants were asked “To rate your perception of the patient-centeredness of the interaction?” Scores ranged from 1”poor” to 5 “excellent”
Patient-HCP discussions
Of the 50 recorded discussions, 12 (46.2%) HCPs were recorded once, 7 (26.9%) HCPs were recorded twice (i.e., with 2 different patients), 4 (15.4%) were recorded three times, 1 (3.8%) was recorded four times, 1 (3.8%) was recorded six times, and 1 (3.8%) was recorded seven times. The discussions were on average 8.93±8.84 (standard deviation) minutes in length. Forty-one (82.0%) recordings mentioned CR.
With regard to objective one, HCPs perceived the quality of interaction as 3.38±0.99 on a 5-point Likert scale. Patient perceptions of the interaction are shown at the bottom of Table 2.
Table 3 displays the average frequency of each element of the discussions uttered by both HCPs and patients based on the RIAS coding. A second RIAS coder audited the coding trail on a random subset (n=7 cases) of audio-recordings, to ensure data quality and to establish the RIAS’ reliability in the CR setting. The average inter-rater reliability was 0.896 for HCP talk and 0.924 for patient talk. Reliability of global affect ratings was reported at 100% percent agreement (within one-point on the rating scale).
Table 3.
Mean Frequency (± standard deviation) of RIAS Discussion Elements and Global Affect Ratings* by CR Referral, in Descending Order
| Patient CR Referral | ||||
|---|---|---|---|---|
|
| ||||
| Code | Total N=50 |
Referred to CR n=35 (70.0%) |
Not Referred to CR n=15 (30.0%) |
p |
| HCP: Gives information- therapeutic | 38.38±36.97 | 42.29±37.91 | 29.27±34.14 | 0.08 |
|
| ||||
| Pt: Shows agreement, understanding | 33.20±29.44 | 36.26±30.59 | 26.07±26.13 | 0.20 |
|
| ||||
| HCP: Counsels- medical/therapeutic | 14.20±19.98 | 16.29±20.99 | 9.33±17.04 | 0.14 |
| HCP: Shows agreement, understanding | 11.94±12.81 | 13.37±14.68 | 8.60±5.84 | 0.35 |
|
| ||||
| Pt: Gives information- lifestyle | 10.16±12.84 | 8.89±12.27 | 13.13±14.07 | 0.30 |
|
| ||||
| HCP: Back-channels | 9.84±9.10 | 9.11±9.81 | 11.53±7.22 | 0.09 |
|
| ||||
| Pt: Gives information- medical | 8.86±12.50 | 9.49±14.31 | 7.40±6.76 | 0.53 |
| Pt: Gives information- therapeutic | 8.10±8.15 | 7.83±7.93 | 8.73±8.91 | 0.77 |
|
| ||||
| HCP: Counsels- lifestyle/ psychosocial | 6.82±17.38 | 8.60±20.46 | 2.67±3.70 | 0.41 |
| HCP: Paraphrase, checks for understanding | 6.52±9.36 | 6.97±10.70 | 5.47±5.21 | 1.00 |
| HCP: Gives information- medical | 6.28±10.41 | 7.20±11.70 | 4.13±6.32 | 0.34 |
| HCP: Gives information- lifestyle | 5.82±7.44 | 5.63±6.76 | 6.27±9.09 | 0.75 |
| HCP: Reassures, optimism | 5.32±6.52 | 4.80±6.97 | 6.53±5.34 | 0.06 |
| HCP: gives orientation, instructions | 5.08±8.67 | 5.91±10.11 | 3.13±3.02 | 0.66 |
| HCP: Ask for understanding | 4.50±6.53 | 5.09±7.31 | 3.13±4.07 | 0.45 |
|
| ||||
| Pt: Interest/ attentiveness* | 4.36±0.69 | 4.29±0.67 | 4.53±0.74 | 0.17 |
| Pt: Paraphrase, checks for understanding | 3.82±4.65 | 4.20±4.95 | 2.93±3.90 | 0.24 |
|
| ||||
| HCP: Friendliness/ warmth | 3.82±0.69 | 3.89±0.72 | 3.67±0.62 | 0.33 |
| HCP: Interactivity* | 3.72±0.88 | 3.89±0.83 | 3.33±0.90 | <.05 |
|
| ||||
| Pt: Friendliness/warmth | 3.72±0.70 | 3.71±0.71 | 3.73±0.70 | 0.91 |
|
| ||||
| HCP: Responsiveness/ engagement | 3.70±0.84 | 3.80±0.83 | 3.47±0.83 | 0.22 |
| HCP: Sympathetic/ empathetic | 3.62±0.60 | 3.57±0.61 | 3.73±0.59 | 0.35 |
|
| ||||
| Pt: All questions –therapeutic | 3.54±4.90 | 4.00±5.49 | 2.47±3.04 | 0.41 |
|
| ||||
| HCP: Dominance/ assertiveness | 3.44±0.54 | 3.51±0.51 | 3.27±0.59 | 0.17 |
|
| ||||
| Pt: Interactivity | 3.30±0.79 | 3.37±0.81 | 3.13±0.74 | 0.40 |
| Pt: Responsiveness /engagement | 3.28±0.70 | 3.37±0.69 | 3.07±0.70 | 0.20 |
|
| ||||
| HCP: Hurried/ rushed | 3.28±1.34 | 3.11±1.32 | 3.67±1.35 | 0.14 |
|
| ||||
| Pt: Dominance/ assertiveness | 3.22±0.51 | 3.20±0.53 | 3.27±0.46 | 0.72 |
|
| ||||
| HCP: Concern, worry | 3.16±5.34 | 3.66±6.03 | 2.00±3.02 | 0.59 |
|
| ||||
| Pt: Reassures, optimism | 3.04±2.70 | 2.63±2.18 | 4.00±3.55 | 0.27 |
|
| ||||
| HCP: Respectfulness | 3.02±0.14 | 3.03±0.17 | 3.00±0.00 | 0.51 |
|
| ||||
| Pt: Respectfulness | 3.00±0.29 | 2.97±0.30 | 3.07±0.26 | 0.28 |
| Pt: Sympathetic/empathetic | 2.98±0.14 | 2.97±0.17 | 3.00±0.00 | 0.51 |
|
| ||||
| HCP: Approval- direct | 2.86±3.72 | 2.71±3.74 | 3.20±3.78 | 0.70 |
|
| ||||
| Pt: Laughs, tell jokes | 2.84±4.42 | 2.83±4.36 | 2.87±4.72 | 0.82 |
|
| ||||
| HCP: Closed question- medical | 2.80±4.65 | 3.06±5.37 | 2.20±2.24 | 0.40 |
| HCP: Gives information- psychosocial | 2.38±8.51 | 3.00±10.03 | 0.93±2.46 | 0.95 |
| HCP: Closed question- lifestyle | 2.18±4.22 | 2.46±4.49 | 1.53±3.56 | 0.39 |
| HCP: Transitions | 2.06±2.45 | 2.37±2.67 | 1.33±1.72 | 0.20 |
| HCP: Closed question- therapeutic | 2.04±3.14 | 2.40±3.63 | 1.20±1.21 | 0.69 |
|
| ||||
| Pt: Approval- direct | 2.02±2.85 | 1.80±2.23 | 2.53±4.00 | 0.55 |
| Pt: Unintelligible utterance | 2.00±3.21 | 2.06±3.69 | 1.87±1.77 | 0.39 |
| Pt: Gives information -psychosocial | 2.00±4.38 | 1.66±2.87 | 2.80±6.81 | 0.44 |
| Pt: Concern, worry | 1.80±2.23 | 1.37±1.86 | 2.80±2.73 | <.05 |
|
| ||||
| HCP: Laughs, tells jokes | 1.72±2.29 | 1.71±2.38 | 1.73±2.12 | 0.95 |
| HCP: Personal remarks | 1.68±2.90 | 1.54±2.76 | 2.00±3.30 | 0.77 |
| HCP: Asks for opinion | 1.66±2.02 | 1.91±2.06 | 1.07±1.83 | <.05 |
|
| ||||
| Pt: Anxiety/ nervousness | 1.44±0.64 | 1.40±0.60 | 1.53±0.74 | 0.60 |
| Pt: Personal remarks | 1.14±1.97 | 0.97±1.67 | 1.53±2.56 | 0.54 |
| Patient: Anger/ irritation | 1.02±0.14 | 1.03±0.17 | 1.00±0.00 | 0.51 |
|
| ||||
| HCP: Anger/ irritation | 1.00±0.00 | 1.00±0.00 | 1.00±0.00 | 1.00 |
| HCP: Anxiety/ nervousness | 1.00±0.00 | 1.00±0.00 | 1.00±0.00 | 1.00 |
|
| ||||
| Pt: Emotional distress/ upset | 1.00±0.00 | 1.00±0.00 | 1.00±0.00 | 1.00 |
| Pt: Depression/ sadness | 1.00±0.00 | 1.00±0.00 | 1.00±0.00 | 1.00 |
| Pt: Transitions | 0.86±1.21 | 0.83±1.36 | 0.93±0.80 | 0.21 |
|
| ||||
| HCP: Gives information -other | 0.76±2.08 | 0.51±1.17 | 1.33±3.35 | 0.50 |
| HCP: Open question -medical | 0.72±1.75 | 0.80±1.97 | 0.53±1.13 | 0.75 |
|
| ||||
| Pt: All questions -lifestyle | 0.62±0.95 | 0.74±1.07 | 0.33±0.49 | 0.30 |
| Pt: All questions -medical | 0.52±1.34 | 0.60±1.54 | 0.33±0.72 | 0.77 |
|
| ||||
| HCP: Unintelligible | 0.52±0.95 | 0.40±0.74 | 0.80±1.32 | 0.49 |
|
| ||||
| Pt: Asks for understanding | 0.50±0.84 | 0.46±0.85 | 0.60±0.83 | 0.44 |
| Pt: Gives orientation, instructions | 0.50±0.95 | 0.54±1.04 | 0.40±0.74 | 0.68 |
|
| ||||
| HCP: Open question -therapeutic | 0.46±0.95 | 0.60±1.09 | 0.13±0.35 | 0.13 |
|
| ||||
| Pt: Gives information -other | 0.46±1.33 | 0.49±1.44 | 0.40±1.06 | 0.54 |
| Pt: Disagreement, criticism-direct | 0.42±0.93 | 0.37±0.81 | 0.53±1.19 | 0.89 |
| Pt: Open question -lifestyle | 0.34±1.47 | 0.43±1.74 | 0.13±0.35 | 0.94 |
|
| ||||
| HCP: Closed question -other | 0.32±1.08 | 0.37±1.26 | 0.20±0.41 | 0.73 |
| HCP: Disagreement, criticism - direct | 0.24±0.56 | 0.20±0.47 | 0.33±0.72 | 0.70 |
| HCP: Self-disclosure | 0.20±0.64 | 0.23±0.73 | 0.13±0.35 | 0.91 |
| HCP: Asks for reassurance | 0.20±0.49 | 0.20±0.47 | 0.20±0.56 | 0.79 |
| HCP: Legitimation statements | 0.20±0.64 | 0.17±0.57 | 0.27±0.80 | 0.82 |
|
| ||||
| Pt: Asks for reassurance | 0.18±0.56 | 0.14±0.55 | 0.27±0.59 | 0.27 |
| Pt: Compliment -general | 0.16±0.51 | 0.20±0.58 | 0.07±0.26 | 0.57 |
| Pt: All questions -psychosocial | 0.16±0.62 | 0.20±0.72 | 0.07±0.26 | 0.79 |
|
| ||||
| HCP: Bid for repetition | 0.14±0.53 | 0.14±0.55 | 0.13±0.52 | 0.84 |
| HCP: Compliment- general | 0.14±0.64 | 0.03±0.17 | 0.40±1.12 | 0.14 |
|
| ||||
| Pt: Disagreement, criticism-general | 0.14±0.40 | 0.14±0.43 | 0.13±0.35 | 0.88 |
|
| ||||
| HCP: Closed question -psychosocial | 0.12±0.33 | 0.09±0.28 | 0.20±0.41 | 0.26 |
| HCP: Asks for permission | 0.12±0.39 | 0.17±0.45 | 0.00±0.00 | 0.13 |
| HCP: Open question -psychosocial | 0.12±0.39 | 0.14±0.43 | 0.07±0.26 | 0.60 |
| HCP: Partnership statements | 0.12±0.33 | 0.11±0.32 | 0.13±0.35 | 0.85 |
|
| ||||
| Pt: All questions -other | 0.10±0.36 | 0.09±0.37 | 0.13±0.35 | 0.39 |
|
| ||||
| HCP: Empathy statements | 0.08±0.34 | 0.06±0.34 | 0.13±0.35 | 0.17 |
| HCP: Disagreements, criticism -general | 0.06±0.31 | 0.09±0.37 | 0.00±0.00 | 0.35 |
|
| ||||
| Pt: Bid for repetition | 0.02±0.14 | 0.00±0.00 | 0.07±0.26 | 0.13 |
Note: Pt: Patient; HCP: Healthcare Provider; RIAS: Roter Analysis Interaction System
Mann-Whitney U comparing mean frequency of RIAS utterances by CR referral
RIAS coding categories not used: Pt talk- Asks for service; Pt talk- Legitimation statements; Pt talk-Empathy statements; HCP talk- Open question- other
CR referral
There were 35 (70.0%) patients referred to CR. Fifteen (30.0%) patients were called as there was no record of CR referral in the program charts. Of these, none reported being referred to another CR site. Of the 34 (68.0%) participants recruited from the academic hospitals, 30 (88.2%) were referred, all from the inpatient unit.
Four (15.4%) HCPs reported they did not know whether their patients were referred. Of those that did know, 20 (76.9%) HCPs perceived their patients were referred. The concordance between HCP perceptions of patient referral with CR referral form receipt at the CR site was 0.095 (Cohen’s κ).
To test the final objective, differences in CR referral rates were explored. Length of recording (p=0.58), as well as HCP sociodemographic and work-related characteristics were unrelated to CR referral (Table 1). However, HCPs who reported treating more patients per day were significantly less likely to refer than those reporting treating fewer patients. With regard to patient characteristics, there were no significant differences in sociodemographic or clinical characteristics between patients who were referred and those who were not (Table 2).
Some patient-reported perceptions of the discussions were significantly related to CR referral (Table 2). As shown, patients who perceived greater encouragement from their HCPs to go to a class to help manage their cardiovascular disease, and those that perceived their HCP more strongly conveyed that their health behaviour will influence their condition, were significantly more often referred to CR.
Based on the RIAS codes, some elements of the discussions were also related to CR referral (Table 3). With regard to HCP utterances, when they more often asked patients for their opinions, patients were more likely to be referred to CR. With regards to patient utterances, those who expressed concern and worry within their discussions, were significantly less likely to be referred to CR. Moreover, the affect-related rating of interactivity was also related to greater CR referral. Finally, there were trends towards greater CR referral where HCPs gave therapeutic information, and provided less reassurance and optimism to patients.
Finally, the logistic regression model testing the effects of these variables in relation to CR referral is presented in Table 4. HCP request for opinion was excluded from the model due to insufficient sample size. As shown in Table 3, this element was not common in the recorded discussion. Moreover, volume of patients per day was also excluded due to concerns regarding intra-class correlations. The logistic regression model was significant overall (F=16.73, p<.01), and the model accounted for 42% of the variance in referral rates (Nagelkerke R2). As shown, patients were almost three times more likely to be referred to CR where HCPs were more interactive in the discussion, and were 36% less likely to be referred if they exhibited more concern and worry during their interaction.
Table 4.
Logistic Regression Model Testing Significance of Discussion Perceptions and Elements by CR Referral
| β | SE | Wald | p | OR | 95% CI | ||
|---|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||||
| Did your HCP encourage you to go to a specific group or class to help you manage your health condition? | 0.66 | 0.61 | 1.17 | 0.28 | 1.94 | 0.58 | 6.48 |
| Did your HCP convey that what you should do to take care of yourself influences your health condition? | 0.14 | 0.84 | 0.03 | 0.86 | 1.16 | 0.22 | 5.99 |
| Pt: Concern, Worry | −0.45 | 0.17 | 6.76 | 0.01 | 0.64 | 0.45 | 0.89 |
| HCP: Interactivity | 1.04 | 0.52 | 3.94 | <0.05 | 2.82 | 1.01 | 7.86 |
Note: CR: Cardiovascular Rehabilitation; HCP: Healthcare Provider; SE: Standard Error; CI: Confidence Interval; OR: Odds Ratio
Discussion and conclusion
Discussion
This is the first study to have examined the nature of patient-HCP communication regarding CR referral. The discussions most-often consisted of nurses and patients sharing information about their care, and showing understanding and agreement. Patients perceived the discussions very positively, but contrarily HCPs perceived the quality of the conversations as low. Moreover, HCPs were not often cognizant of whether or not their patients were referred to CR, and their referral rates were inversely related to their patient care volume. Overall, discussions where patients expressed less worry and HCPs were more interactive were associated with CR referral.
The majority of the interactions were centered on HCPs giving therapeutic information and patients showing agreement and understanding. It was disconcerting that HCPs quite rarely were cognizant whether a patient was referred. The latter can perhaps be explained by the fact that nurses, the most common HCP type in this study, cannot sign-off on a CR referral in the province where the study was conducted. They would have to complete the form and pass it to a nurse-practitioner or physician to sign the form. However, in accordance with a recent statement from the American Heart Association, it is recommended that all HCPs are involved in the referral process, (Arena et al., 2012) so that CR utilization rates can be increased.
The former finding that HCPs were unsatisfied with the quality of the recorded interactions, as well as that having fewer patients under their charge, and engaging in greater interactivity (which was unfortunately not a common occurrence in the recordings), were related to greater patient CR referral, suggests that there may be room to increase the time spent and improve the quality of CR referral discussions at the bedside. This is especially important since HCP endorsement of CR is found to be the principle predictor for both CR referral and enrollment (Ades et al., 1992; Jackson et al., 2005; Shanks et al., 2007). Indeed, previous research has established the importance of interpersonal communication for patient health outcomes and compliance (Bartlett et al., 1984; Burgoon, 1996), and that HCPs can be successfully trained to improve the quality of their communication (Kim et al., 2013; Ratzan, 1996). Indeed, even short-term training, of less than 10 hours, is successful in improving HCP communication skills (Dwamena et al., 2012). While time is certainly limited in the current era of short hospital stays (Mitoff et al., 2005), given the substantive benefits of CR (Taylor et al., 2004), and that adoption of other secondary prevention measures post-hospitalization are much higher than they are for CR (Kottke et al., 2009), it is imperative that we develop some proven strategies to ensure CR referral and enrollment-enhancing patient communication before every indicated patient is discharged.
Caution is warranted when interpreting these results. First, the study was limited in the small number of audio-recorded discussions. It is possible that other conversational elements were related to CR referral, but that the study was underpowered to detect such differences. Given this is the first study of this nature, replication with a larger sample would enable ascertainment of “true” conversational elements which may be related to CR. Second, the study is limited in its generalizability. Specifically, the study was conducted in an environment where CR is paid mostly through provincial health insurance, so the issues identified herein may not be applicable in systems with other payment models. Third, the results are potentially biased due to selection issues, particularly that HCPs who consented to participate may not be representative of all HCPs. Participating patients and HCP may have been more positive in their attitudes and perceptions of CR than those who did not participate.
Fourth, in the absence of blinding, an expectation bias could have impacted the discussions. For instance, the recorded discussions may have been more likely to concern CR, than discussions that are not recorded. It is also possible that HCPs took extra care to optimize their communication, in a way that they would not have, if their discussions were not being recorded. It is likely that the frequency and quality of CR discussions is lower in the real world. This is also supported by the relatively high rate of CR referral in this study, than what is observed in population-based studies (Suaya et al., 2007). As part of quality assurance, the academic hospitals do assess the proportion of inpatients referred. While data is not available for the time of data collection for this study, referral rates from the third-quarter of 2013 showed much lower referral (33.9%).
Fifth, the time-limited nature of the recordings meant that we would not capture CR conversations that may have occurred at other points in the patient continuum of care. These other discussions or interactions with other HCP may have influenced whether or not the patient was referred to CR. Sixth, the small number of significant p-values identified in testing the second objective, may be chance findings as a result of multiple testing. Sixth, there are some limitations to our operationalization of the dependent variable of referral. Some patients may not have been referred to CR for valid personal or clinical reasons which were uncharted, and hence unmeasured in the current study. Moreover, for those patients for whom there was no charted referral and were called, their reporting of referral would be limited by recall failure or lack of awareness of referral to a site closer to home. Finally, some referrals for patients recruited from the community hospital may have been generated during outpatient visits. Seventh, some of the items were investigator-generated for the purposes of this study. Hence, their reliability and validity are unknown. Replication is warranted to ensure the findings are robust and not explained by alternative factors.
In conclusion, patient-HCP discussions about CR tend to involve HCPs giving information about therapy, followed by patients showing understanding and agreement. In addition these discussions involved HCP giving information and counselling around medical, psychosocial and therapeutic regimens, patients giving information surrounding their lifestyle, followed by their medical and therapeutic concerns. Discussions marked by greater interactivity and less patient concern and worry were related to greater patient CR referral. Further research to replicate these initial findings, and to assess whether HCPs can be trained to communicate in a referral-enhancing manner such that patient referral rates are increased, is warranted.
Acknowledgments
I confirm all patient/personal identifiers have been removed or disguised so the patient/person (s) described are not identifiable and cannot be identified through the details of the story.
We gratefully acknowledge the statistical input of Mirka Ondrack, MSc, of York University.
Funding
This study was funded by the Canadian Institutes of Health Research grant # TSH-112564.
Footnotes
There are no conflicting interests.
References
- Ades PA, Waldmann ML, McCann WJ, et al. Predictors of cardiac rehabilitation participation in older coronary patients. Archives of Internal Medicine. 1992;152(5):1033–1035. [PubMed] [Google Scholar]
- Arena R, Williams M, Forman DE, et al. Increasing referral and participation rates to outpatient cardiac rehabilitation: The valuable role of healthcare professionals in the inpatient and home health settings: a science advisory from the American Heart Association. Circulation. 2012;125(10):1321–1329. doi: 10.1161/CIR.0b013e318246b1e5. [DOI] [PubMed] [Google Scholar]
- Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond a presidential advisory from the American Heart Association. Circulation. 2011;124(25):2951–2960. doi: 10.1161/CIR.0b013e31823b21e2. [DOI] [PubMed] [Google Scholar]
- Bartlett EE, Grayson M, Barker R, et al. The effects of physician communications skills on patient satisfaction; recall, and adherence. Journal of Chronic Diseases. 1984;37(9–10):755–764. doi: 10.1016/0021-9681(84)90044-4. [DOI] [PubMed] [Google Scholar]
- Burgoon M. (Non) Compliance with disease prevention and control messages: communication correlates and psychological predictors. Journal of Health Psychology. 1996;1(3):279–296. doi: 10.1177/135910539600100303. [DOI] [PubMed] [Google Scholar]
- Dwamena F, Holmes-Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database of Systematic Reviews. 2012;12(12):CD003267. doi: 10.1002/14651858.CD003267.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace SL, Abbey SE, Shnek ZM, et al. Cardiac rehabilitation II: Referral and participation. General Hospital Psychiatry. 2002;24(3):127–134. doi: 10.1016/s0163-8343(02)00179-2. [DOI] [PubMed] [Google Scholar]
- Grace SL, Chessex C, Arthur H, et al. Systematizing inpatient referral to cardiac rehabilitation 2010: Canadian Association of Cardiac Rehabilitation and Canadian Cardiovascular Society joint position paper endorsed by the Cardiac Care Network of Ontario. The Canadian Journal of Cardiology. 2011;27(2):192–199. doi: 10.1016/j.cjca.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Grace SL, Evindar A, Abramson BL, et al. Physician management preferences for cardiac patients: Factors affecting referral to cardiac rehabilitation. The Canadian Journal of Cardiology. 2004;20(11):1101–1107. [PubMed] [Google Scholar]
- Grace SL, Gravely-Witte S, Brual J, et al. Contribution of patient and physician factors to cardiac rehabilitation enrollment: A prospective multilevel study. European Journal of Cardiovascular Prevention and Rehabilitation. 2008;15(5):548–556. doi: 10.1097/HJR.0b013e328305df05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heran BS, Chen JM, Ebrahim S, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database of Systematic Reviews. 2011;(7) doi: 10.1002/14651858.CD001800.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) The American Journal of Cardiology. 1989;64(10):651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows: Version 20.0. Armonk, NY: IBM Corp; 2011. [Google Scholar]
- Jackson L, Leclerc J, Erskine Y, et al. Getting the most out of cardiac rehabilitation: a review of referral and adherence predictors. Heart. 2005;91(1):10–14. doi: 10.1136/hrt.2004.045559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John D, MacArthur CT. Research Network on Socioeconomic Status and Health. 2000. The MacArthur Scale of Subjective Social Status. [Google Scholar]
- Kim YM, Rimon J, Winnard K, et al. Improving the quality of service delivery in Nigeria. Studies in Family Planning. 2013;23(2):118–127. [PubMed] [Google Scholar]
- Kottke TE, Faith DA, Jordan CO, et al. The comparative effectiveness of heart disease prevention and treatment strategies. American Journal of Preventive Medicine. 2009;36(1):82–88. doi: 10.1016/j.amepre.2008.09.010. [DOI] [PubMed] [Google Scholar]
- Lennon O, Carey A, Gaffney N, et al. A pilot randomized controlled trial to evaluate the benefit of the cardiac rehabilitation paradigm for the non-acute ischaemic stroke population. Clinical Rehabilitation. 2008;22(2):125–133. doi: 10.1177/0269215507081580. [DOI] [PubMed] [Google Scholar]
- McCorry NK, Corrigan M, Tully MA, et al. Perceptions of exercise among people who have not attended cardiac rehabilitation following myocardial infarction. Journal of Health Psychology. 2009;14(7):924–932. doi: 10.1177/1359105309341144. [DOI] [PubMed] [Google Scholar]
- Mitoff PR, Wesolowski M, Abramson BL, et al. Patient-provider communication regarding referral to cardiac rehabilitation. Rehabilitation Nursing. 2005;30(4):140–146. doi: 10.1002/j.2048-7940.2005.tb00097.x. [DOI] [PubMed] [Google Scholar]
- Nelson CL, Herndon JE, Mark DB, et al. Relation of clinical and angiographic factors to functional capacity as measured by the Duke Activity Status Index. The American Journal of Cardiology. 1991;68(9):973–975. doi: 10.1016/0002-9149(91)90423-i. [DOI] [PubMed] [Google Scholar]
- Prior PL, Hachinski V, Unsworth K, et al. Comprehensive cardiac rehabilitation for secondary prevention after transient ischemic attack or mild ttroke: I: Feasibility and risk factors. Stroke. 2011;42(11):3207–3213. doi: 10.1161/STROKEAHA.111.620187. [DOI] [PubMed] [Google Scholar]
- Ratzan SC. Effective decision-making: A negotiation perspective for health psychology and health communication. Journal of Health Psychology. 1996;1(3):323–333. doi: 10.1177/135910539600100306. [DOI] [PubMed] [Google Scholar]
- Roter D, Larson S. The Roter interaction analysis system (RIAS): Utility and flexibility for analysis of medical interactions. Patient Education and Counseling. 2002;46(4):243–251. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare mprofessionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on C. Stroke. 2006;37(2):577–617. doi: 10.1161/01.STR.0000199147.30016.74. [DOI] [PubMed] [Google Scholar]
- Scott LB, Gravely S, Sexton T, et al. Examining the effect of a patient navigation intervention on outpatient cardiac rehabilitation awareness and enrollment. Journal of Cardiopulmonary Rehabilitation and Prevention. 2013;33(5):281–291. doi: 10.1097/HCR.0b013e3182972dd6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanks LC, Moore SM, Zeller RA. Predictors of cardiac rehabilitation initiation. Rehabilitation Nursing. 2007;32(4):152–157. doi: 10.1002/j.2048-7940.2007.tb00169.x. [DOI] [PubMed] [Google Scholar]
- Stone JA, Arthur HM, Suskin N. Canadian guidelines for cardiac rehabilitation and cardiovascular disease prevention: Translating knowledge into action. 3. Canadian Association of Cardiac Rehabilitation; 2009. [Google Scholar]
- Suaya JA, Shepard DS, Normand SL, et al. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116(15):1653–1662. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- Tang A, Marzolini S, Oh P, et al. Feasibility and effects of adapted cardiac rehabilitation after stroke: A prospective trial. BMC Neurology. 2010;10:40. doi: 10.1186/1471-2377-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: Systematic review and meta-analysis of randomized controlled trials. The American Journal of Medicine. 2004;116(10):682–692. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- Tsui CK, Shanmugasegaram S, Jamnik V, et al. Variation in patient perceptions of healthcare provider endorsement of cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation and Prevention. 2012;32(4):192–7. doi: 10.1097/HCR.0b013e318255a39d. [DOI] [PubMed] [Google Scholar]
- The Roter Interaction Analysis System (RIASWorks) [accessed 2 February 2012];Evidence-based communication for education research and practice. 2012 Available at: http://www.riasworks.com/resources_i.html.
- Thomas RJ, King M, Lui K, et al. AACVPR/ACCF/AHA 2010 Update: Performance Measures on Cardiac Rehabilitation for Referral to Cardiac Rehabilitation/Secondary Prevention Services Endorsed by the American College of Chest Physicians, the American College of Sports Medicine, the American Physical Therapy Association, the Canadian Association of Cardiac Rehabilitation, the Clinical Exercise Physiology Association, the European Association for Cardiovascular Prevention and Rehabilition the Inter-American Heart Foundation, the National Association of Clinical Nurse Specialists, the Preventative Cardiovascular Nurses Association, and the Society of Thoracic Surgeons. Journal of the American College of Cardiology. 2010;56(14):1159–1167. doi: 10.1016/j.jacc.2010.06.006. [DOI] [PubMed] [Google Scholar]
- Van Weert J, Van Dulmen S, Bär P, et al. Interdisciplinary preoperative patient education in cardiac surgery. Patient Education and Counseling. 2003;49(2):105–114. doi: 10.1016/s0738-3991(02)00091-5. [DOI] [PubMed] [Google Scholar]
- World Health Organization. [acessed 17 March 2012];Cardiovascular Diseases: fact sheet N°317. 2011 Available at: http://www.who.int/mediacentre/factsheets/fs317/en/index.html.